Chronic Obstructive Pulmonary Diseases (COPD) and Asthma & OSA
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
Overview of Obstructive Pulmonary Diseases
These conditions block airflow, especially when breathing out.
Asthma → reversible airway narrowing
COPD (Chronic Bronchitis + Emphysema) → not fully reversible, gets worse over time
OSA → airway collapses during sleep, not a lung disease but affects breathing
Pulmonary Diagnostic Tests
Pulse oximetry – oxygen saturation
Capnography – CO₂ levels
Pulmonary function tests (PFTs) – airflow & lung capacity
Bronchoscopy – look inside airways
Thoracentesis – remove pleural fluid
Exercise testing – how breathing affects ADLs
Pulmonary System Assessment
Inspection – breathing effort, chest shape
Palpation – chest expansion
Percussion – air vs fluid
Auscultation – wheezes, crackles
What is Obstructive Sleep Apnea (OSA)?
OSA is when breathing repeatedly stops during sleep:
Stops ≥10 seconds
Happens ≥5 times per hour
Why it happens
When sleeping:
Muscles relax
Tongue & soft tissues fall back
Upper airway gets blocked
Risk factors
Obesity
Short neck
Large uvula
Smoking
Enlarged tonsils/adenoids
Treatment (non-surgical)
CPAP (continuous positive airway pressure)
Keeps airway open during sleep
Positioning devices
Weight loss
Smoking cessation
What is asthma?
Chronic inflammatory disease
Airways tighten suddenly
Reversible
Affects airways only, not alveoli
What’s happening in the lungs
Swelling of airway walls
Bronchospasm
Thick mucus
Narrow airways (bronchoconstriction)→ ↓ airflow
Asthma triggers
Smoke (cigarette, wood)
Pollution
Animals (fur/dander)
Mold, pollen
NSAIDs / aspirin (in some patients)
MSG
Exercise
Cold air
Prevalence of Asthma
More common in adult women than men
Slightly more prevalent among African-Americans than Caucasians
Number of people with asthma continues to grow
Signs & symptoms
Wheezing
Shortness of breath
Chest tightness
Prolonged expiration
Accessory muscle use
Severe attacks → hypoxia, hypoxemia - ↓ LOC, tachycardia
Intervention
Management
Tailored to meet the patients triggers
Use peak flow meter and adjust accordingly
Green – asthma control
Yellow – use prescribed reliever drug* rescue inhaler
Red Zone – need reliever drugs & seek medical help!
*continuously in yellow might need a better plan.
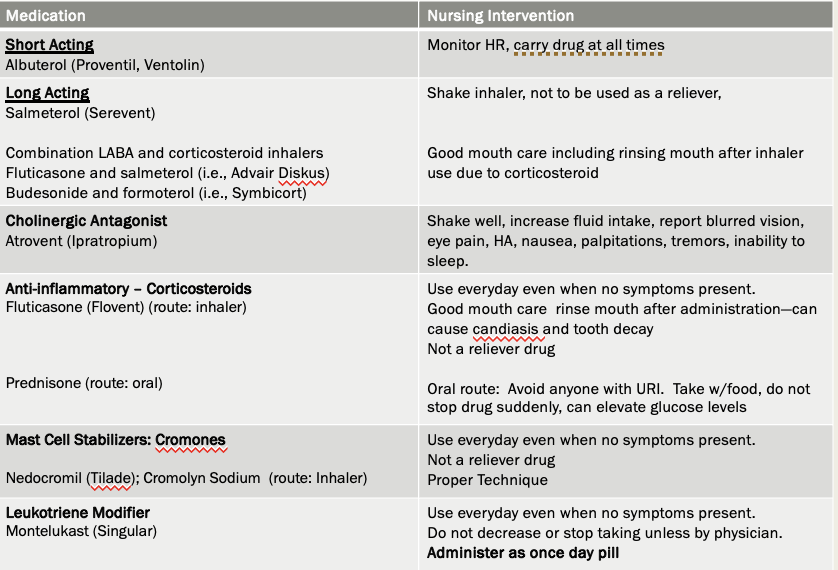
Asthma medications
Rescue meds
Short-acting beta₂ agonists (SABA)
Example: albuterol
Used during attacks
Controller meds
Inhaled corticosteroids (avoid systematic s/s from oral)
LABAs (long-acting beta₂ agonists)
Leukotriene modifiers (montelukast)
Monoclonal antibodies (IgE)
⚠ Always give SABA before LABA
Other treatment
Exercise and activity to promote ventilation and perfusion
Oxygen therapy via mask or nasal cannula (acute asthma attack)
Overview of Beta2-Agonists Bronchodilators
Suffix: TEROL
Action: Dilates bronchi
SE: (from activating sympathetic nervous system)
–Tachycardia
–Palpations
–Irregular heart reate
–Tremors
–Anxiety/insomnia
–Thrush ( rinse mouth after inhaler use)
–Avoid caffeine (increases Ses)
SABA (Short Acting Beta Agonists)
–ex albuterol
–Rescue Inhaler: Quick relieve of acute symptoms
–Usually administered as 2 puffs prn
SABA (Short Acting Beta Agonists)
–ex albuterol
–Rescue Inhaler: Quick relieve of acute symptoms
–Usually administered as 2 puffs prn
REMEMBER ALWAYS ADMINISTER SHORT ACTING THEN LONG ACTING!
Overview of Muscarinic Antagonist or anticholinergic bronchodilator
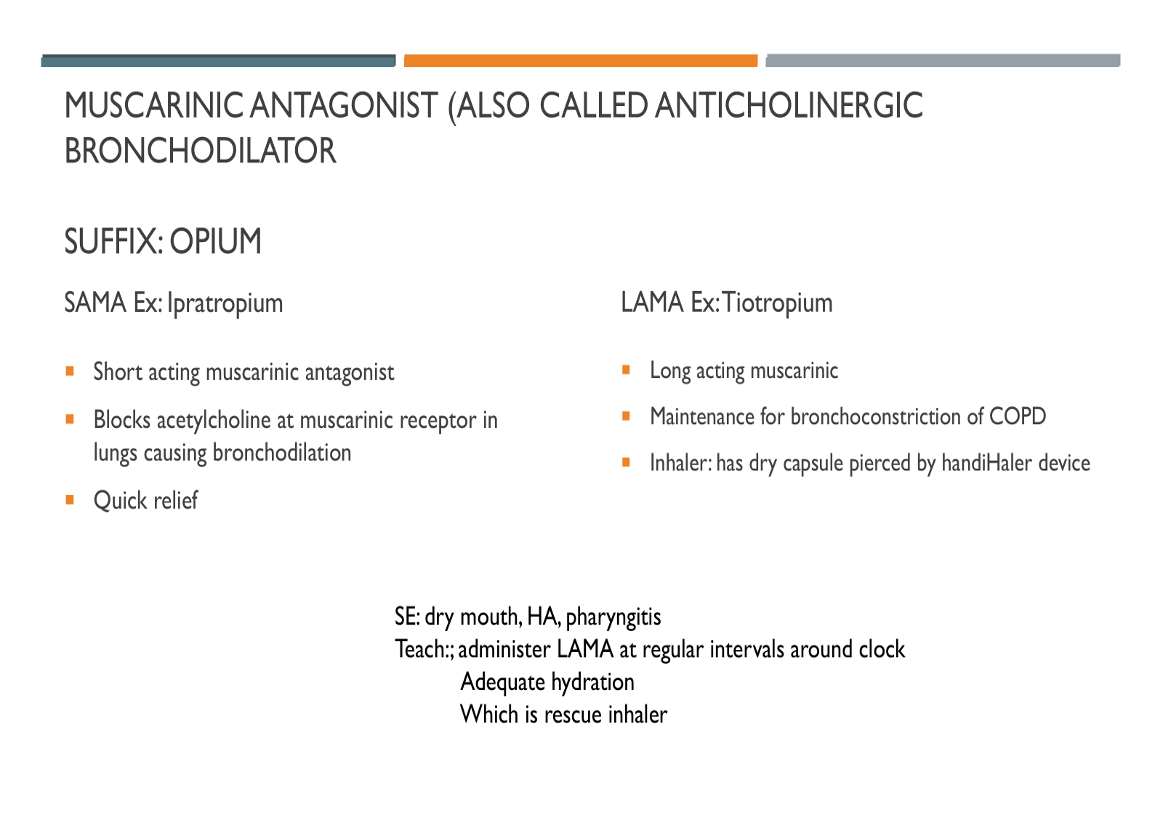
What is Leukotriene Modifiers: Montelukast. How to take it?
Used as additional treatment in addition to other medications such as SABA and LABAs or corticosteroids DOES NOT replace other therapies—important pt teaching point
Administered as a once a day pill
Must take daily as it’s effectiveness requires regular use
What is Theophylline; toxicity; s/e
methylxanthine
Used to help open the airways in asthma and COPD
Works by relaxing bronchial smooth muscle → easier breathing
Blood levels 10-15
Toxicity: >20
SE: HA, GI distress, N/V/D
Signs of toxicity: tachycardia, palpitations, seizures
Asthma Prevention and Treatment key takeaways
What is Status asthmaticus? It can cause? Treated with?
Severe, life-threatening, acute episode of airway obstruction
Intensifies once it begins, often does not respond to common therapy
Can cause:
Pneumothorax
Respiratory arrest
Treated with:
IV steroids
Bronchodilators (potent)
Oxygen
Epinephrine
Management & Teaching for Intermittent and persistent asthma
Avoid triggers of acute attacks
Pre-medicate before exercising
Short-term (rescue or reliever) medication
Long-term or controller medication
Assessment during acute exacerbation
Respiratory and heart rate
Use of accessory muscles
Percussion and auscultation of lungs
Peak Expiratory Flow Rate (PEFR )to monitor airflow obstructin/airway function
–Maximum rate a person can exhale after full inhalation
ABGs
Pulse oximetry
Management during Acute asthma exacerbations
O2 via nasal cannula or mask to achieve a PaO2 of at least 60 mm Hg or O2saturation greater than 90%
–Continuous oxygen monitoring with pulse oximetry
Bronchodilator treatment
–Short-acting β2-adrenergic agonists (SABAs)
What happen to the body during Severe and life-threatening exacerbations
“Silent chest” - it means air is NOT moving
Severely diminished breath sounds
Absence of wheeze after patient has been wheezing
Patient is obviously struggling
Life-threatening situation
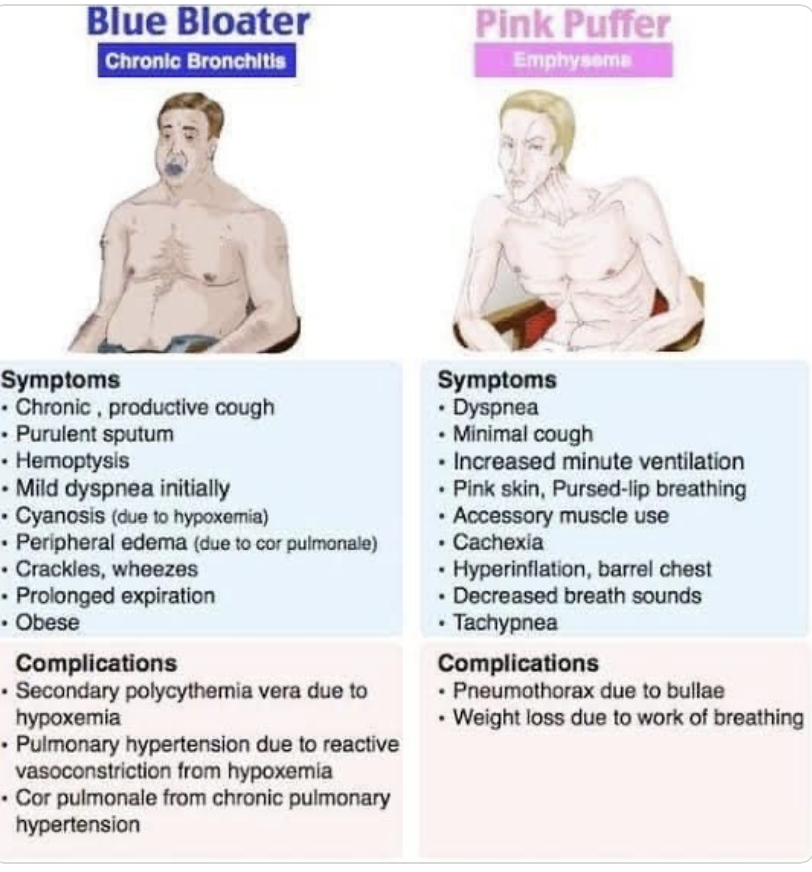
2 main disease of COPD
Chronic Bronchitis
Emphysema
Most patients have features of both.
Main Cause of COPD
Chronic exposure to irritants
Cigarette smoking is the #1 cause
Also includes:
Secondhand smoke
Occupational dust/chemicals
Air pollution
What is chronic bronchitis?
inflammation of bronchi and bronchioles
Affects airways only (NOT alveoli)
Caused by long-term irritation
Airways become:
Swollen
Narrowed
Filled with thick mucus
Sign and symptoms of Bronchitis
What is acute bronchitis?
Acute infection or inflammation of the airways or bronchi
Commonly follows a viral illness
Symptoms similar to those of pneumonia but does not demonstrate pulmonary consolidation and chest infiltrates
–Cough
–Productive/non
–Sore throat
–Post nasal drip
–Fatigue
What is emphysema?
Destruction of alveoli
Loss of lung elasticity
Alveoli stretch and form bullae (air pockets)
Damage is permanent
Air gets trapped during exhalation
Lungs become hyperinflated
Sign and symptoms of emphysema
What Happens in COPD Overall
Alveoli damage
V/Q mismatch- V (ventilation) = air getting to the alveoli Q (perfusion) = blood flowing past the alveoli
Increased oxygen demand
Pulmonary hypertension
Leads to Cor Pulmonale (right-sided heart failure)
Signs of right-sided heart failure:
Peripheral edema
Jugular vein distention
Weight gain
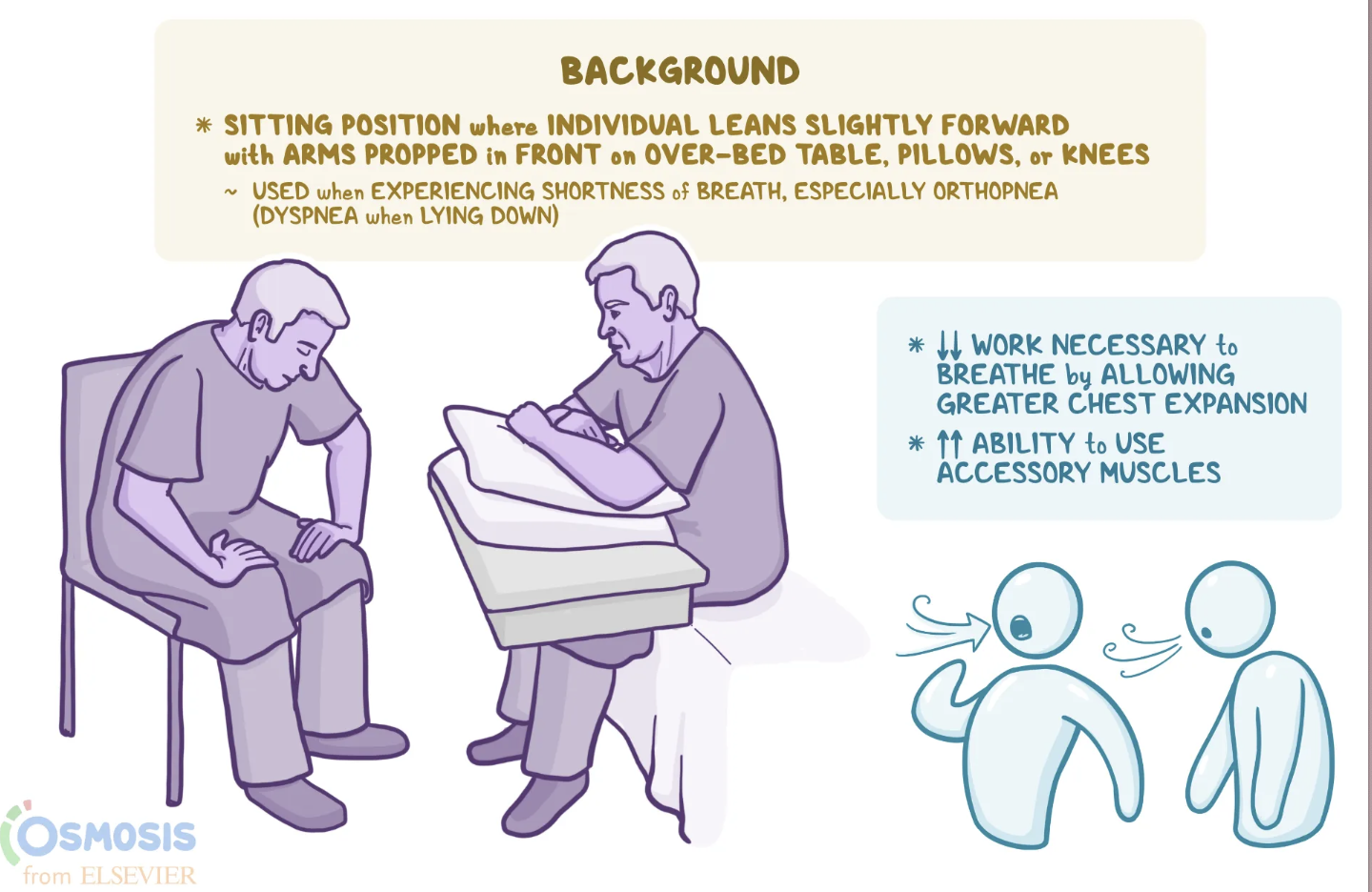
Breathing Positions & Techniques (VERY TESTED)
Tripod Position
Leaning forward
Uses accessory muscles
Increases lung expansion
Decreases work of breathing
Pursed-Lip Breathing
Inhale through nose → Exhale slowly through puckered lips
Helps by:
Keeping airways open longer
Releasing trapped air
Slowing breathing
Improving gas exchange
Often combined with tripod position
Diagnostic Tests for COPD
Pulse oximetry – oxygen saturation
ABGs – oxygen, CO₂, acid-base status
Pulmonary Function Tests (PFTs) – confirms COPD
Chest X-ray
CBC
Chronic hypoxia → polycythemia (can occur)
Sputum cultures (look for any infection)
Serum electrolytes
What is Pulmonary Function Test?
A non-invasive breathing test measuring lung capacity, airflow, and gas exchange to diagnose lung diseases such as COPD or Asthma.
Drug Therapy
Bronchodilators
Beta-agonists
Cholinergic antagonists
Methylxanthines (Theophylline)
👉 Open airways
Corticosteroids
Reduce inflammation
Inhaled or systemic
Mucolytics
Thin thick secretions
Make coughing easier
NSAIDs
Other Therapies
Exercise Conditioning
Suctioning
Hydration
Vibratory Positive Pressure Devices (PEEP)
–Holds airway open – breath into it.
Surgical Management
Lung reduction surgery removes the most damaged parts of the lungs (usually from emphysema).
Median Sternotomy
Surgeon makes an incision down the middle of the chest
Chest is opened to access both lungs
More invasive
Longer recovery time
VATS (Video-Assisted Thoracotomy Surgery)
Minimally invasive
Small incisions
Camera and instruments inserted into chest
Less pain
Shorter recovery
Fewer complications
VATS is preferred when possible
This helps the healthier lung tissue work better and makes breathing easier.
⚠ It does not cure COPD, but it can:
Improve breathing
Improve exercise tolerance
Improve quality of life in selected patients
Postoperative Care & Monitoring (After Surgery)
Key postoperative priorities:
Airway & breathing
Monitor oxygen levels
Watch for respiratory distress
Chest tube management
Prevent pneumothorax
Monitor drainage and air leaks
Pain control
Pain can limit deep breathing → increases pneumonia risk
Early mobilization
Prevents atelectasis and blood clots
Pulmonary hygiene
Incentive spirometry
Deep breathing and coughing exercises
Possible Complications (Why Close Monitoring Is Needed)
COPD patients are high risk for complications such as:
Pneumothorax (collapsed lung)
Respiratory failure
Infection or pneumonia
Prolonged air leaks
Cardiac complications
Community-Based Care
Home care management - Helping the patient manage COPD in their daily life at home.
–Long-term use of oxygen
–Pulmonary rehabilitation program
Teaching for self-management
–Drug therapy (how to take the medicine in times of exacerbation)
–Manifestations of infection (COPD patients are high risk for respiratory infections.)
–Breathing techniques (pursed lip)
–Relaxation therapy (COPD often causes anxiety, which makes breathing worse.)