18. adenoviridae, papillomaviridae, polyomaviridae
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
what type of genome do papillomaviridae, polyomaviridae, and adenoviridae have? where do they replicate and how can they affect the host cell?
DNA
replicate in nucleus → mechanisms to induce S phase of cell
can transform cells (“DNA tumor virus”)
are papillomaviruses, polyomaviruses, and adenoviruses naked or enveloped?
naked → very stable in environment
what are the most medically important species papillomaviruses infect? are they zoonotic?
bovine > equine > canine
mostly species specific → not zoonotic
how are papillomaviruses transmitted?
direct or indirect contact
via wounds or abrasions
sexual transmission
spread via fomites
can shed without lesions
what type of diseases/clinical presentations do papillomaviruses cause?
most cause self-limiting, benign warts
some can cause tumors (inhibit tumor suppressors in cells)
subclinical infections common
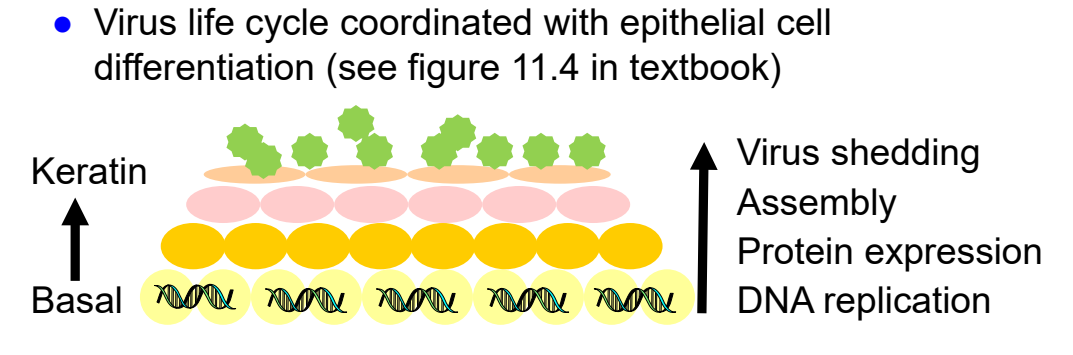
papillomaviridae pathogenesis
wound/abrasion needed to access basal layer
replication in stratified squamous epithelial cells
skin (keratinocytes)
mucous membranes (stratified squamous epithelium)
induces cell division (hyperplasia) → papilloma
virus life cycle coordinated with epithelial cell differentiation
DNA replication in basal layer → virus shedding in keratinized layer
what are the clinical signs of bovine papillomavirus? what is the distribution of the lesions?
classic warts on skin
more common on head, neck, and shoulders
also on teats, penis, body
**NOT pruritic or painful
usually benign, regress spontaneously
can interfere with function, milking, etc.
large masses possible
what are predisposing factors to bovine papillomavirus?
more common in calves and yearlings
more common in winter & housed animals
can bovine papillomavirus be found on/in normal skin?
yes → persistent virus common with detection of DNA in normal skin
trauma → virus replication & papilloma
what is the difference between papillomas and fibropapillomas?
papillomas → epithelium
fibropapillomas → epithelium + underlying dermal tissue
what types of tumors can bovine papillomaviruses cause? what is required for tumorigenesis?
carcinoma of the GI tract
hematuria and/or carcinoma of the urinary bladder
both GI and bladder disease require co-carcinogen
BPV infection + bracken fern ingestion
how is bovine papillomavirus diagnosed?
clinical appearance usually sufficient
histopathology of lesion
IHC or EM
PCR → careful because BPV can be found in normal skin
no virus isolation because cell culture system difficult
bovine papillomavirus treatment/control
treatment
regress on their own in 1-6 months
leave alone unless interfering with function
control
prevent animal-to-animal and fomite spread
what two lesions can equine papillomavirus cause?
papillomas (warts)
aural plaques
what is the typical appearance of equine cutaneous papillomas? what is their distribution?
appearance
benign warts
multiple small, raised papillomas is typical (miliary pattern)
locations
most common: lips & noses
less common: eyelids, inner pinnae of ears, genitalia & legs
**not pruritic or painful

in what age group are equine cutaneous papillomas most common?
most common in young animals (1-3 years old)
what is the characteristic appearance of equine aural plaques?
flat cutaneous lesion inside pinna
can be very large
benign
not pruritic or painful

equine papillomavirus treatment/control
treatment
warts regress on their own in 1-9 months → leave them alone!!
aural plaques often don’t regress
only perform surgery if interfering with function
control
prevent animal-to-animal and fomite spread
what are sarcoids? what is their biological behavior?
connective tissue tumors of horses and other equids
can be locally aggressive, but do not metastasize and are benign
can be persistent & recurrent
what are common locations for sarcoids?
head > neck/trunk/shoulders
less common on ventral abdomen and legs
equine sarcoids are strongly associated with infection of what virus?
BPV (bovine papillomavirus)
sarcoid treatment
avoid treatment unless:
interfering with normal function
growing, ulcerating, chronic damage
what types of papillomas can canine papillomavirus cause?
oral, ocular, cutaneous
which type of canine papilloma is most common?
oral papillomas
where are canine oral papillomas typically located? what age group do they most commonly affect?
location:
lips >>> inside cheeks, palate, tongue, oropharynx (esophagus)
affect puppies or young dogs
usually < 6 months; up to ~2 years
where are ocular papillomas located? (canine papillomavirus)
cornea, conjunctiva
what are predisposing factors to cutaneous papillomas? (canine papillomavirus)
older, often immunocompromised dogs
rarely occurs with oral papillomas
how is canine papillomavirus diagnosed?
clinical appearance, especially for oral papillomas in young dogs
histopathology ± IHC
PCR (interpret carefully because normal skin can be +)
canine papillomavirus treatment
most regress on their own in 1-2 months → leave them alone
if they don’t regress and are large, surgical excision BUT surgery is associated with recurrence
what species of bird is most severely affected by avian polyomavirus?
budgerigars (parakeets)
clinical signs of avian polyomavirus in budgerigars (parakeets)
rapidly fatal “Budgerigar fledgling disease”
<10-15 days of age
SQ hemorrhages, CNS signs
feather abnormalities (abnormal molt)
>15 days of age
how does avian polyomavirus present in other birds?
other psittacines & rarely other birds
usually subclinical
disease can occur:
peracute death in neonates
hemorrhagic, edema, pneumonia, or CNS disease
what are other differentials for abnormal feathers in parrots?
sporadic abnormal molt (aka French molt)
excessive molting ± broken tail or wing feathers
psittacine beak & feather disease virus (circovirus)
how is avian polyomavirus transmitted?
feather dust
feces
respiratory secretions
in ovo (budgies) → transmission to egg
avian polyomavirus control
killed virus vaccine
in general, how are adenoviruses transmitted?
direct contact or aerosol (shed in respiratory & other secretions)
what is another name for canine adenovirus-type 1?
infectious canine hepatitis
how is canine adenovirus-type 1 transmitted?
virus is shed in urine, feces, & saliva
transmission via direct contact with infectious materials or droplets (sniffing, eating, etc.)
enters nasopharynx, oropharynx, conjunctiva, etc.
canine adenovirus-type 1 pathogenesis
oronasal infection (tonsillar crypts)
draining lymph node infection
viremia
spread to liver & kidneys
possible spread to CNS
what types of diseases/clinical signs are associated with canine adenovirus type-1?
acute disease → systemic infection
fever, abdominal pain, jaundice, vomiting, petechial hemorrhages and bloody diarrhea, anemia
hemorrhage → lack of clotting factors, endothelial cell damage, and DIC
severe hemorrhage = poor prognosis
CNS signs
hepatic encephalopathy in domestic dogs
(encephalitis in foxes; rarely domestic dogs)
peracute death
no clinical signs
mild or subclinical infection (persists in kidneys)
what causes “blue-eye” keratitis?
type III immune complex hypersensitivity
immune complexes deposit in vessels of ciliary body → block fluid exchange → bilateral corneal edema
what is the difference between CAV-1 and CAV-2 modified live vaccine?
CAV-1 MLV → “blue-eye” keratitis is common side-effect (same as natural infection)
CAV-2 MLV → no blue-eye and simultaneous protection against both CAV-1 and CAV-2 (cross protection)
what type of disease does canine adenovirus-type 2 cause?
local respiratory infection (not systemic)
infectious laryngotracheitis (“kennel cough”)
canine adenovirus-type 2 clinical signs
dry, harsh, hacking cough
± fever, nasal discharge