Chronic Obstructive Pulmonary Diseases - Emphysema vs. Chronic Bronchitis (Smarty PANCE)
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
A patient presents with a chronic cough that is productive of phlegm occurring on most days for 3 months of the year for 2 or more consecutive years. Stocky, overweight patient. Crackles and wheezes on auscultation. Chest radiograph: peribronchial and perivascular markings. What's the diagnosis?
Chronic bronchitis

A patient presents with minimal cough, thin, with barrel-chest, decreased heart and breath sounds, pursed-lip breathing, end-expiratory wheezing, and scattered rhonchi. Chest X-ray reveals a flattened diaphragm, hyperinflation, and a small, thin appearing heart. PFTs show a decreased FEV1 / FVC ratio. What's the diagnosis?
Emphysema

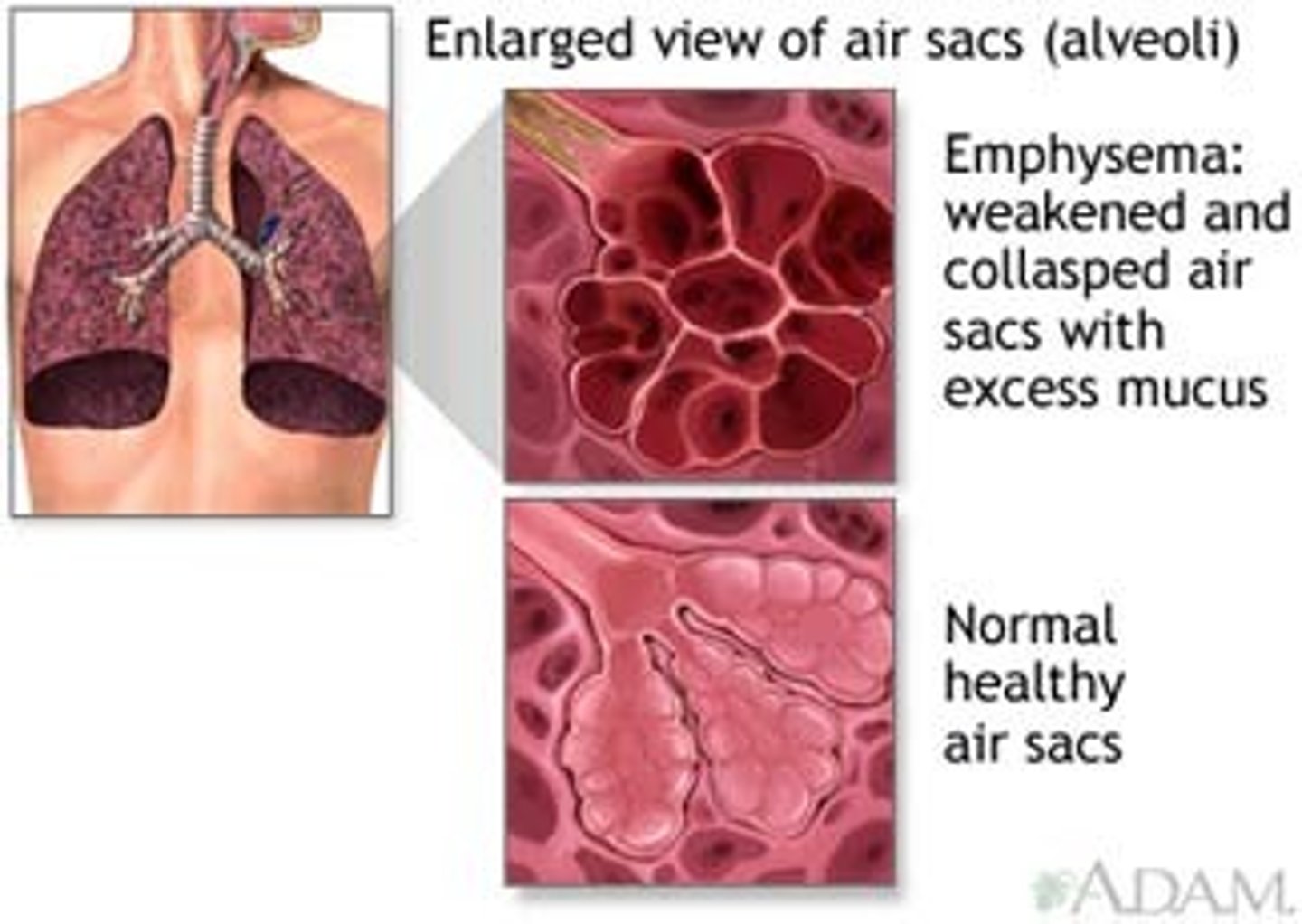
What is emphysema and how is it different from chronic bronchitis?
Emphysema is a form of COPD due to structural changes in the lung - air spaces are enlarged as a consequence of the destruction of alveolar septae vs chronic bronchitis which is due to clinical features - chronic sputum production every day for at least 3 months per year for 2 consecutive years
What is the name given to patients with emphysema?
Patients with emphysema, a component of chronic obstructive pulmonary disease, are sometimes referred to as "pink puffers."
Why are "pink puffers" pink and why are they puffers?
Dyspnea and shortness of breath due to decreased gas exchange cause patients to exhale slowly through pursed lips to increase pressure in airways to keep airways from collapsing. Individuals are able to oxygenate blood (pink) but they have to purse their lips to do so (puffers) = Pink Puffers!
What happens to lung compliance in emphysema?
Lung compliance increases in emphysema due to loss of elastin
What are the physical examination features of "pink puffers"?
Thin patient (weight loss from excessive work with ventilation) with predominant emphysema, complaining of severe dyspnea and often using accessory muscles of respiration, especially with exertion. Cough is rare. Edema and polycythemia are absent. Breath sounds are diminished; adventitious sounds are absent.
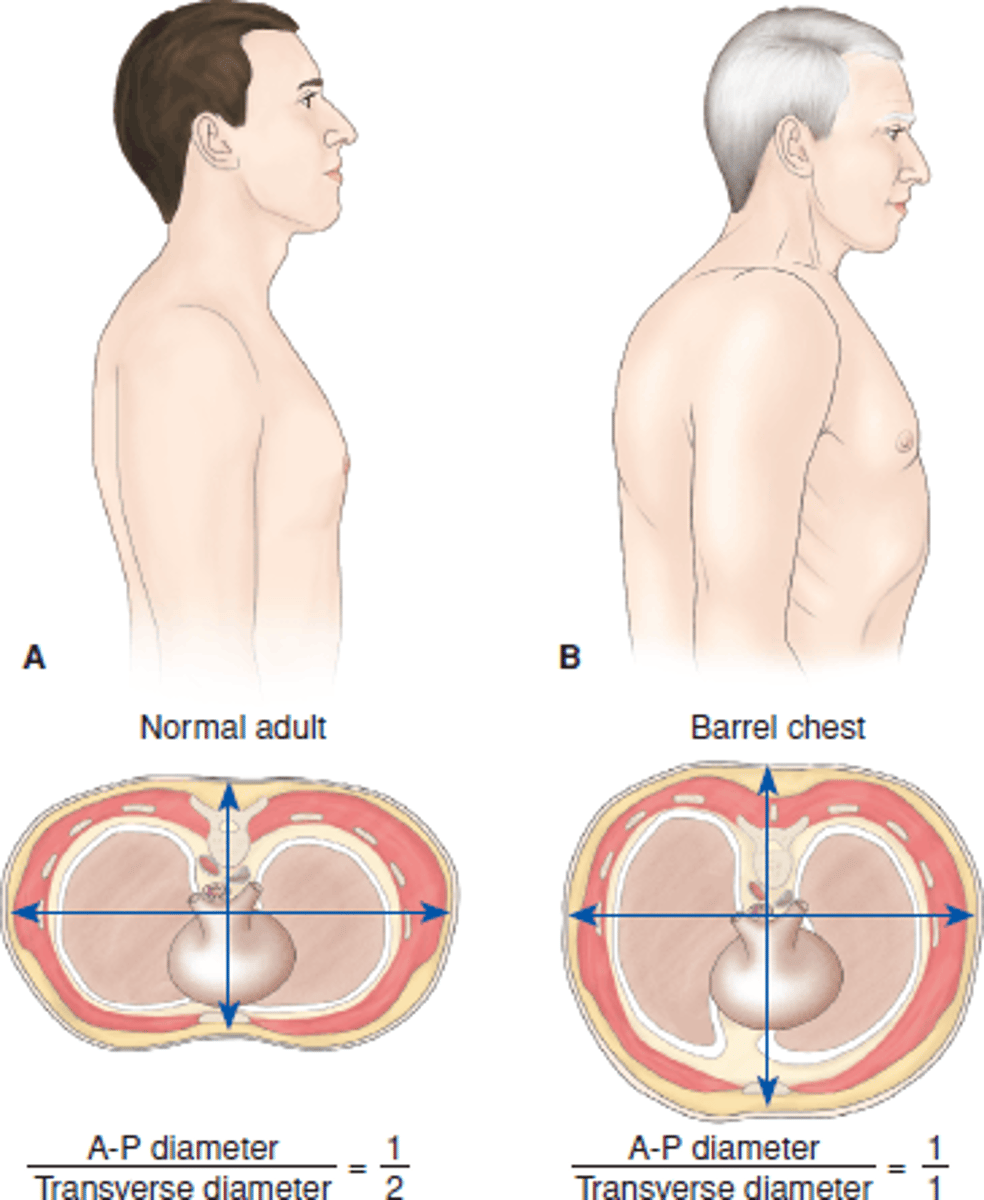
What chest shape is consistent with emphysema?
Emphysema patients often described as having a barrel shaped chest due to air trapping and hyperinflation of lungs
What are PFT findings with emphysema?
PFTs show an increased TLC (from air trapping) and decreased FEV1 / FVC ratio
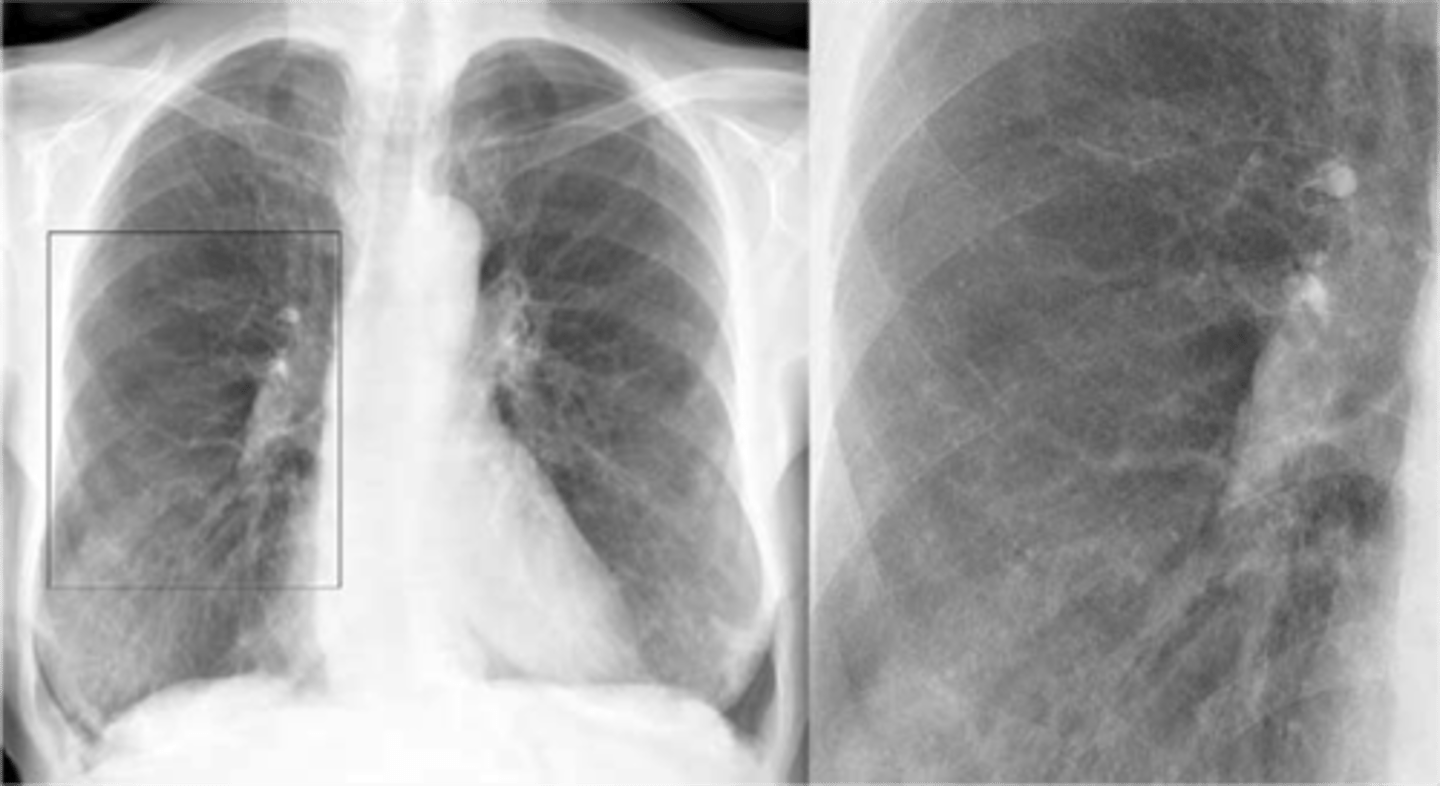
What is noted on the chest radiographs in these patients?
Hyperinflation, flattened diaphragms, and diminished vascular markings, particularly at the apices

What is the most effective therapy for most patients with emphysema?
The most effective therapy for most patients with emphysema is smoking cessation
What is the mainstay of therapy for emphysema?
Treatment depends on severity. For most patients a combination of short-acting (SABA) or long-acting (LABA) beta 2 agonist and short-acting (SAMA) or long-acting (LAMA) muscarinic agent (also known as an anticholinergic agent) +/- inhaled glucocorticoids
How are COPD exacerbations managed?
COPD exacerbations are managed with systemic glucocorticoids, antibiotics (tailored to the likelihood of specific pathogens), and antiviral therapy when influenza is suspected
In addition to smoking cessation, what preventative treatment is indicated for patients with emphysema?
Infection is a common cause of COPD exacerbation. Influenza and pneumococcal vaccination can help reduce infections and exacerbations
What is chronic bronchitis?
Chronic bronchitis is a type of chronic obstructive pulmonary disease (COPD) which includes chronic bronchitis and emphysema. that is characterized by hyperplasia of mucus-secreting glands at the level of the bronchi. Defined by clinical features of chronic productive cough lasting at least three months over a minimum of two years
How is chronic bronchitis differentiated from emphysema?
Chronic bronchitis is defined by clinical features (chronic cough) vs emphysema which is defined by structural changes (enlarged air spaces secondary to alveolar destruction)
What term is given to patients with chronic obstructive pulmonary disease with chronic bronchitis?
Chronic obstructive pulmonary disease patients with chronic bronchitis are typically termed as "blue bloaters"
Why are "blue bloaters" blue?
Color indicative of hypoxia observed in the bluish tint of skin and mucous membranes
What hematological compensation due to chronic hypoxemia can patients with chronic bronchitis have?
Due to chronic hypoxemia, patients with chronic bronchitis can have polycythemia
How does chronic bronchitis affect CO2 and O2 level in the blood?
Bronchitis, particularly the chronic form, can lead to hypercapnia (increased CO2) and hypoxemia (low O2) resultant of shunting in the lungs
What will be seen on arterial blood gasses in patients with chronic bronchitis?
Respiratory acidosis (arterial PCO2 > 45mmHg, bicarbonate > 30mEq/L)
What will be seen on CXR in patients with chronic bronchitis?
Large, horizontal heart, and increased bronchial markings particularly at the bases and thickening of the bronchial walls
How many pack-years does a patient have who smoked five cigarettes per day for ten years?
2.5 pack-years. There are 20 cigarettes in a pack so pack-years = number of years smoked × (cigarettes per day ÷ 20)
The chronic hypoxemic vasoconstriction from chronic bronchitis can lead to what complication?
The chronic hypoxemic vasoconstriction from chronic bronchitis can lead to cor pulmonale (right-sided heart failure as a result of disease of the lungs or the pulmonary blood vessels)
What additional preventative measures should be provided to all patients with COPD?
Vaccination against both influenza and pneumococcal disease
What is the diagnostic gold standard for chronic bronchitis?
Diagnosis is clinical but confirmed by biopsy (gold standard) with a Reid index above 50 percent
What is the treatment for chronic bronchitis?
Treatment depends on the severity and includes a combination of short-acting (SABA) or long-acting (LABA) beta 2 agonist and short-acting (SAMA) or long-acting (LAMA) muscarinic agent (also known as an anticholinergic agent) +/- inhaled glucocorticoids
When should long-term oxygen therapy be initiated in patients with chronic bronchitis?
Long-term oxygen therapy should be initiated all patients with COPD who have chronic hypoxemia defined as resting PaO2 < 55 mmHg or SaO2 <89%
Cough: Emphysema
•Uncommon during mild and moderate stage
•Some coughing during severe stage with infection
Cough: Chronic Bronchitis
• Common. This is a Classic sign
• More severe stage in the mornings
Sputum: Emphysema
•Uncommon
•Little mucus
Sputum: Chronic Bronchitis
•Common
•Classic sign: copious amounts, purulent
Pursed-lip breathing: Emphysema
Common
Pursed-lip breathing: Chronic Bronchitis
Uncommon
Palpation of the chest: Emphysema
•Decreased tactile fremitus
•Decreased chest expansion
•Point of maximal impulse (PMI) often shifts to the epigastric area
Palpation of the chest: Chronic Bronchitis
Normal
Percussion of the chest: Emphysema
Hyperresonance, decreased diaphragmatic excursion
Percussion of the chest: Chronic Bronchitis
Normal
Auscultation of the chest: Emphysema
•Diminished breath sounds
•Prolonged expirations
•Diminished heart sounds
Auscultation of the chest: Chronic Bronchitis
•Crackles
•Wheezes
Chest radiograph: Chronic Bronchitis
•Lungs may be clear if only large bronchi are affected
•Occasionally: Translucent (dark) lung fields, depressed or flattened diaphragm
.•Common: Right ventricle (cor pulmonale) and/or left ventricle enlargement.
•Fibrotic-appearing lung markings are often seen, commonly referred to as a dirty chest x-ray.
Chest radiograph: Emphysema
•Common: Translucent (dark) lung fields, depressed or flattened diaphragms, long and narrow heart (pulled downward by diaphragms), increased retrosternal air space (lateral radiograph).
•Occasionally: Cor pulmonale (signs of cardiomegaly), emphysematous bullae.