Acute Hyperglycemia: DKA and HHS
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
DKA
most common cause of death in children with T1DM
DKA
reduced insulin concentrations due to "absolute insulin deficiency," causing an increase in counterregulatory hormones such as catecholamines, cortisol, and glucagon
- most often occurs in T1DM
- mortality rate <5%
- hyperglycemia due to increased gluconeogenesis and glycogenolysis and decreased glucose utilization
- increased lipolysis leads to an increase in FFA which leads to hepatic fatty acid oxidation, forming ketone bodies, which results in ketonemia and metabolic acidosis
hyperglycemia + hyperketonemia + metabolic acidosis
what is the definition of DKA?
hyperglycemia + dehydration
definition of HHS
HHS
reduced insulin concentrations caused by a "relative insulin deficiency," where endogenous insulin secretion is adequate enough to stop ketogenesis but not to facilitate glucose utilization
- common in T2DM primarily due to illness
- measured by C-peptide
- hyperglycemia due to increased gluconeogenesis and glycogenolysis and decreased glucose utilization
- dehydration painted with decreased fluid intake causes hyperosmolarity
- mortality rate 20%
corticosteroids
thiazide diuretics
atypical antipsychotics: Quetiapine, Olanzapine
acute hyperglycemia causes are infections, inadequate/omitted insulin, pancreatitis, and the following medications:
DKA
which acute hyperglycemic state is described below?
- develops over hours to days
- usually alert (unless severe)
- n/v, abdominal pain
- fruity breath
- Kussmaul breathing
- polyuria, polydipsia, weight loss, dehydration
HHS
which acute hyperglycemic state is described below?
- develops over days to weeks
- change in cognitive state
- severe dehydration
- often co-presenting with another acute illness
- polyuria, polydipsia, weight loss
>250 mg/dl
at what glucose level could someone be diagnosed with DKA?
> 600 mg/dl
at what glucose level could someone be diagnosed with HHS?
mild: 7.25-7.30
moderate: 7.00-7.24
severe: <7
at what pH level could someone be diagnosed with DKA?
>7.3
at what pH level could someone be diagnosed with HHS?
>320 mOsm/kg
at what serum osmolality could someone be diagnosed with HHS?
mild: >10
moderate and severe: >12
at what anion gap could someone be diagnosed with DKA?
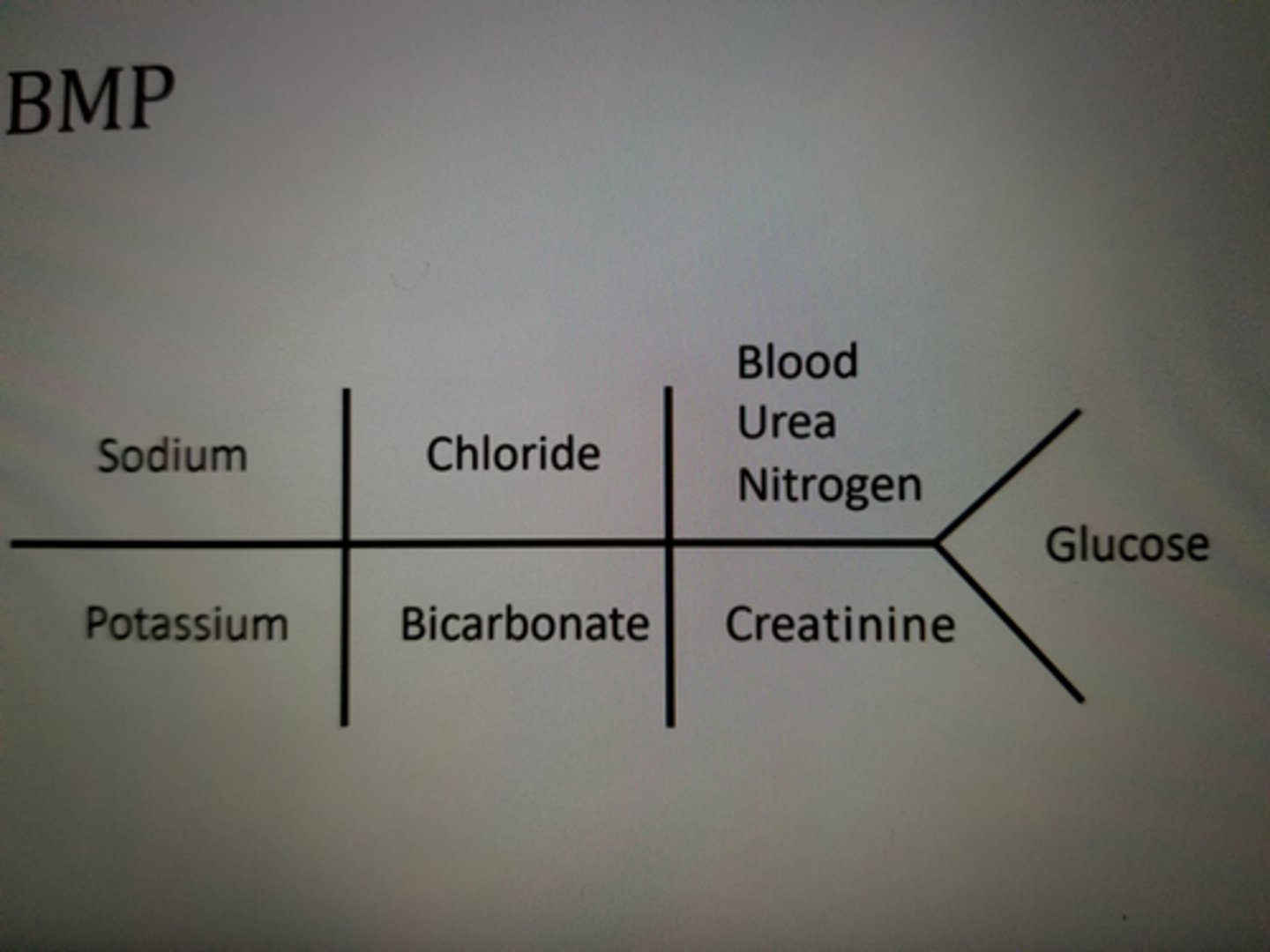
AG = Na - Cl - HCO3
formula to calculate anion gap
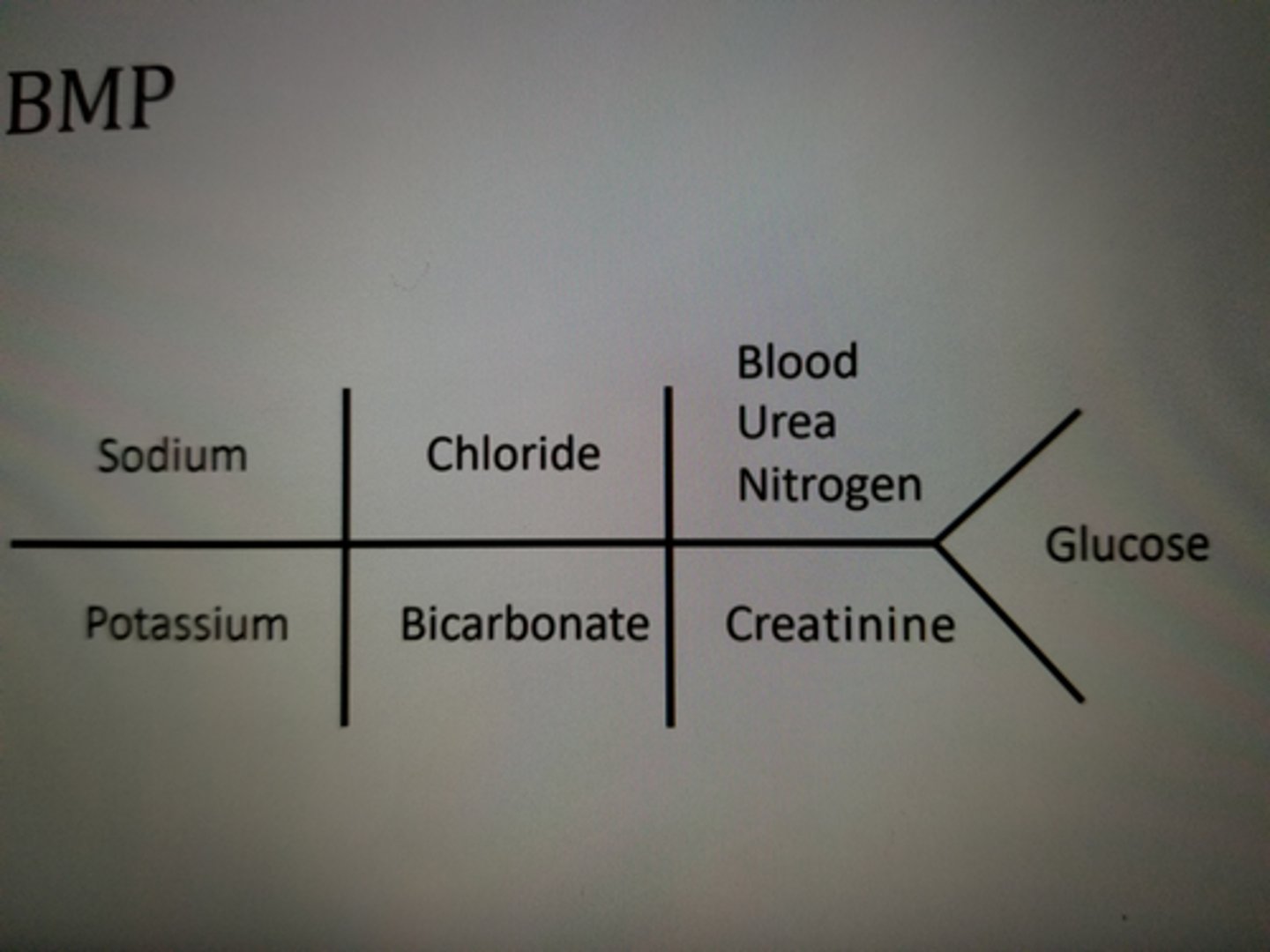
Osmolality (mOsm/kg) = 2Na + (Glu/18) + (BUN/2.8)
formula to calculate serum osmolality
fluid management
goal is to expand volume and increase renal perfusion in patients with DKA or HHS
0.9% NS
what is the initial fluid of choice in acute hyperglycemia?
15-20 ml/kg in the first hour
what is the initial rate of 0.9% NS for acute hyperglycemia?
200-500 ml/h
what is the maintenance rate of fluids for acute hyperglycemia?
- use corrected sodium to determine which maintenance fluid to use
Corrected Na = measured Na + [0.016*(glu-100)]
formula for corrected Na.
0.45% NaCl
if the corrected sodium is normal (135-145 mEq/L) or elevated use ______ as your maintenance fluid (200-500 ml/h).
0.9% NaCl
if the corrected sodium is low (<135 mEq/L), use _____ as your maintenance fluid (200-500 ml/h).
true
T/F: Hyperglycemia is corrected faster than ketoacidosis.
add D5W to maintenance fluids
reduce maintenance rate to 150-250 ml/h
Hyperglycemia is corrected faster than ketoacidosis. Once plasma glucose levels are <200 mg/dl for DKA and <300 mg/dl for HHS, add _____ to maintenance fluids to avoid hypoglycemia and reduce the maintenance rate to ______ ml/h.
150-200 mg/dL
blood glucose target for DKA
200-250 mg/dL
blood glucose target for HHS
0.1 units/kg of rapid-acting insulin SUBQ
For mild, moderate, or uncomplicated DKA, give an initial bolus of ____ units/kg of _____-acting insulin SUBQ.
maintenance = 0.1 units/kg/h OR 0.2 units/kg/2h of rapid-acting insulin SUBQ
For mild, moderate, or uncomplicated DKA, give an initial bolus of 0.1 units/kg of rapid-acting insulin SUBQ and maintenance of ____ units/kg every ____ hour(s) of ____-acting insulin SUBQ.
IV infusion of regular insulin at 0.1 units/kg/h
Optional IV bolus: 0.1 units/kg of regular insulin
For mild, moderate, or severe DKA, start an IV infusion of ____ insulin at _____ units/kg/hr. May give an optional IV bolus of _____ units/kg of _____ insulin
IV infusion: regular insulin at 0.05 units/kg/h
For patients with HHS and no ketonemia or acidosis, start an IV infusion of ____ insulin at _____ units/kg/h.
IV infusion: regular insulin at 0.1 units/kg/h
For patients with HHS and ketonemia or acidosis, start an IV infusion of ____ insulin at _____ units/kg/h.
2-4 hours
monitor patients with DKA or HHS every ___ hours until stable.
BG < 200 mg/dl
venous pH >7.3
bicarb > 18 mEq/L
serum ketones < 0.6
criteria for resolved DKA
BG < 250 mg/dl
serum osmolality < 300 mOsm/kg
urine output > 0.5 ml/kg/h
mentally alert
criteria for resolved HHS
0.5-0.6 units/kg/day
- split between basal and bolus with a sliding scale correctional insulin if needed
When DKA or HHS is resolved, IV regular insulin infusion can be transitioned to SubQ rapid-acting insulin. Patients can be restarted on their home regimen of insulin. For insulin naive patients, start at ____ units/kg/day.
1-2 hours
Before stopping IV insulin infusion, there must be an overlap of ____ hours after SubQ insulin begins to ensure adequate plasma insulin levels.
<5mEq/L
Insulin administration, correction of acidosis, and volume expansion can cause hypokalemia. Initiate potassium replacement once potassium levels are <____ mEq/L.
20-30 mEq of K+
Insulin administration, correction of acidosis, and volume expansion can cause hypokalemia. Initiate potassium replacement once potassium levels are <5 mEq/L. Add _____ of K+ to each liter of maintenance fluid to maintain a potassium level of 4-5 mEq/L
<1 mg/dL
Only replace phosphate if serum phosphate is <____mg/dL AND the patient has muscle weakness and respiratory depression. Administer 20-30 mEq/L of potassium phosphate with maintenance fluids
bicarbonate
only used to correct acidosis if pH is < 7, and the patient is hypotensive despite fluid therapy.
- BG monitoring every 1-2 hours
- when glucose is <250 mg/dL, reduce IV infusion rate and add dextrose to maintenance fluids
how to manage hypoglycemia during the treatment of DKA or HHS?
- K+ monitoring every 4 hours
- add potassium replacement to maintenance fluids
how to manage hypokalemia during the treatment of DKA or HHS?
- monitor renal function daily
- typically resolves with fluid replacement
how to manage AKI during the treatment of DKA or HHS?
- monitor mental status
- rate of fall of osmolality should not be >8 mOsm/kg/d
- Mannitol and mechanical ventilation: treatment of choice
how to manage cerebral edema during the treatment of DKA or HHS?
VTE prophylaxis with LMWH (lovenox)
how to manage thrombosis during the treatment of DKA or HHS?
B. Insulin lispro 8 units/hr IV continuous infusion
FG is a 14-year old 52 kg girl who presents to the ED for confusionand vomiting. The lab values are as follows: HbA1c is 13%, Glucose450 mg/dL, Arterial pH is 7.3, serum potassium level is 4.8 mEq/L,and plasma is positive for ketones. What is the most appropriate treatment for this patient at this time?
A. Insulin glargine 10 units SQ
B. Insulin lispro 8 units/hr IV continuous infusion
C. Insulin regular 5 units IV bolus
D. Potassium chloride 20 mEq IV
E. Sodium bicarbonate 100 mEq IV