Pulmonology Combined- Week 3
1/201
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
202 Terms
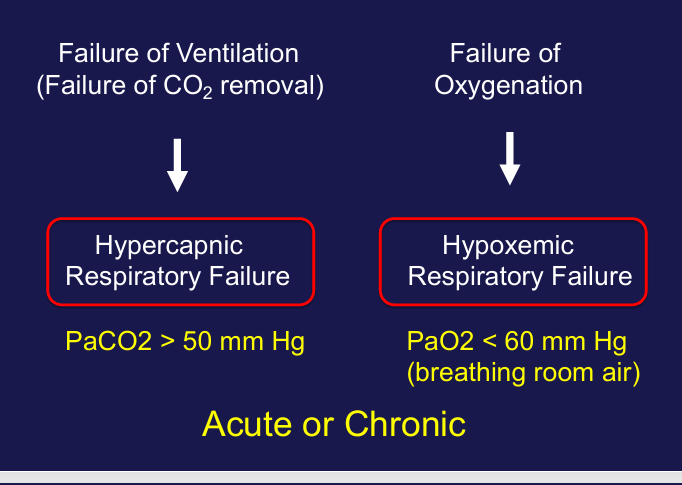
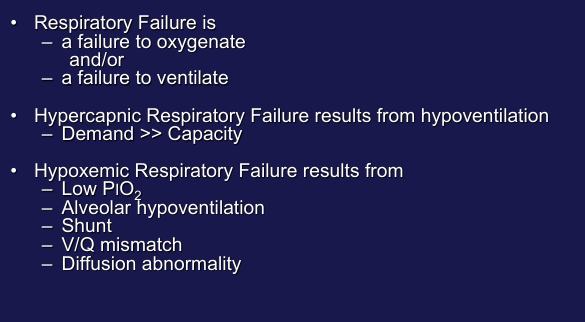
respiratory failure
-failure to oxygenate
-failure to ventilate
terms- failure of ventilation, failure of oxygenation
causes of alveolar hypoventilation
-decreased respiratory drive and/or effort: drugs, sleep, breath-holding
-neuromuscular incompetence: failed neuromuscular transmission (spinal cord, peripheral nerve), muscle weakness
-muscle fatigue due to increased load: abnormal mechanics (obesity, chest wall deformity)
-increased dead space
hypercapnic respiratory failure
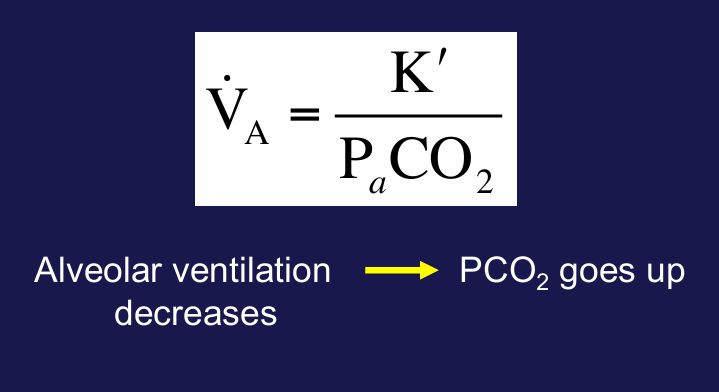
ventilatory capacity v. ventilatory demand
-ventilatory capacity: maximal spontaneous ventilation that can be maintained without fatigue
-ventilatory demand: minute ventilation required to maintain an alveolar ventilation rate that results in a physiologically acceptable PaCO2
-normally, capacity >> demand
-hypercapnic respiratory failure results from: reduction in ventilatory capacity and/or increase in ventilatory demand
-decreased ventilatory capacity: decreased respiratory drive and/or effort, neuromuscular incompetence
-increased ventilatory demand: increased dead space, increased respiratory drive (acidemia)
clinical consequences of hypercapnia
-depend upon the rate and severity and the ability to compensate
-CNS effects: anxiety, irritability, confusion, stupor, coma, death
-cardiovascular effects: hypertension, hypotension, ventricular irritability
hypercapnic respiratory failure
-CO2 is an acid
-elevations in PaCO2 represent an “acidosis”- alveolar hypoventilation can be termed a “respiratory acidosis”
-blood pH determined by a balance between PaCO2 and serum bicarbonate produced by the kidneys
-when PaCO2 rises, the kidneys generate bicarbonate to buffer the change in pH
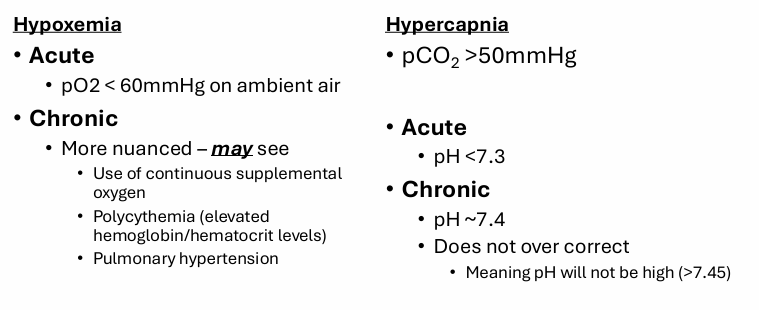
acute v. chronic hypercapnic respiratory failure
-acute: minutes to hours, renal compensation is limited, pH < 7.3
-chronic: days or longer, renal compensation is nearly complete, pH nears (but won’t exceed) 7.40
hypoxemic respiratory failure
-failure to oxygenate
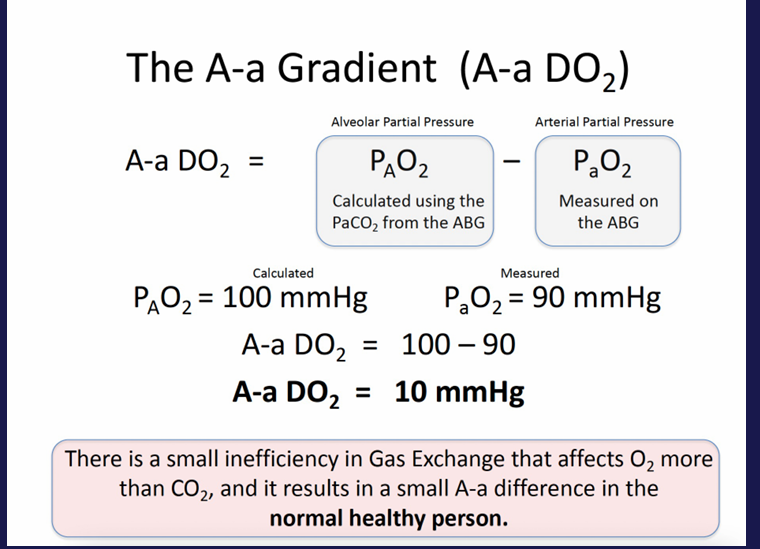
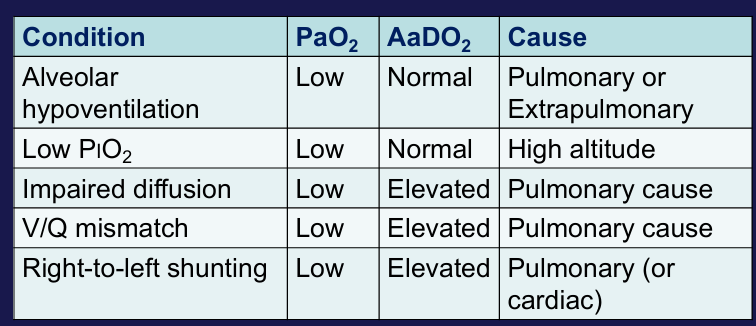
A-a gradient
causes of hypoxemia
-many clinical scenarios involve more than one mechanism for hypoxemia
clinical consequences of hypoxemia- tissue hypoxia
-CNS effects: impaired judgment/motor/cognitive function, depressed brainstem function
-cardiovascular effects: cardiac arrhythmias, myocardial depression, shock
-other organ system failures
signs and symptoms of hypoxemic respiratory failure- acute v. chronic
-acute: dyspnea, tachypnea, cyanosis, somnolence, asterixis, seizures, tachycardia
-chronic: polycythemia, pulmonary hypertension/cor pulmonale
clinical examples of hypoxemic respiratory failure
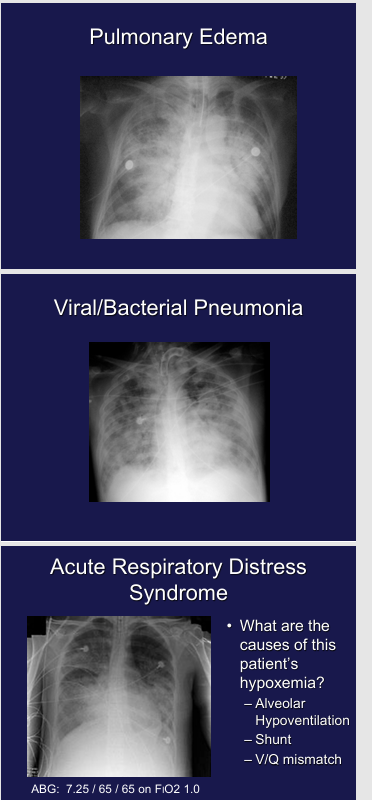
hypoxemic respiratory failure- acute or chronic?
-cannot tell from ABG
-signs of chronicity: polycythemia, pulmonary hypertension/cor pulmonale
supplemental oxygen in hypoventilation
-every mmHg increase in PiO2 should cause a corresponding increase in PAO2
-since it is easy to increase PiO2, hypoxemia due to pure hypoventilation is easy to fix
conclusions
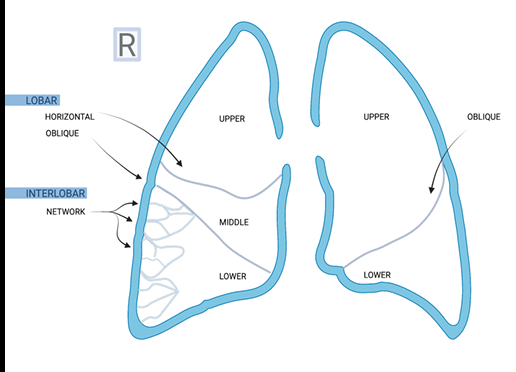
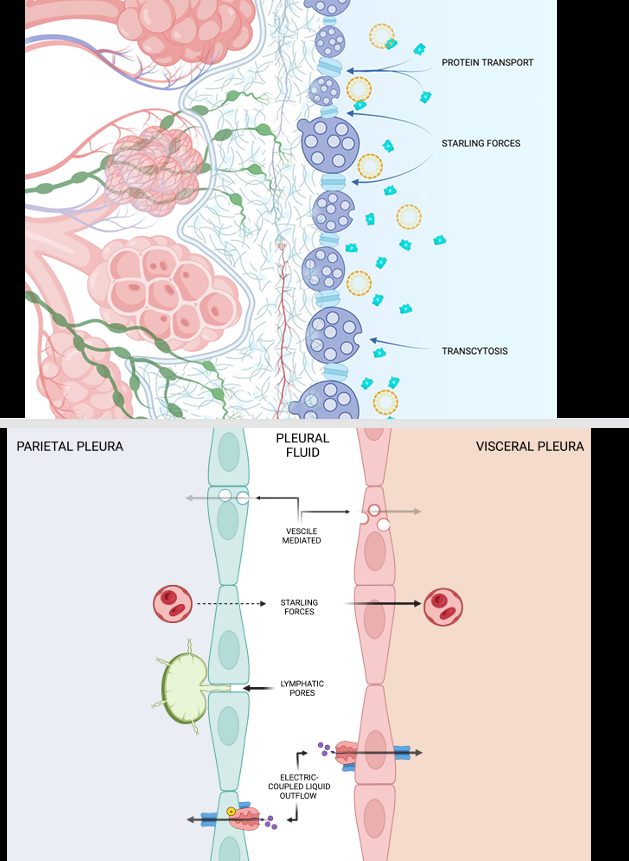
pleura physiology
-fluid enters via net pressure gradient across pleura
-fluid exits via pores in parietal pleura, gradient absorption via visceral pleura, active cellular mechanism: protein transport, fluid transport, mesothelial cells (similar permeability to microvascular endothelium)
-adaptive physiology: increased fluid loads result in increased transit through parietal pores, removal of fluid and protein by transcytosis (presumed, still needs to be directly proven in the pleura)
what is the advantage of fluid?
-less compressible as compared to air, movement of one translates immediately to the other (hydraulic)
-lubrication to diminish shearing forces on movement
mechanical coupling
-at rest, recoil of chest wall opposed by recoil of lung
-natural elastic recoil of the lung however does not result in collapse of the lung due to 3 forces acting in the thoracic cavity: deformation pressures of the chest, recoil pressures of the lung, resorptive pressures of the fluid
-on average, deformation of chest in balance with recoil of lung
-regulating forces of the pleura (oncotic and hydrostatic pressures) must be more than that of the anatomic forces (chest dormation and lung recoil)
-imbalances in pleural fluid result in a decoupling of chest and lung such that the chest wall would bow out and the lung would collapse
-essential to this coupling is keeping the space gas and nearly fluid free
pleural anatomy
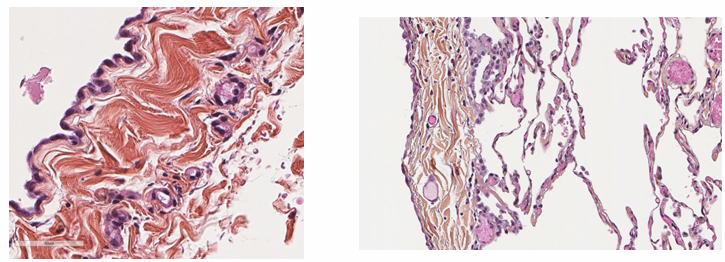
-visceral pleura
transport across pleura
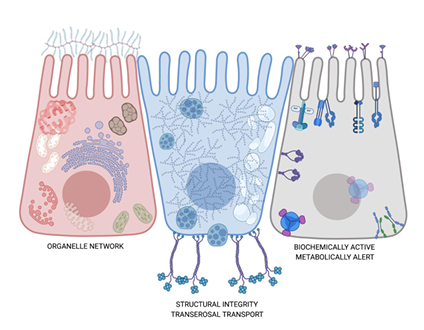
mesothelial cell
pathophysiology
-imbalance in pleural pressure
-poor lymphatic drainage
-increased permeability
-poor cellular function
-vascular obliteration
-fibrotic deposition
-changes surface topography of lung pressure
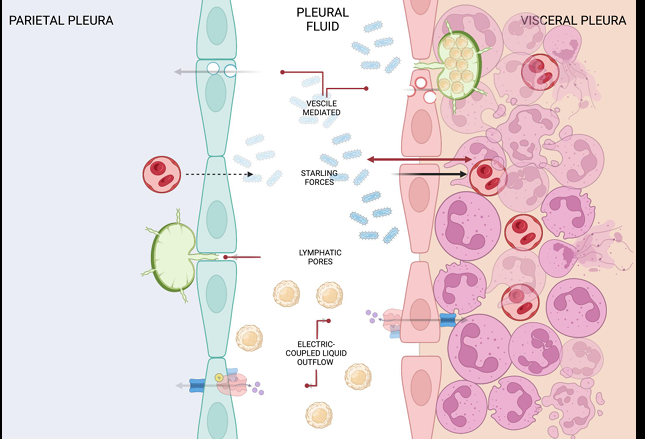
-diseased pleura
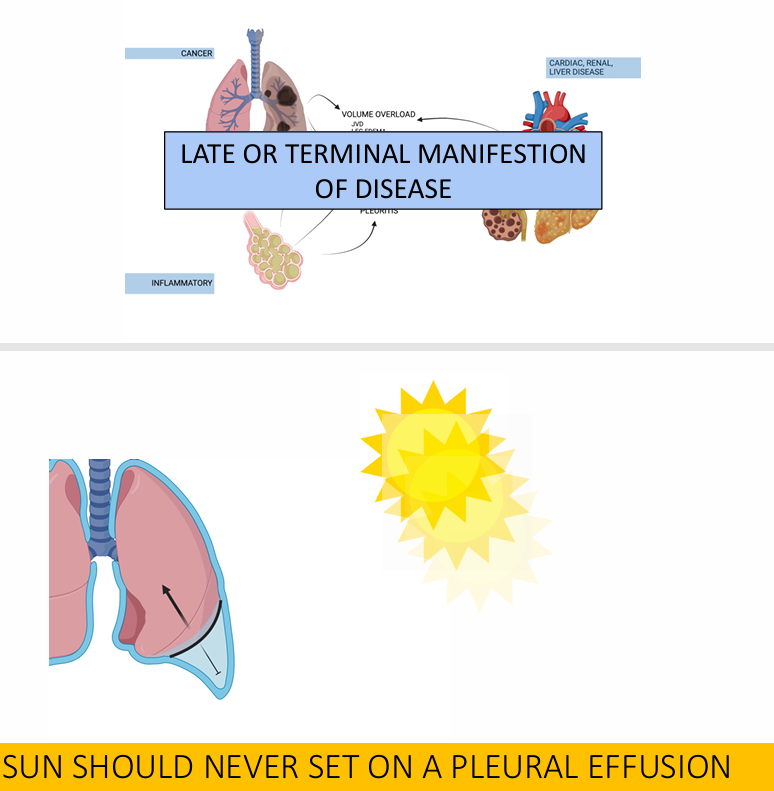
first question to ask
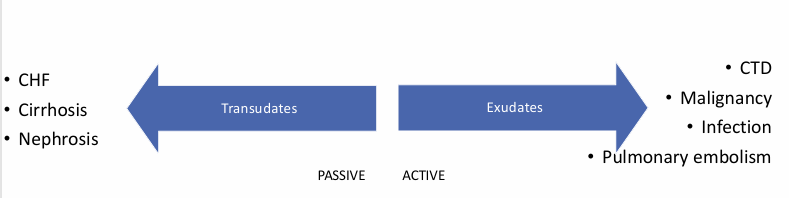
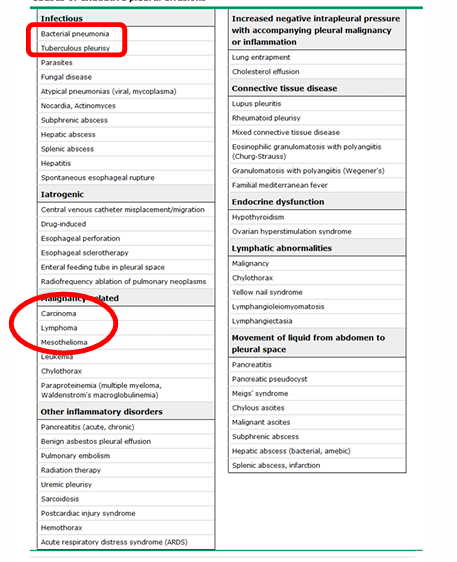
causes of exudative pleural effusions
Light’s criteria
-fluid is exudate if any of the following is true:
1) pleural TP/serum TP > 0.5
2) pleural LDH/serum LDH > 0.6
3) pleural LDH > 2/3 upper limit of normal
three test rule
-fluid is exudate if any of the following is true:
1) pleural TP > 2.9 mg/dL
2) pleural cholesterol > 45 mg/dL
3) pleural LDH > 0.45 upper limit of normal
borderline exudates occur in
-CHF
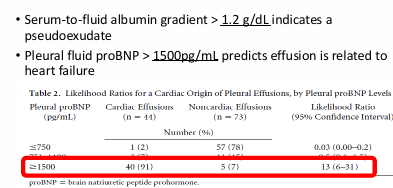
____ must be ruled out
-MPE
-MPE can be transudates in 3-5% of cases
-flow cytometry can help identify MPE due to pleural lymphoma
-pleural fluid cytology has a sensitivity of ~60% for MPE
-pleural fluid volume > 60 mL increases yield
pleural fluid cell count
-pleural hct/serum hct > 0.50 is diagnostic of hemothorax
-WBC differential: neutrophils suggest bacterial infections, eosinophilia can be from PTX or trauma/blood among other conditions, lymphocytosis suggests MTb/inflammatory conditions/MPE
manifestation of pleural disease
visual evaluation
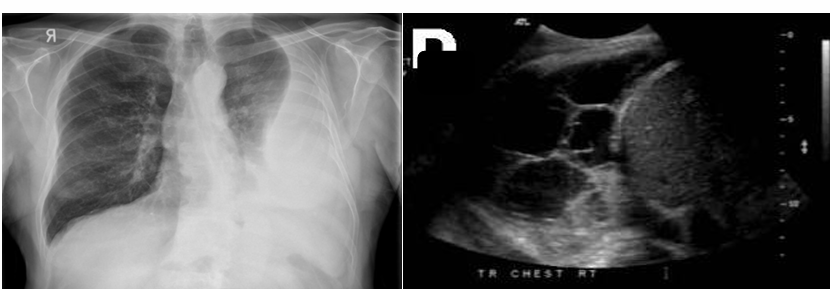
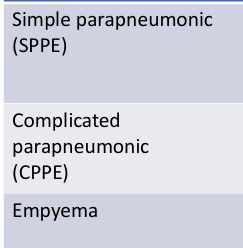
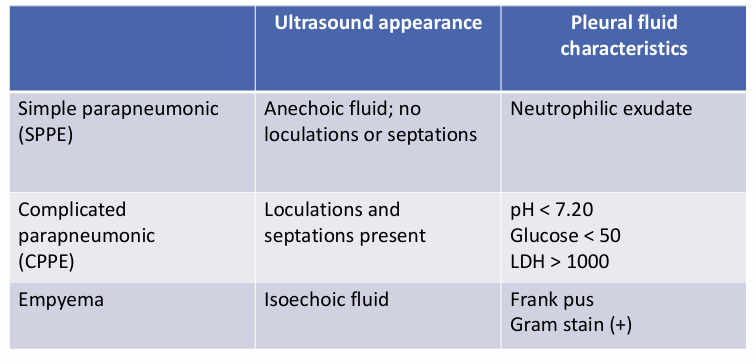
parapneumonic effusions and empyema- ultrasound appearance, pleural fluid characteristics
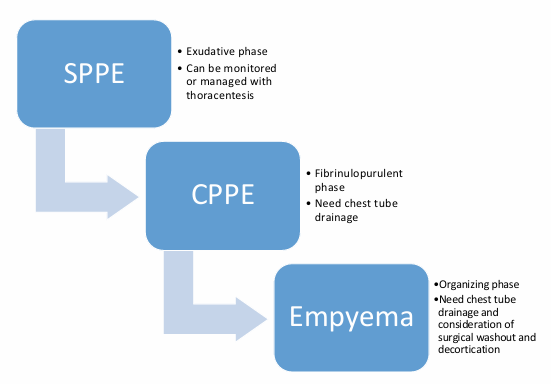
SPPE → CPPE → empyema
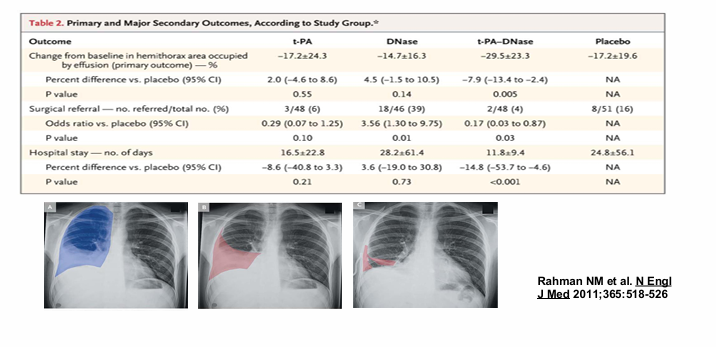
_____ facilitate drainage and reduce surgical referral for CPPE
-tPA and DNase
chylothorax
-diagnostic criteria: TG > 110 mg/dL is a chylothorax, TG < 50 mg/dL is NOT a chylothorax, between 50 and 110 mg/DL send chylomicrons
-etiologies: malignancy (lymphoma), iatrogenic, traumatic, cirrhosis, CHF
eosinophilic pleural effusions
-eosinophils are NOT commonly found in pleural tissue
-most common causes include trauma (blood and air)
-other considerations: pulmonary embolism, drugs, benign asbestos pleural effusions, infection, malignancy
asbestos-related pleural disease
-BAPEs: often unilateral, exudative effusions, typically resolve spontaneously over months, diagnosis of exclusion- must exclude MPE and malignant mesothelioma
-pleural plaques and diffuse pleural thickening
-malignant mesothelioma
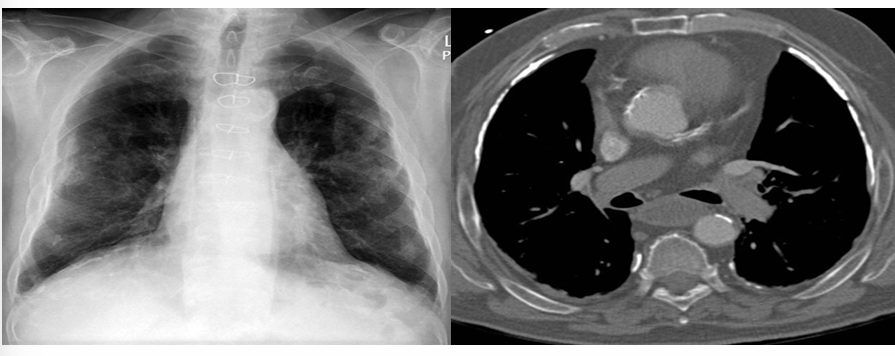
hemothorax
-early identification is key: history of trauma or thoracic procedures, anticoagulation and/or coagulopathy, ultrasound and CT can be diagnostic (35-70HU)
-rapid drainage critical to prevent empyema and fibrothorax: large bore chest tubes favored, early involvement of thoracic surgery, caution with use of intrapleural fibrinolytics, resuscitation
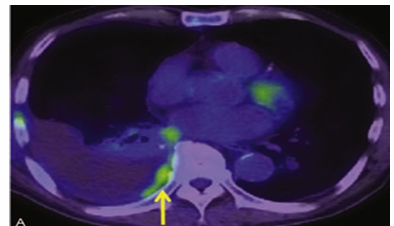
_____ can help identify MPE
-PET-CT
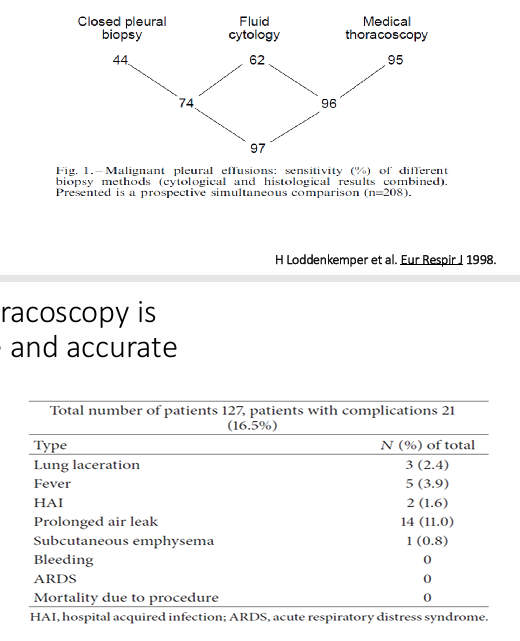
closed/blind pleural biopsy
-has low yield for MPE
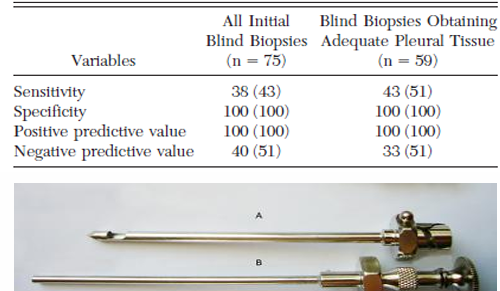
diagnosis of tuberculous pleuritis
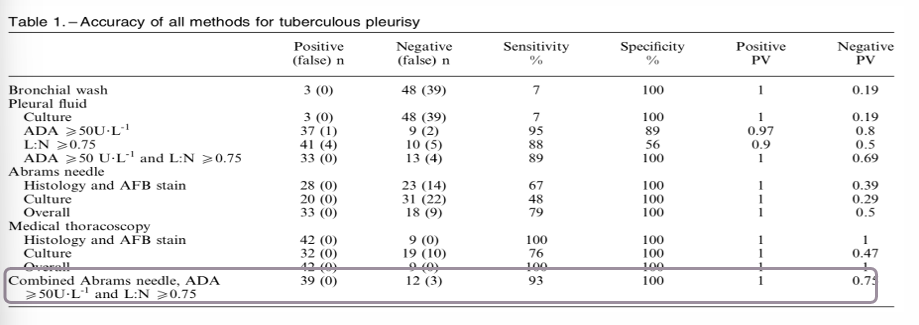
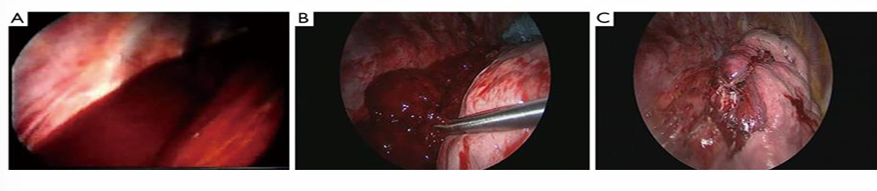
thoracoscopy
-safe and accurate
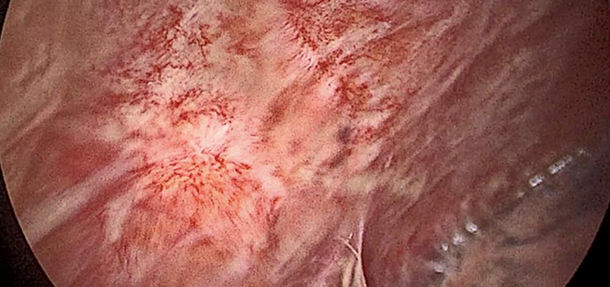
-inflamed pleura and adhesions
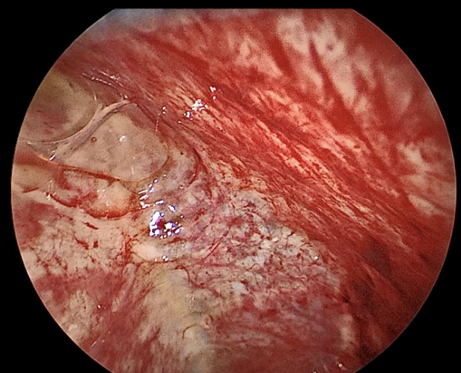
-fibrinopurulence in pleural space
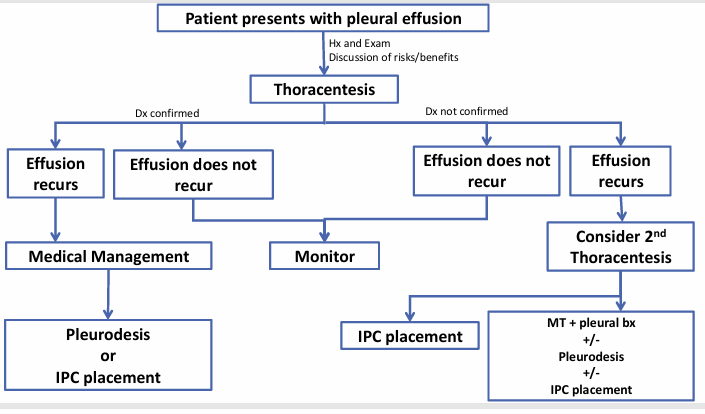
patient presents with pleural effusion- steps
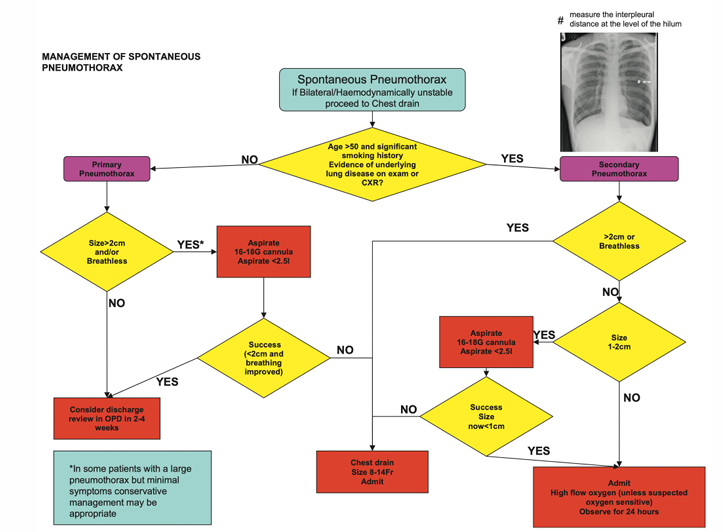
management of spontaneous pneumothorax
respiratory failure
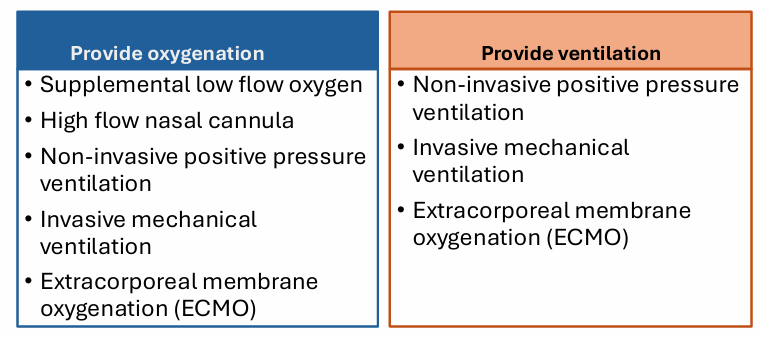
treatment for respiratory failure- in addition to treating/managing the underlying cause
1) supplemental oxygen (low flow)
2) high flow nasal cannula
3) non-invasive positive pressure ventilation
4) mechanical ventilation
5) extracorporeal membrane oxygenation (ECMO)
-all can be used in treatment of chronic respiratory failure
-2 and 5 can be used in acute forms of respiratory failure
treatment to improve gas exchange
supplemental low flow oxygen
-delivers oxygen via nasal cannula, face mask, face tent
-you set: flow rate, FiO2 (sometimes)
-can be used in: acute hypoxemia, chronic hypoxemic respiratory failure

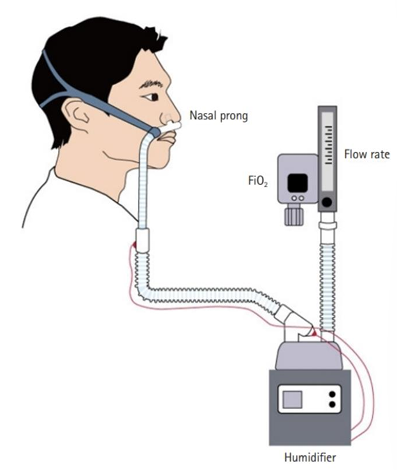
high flow nasal cannula (HFNC) or high flow nasal oxygen
-delivers warmed humidified air via large nasal prongs
-you set: flow rate of oxygen delivery, FiO2
-can be used in: acute hypoxemic respiratory failure, significant work of breathing
non-invasive ventilation
-delivers positive pressure ventilation via a tight-fitting mask
-you set: pressure to be delivered, FiO2, respiratory rate (sometimes)
-can be used in: acute and chronic hypercapnic or hypoxemic respiratory failure

invasive mechanical ventilation
-delivers oxygen as a pressure or volume targeted breath via a tube in the trachea
-provides ventilation and oxygenation
-you set: mode, pressure or volume, rate, FiO2, PEEP
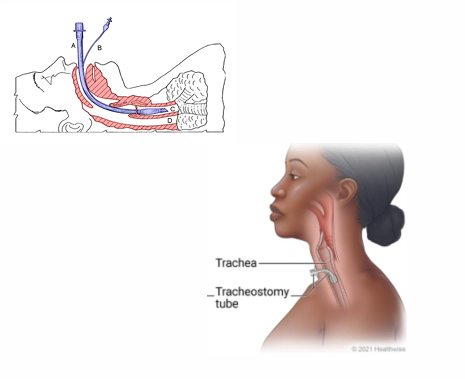
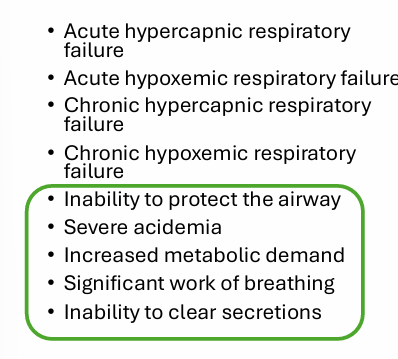
invasive mechanical ventilation can be used in
breathing with a ventilator
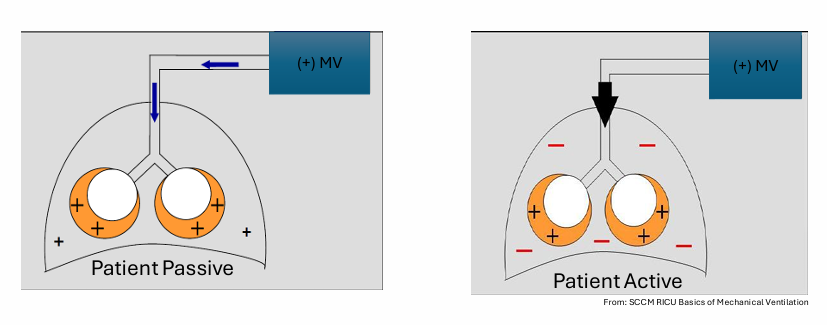
exhalation
-as with normal spontaneous breathing, expiration is passive
-relies on elastic recoil of lung and chest wall
-limited by airway resistance
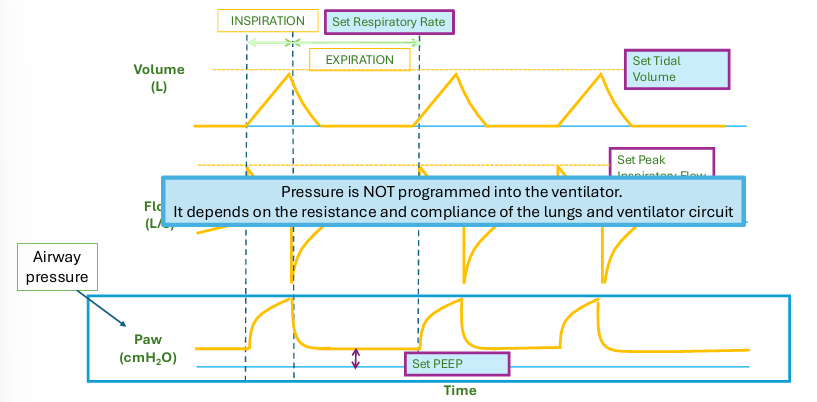
setting the ventilator
-the ventilator pushes gas into the lungs, the rest depends on what you set
-what you set: mode, volume or pressure, respiratory rate (in controlled modes), FiO2, positive end expiratory pressure (PEEP), flow (in some modes)
mode
-determines how the breath is delivered and how often (volume or pressure)
-volume control ventilation one of the most common modes
volume assist control ventilation
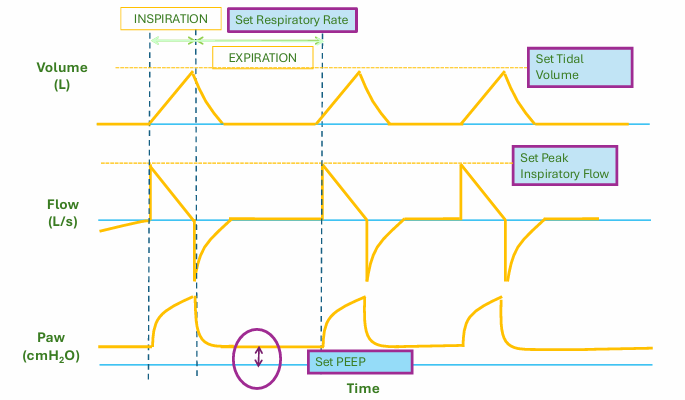
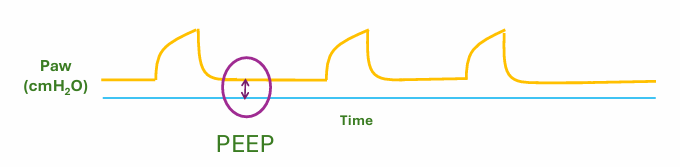
PEEP
-minimum pressure maintained in the ventilator circuit at all times
-keeps alveoli from collapsing
-opens collapsed alveoli
____ is NOT programmed into the ventilator
-pressure
-depends on the resistance and compliance of the lungs and ventilator circuit
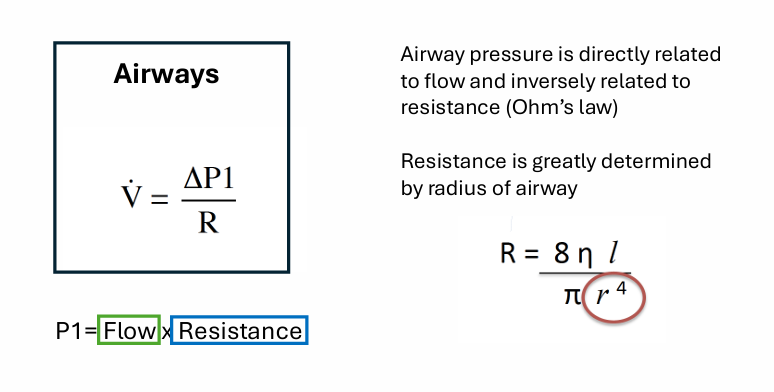
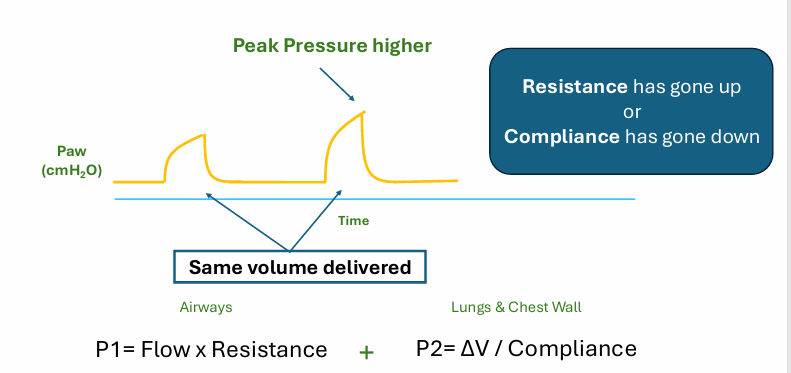
determinants of pressure
-airways
-lungs and chest wall
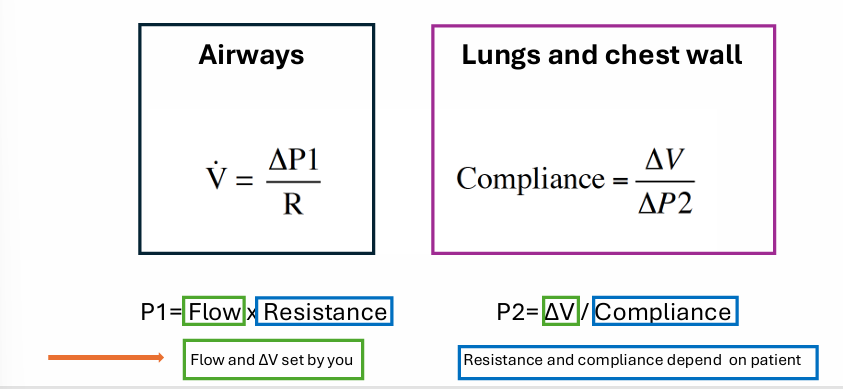
determinants of pressure- airways
-disease of the airways increase resistance
determinants of pressure- lungs and chest wall
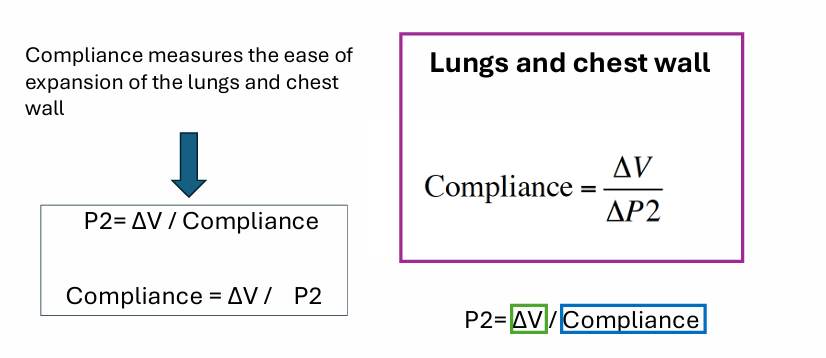
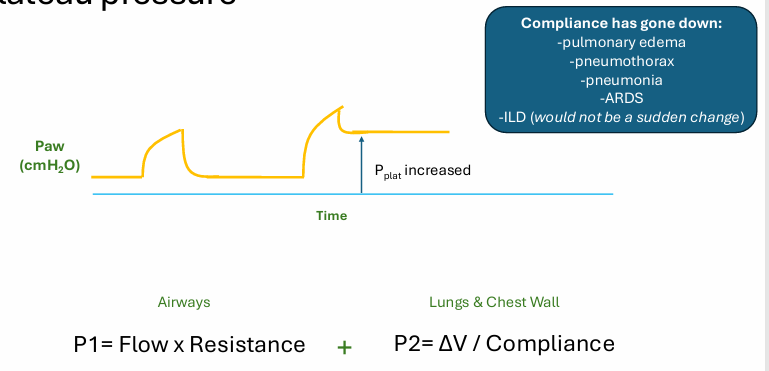
peak pressure with volume assist control ventilation
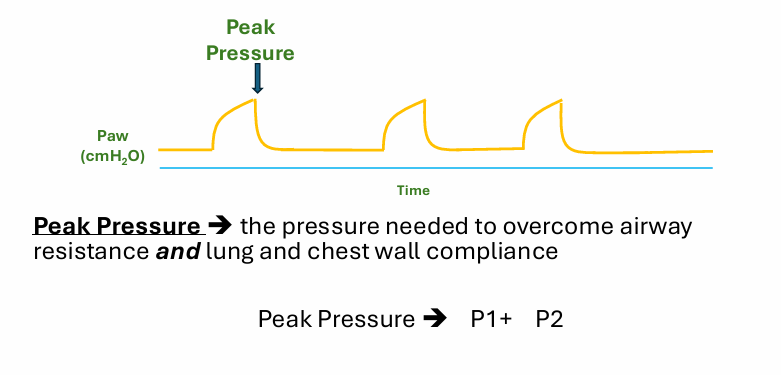
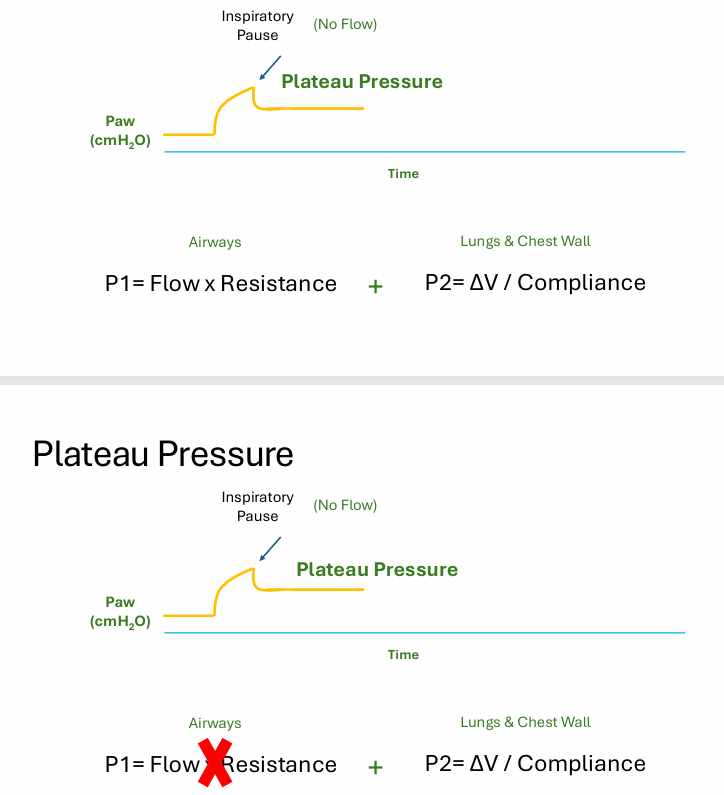
plateau pressure
-needed to measure compliance
plateau pressure- static compliance
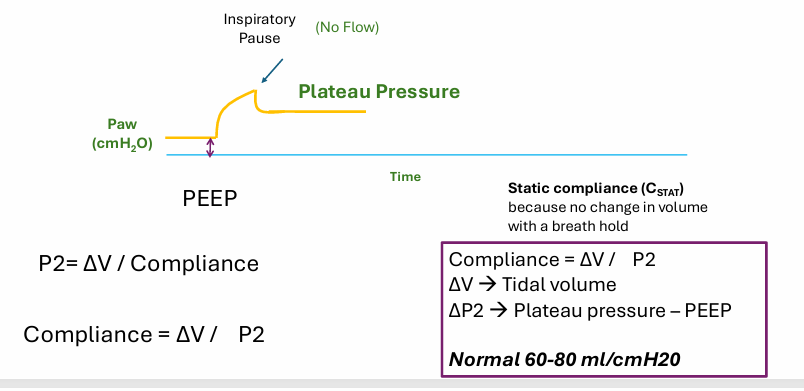
why is compliance so important clinically?
-tells us there is a problem with the lungs
-studies have shown that worsening compliance over time on the ventilator worsens outcomes
-use the interpretation compliance a lot in clinical medicine
-measurements can help diagnose different disease processes
changes in pressure
how to determine if an increase in peak pressure is due to resistance going up or compliance going down
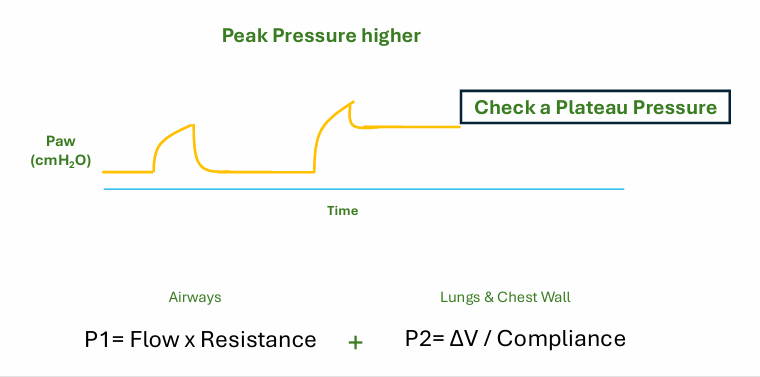
what is a plateau pressure?
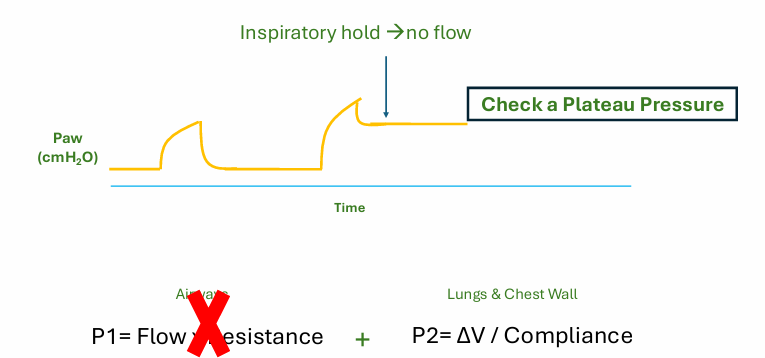
increased peak pressure with normal plateau
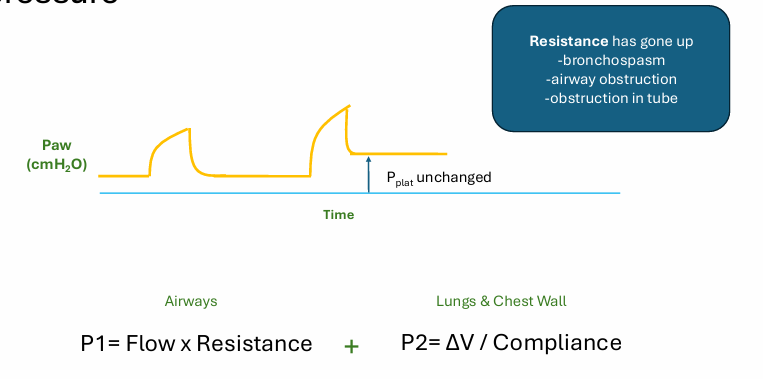
increased peak pressure with increased plateau pressure
auto PEEP
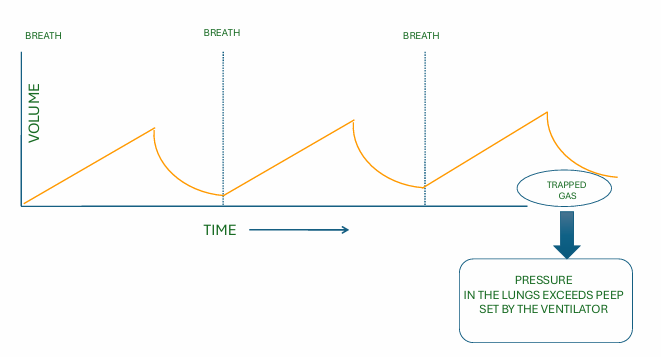
consequences of auto PEEP
-impaired ventilation
-pneumothorax
-hypotension
-increased dead space
-patient-ventilator asynchrony
how to fix auto PEEP on ventilator?
-treat asthma
-allow more time for exhalation: reduce respiratory rate, reduced tidal volume, give breath faster
conclusions
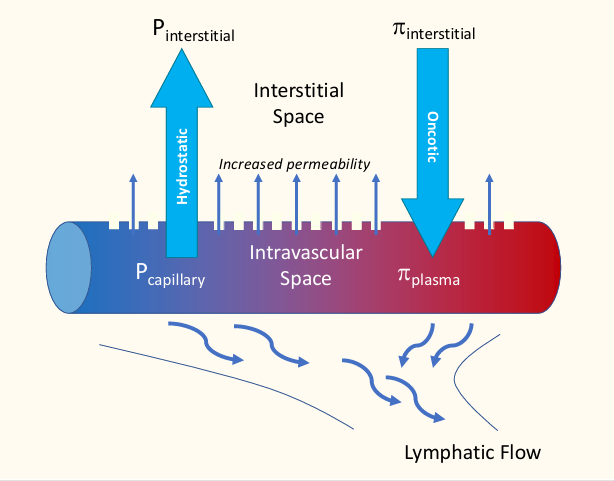
Starling equation
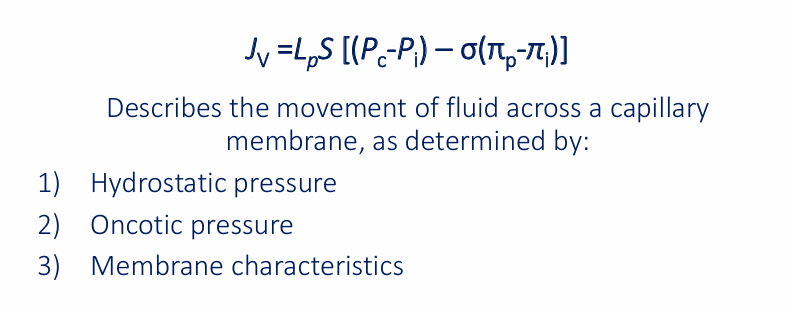
interstitial space to lymphatic flow
pulmonary edema


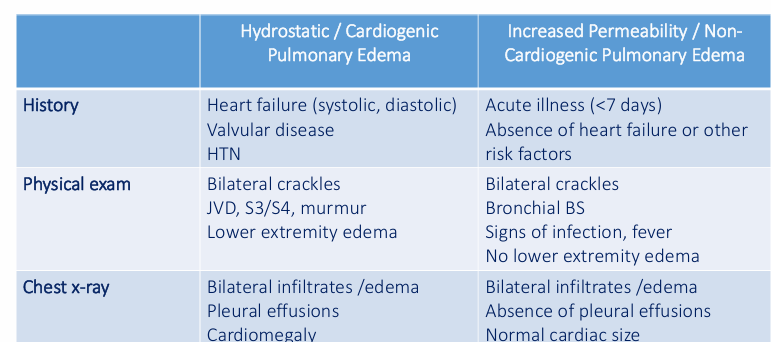
pulmonary edema- history, physical exam, chest x-ray

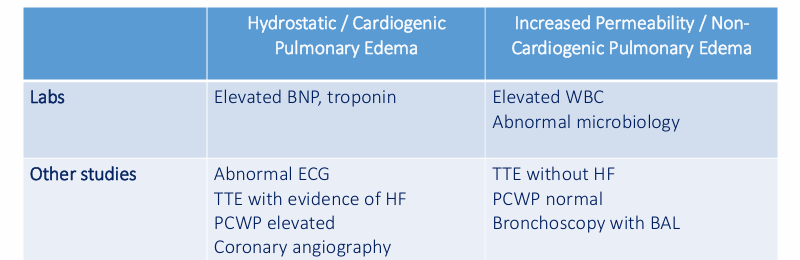
pulmonary edema- labs, other studies
non-cardiogenic pulmonary edema
-acute respiratory distress syndrome (ARDS)
-other: neurogenic, high altitude pulmonary edema (HAPE), opioid overdose, medications/toxins
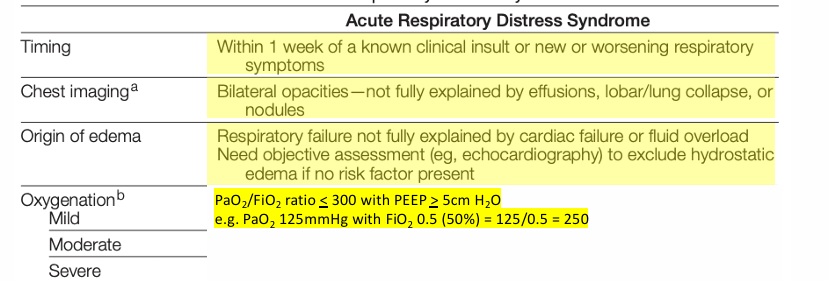
Berlin definition of ARDS
global definition of ARDS- 2023 update
-includes patients who are not mechanically ventilated including: high-flow nasal oxygen (HFNO) or non-invasive positive pressure ventilation (NIPPV)
-allows for use of lung ultrasound and SpO2 in resource-limited settings
epidemiology of ARDS
-historical incidence of ~86/100,000 person-years
-berlin definition as of 2012 has a more encompassing definition
-approximately 10-15% of ICU admissions and up to 23% of mechanically ventilated patients meet criteria for ARDS
-in recent years, ARDS incidence and admissions increased in the setting of the COVID-19 pandemic
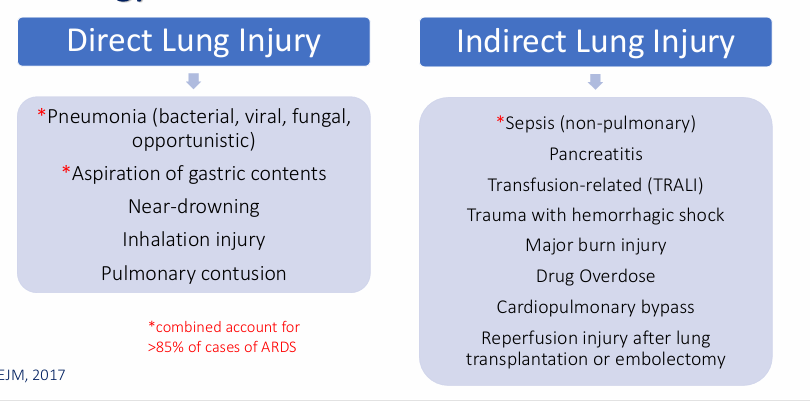
etiology of ARDS
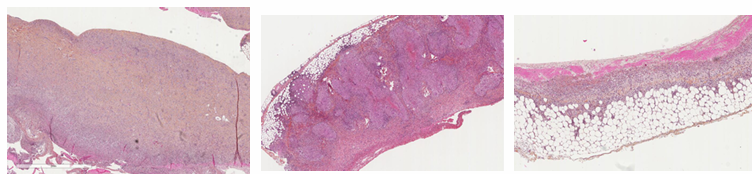
gross pathology

ARDS pathologic stages
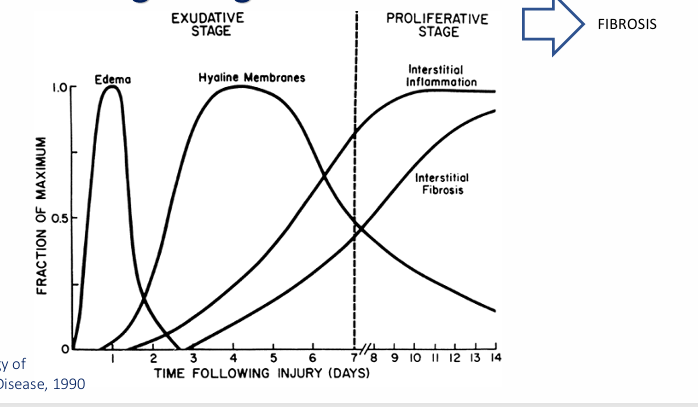
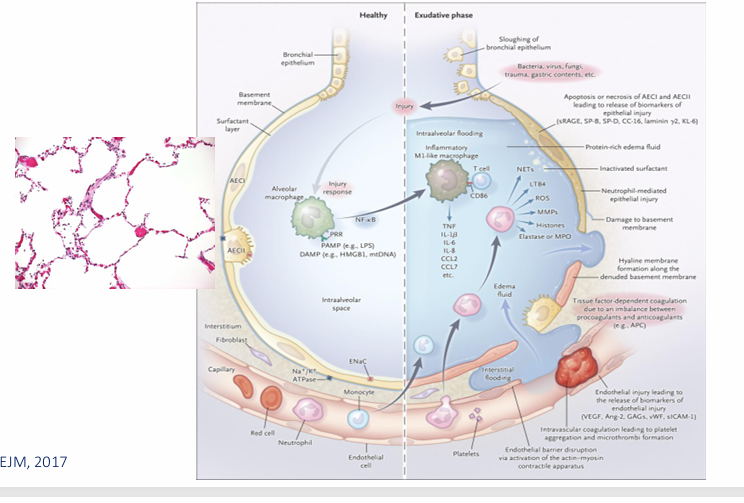
healthy → exudative phase
proliferative → fibrotic phase
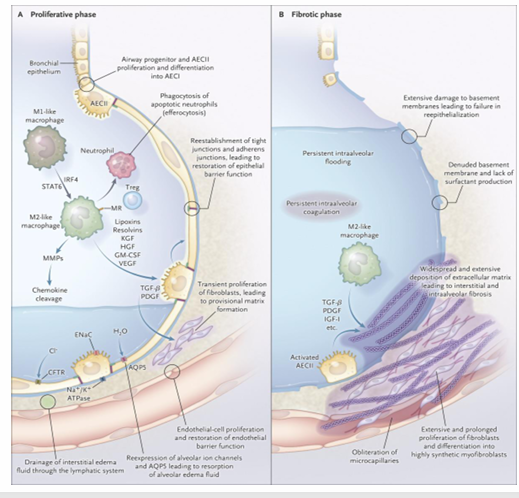
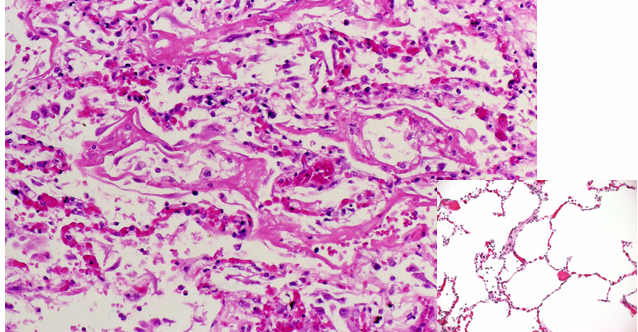
-acute exudative stage
-hyaline membrane formation
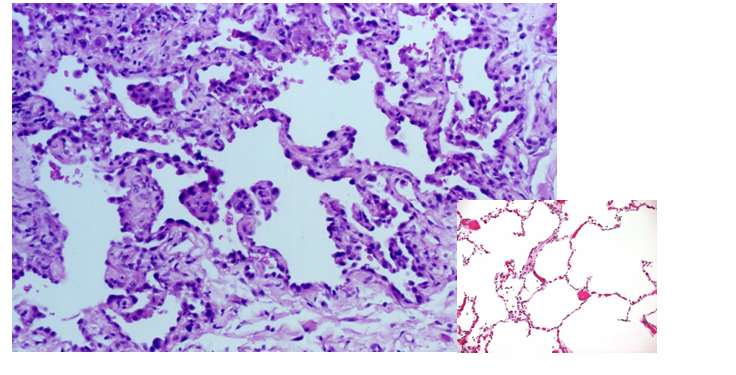
-proliferative stage
-pneumocyte hyperplasia
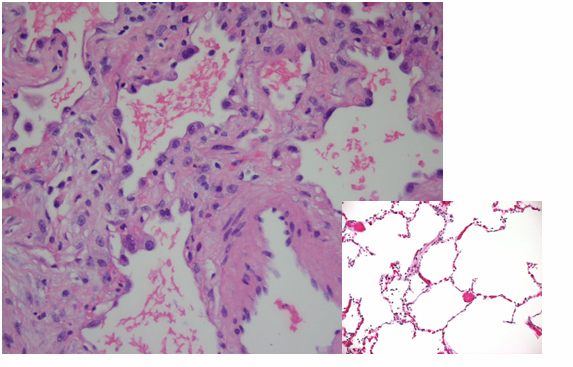
-fibrotic stage
-interstitial fibrosis
pathophysiologic consequences
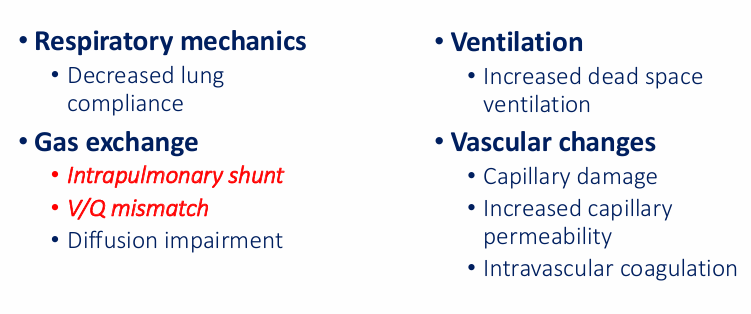
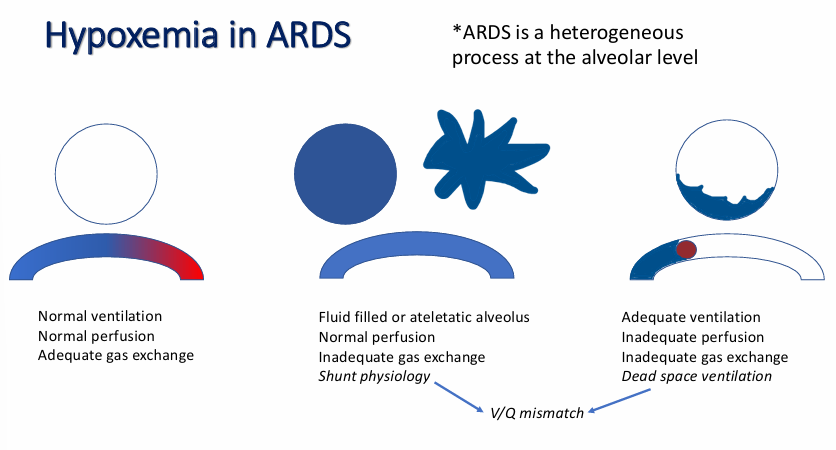
hypoxia in ARDS