Lecture 15: Joint Arthroplasty Material Properties
1/56
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
What are indications for arthroplasty / joint replacement?
Certain types of fractures
Poor healing secondary to lack of blood flow
Painful joints that have been resistant to other forms of treatment
Post-traumatic / surgery that resulted in joint destruction
What is the goal of joint replacement?
To improve function of a joint and decrease pain for long-term usage
What is the relationship between age and the life-span of a joint replacement?
Inverse relationship
The older you are → longer the replacement is good for
What is the most common joint replacement?
TKA is most common (THA most successful and cost-effective)
What are mechanical reasons that may cause a joint replacement to fail?
Instability / dislocation
Aseptic loosening
Wear and osteolysis
T/F: Type and location greatly influence the success rate of a joint replacement
True!
Why is finite element modeling important?
Used to help improve the fit of the implant for the patient to reduce the number of poor outcomes
After a hip replacement, what changes can be seen in their gait?
Patient’s often have balance deficits and slower walking speeds
Reduced GRF or patterns of muscle activity
Reduced joint forces or motion compared to the unaffected/normal side
Reduced ROM
Why is abnormal gait seen in patient’s who are post-THA?
Abnormal gait can serve as a protective measure to reduce the load on the prosthetic
This can be good early on but leads to problems down the road (e.g., increase the likelihood of needing a contralateral hip or knee replacement)
Why is gait training important after an individual undergoes a joint arthroplasty?
To teach the patient how to use the replacement more effectively and avoid potential problems
Abnormal gait has been shown to create ____x more likelihood of developing the need for a contralateral knee or hip replacement
Abnormal gait has been shown to create a 400x more likelihood of developing the need for a contralateral knee or hip replacement
(increased knee adduction moment on the contralateral knee)
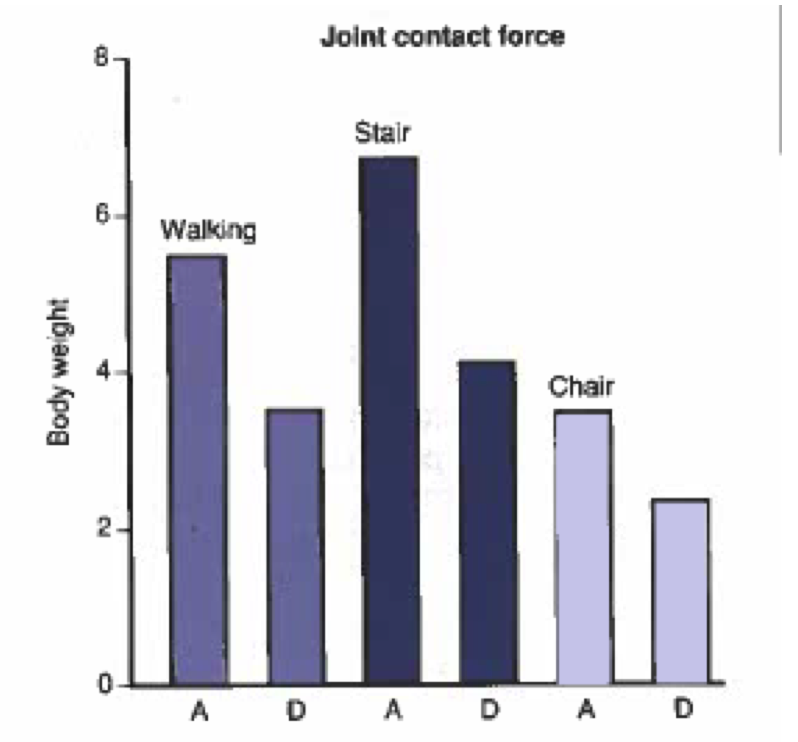
Predicted joint forces are minimized when the joint center is moved in what direction(s)?
Medially, inferiorly, and anteriorly
Photo:
A = Normal location of hip joint center
D = medial, inferior, anterior hip joint ceneter
T/F: The knee joint is a hinge joint.
Why or why not?
False!
Hinge joint means only 1 DOF & knee joint needs to allow for 3D movement (rotation, frontal plane movement, etc.)
A TKA needs to allow for __ DOF
A TKA needs to allow for 3 DOF
Why does a replaced knee need to be stabilized?
The ACL and PCL are commonly cut / removed during a joint replacement
This means that the joint arthroplasty itself needs to provide the stability for the joint
What is the most important thing to manage for an individual post-TKA?
Pain!
With a total knee replacement, in what phases (of gait) are deficits common? What deficits are observed in these phases?
Full extension deficit can be observed in both heel-strike and midstance
An associated adduction movement of the knee produces an asymmetric load distribution in which plane?
Frontal plane
What causes an asymmetrical load distribution in the frontal plane of the knee?
Associated adduction movement
Residual varus of the knee leads to what?
Break down of the knee joint
Shear force at the knee post-TKA can lead to what?
Damage of the polyethylene articulation
Stress of bone bed
(caused from friction)
What are the major therapy goals post-TKA?
Control pain
Improve ROM of the knee
WBAT right away (to try and get normal arthrokinematics)
What are the pros and cons of using metals for a joint arthroplasty?
Pros: excellent bony in-growth properties
Cons: metals wear out
What are the pros and cons of using plastics for a joint arthroplasty?
Pros: makes a good liners (used as acetabular cups, tibial trays, etc.)
Cons: fatigue wear is an issue (esp. when in contact with harder material); may generate particles that break off with wear
What are the pros and cons of using ceramics for a joint arthroplasty?
Pros: more wear resistance (good for longevity)
Cons: tendency to fracture (esp. in large joints)
A prosthetic is typically made with a _________ of materials
A prosthetic is typically made with a combination of materials
What materials are typically used in a hip joint arthroplasty?
Metal and Plastic
Ball and socket are both made of metal and a plastic spacer is placed in-between
What are the two ways that a hip replacement implant is secured?
Press-Fitting — fit snuggly into the bone and bone forms around the implant (develop a “perfectly fitted” joint)
Cemented - cemented into place; less strong and can lead to osteolysis as well as potential air bubbles (which can cause stress concentration areas)
What was ceramics-on-ceramics designed for?
Designed to be the most wear resistant of all hip replacement implants (they are more scratch resistant and smoother)
What is a concern with ceramics-on-ceramic hip replacement implants?
Material failure (breakage) in-vivo
What are the pros of using a 3D printer for joint replacement implants?
Less error
The joint replacement implant is more custom (don’t need to worry about sizing)
T/F: Soft tissue replacements have been just as successful as other joint replacements / arthroplasty
False
However, replacements for intra-articular structures have become more common
What material(s) have typically been used for soft tissue replacement?
Elastomeric materials (e.g., silicone and polyurethane)
What typically causes failure of a soft tissue replacement? What do these failure methods lead to?
Thermal fatigue wear
Mechanical/Environmental Cracking
Both of these failure modes can result in debris → eliciting an inflammatory response / toxin poisoning → rejection
What does bone cement consist of?
90% polymethyl-methacrylate (PMM)
10% crystals (e.g., barium sulfate or zirconium oxide)
What are the pros and cons of bone cement?
Pros: allows for forgiveness in fitting (doesn’t have to fit “exactly” tight) and makes replacement smoother
Cons: can have impurities (air bubbles), brittle/weaker and prone to fatigue failure, and can have debris that break off (and cause body to reject prosthetic or scratch/damage fine joint surface)
Bone cement may support the colonization of ________ which can cause development of __________.
Bone cement may support the colonization of bacteria which can cause the development of post-operative infections (which can cause rejection of joint)
What is the biggest concern with joint replacement?
Wear in terms of longevity and debris formation
T/F: Biocompatibility of joint replacements is still a big concern
False!
Use to be a concern, but largely gone now (rarely have rejection due to material)
Debris from joint replacements can cause what?
Can create physiological cell responses that will cascade into reactions leading to osteolysis
What is the relationship between the size of debris/particle and osteolysis?
Direct Relationship w ith size of particles
Particles with a certain size have greater effects than particles that are out of the range
What must companies show now regarding joint replacements? Why?
Companies must prove that their joint replacements are safe through…
Wear particle size
Shape distribution
Concentration development
This is to try and prevent debris (which lead to osteolysis)
What is osteolysis?
Often created by debris which cause a cascade of cell responses that stimulate osteoclast function while inhibiting osteoblast function (leading to a loosening of the implant)
What mechanical factors contribute to the development of osteolysis? Why/How?
Load mismatch or stress shielding (the JRF and the load that a prosthetic can withstand do not match)
Micromotion (instability)
Both can lead to release of cytokines resulting in lack of osteointegration of implant
What are the pathomechanics of osteolysis?
Debris migrates to surrounding soft tissue
Causes inflammatory response
Macrophages try and rid the debris (but material not biodegradable)
Excessive amount of cytokine release (leads to vascularization in tissue)
Chronic inflammation (due to vascularization)
Osteolysis and Implant Failure
T/F: The process in which osteolysis occurs can lead to the development of cancer
True!
Debris may promote a significant foreign body reaction which can result in the development of cancer in the area
What factors affect longevity of a joint replacement?
Age
Patient activity level
Patient weight
Gender
How does age affect longevity of a joint replacement?
Younger patients have less longevity of an implant
Most likely due to being more active, etc.
Longevity increases every year after 60 y/o
How does patient activity affect longevity of a joint replacement?
The more active a patient is the less longevity the joint replacement has
More active means more JRF and torque on the implant
How does patient weight affect longevity of a joint replacement?
The heavier a patient is the less longevity the joint replacement has
Due to more force, etc. being placed on the implant
Do men or women have less problems with joint replacements? Why is this most likely the case?
Women
Thought that women probably take better care of their joint replacements
Why has the number of revisions after a joint replacement increased?
Patients have been getting replacements at a younger age
Typically when we are younger → more active, meaning we are wearing out the joint more
Additionally, implants are not designed to last long enough for younger patients (most implants last 20-25 years)
What are reasons for revision of a joint replacement?
Loosening or dislocation of the implant
Fracture of the bone or prosthesis
Other mechanical complication (such as implant wear)
T/F: Joint replacement revisions are just as successful as the initial surgery
False!
Joint replacement revisions are more difficult and not as successful
Longevity of an implant _______ with each revision
Longevity of an implant decreases with each revision
How is motion affected by joint replacement revisions?
Patients tend to recover less overall motion
What are the signs and symptoms of joint replacement failure?
Increased pain
Loss of function
Loss of motion
Joint dislocation
Clunking noise (with joint motion)