Module 2 - Chest Radiography
1/38
Earn XP
Description and Tags
Flashcards for General Chest Radiography Concepts
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
What is the rationale for using a PA projection over an AP in chest radiography?
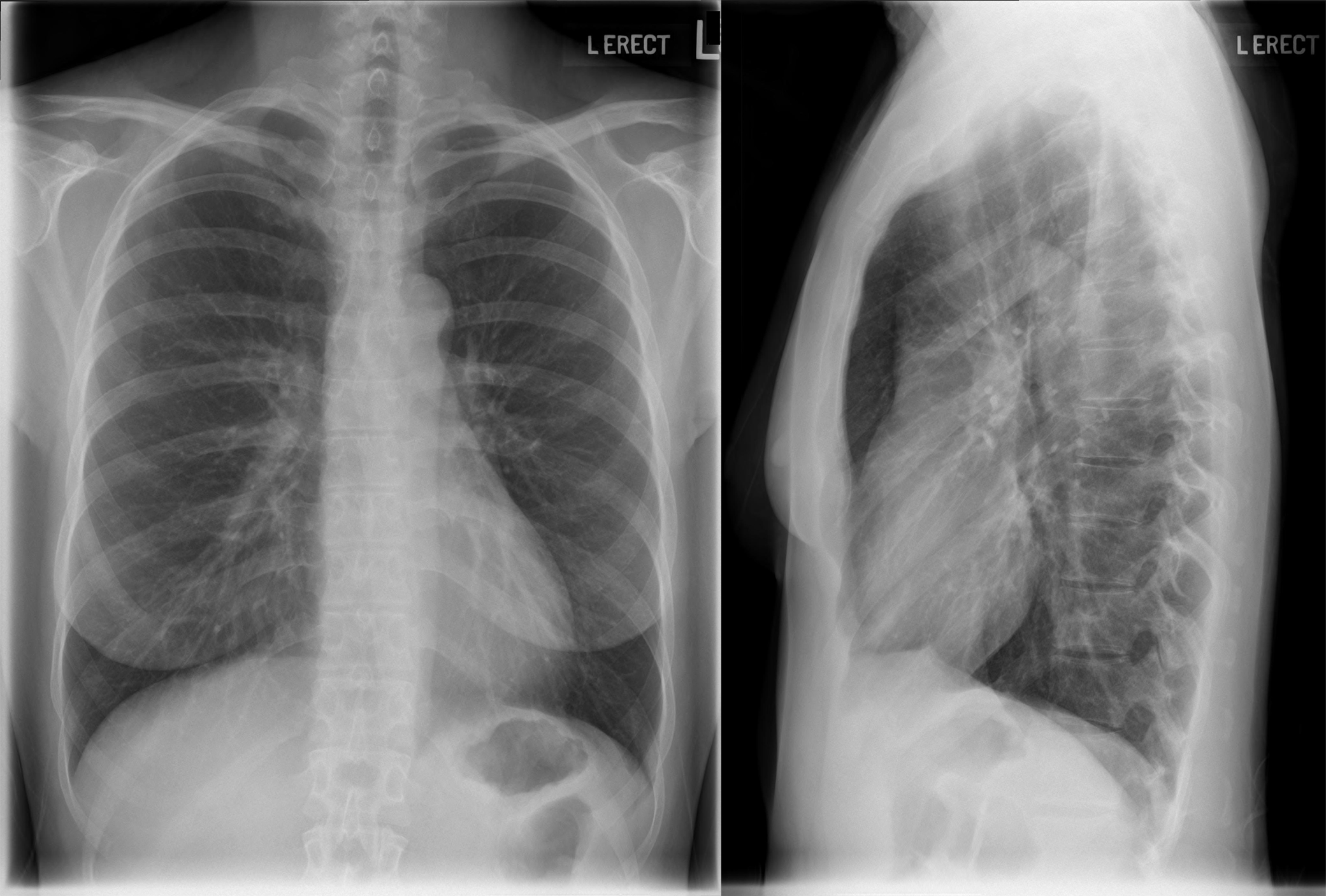
PA projection reduces heart magnification, removes scapulae from lung fields, and usually results in better inspiration.
What anatomical structures are key for evaluating positioning on a chest radiograph?
Clavicles, scapulae, ribs, apices, costophrenic angles, hilum, and diaphragm.
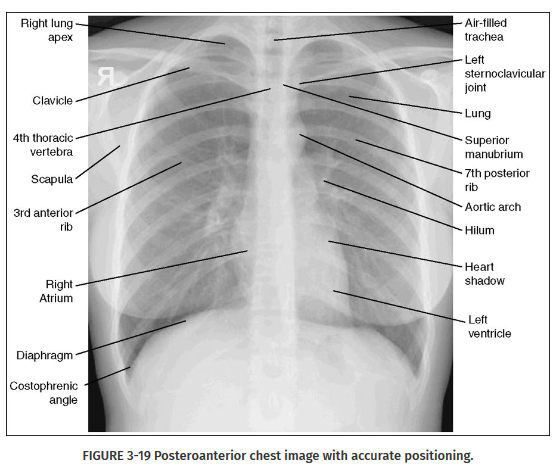
Where are the lung apices located?
Above the clavicles, extending to the level of T1.

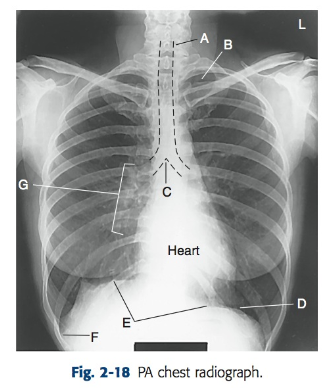
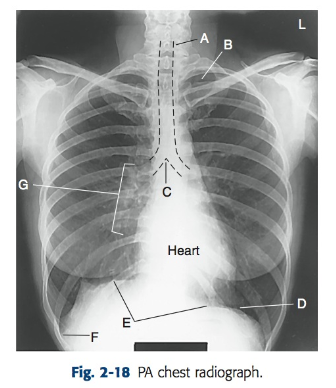
What is the carina and why is it important?
The carina (C) is where the trachea bifurcates into bronchi; it helps assess endotracheal tube placement.
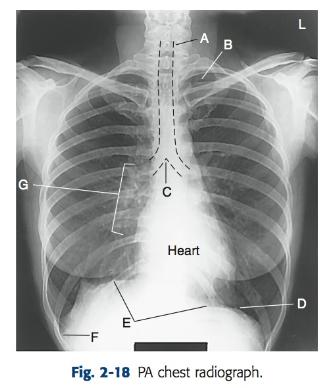
What is the hilum?
(G) The root area of each lung where vessels, bronchi, and lymphatics enter and exit.
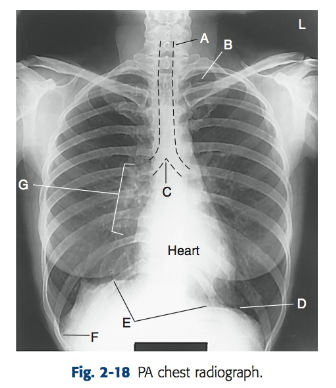
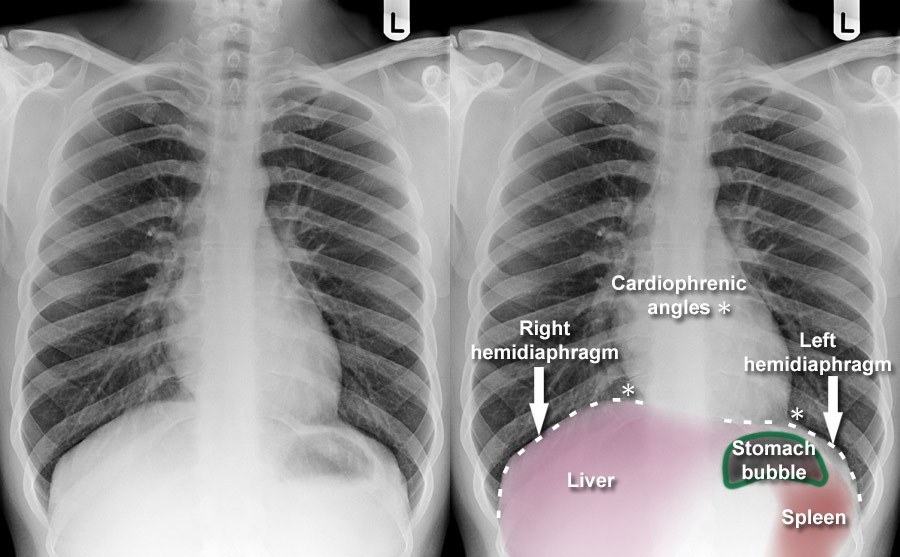
What are costophrenic angles?
(F) The most inferior and lateral parts of the lung where the diaphragm meets the ribs; important for detecting fluid.
How do you detect tilt on a PA/AP chest X-ray?
Uneven lung apices; clavicles at unequal heights; chest longitudinal axis not parallel to IR.

How is rotation assessed on a PA/AP CXR?
Medial clavicles should be equidistant from the spine; spinous processes centered; trachea midline.
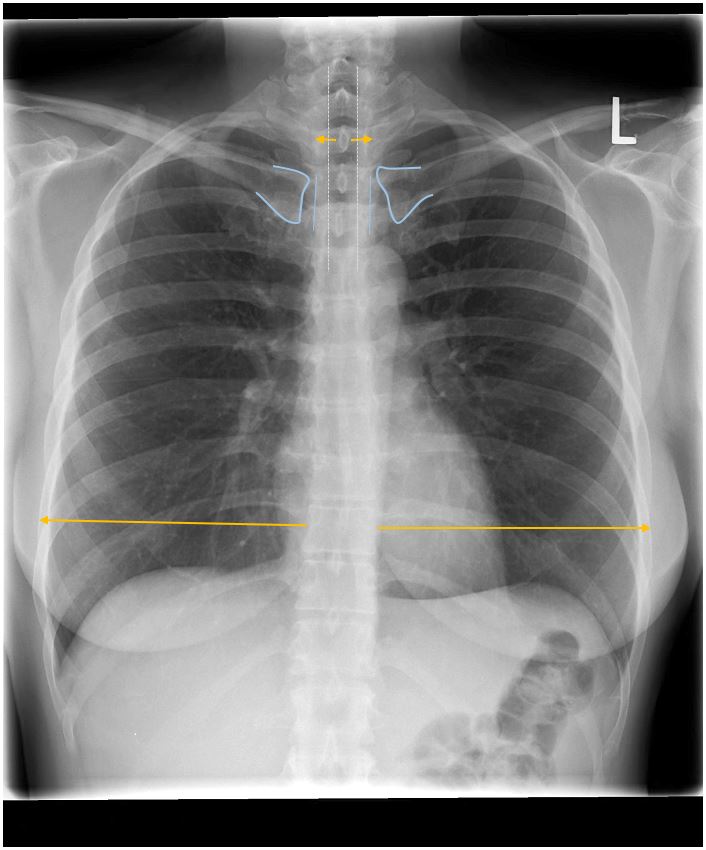
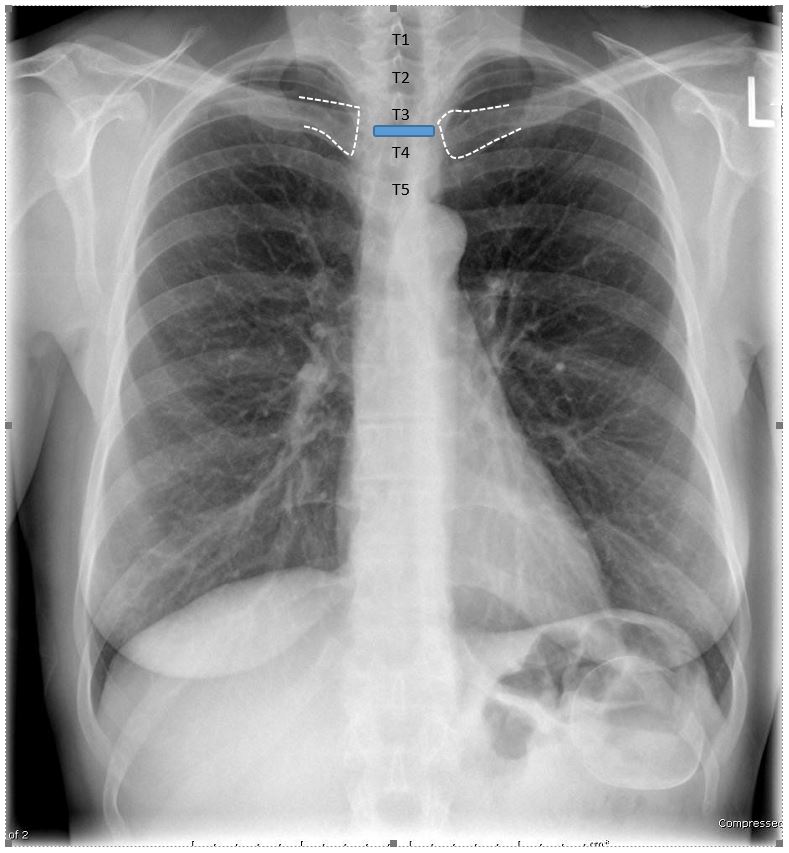
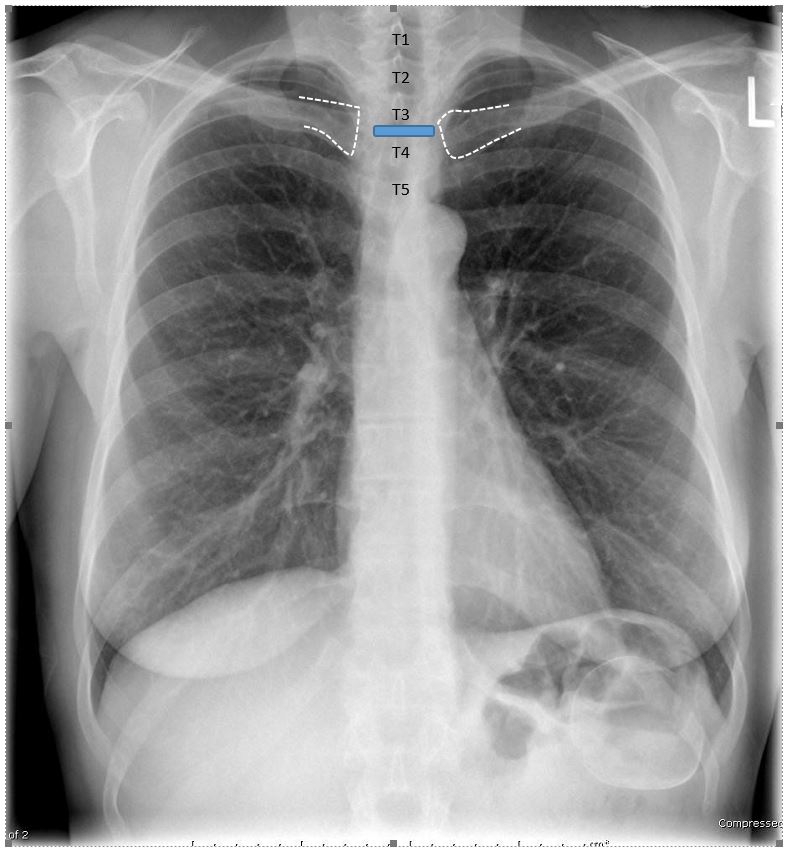
What is the key landmark for evaluating flexion/extension on PA/AP?
The medial clavicle ends relative to the T3-T4 intervertebral disc space. (none seen in image)
Why is the left lateral projection typically preferred?
To reduce heart magnification by placing the heart closer to the IR.
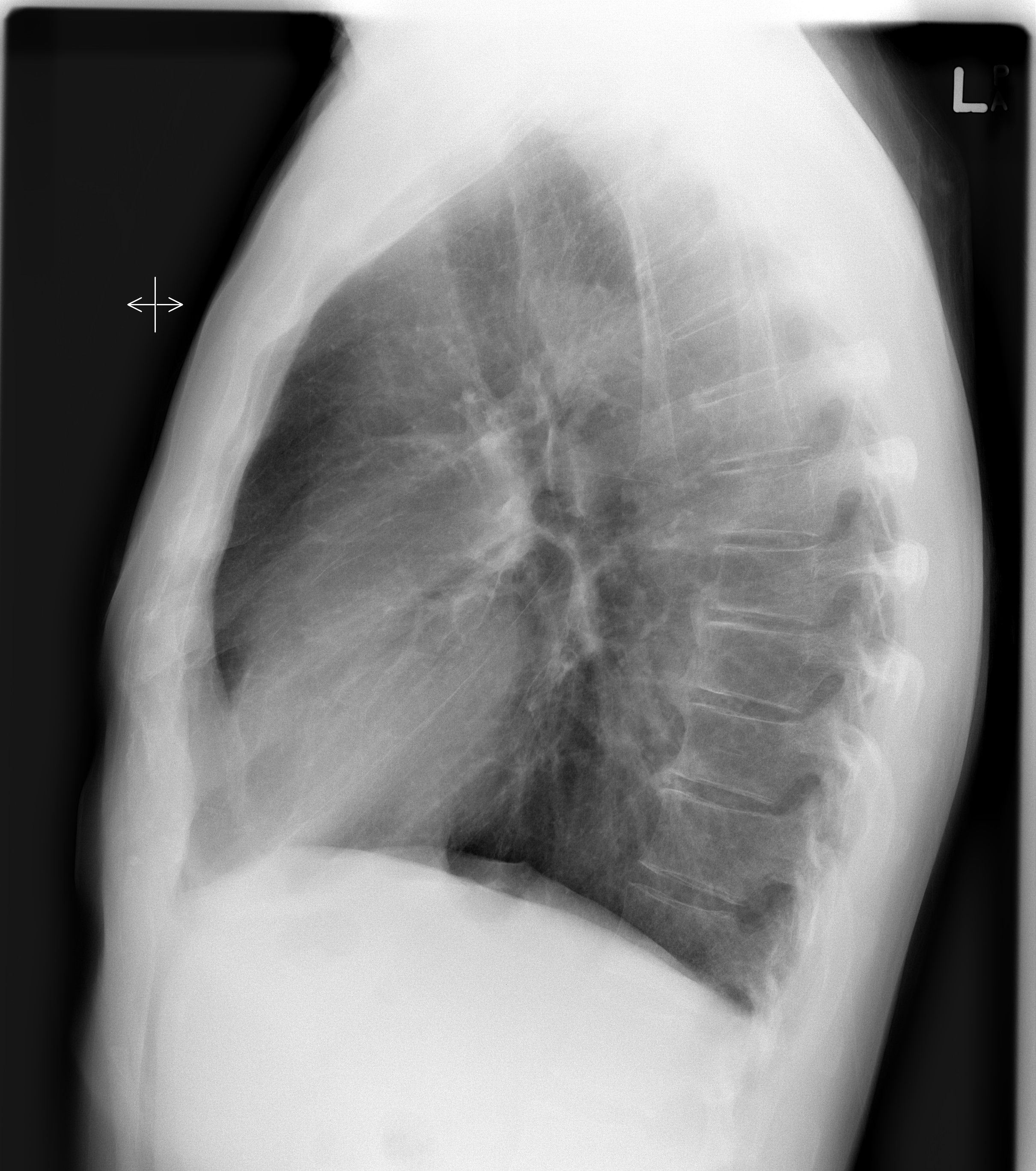
What are criteria for no tilt on a lateral chest radiograph?
Stacked posterior ribs, open intervertebral joints, and aligned hemidiaphragms. (Image shows tilt away from IR)
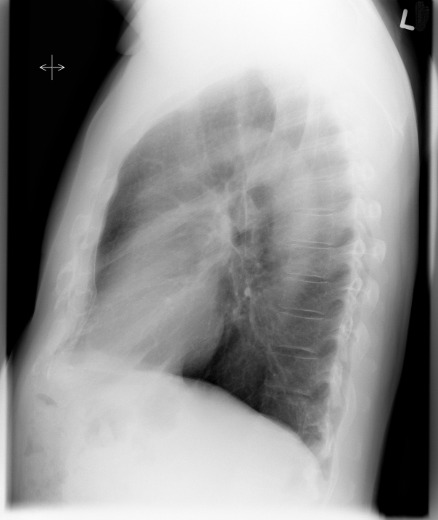
How do you detect rotation on a lateral chest X-ray?
Look for separation of posterior ribs and whether the sternum is in profile.
What landmark helps identify the left hemidiaphragm?
The gastric air bubble (fundus of stomach).
Why must arms be raised in a lateral chest X-ray?
To clear soft tissue from the upper thorax and visualize the retrotracheal space (Raider’s triangle).

How do you remove the scapulae from the lung fields in PA/AP projections?
Roll the shoulders forward.
How many posterior ribs should be visible above the diaphragm on a PA/AP chest to indicate adequate inspiration?
At least 9 full posterior ribs.
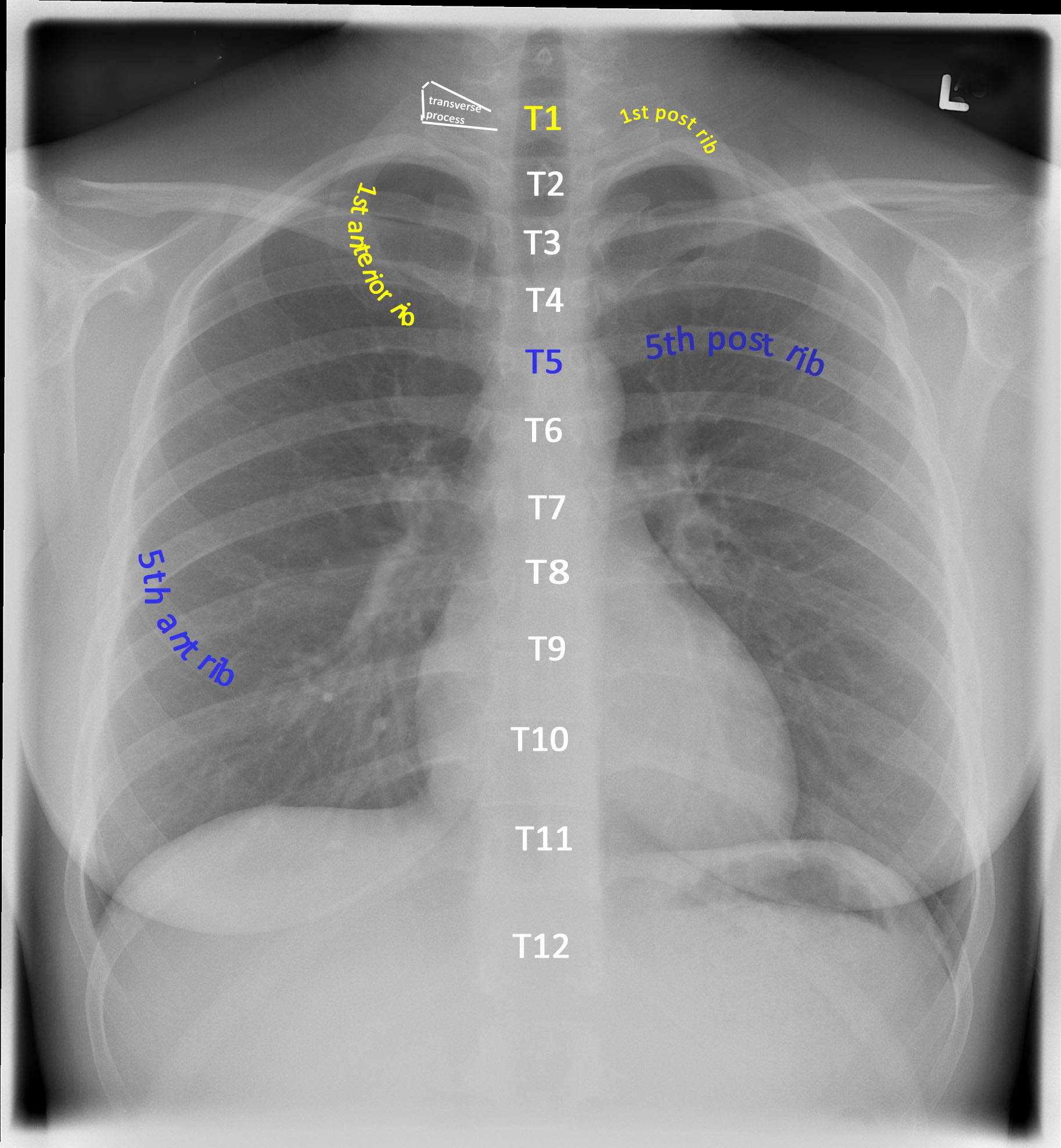
How many posterior ribs should be visible on a PA expiration chest?
8 or fewer.
What level should the diaphragm reach on a lateral CXR for full inspiration?
Below the T11 vertebra.

What are key indicators of good chest radiograph image quality?
Sharp outlines, visible thoracic spine through heart, lung markings throughout, air-filled trachea, and no motion artifact.
What does poor inspiration mimic on a CXR?
Pathology such as pneumonia or pulmonary edema.
How can voluntary motion be minimized?
Shorten exposure time and give clear breathing instructions.
What does waist flexion/extension affect on an AP/PA CXR?
The vertical position of the medial clavicles.
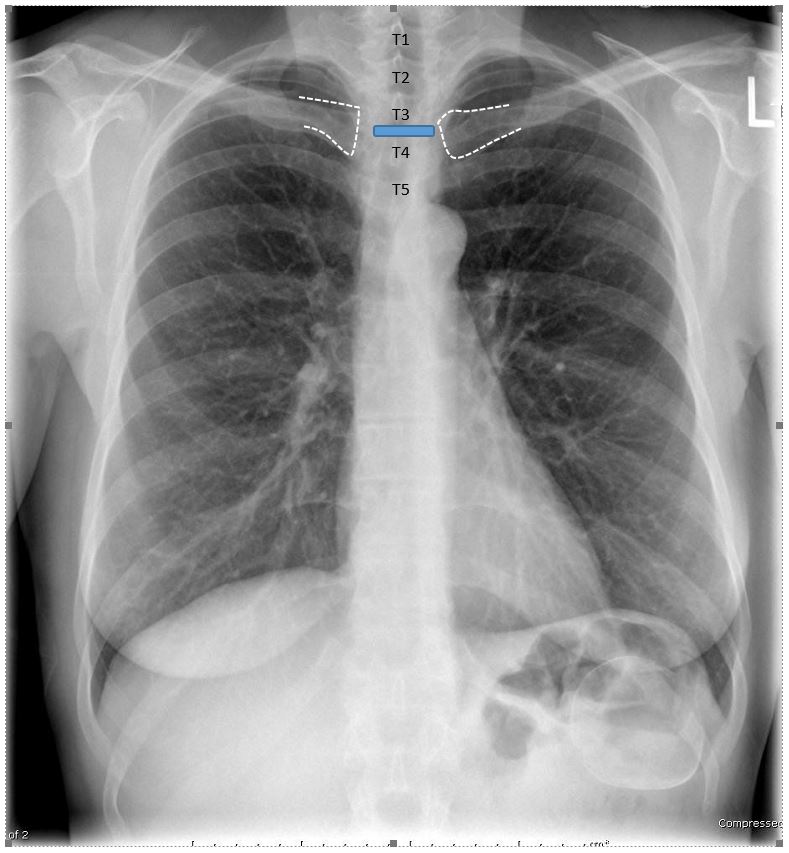
What causes the clavicles to appear too high on a CXR?
Patient extension at the waist or incorrect beam angulation.
What is the significance of “posterior” ribs in a lateral chest X-ray?
They are the reference for evaluating rotation (they should be superimposed).
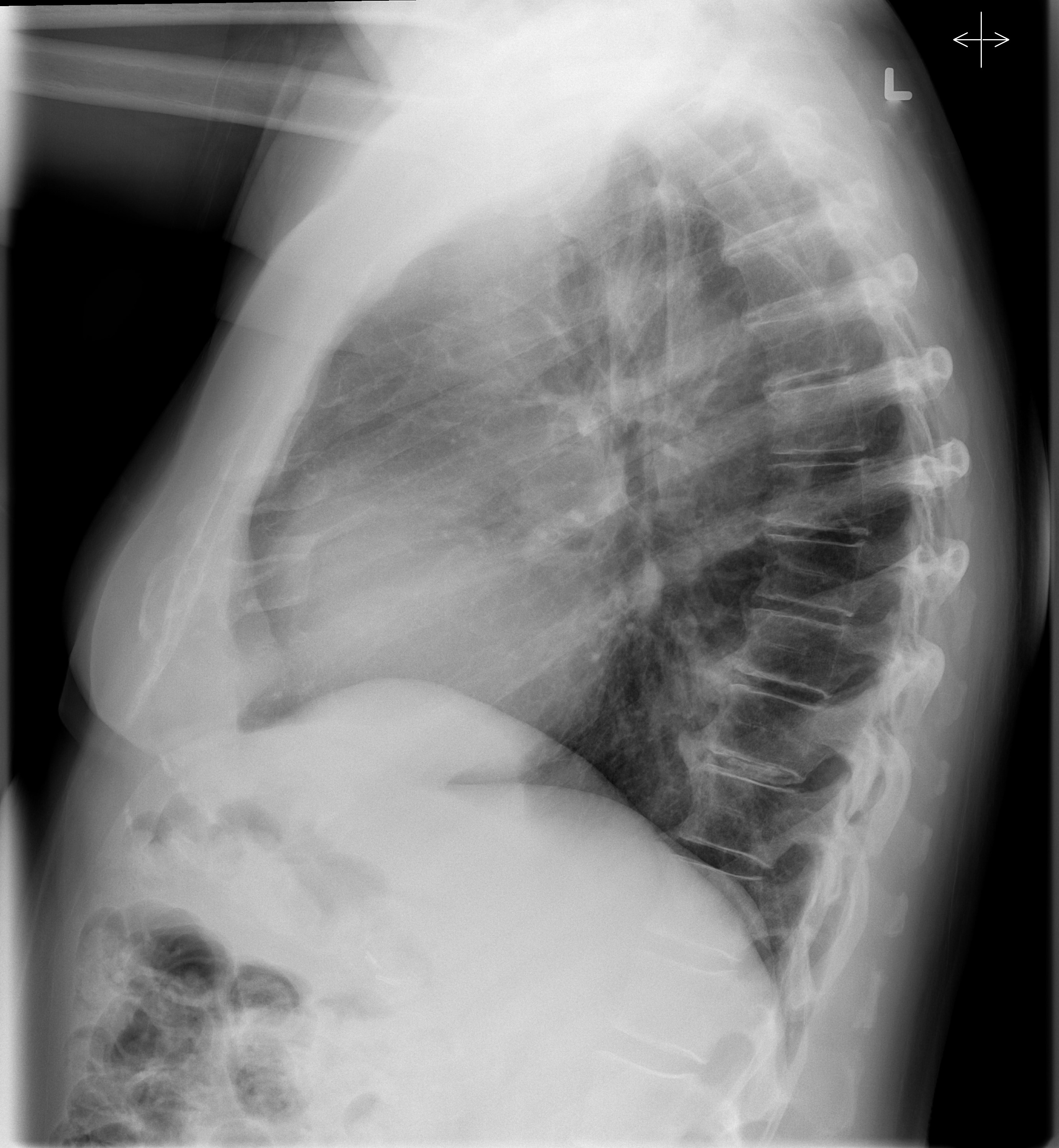
On a lateral CXR, the right posterior ribs appear higher. What does this mean?
The patient is tilted toward the IR.
On a PA chest X-ray, the medial clavicle ends are at T2. What does this indicate?
The patient may be extended or there may be an incorrect caudal beam angle.
What is the purpose of an inspiration/expiration chest exam?
To evaluate pneumothorax or foreign body by comparing lung inflation.
What does it mean if the ribs appear more horizontal on a CXR?
The patient is extended at the waist.
What positioning error causes the heart to appear artificially enlarged on an AP chest X- ray?
Increased object-to-image distance (OID) due to supine or AP positioning.
What is the expected location of the medial clavicle ends on an acceptable AP CXR?
At the level of the T3-T4 intervertebral disc space (T3 is acceptable).
How do you assess for proper lateral alignment in a lateral chest X-ray?
The midcoronal plane should be parallel to the IR; look for symmetric apices and hemidiaphragms.
What is the main difference between voluntary and non-voluntary motion on a chest X- ray?
Voluntary motion (e.g., breathing) can be controlled; non-voluntary motion (e.g., heart) cannot.
How can a technologist reduce motion artifact if a patient is unable to hold their breath?
Decrease the exposure time by increasing mA (to maintain mAs).
What anatomical features should remain sharp to confirm no motion artifact?
Heart borders, diaphragm edges, and lung markings.
Why might hypersthenic patients require a caudal angle on AP chest X-rays?
They often flex at the waist, causing clavicles to project superiorly.
In which clinical scenario would an expiration chest X-ray be ordered?
To assess for small pneumothorax or air-trapping (e.g., in inhaled foreign body cases).
How should technologists adapt positioning when one shoulder has limited ROM?
Raise the "good" arm as high as possible to reduce superimposition in the lateral view.
What is the “light trick” used for in lateral chest positioning?
To help align the torso so the posterior ribs are superimposed by checking the collimator light’s shadow on both sides of the patient.
Why does a larger patient require more rotation to achieve a true lateral CXR?
Greater beam divergence and OID require compensation to maintain rib superimposition.