DSA21 - Chronic Diarrheas and Inflammatory Bowel Disease
1/3
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
4 Terms
Inflammatory Bowel Disease (IBD)
Define Condition:
Crohn Disease (Ileum) + Ulcerative colitis (Rectum); Dx of Exclusion
-Hx:
> Bimodal Age Distribution
>> Age 15-30 y/o
>> Age 50-80 y/o
> More in White, Jewish Populations
>> Female = Crohn (hormones)
>> Male = UC
> Vit D Deficiency
-Sx/PE:
> Episodes/Flares
> Arthritis (peripheral joints, Ankylosing Spondylitis, Sacroiliitis, Migratory Polyarthritis)
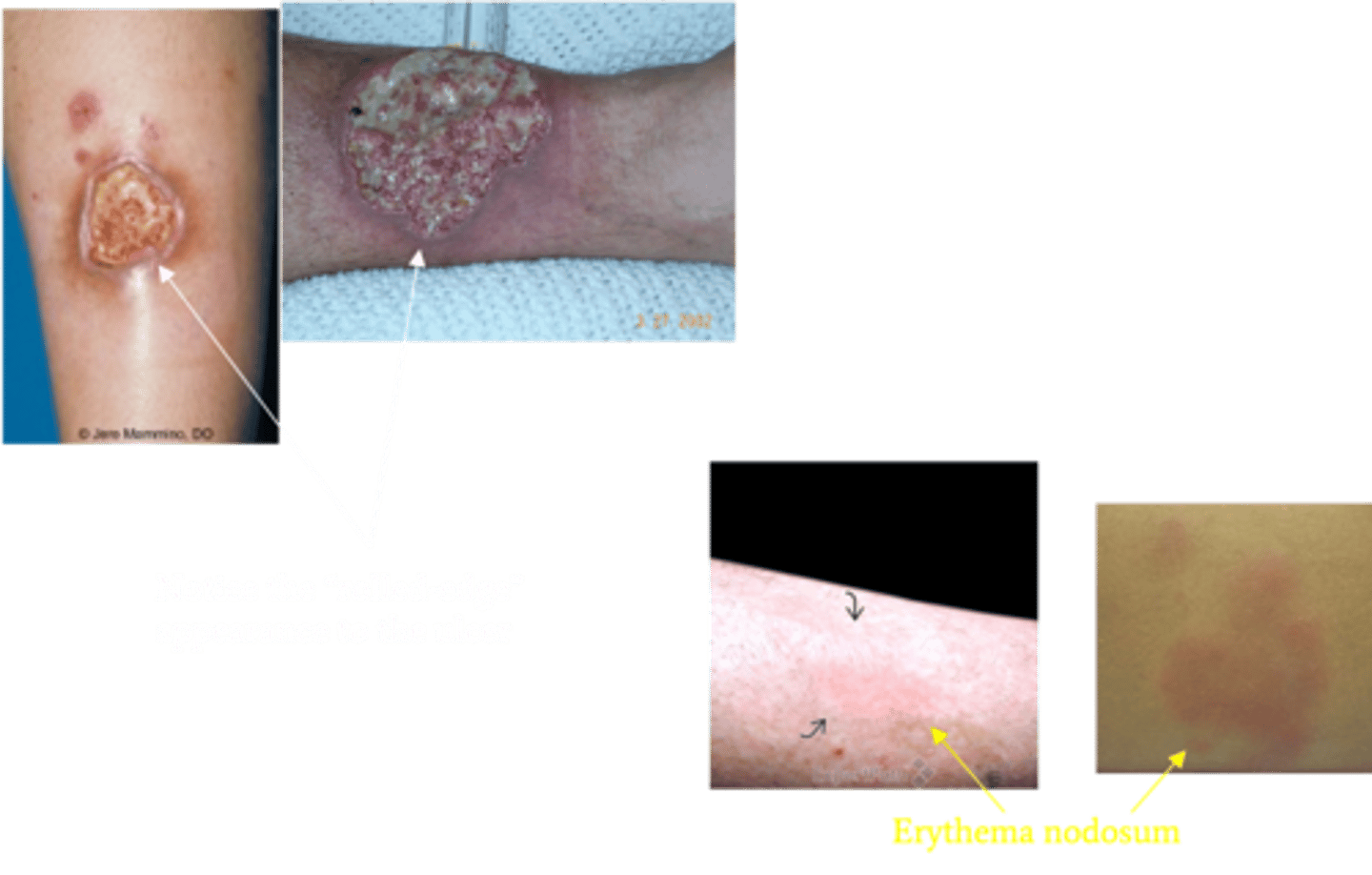
> Erythema nodosum (painful)
> Pyoderma gangrenosum
>> MC in 50s to 60s
>> Deep, necrotic skin ulceration
>> Distinctive rolled edges and violaceous border, more common in Crohn
>> Need to treat main cause
> PSC (in UC)
> Uveitis
-Dx:
> Elevated CRP
> Elevated ESR
Crohn Disease (if only Colon = Crohn colitis)
Define Condition:
Transmural inflammation involving ileum, but may involve any area of GI tract
-Hx:
> FEMALES
> Smoking
> FHx
-Path:
> Genetics = D/t NOD2 gene (protein for defending against intestinal bacteria) mutation -> ↑intestinal bacteria to penetrate past epithelium -> trigger inflammatory reactions
> Immune Defect = Defect in Th1 T-Cells --> Cytokine mediated chronic inflammation
> Cell Defect - Defects in intestinal epithelial tight junction barrier function
-Sx/PE:
> Intermittent RUQ Pain
> Watery/Non-Bloody Diarrhea
> Weight Loss
> Deficiencies:
>> Vit Deficiency fat soluble vitamins (ADEK) = Duodenum, Jejunum, Ileum
>> Folate Deficiency = Jejunum
>> Iron Deficiency = Duodenum & Upper Jejunum
>> Vit B12 & Bile Acid Deficiency = Terminal Ileum (Impaired absorption --> Fat malabsorption ==> Steatorrhea)
-Dx:
> (+) ASCA (Anti-Saccharomyces cerevisiae Abs)
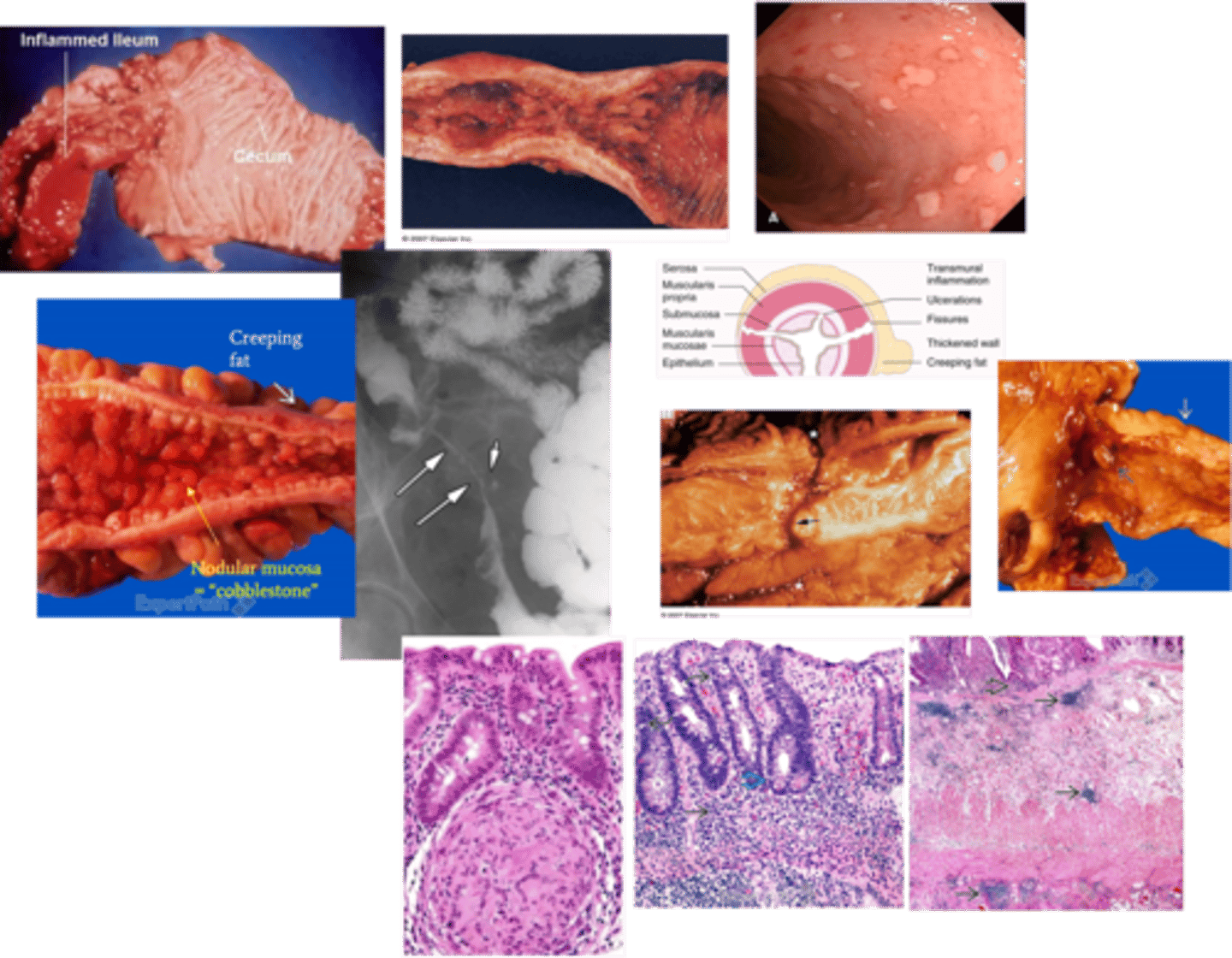
> Endoscopy:
>> "Cobblestone" Deep Ulcers: Ileal stricture w/ effaced folds, heaped-up nodular mucosa
>> Fat Wrapping/Creeping Fat: Transmural inflammation heals --> Condensed mesentery tissue pulls fat around bowel
>> Segmental "Skip" Lesions
>> Strictures: Marked thickening of bowel wall (transmural inflammation) --> Stenosis of Lumen (stricture)
>> Fistulas: Transmural inflammation --> Fissures --> Extends deep ==> Fistula tracts
>> Right-sided predominance:
>>> MC = Terminal ileum
>>> Only SI = 40%
>>> SI and Colon = 30%
>>> Only Colon = 30%
>> Rectum-sparing (1/3 of cases) - can have oral involvement (aphthous ulcers) and anal involvement (fistulae)
> Imaging: "String Sign"
>> D/t severe narrowing from edema + spasm + fibrosis
>> Frequently a/w Proximal Dilation
> Biopsy: Non-caseating granulomas + Crypt Abscesses
-Prog:
> Colon Cancer (need colonoscopy & Bx every 2-3 yrs after 8 yr Dx)
>> PSC --> HIGH RISK of Colon Cancer
> Small Bowel ACA
> Anal Cancer
Ulcerative Colitis
Define Condition:
Inflammation limited to colon and rectum, and extends only into the mucosa and submucosa
-Hx:
> Smoking is protective
> A/w PSC
-Path:
> Immune Defect = Defect in Th2 T-Cells --> Elaborates IL-13 (key cytokine in initiating pro-inflammatory cascade)
> Categories (based on location): Rectum is almost always involved (95%)
>> Only Rectum = Proctitis
>> Rectum + Sigmoid = Proctosigmoiditis
>> Left side of LI = Left-sided
>> Entire Colon = Pancolitis
> Mucosa & Submucosa only
-Sx/PE: Episodic
> Bloody Diarrhea
> Lower Abdominal Cramping
> Fatty Stools
> Wt Loss
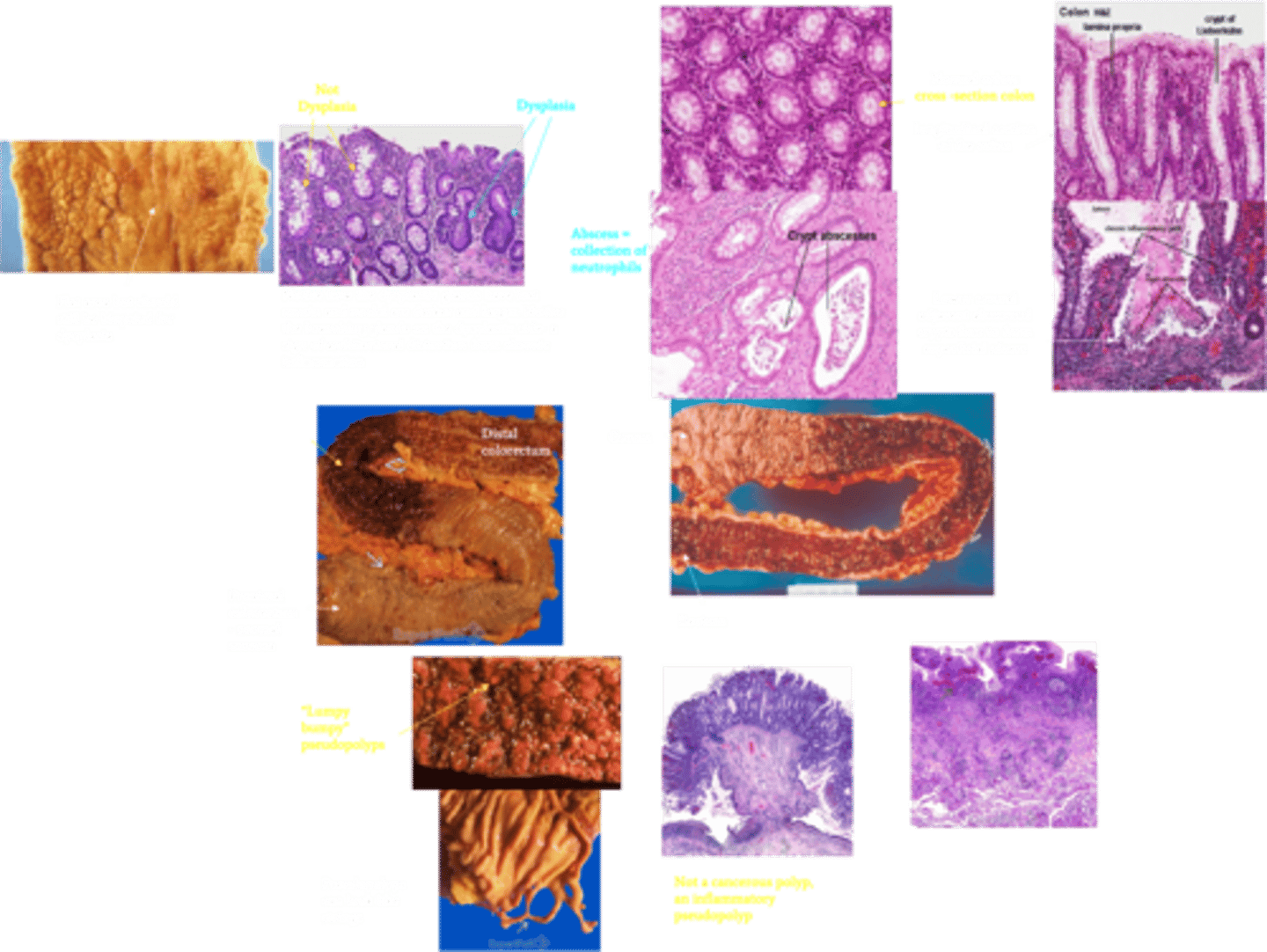
-Dx:
> Serum: (+) p-ANCA/MPO-ANCA
> Endoscopy: Backwash Ileitis
>> May involve terminal ileum d/t incompetent ileocecal valve --> reflux of inflammatory mediators from colon --> Superficial mucosal inflammation
> Imaging: "Lead-pipe appearance" d/t loss of haustra in diseased section of colon (smooth walled and cylindrical like)
> Gross:
>> Bloody & diffusely Ulcerated (no skip lesions) - extends proximally
>> Isolated islands of regenerating mucosa bulging into lumen (Lumpy, bumpy inflammatory pseudopolyps)
> Biopsy:
>> Superficial mucosal disease
>> Mild (erosions) to severe (ulcers penetrating mucosa to submucosa) +/- cryptitis and Crypt Abscesses
-Prog:
> IDA d/t blood loss
>> Bloody diarrhea w/ mucus
>> Rectal bleeding
> Risk of Colon ACA (more in pts w/ Pancolitis 10+ yrs)
>> Dysplasia of colonic mucosa (FLAT mucosa) = High risk
>> Usually infiltrative w/o obvious exophytic masses
> Toxic Megacolon
>> Cessation of colonic contractions d/t NO made by neutrophils & macrophages ==> inhibits smooth-muscle tone and disturb NM function ==> Intestinal dilation ==> Distension ==> PERFORATION
> PSC --> HIGH RISK of Colon Cancer
FPs (False positives) and FNs (False negatives) results are not uncommon
Why can't serologic markers be used to definitely rule in or rule out IBD?