ch 9: Drug Misuse and Addiction
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
what are recreational drugs + most popular (legal + illegal) (4)
psychoactive substances consumed voluntarily
have the potential to be used in a problematic way
illegal in US → marijuana
legal drugs: alcohol, tobacco
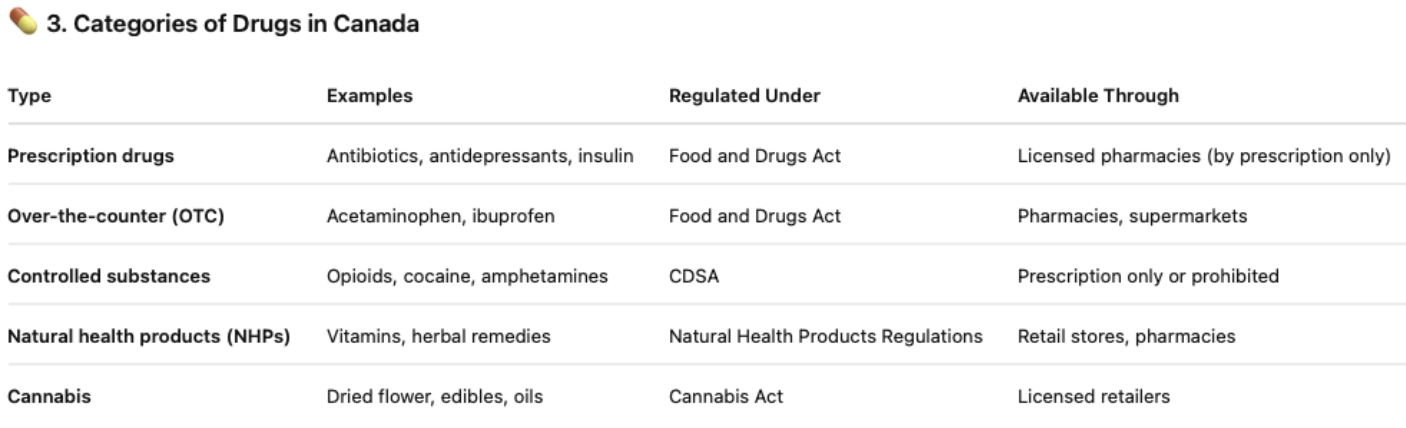
categories of drugs in Canada (5)
prescription drugs: antibiotics, antidepressants, insulin
over-the-counter (OTC): acetaminophen, ibuprofen
controlled substances: opioids, cocaine, amphetamines
natural health products (NHPs): vitamins, herbal remedies
cannabis: dried flower, edibles, oils
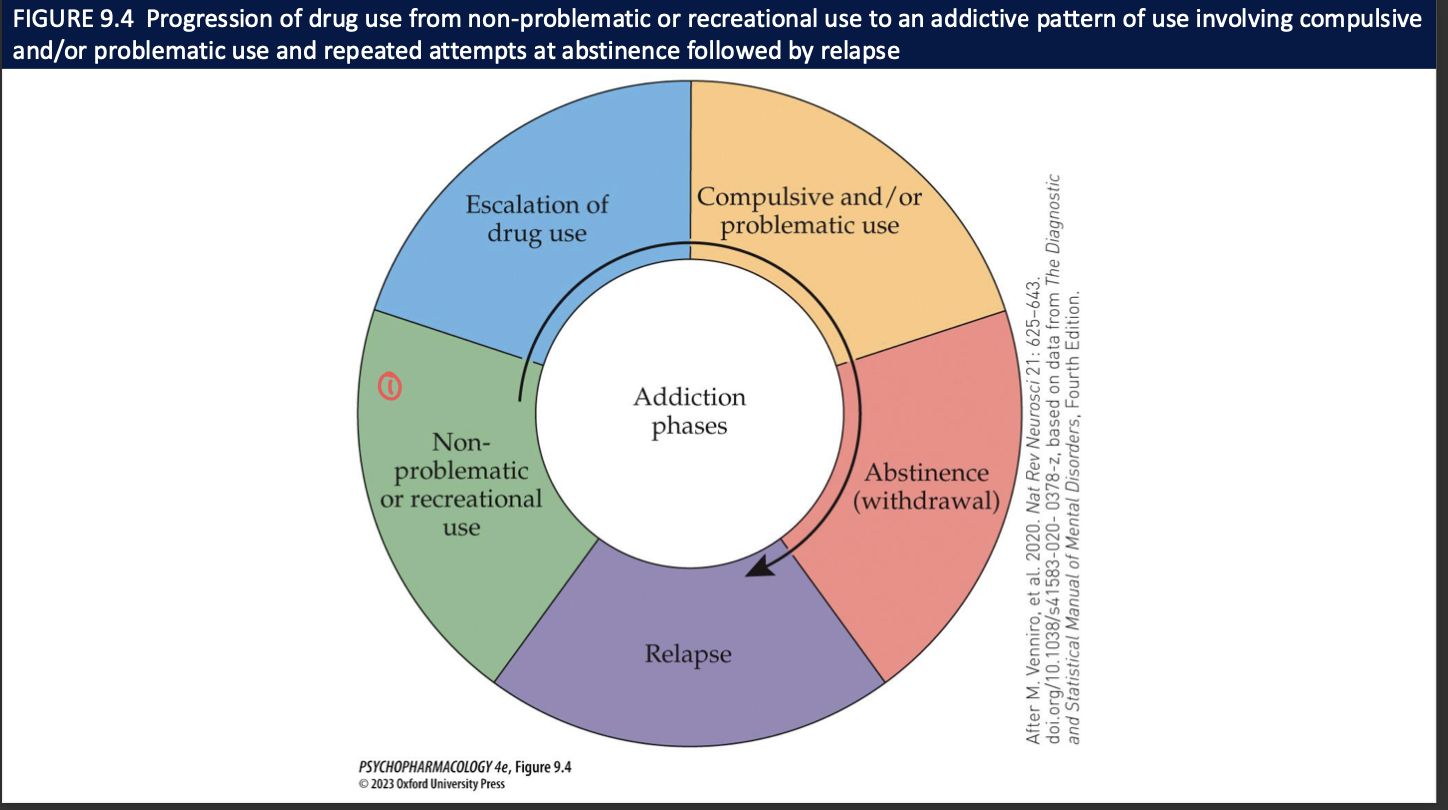
what characterizes a drug addiction (3)
considered to be chronic, relapsing behavioural disorder
focus is on compulsive features of drug seeking + use including craving
individuals remain addicted for long periods of time → drug-free periods (remission) often followed by relapses
substance use vs substance-induced disorders (2)
substance use disorders: cognitive, bhvrl and physiological symptoms indicating that the individual continues using the substance despite significant substance-related problems
substance-induced disorders: reversible substance-specific syndrome due to recent ingestion of a substance (ie, ↑bp)
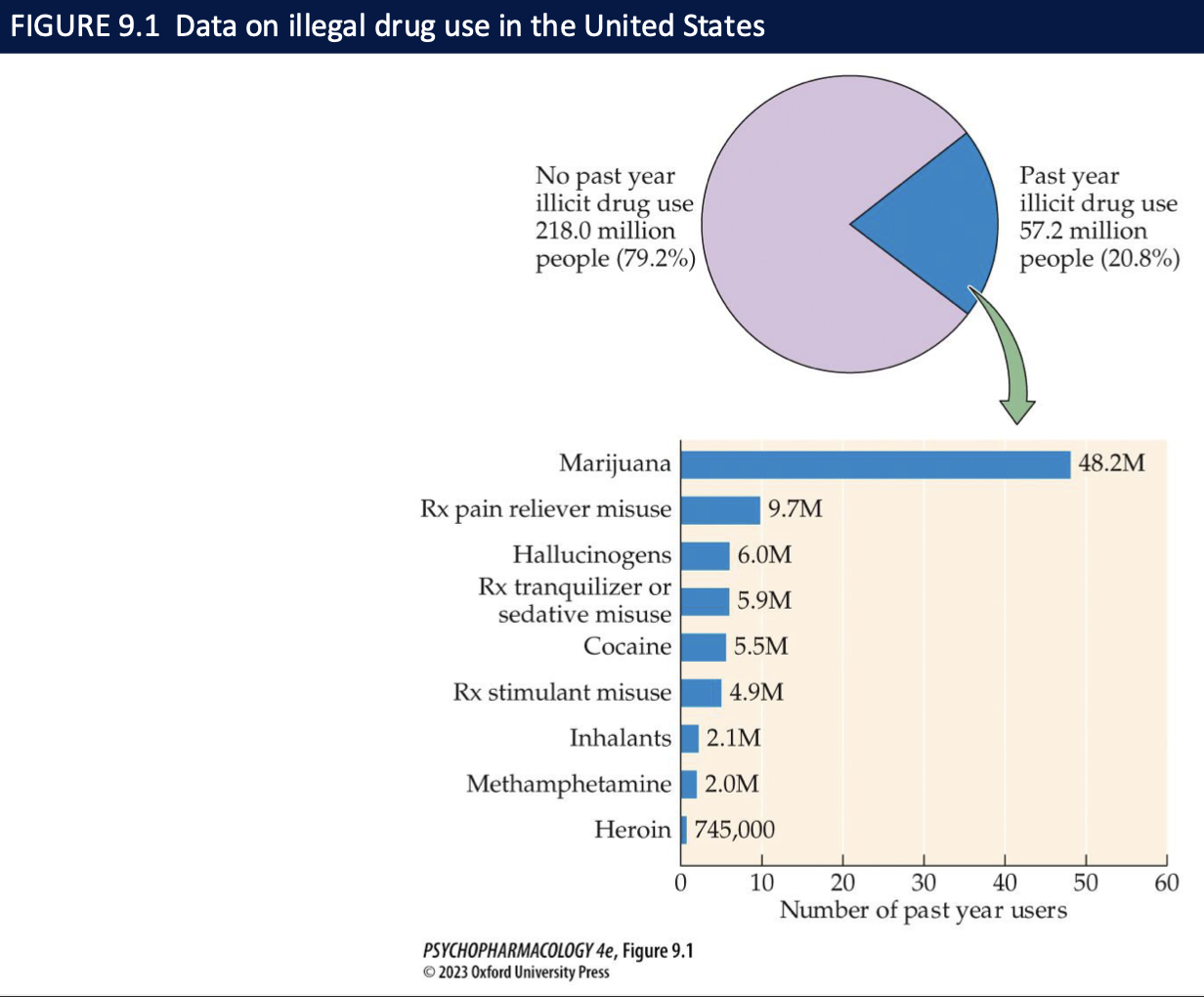
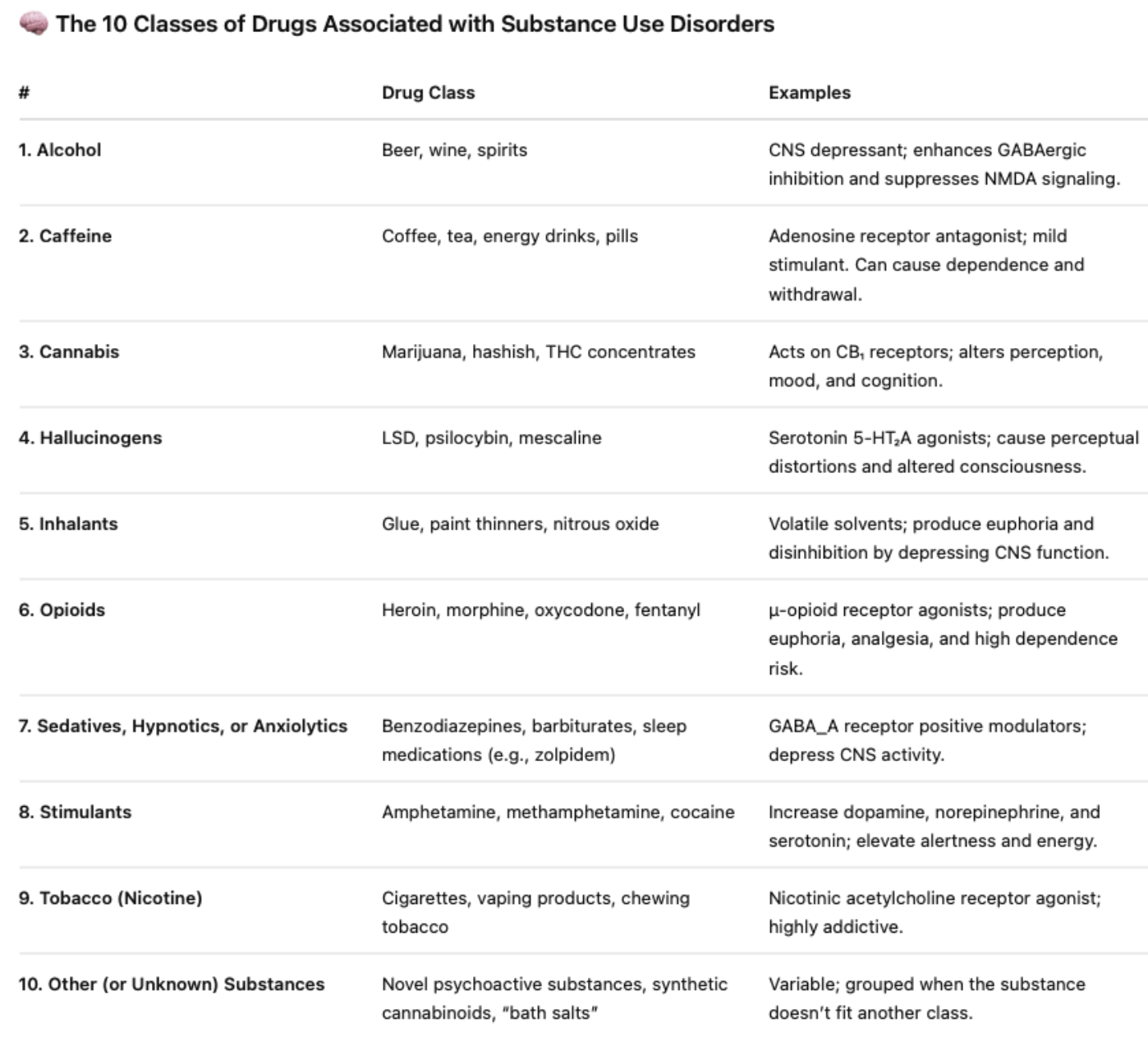
substance-related disorders → what do they have in common + what are the 10 classes
all substances have the ability to activate the neural circuitry that mediates rewards
alcohol: beer, wine, spirits
caffeine: coffee, tea, energy drinks, pills
cannabis: marijuana, hashish THC concentrates
hallucinogens: LSD, mescaline
inhalants: glue, paint thinners, nitrous oxide
opioids: heroin, morphine, oxycodone, fentanyl
sedatives, hypnotics, anxiolytics benzodiazepines, barbiturates
stimulants: amphetamine, methamphetamine, cocaine
tobacco (nicotine): cigarettes, vaping, chewing tobacco
other (unknown) substances
DSM-5 criteria to diagnose substance use disorder (3)
pattern of use must be problematic + must lead to clinically significant impairment or distress
no single criterion for determining presence of a substance use disorder
severity: mild-severe → depending on how many of the diagnostic criteria are met
____ is the only compulsive behavioural disorder in the DSM-5 → meets several of the criteria for ______ and shows similar _____ and ______ dysfunctions
gambling
substance abuse disorder
neurobiological
cognitive
two types of progression in drug use
gateway theory: progress from legal substances like alcohol → marijuana → cocaine/heroin/etc
regular pattern → problematic use (addictive) and many people mature out of it → alcohol/illicit drug use decline w age
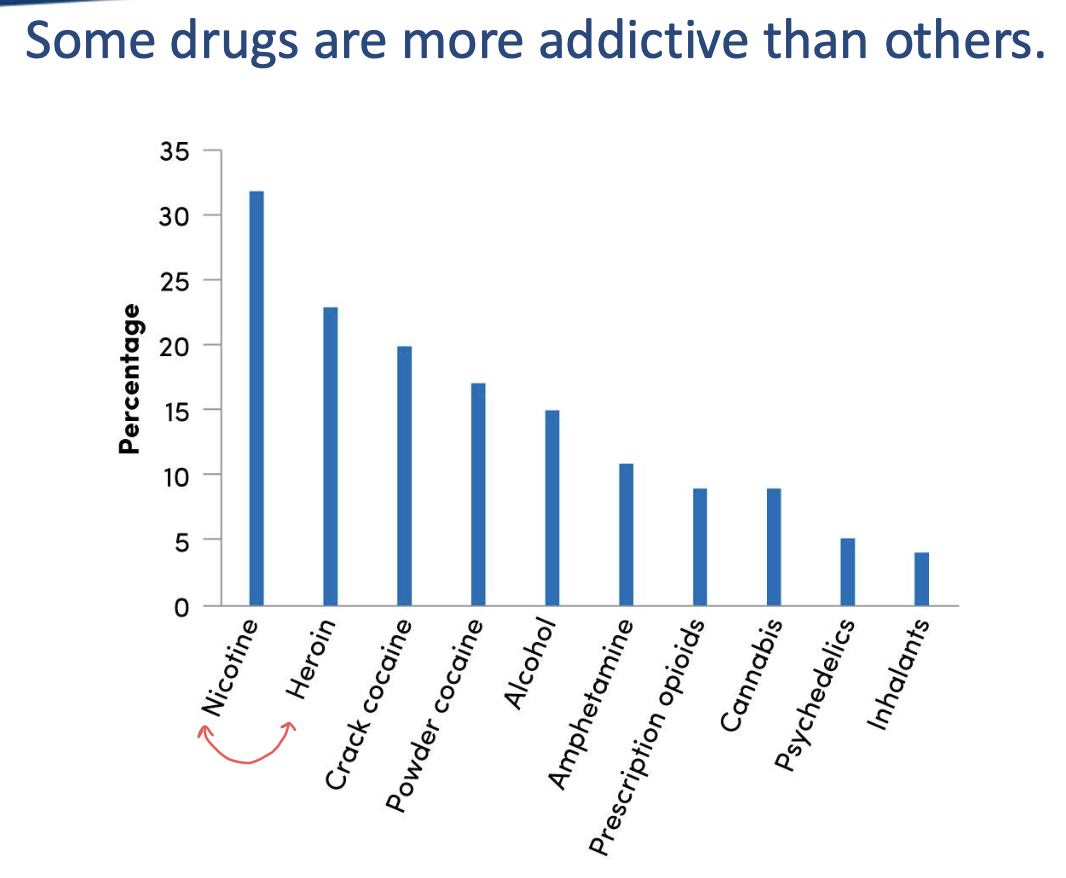
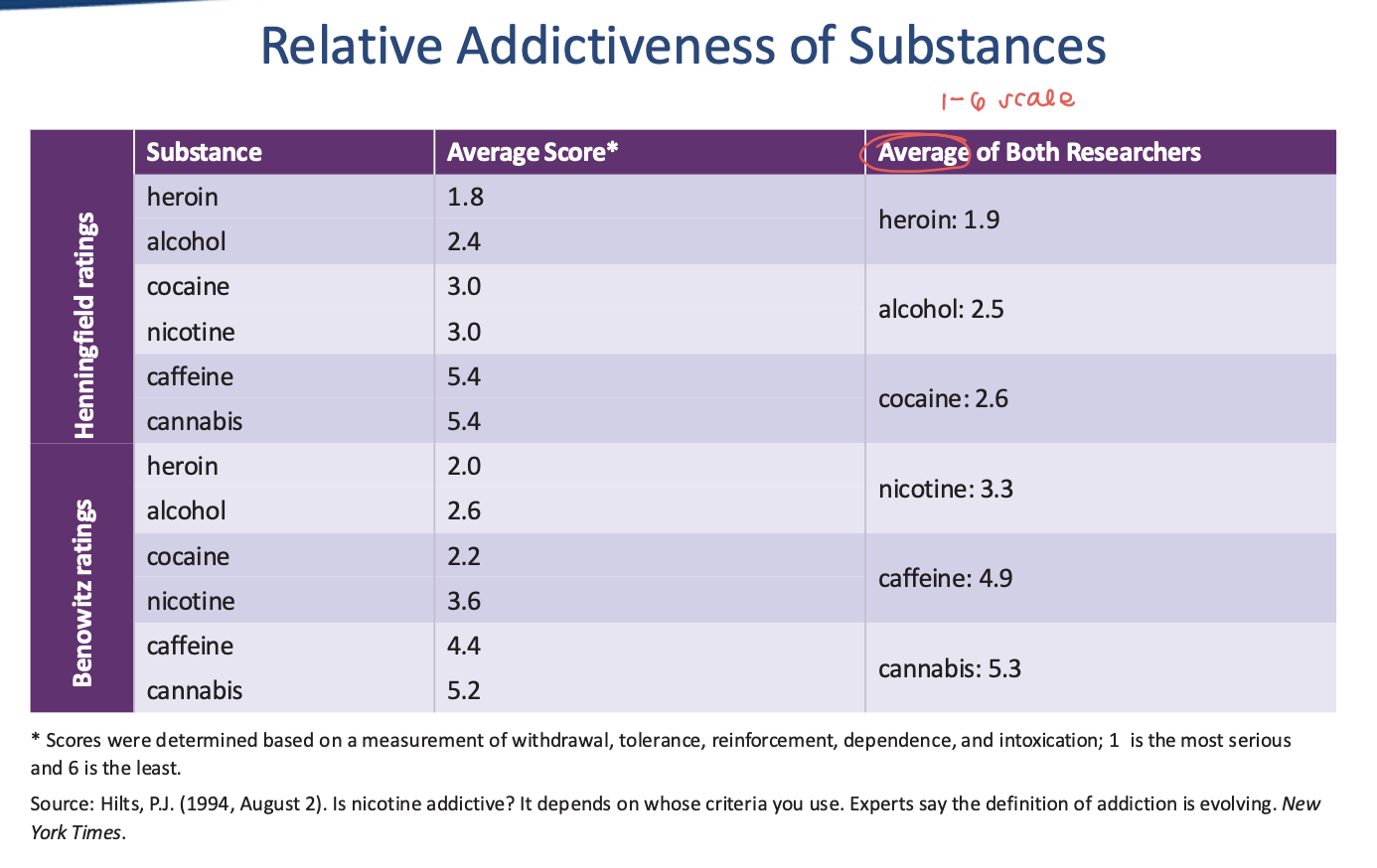
schedule of controlled substances + factors that need to be considered (4)
5 classes → based on degree of potential misuse and medicinal value
capture ratio: percent who try a drug and become habitual users
considering withdrawal, tolerance, reinforcement, dependence, and intoxication
heroin, alcohol, nicotine most addictive → caffeine, hallucinogens, cannabis least addictive
about ___% of Canadians (____million people) will meet the criteria for a substance use disorder at some point in their life → many struggle from _____ (AUD) → ___% of males and % of females of the age of ___
21.6%
6 million ppl
alcohol use disorder (AUD)
5% of males
2% of females
15
how does addiction correlate w race in Canada? (3)
significant negative impacts on indigenous communities → solvent abuse
alcohol deaths are twice as high + illegal drug deaths three times as high in indigenous communities vs general population
also high in African, Caribbean, and Black Canadians
how does addiction correlate w age in Canada? (4)
20-24 year old Canadians are most likely to exceed Canada’s low-risk drinking guidelines
age 55 and older tend to use alcohol + other drugs less frequently than younger Canadians
alcohol _ prescription drug abuse increases
substance abuse symptoms can mimic other medical/bhvrl conditions
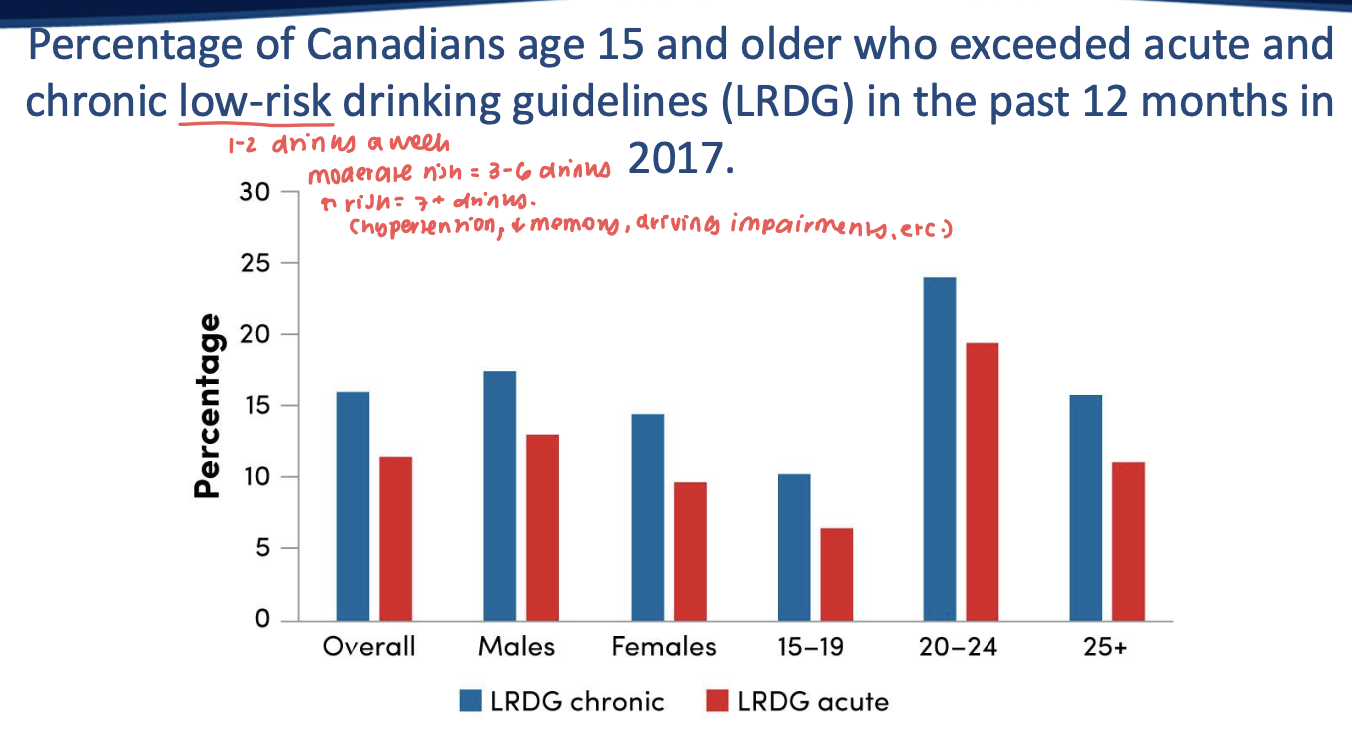
how does addiction correlate w gender in Canada? (4)
sex differences linked to female reproductive hormones/differences in stress responding
men are 70% more likely to be dependent on drugs/alcohol
men more likely to begin abusing drugs as a part of a pattern of risky bhvr or to enhance social bhvr
women: more likely to use drugs to reduce stress, anxiety, loneliness, depression → progress faster from first use to problematic use (telescoping)
how is addiction co-diagnosed with a psychiatric disorder in men vs women (2)
women: depression, anxiety, phobias
men: ADHD and antisocial personality disorder
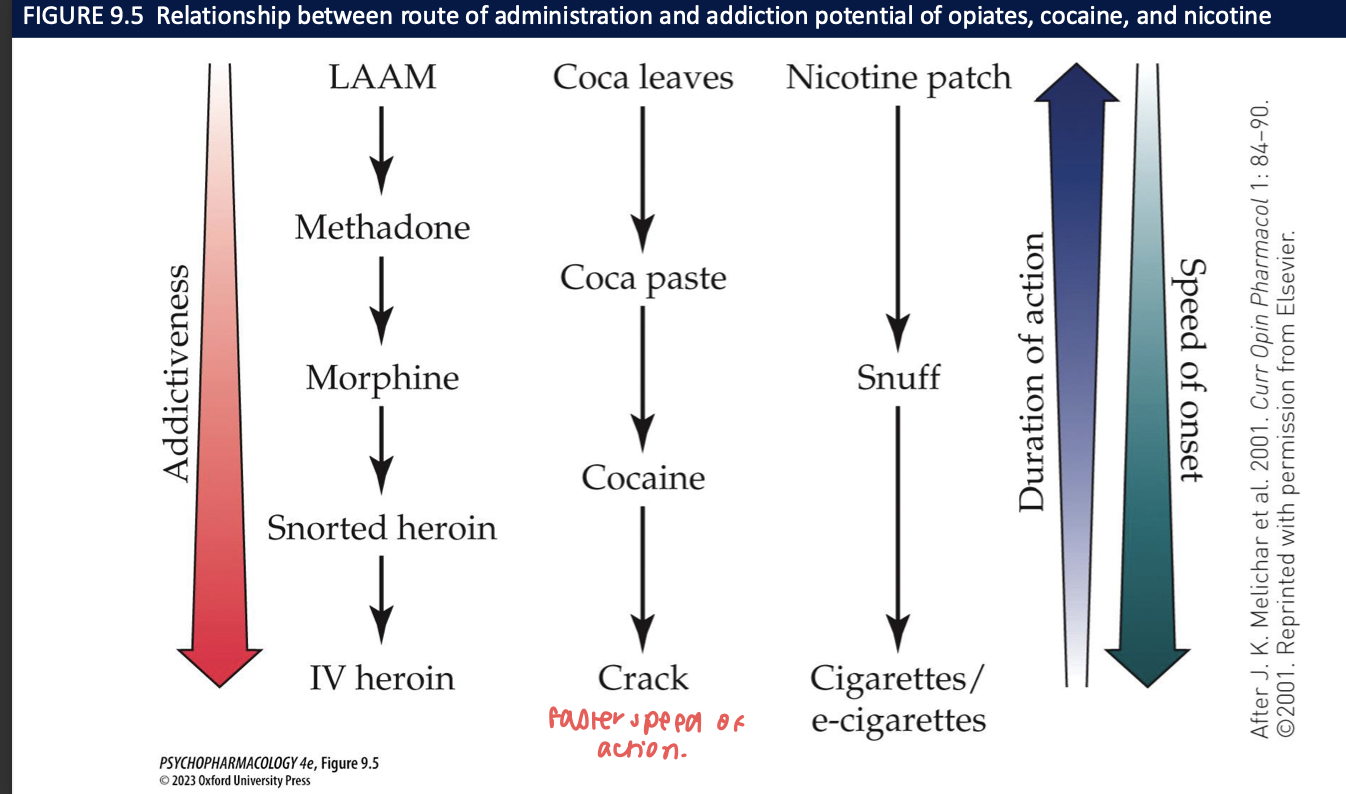
how does the route of administration affect the addictive potential of a substance?
routes that cause fast onset of drug action have the greatest addiction potential → produce strongest euphoric effects + shortest latency
shorter latency btw response + reinforcement would lead to stronger + faster drug conditioning
IV/inhalation: rapid drug entry + fast onset of drug action → shorter duration
oral/transdermal: relatively slow absorption → slow drug availability to the brain
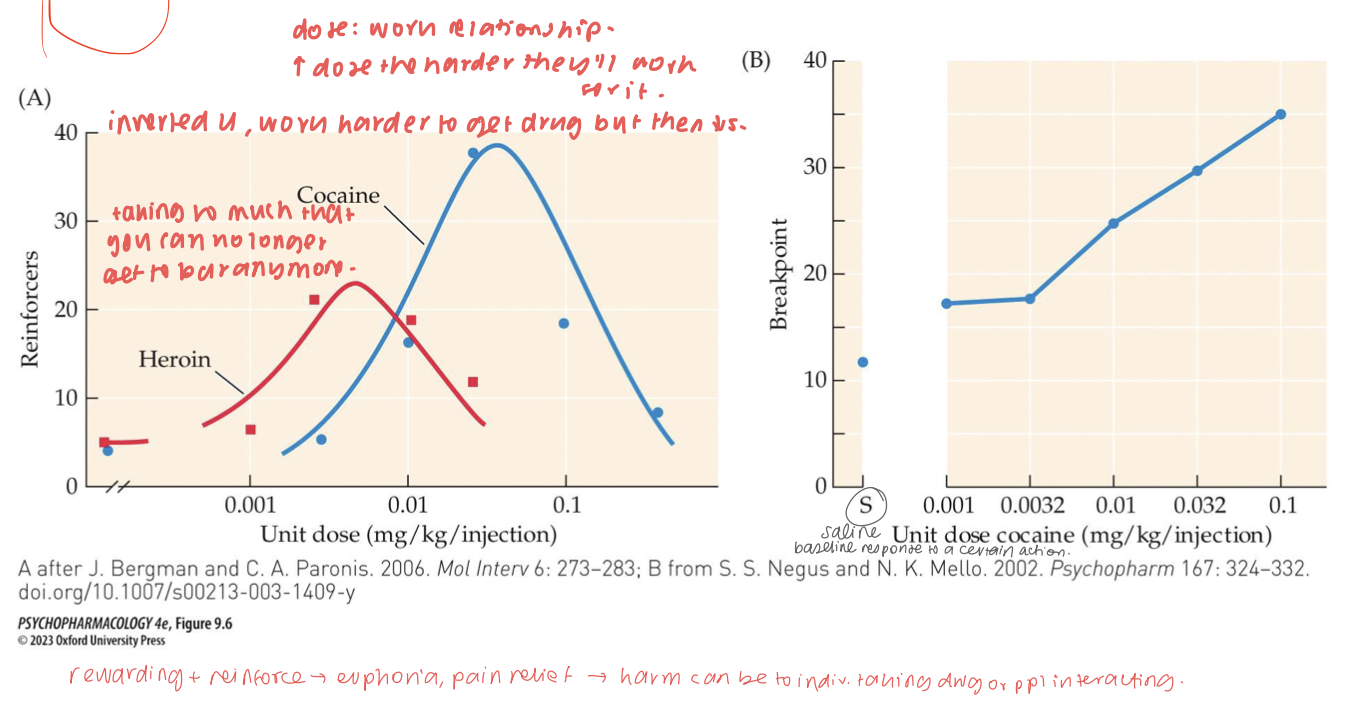
In IV self-administration, how do fixed-ratio and progressive-ratio schedules differ, and what does breakpoint index? (2)
FR: same number of presses per infusion; yields U-shaped dose–response for reinforcers (low dose = weak effect; mid = peak; high dose = aversion/sedation ↓ responding).
PR: response requirement escalates each infusion; the breakpoint (last ratio achieved) indexes motivation/reinforcing strength of the drug.
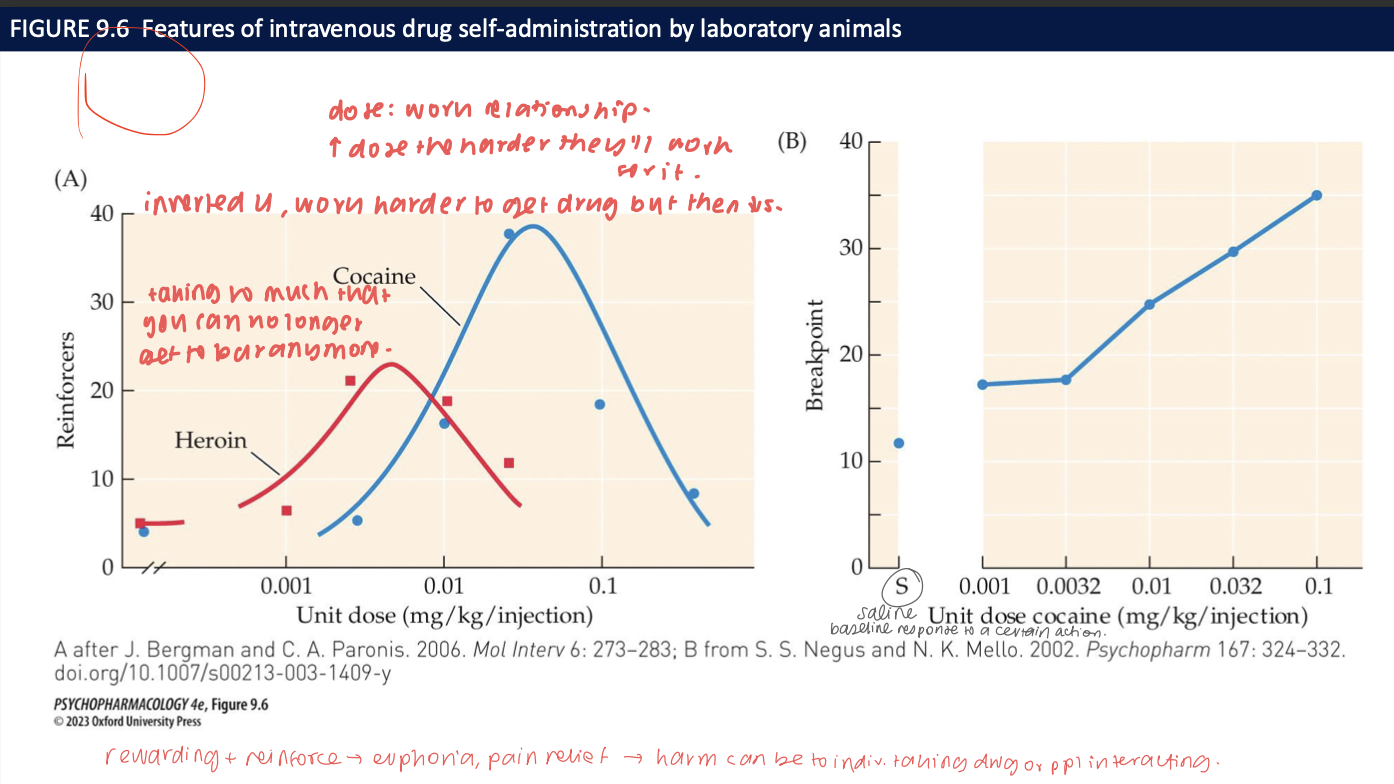
Why do many drugs show a U-shaped self-administration curve under fixed-ratio (FR) schedules? (2)
Low doses are sub-threshold (not rewarding enough) → low responding; moderate doses maximize reward with tolerable side effects → peak responding;
high doses produce aversive/sedating/toxic effects or rapid satiation → reduced responding.
In the reinstatement model, what 3 triggers can restore extinguished drug seeking, and what do they represent clinically? (4)
Drug priming,
stress, and
drug-paired cues.
Clinically map to drug exposure, stressful events, and environmental reminders, respectively—key drivers of relapse in humans.
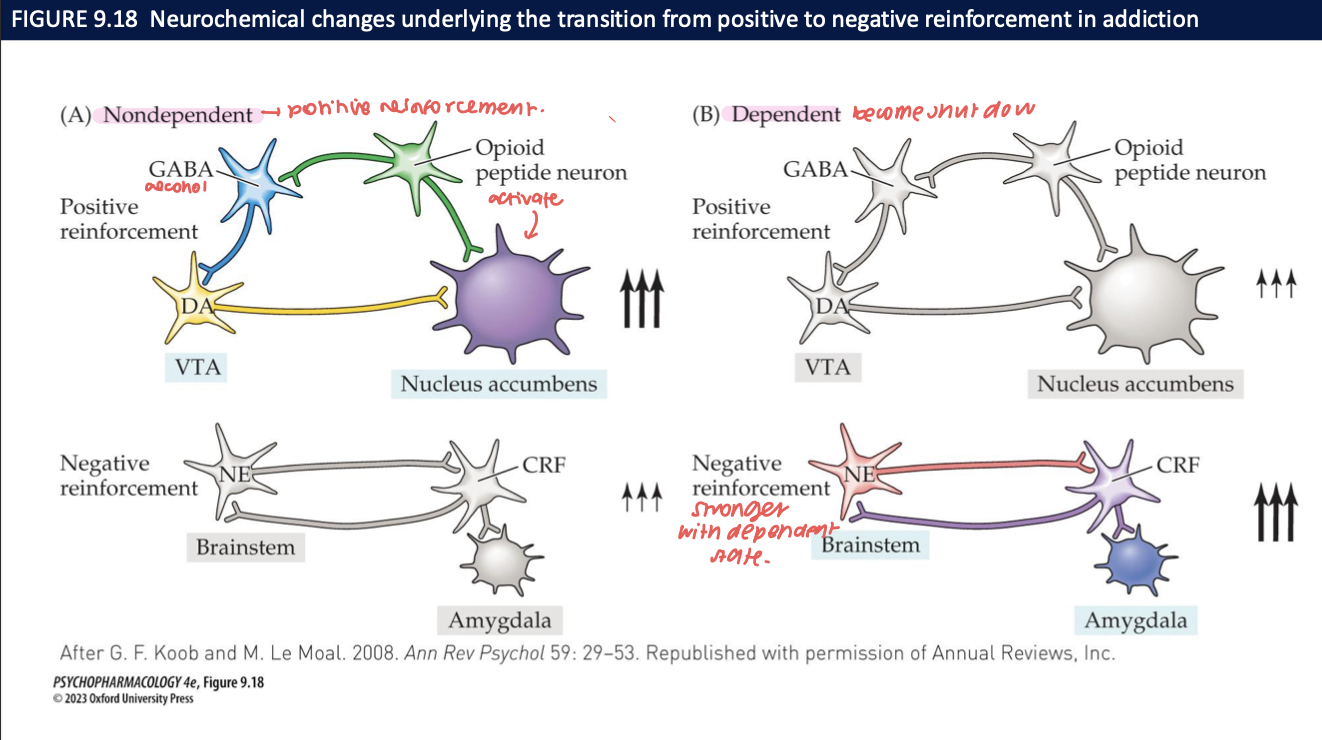
____ plays a key role in establishing and maintaining drug addiction → withdrawal symptoms (______) motivates users to take the drug again → (_____)
physical dependence
abstinence syndrome
negative reinforcement
what do the experimental results from heroin studies support in the treatment of opioid-dependence? (2)
support the use of agonist replacement theory in the treatment of opioid-dependence
ie. methadone or buprenorphine
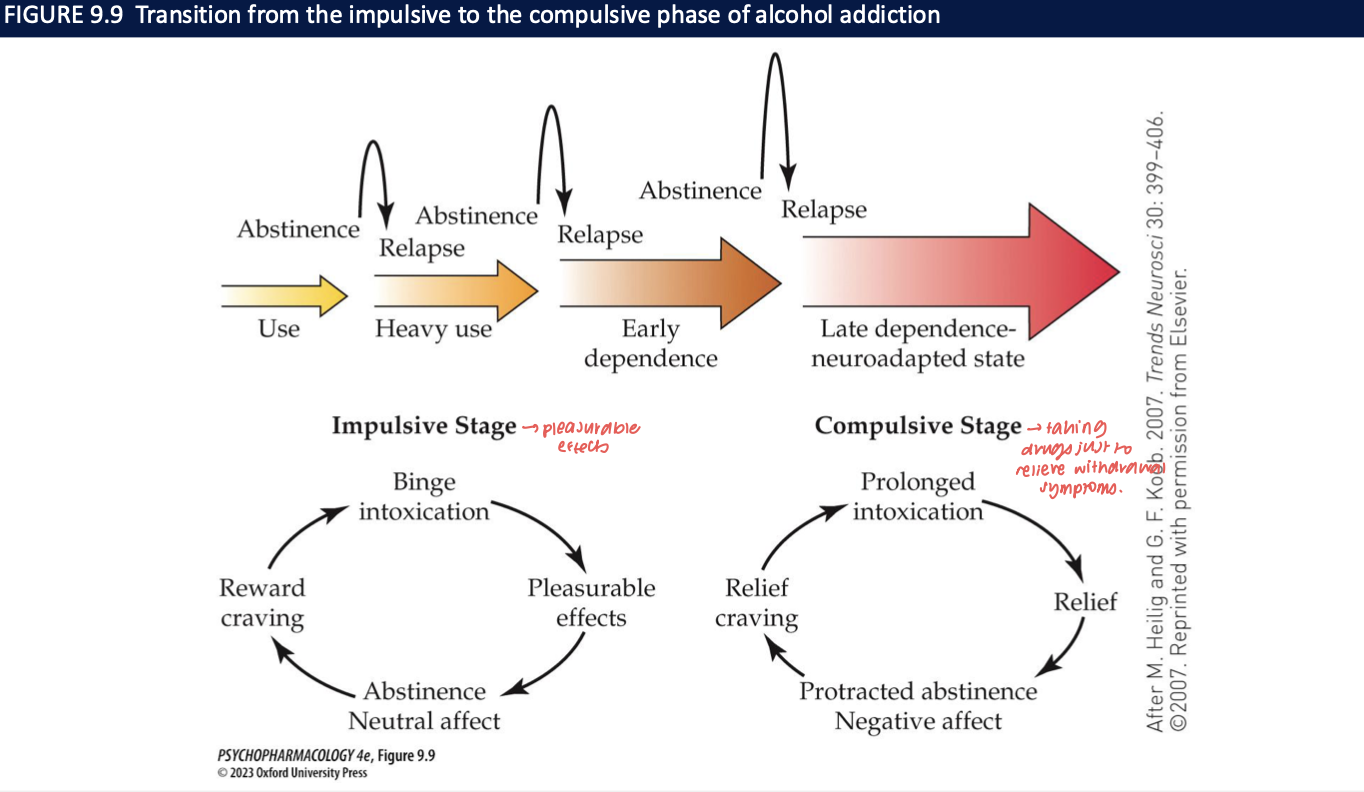
drug-taking behaviour progresses from _____ → ______. this process may be due to _____ system in the brain (_____)
impulsive stage
compulsive stage
gradual recruitment of an antireward system
neuroadapted state
how do genetic factors contribute to the risk for addiction? (3)
heritability of substance use disorders is in the range of 40-60%
remaining variability is due to environmental factors → epigenetic and gene-by-environment interactions
genetic component is only expressed in ppl w specific life events ie. stressful events
Name key psychosocial risk factors for developing SUD, especially in adolescence. (10)
Younger age;
less education;
minority status (contextual inequities);
unemployment;
conduct problems;
high stress load & poor coping;
family conflict/violence;
inadequate parental monitoring;
childhood maltreatment;
psychiatric comorbidity (anxiety, mood, personality disorders). 🧠
Contrast the self-medication and shared etiology hypotheses for SUD–psychopathology comorbidity. What’s the current evidence? (3)
Self-medication: people use drugs to relieve symptoms (e.g., anxiety → sedatives, depressed→ stimulants).
Shared etiology: common genetic/environmental vulnerabilities raise risk for both addiction + psychiatric disorders
Evidence: not mutually exclusive—both likely operate; varies by person and drug. 🔁
How can social environment raise or lower addiction risk? Give risk and protective examples. (2)
Risk: social facilitation and drug-using peer groups, subculture norms, loss of conventional roles/responsibilities, family instability.
Protective: supportive network, stable lifestyle/structure, alternative reinforcers (work, hobbies, sports), and coping-skills training for stress. 🛡
natural recovery from substance misuse + addiction (2)
transitioning from substance misuse/addiction → non-problematic use → nonuse without assistance
may be facilitated by transitional life events and/or negative consequences of continuing drug use
what helps the maintenance of abstinence (5)
avoiding drug-associated cues,
non-drug sources of reinforcement,
new social support networks,
financial stability
achieving a general structure to the individual’s life
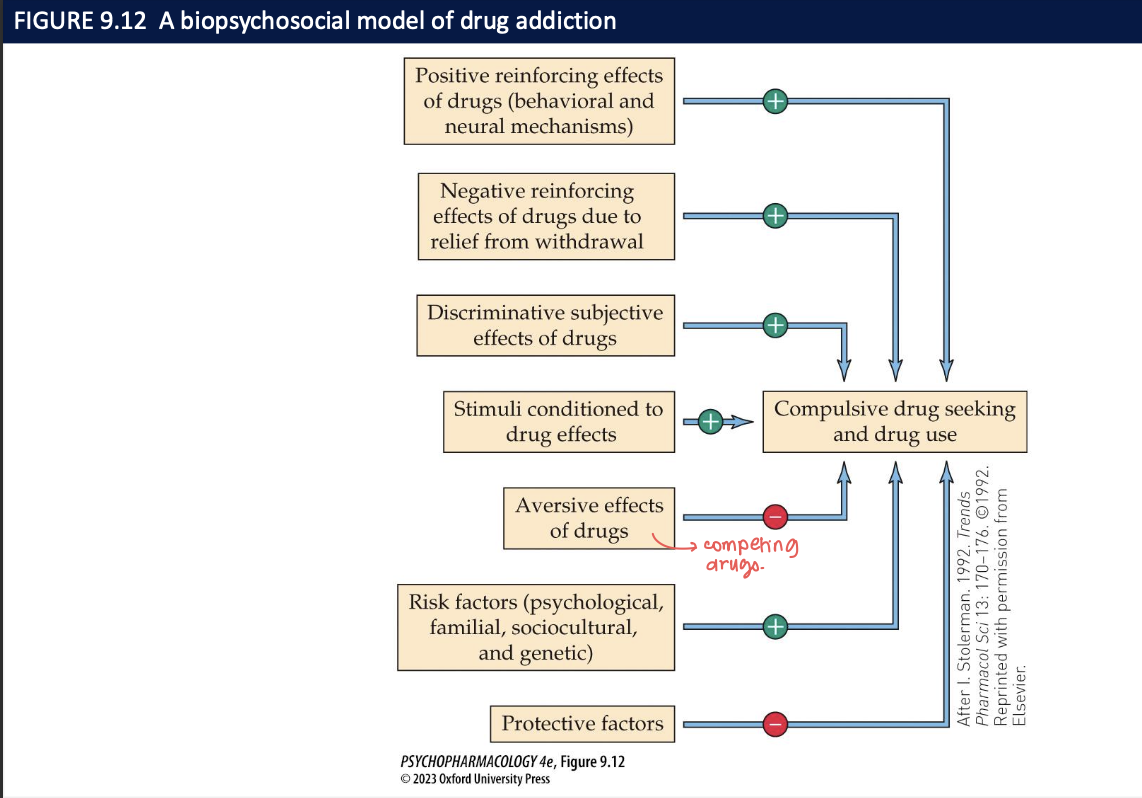
biopsychosocial model of addiction (2)
includes the full range of pharmacological, biological, and psychological/sociocultural factors that influence addiction risk
some factors promote the likelihood of substance misuse + addiction → others reduce it
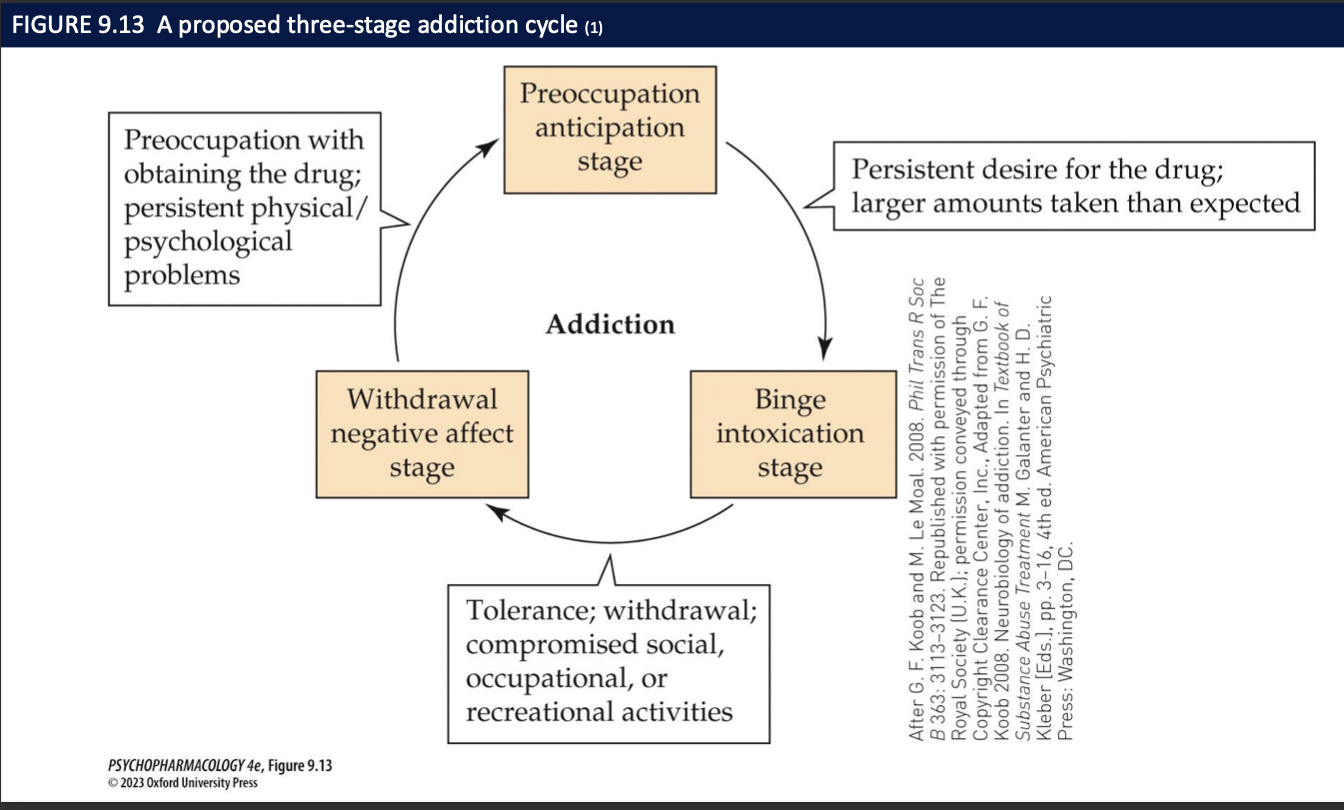
development of addiction has been conceptualized as a repeating cycle of 3 stages:
preoccupation with + anticipation of obtaining + using the substance
escalating use → drug binges + intoxication
withdrawal + associated negative effects
how do most recreational drugs affect the reward circuit in the brain? (5)
all recreational drugs activate the mesolimbic DA pathway from the VTA → NAcc
psycho-stimulants: directly elevate synaptic DA lvls
opioids/alcohol/nicotine/cannabinoids indirectly ↑ NAc DA
opioids: u-opioid disinhibits VTA neurons
nicotine excites VTA
alcohol/cannabinoids modulate network that increases net DA
_____pathway important bc early use is dominated by _____ → the drug ___ the probability of ___ bc it feels good/strongly wanted
the mesolimbic DA pathway from the VTA → NAcc
positive reinforcement
increasing
re-use
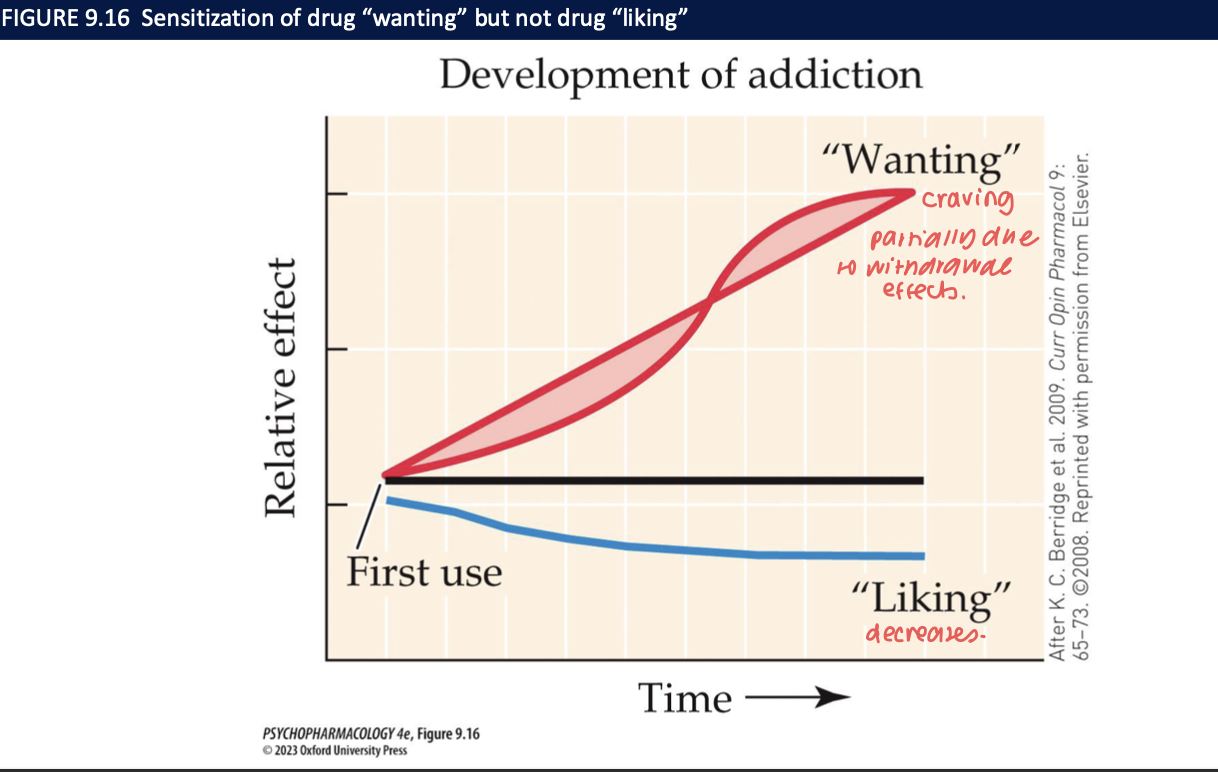
incentive sensitization theory (4)
distinction btw liking vs wanting a reward
drug reward declines due to tolerance
liking peaks early then declines → wanting increases + stays high
positive → negative reinforcement
What neural changes drive the preoccupation/anticipation stage of addiction, and how do they bias behavior? (3)
PFC dysregulation (dlPFC/ACC: control↓; vmPFC/OFC: over-valuation of drug cues) ➜ corticostriatal shift from goal-directed (DMS) to habit (DLS) ➜ cue-triggered seeking and poor impulse control → relapse.
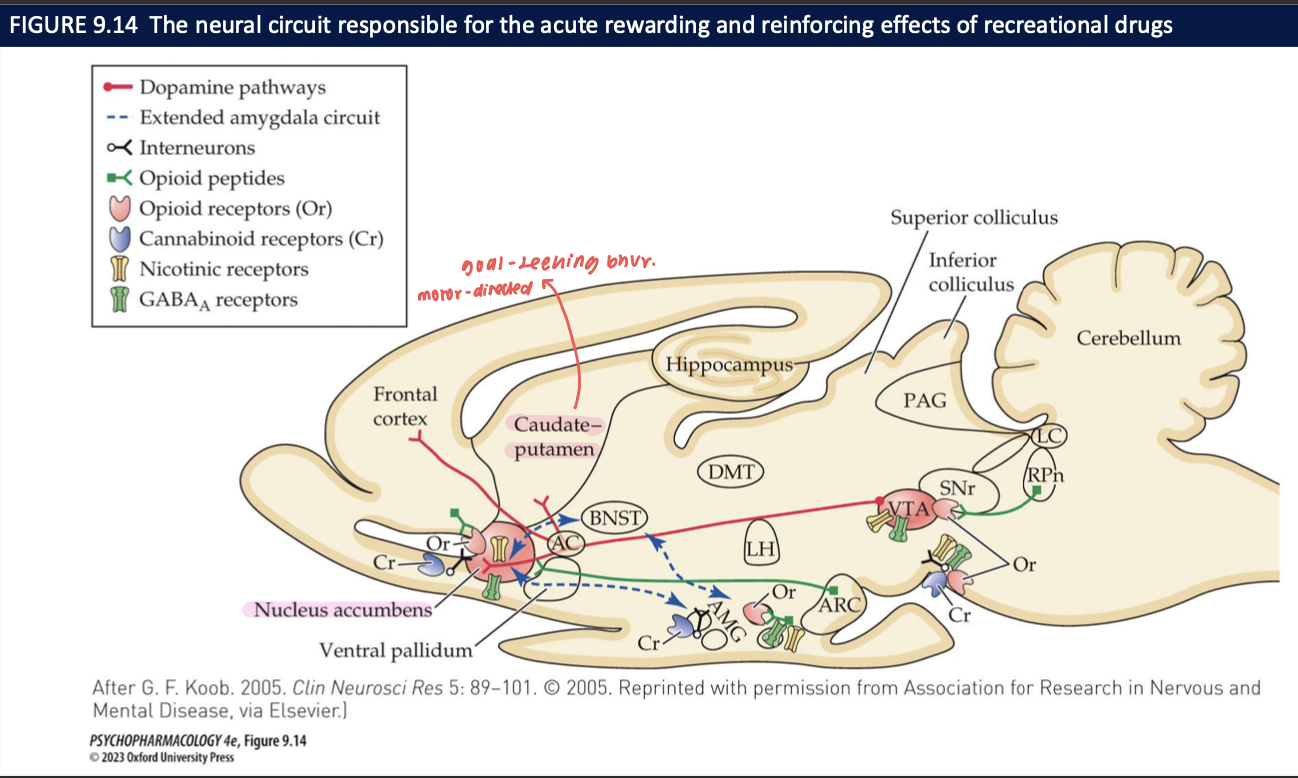
In the binge/intoxication stage, distinguish reward (“liking”) from incentive salience (“wanting”) and name the core circuit. (4)
Liking = hedonic pleasure; wanting = motivational pull of drug/cues.
Core circuit: mesolimbic DA, VTA → nucleus accumbens (NAc).
Stimulants ↑ DA directly (DAT effects);
opioids, nicotine, alcohol, cannabinoids ↑ DA indirectly (e.g., μ disinhibition of VTA).
How do liking and wanting change with repeated use, and what signals stamp in cue–drug learning? (4)
Liking ↓ (tolerance);
wanting ↑/persists (incentive sensitization to cues).
Phasic DA reward-prediction-error signals strengthen cue–drug associations.
Opioid & endocannabinoid systems also reinforce.
Which systems mediate the withdrawal/negative affect stage, and how does motivation shift? (2)
CRF, NE, dynorphin in the extended amygdala → hyperkatifeia (dysphoria, anxiety) and anhedonia.
Motivation flips from positive (“use to feel good”) to negative reinforcement (“use to stop feeling bad”).
Why can craving reappear long after abstinence? What neural substrates are implicated? (2)
Long-lasting plasticity in reward (VTA→NAc) and anti-reward (extended amygdala) circuits;
gene/epigenetic changes and altered synaptic strength sustain vulnerability to cue-induced craving.
Summarize the brain disease vs choice/motivational models of addiction and the testable prediction each makes. (3)
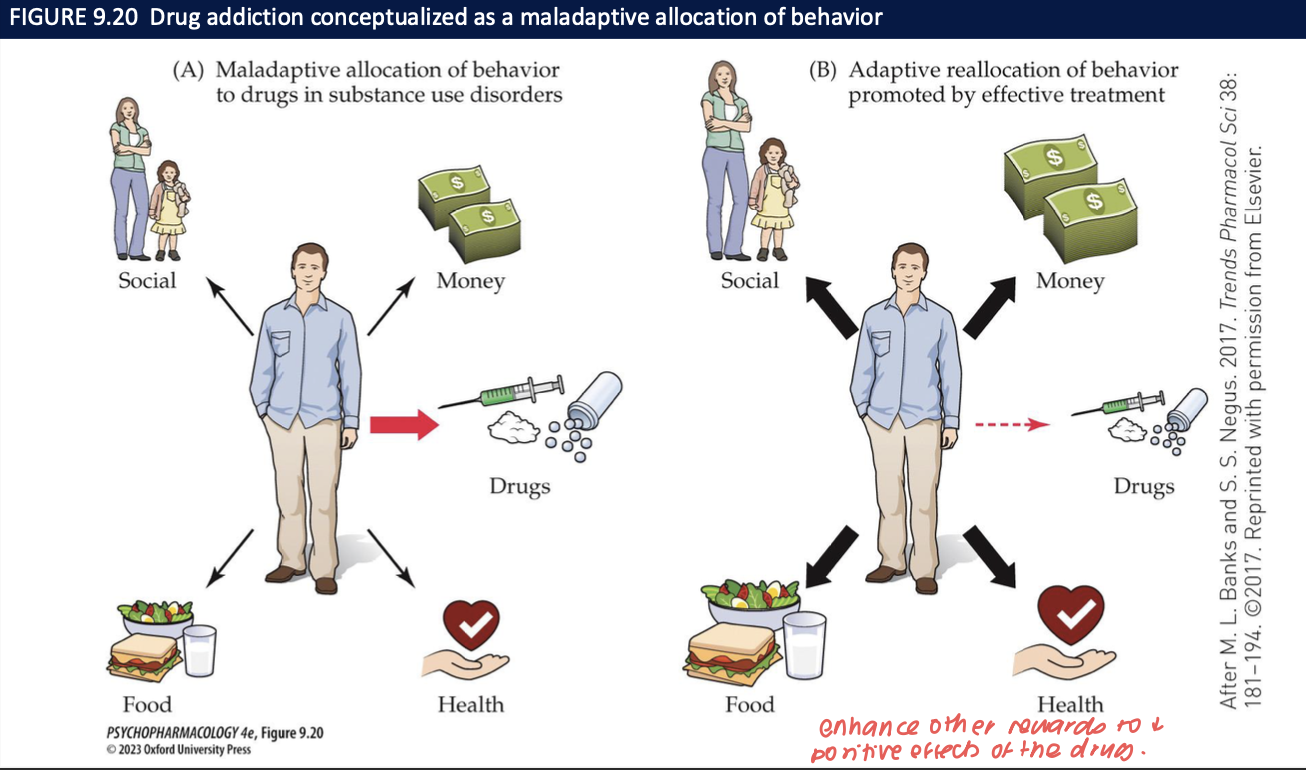
Brain disease: pathological circuit dysregulation; predicts persistent vulnerability despite intentions.
Choice/motivational: drug use serves functions (relief, scarce alternatives); predicts changing contingencies (access to non-drug rewards) reduces use. Best view integrates both.
What is contingency management, and why does it work? (2)
Behavioral treatment delivering immediate, certain non-drug rewards for verified abstinence.
It reallocates behavior toward alternative reinforcers, countering delay discounting and competing with drug reward.