Chapter 19: The Kidneys Part 2単語カード | Quizlet
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
What is the juxtaglomerular apparatus?
Contains the Macula Densa: junction of ascending loop of Henle and renal corpuscles
contains juxtaglomerular or granular cells
- afferent arteriole
- produce renin
What are mesangial cells?
smooth muscle cells (modified)
- between and around loops of glomerular capillary
- regulate blood flow by contractile activity
- they contract and alter blood flow through the capillaries
- also secrete cytokines associated w/immune and inflammatory processes
What are the 3 basic process that take place in the nephron?
filtration, reabsorption, secretion
Urine formation
What is the standard glomerular filtration rate or GFR?
for a 70 kg person
180L/24 hours
7.5L/hour
125mL/min
3L of plasma filtered sixty times per day
300 mOsm
Is all of the plasma filtered?
filtration fraction = 20%
is the percentage of total plasma volume that filters into the tubule
After filtrate leaves Bowman's capsule, what happens?
it is modified by reabsorption and secretion.
What is reabsorption and where does it occur?
process of moving substances in the filtrate from the lumen of the tubule back into the blood flowing through the peritubular capillaries
filtrate to blood
- only reabsorbs good material
occurs in the Proximal tubule, loop of henle, and distal convoluted tubule
What is secretion and where does it occur?
selectively moves molecules from the blood and adds them to the filtrate in the tubule lumen
Blood to filtrate
occurs ONLY in the distal convoluted tubule
Amount excreted equation
Amt excreted = amt filtered - amt reabsorbed + amt secreted
E = F-R+S
amounts vary w/physiological control
What does it mean when excretion>filtration?
glomerular filtration and tubular secretion
NO reabsorption
What does it mean when excretion
glomerular filtration and some tubular reabsorption
- no secretion
What does it mean when excretion = 0?
glomerular filtration and total tubular reabsorption
NO secretion
How do you calculate filtration of a solute?
filtration of solute = [solute] in plasma x GFR
What is the glomerular filtration rate?
amount of plasma filtered per time
70 kg person -
180 L/24 hrs or 7.5 L/hr or 125 mL/min
3 L of plasma filtered 60 times per day
Where does most reabsorption occur?
in the proximal tubule
What are mechanisms by which reabsorption occurs?
1. Paracellular pathway
2. Epithelial transport
- Na active transport
- 1 and 2 prime active transport symport w/Na
3. Urea passive reabsorption
4. Plasma protein endocytosis
How does reabsorption occur via paracellular pathway?
by using electrochemical gradients
Na and K flow opposite
water follows Na
How does reabsorption occur via epithelial transport?
1⁰ & 2⁰ active transport
Lumen to cell: apical cell surface
- SGLT: Na+-glucose transporter
Cell to interstitial fluid: basolateral cell surface
- GLUT: glucose transporter
- Na+/K+ ATPase
How does reabsorption occur via urea passive reabsorption?
diffusion following [urea] conc. gradient
How does reabsorption occur via plasma protein endocytosis?
only small proteins should enter filtrate and are reabsorbed by endocytosis
Glucose transport maximum
The proximal tubule can only reabsorb a limited amount of glucose (~375 mg/min)

Renal threshold for glucose
When the blood glucose level exceeds about 160-180 mg/dL, the proximal tubule becomes overwhelmed and begins to excrete glucose in the urine
Reabsorption: What are 2 key factors of transport maximum for Glucose?
1. renal threshold
2. saturation of transporters
What is saturation of transporters?
refers the max rate of transport that occurs when all available carriers are occupied by substrate
# solutes vs # of transporters and speed of transport

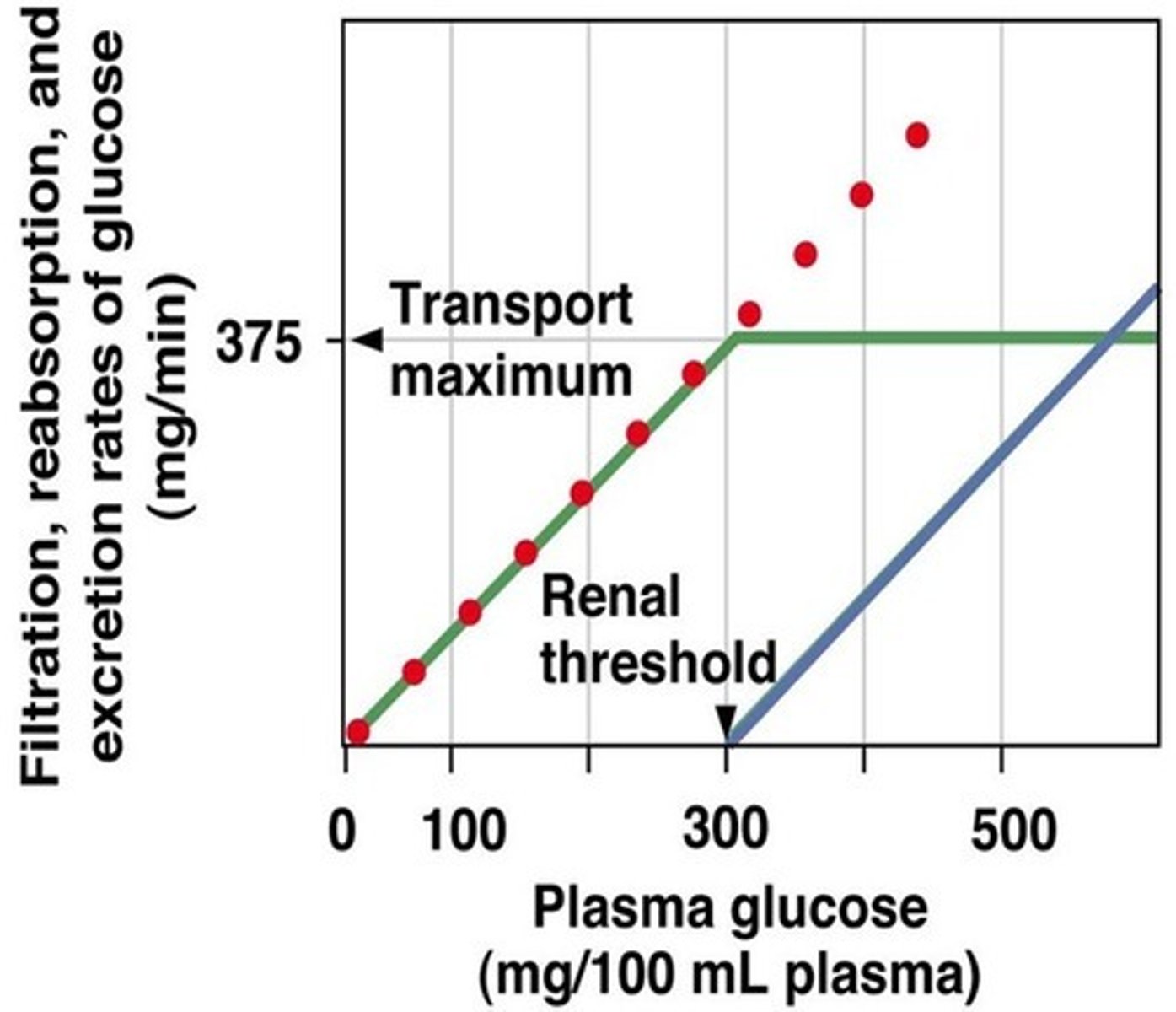
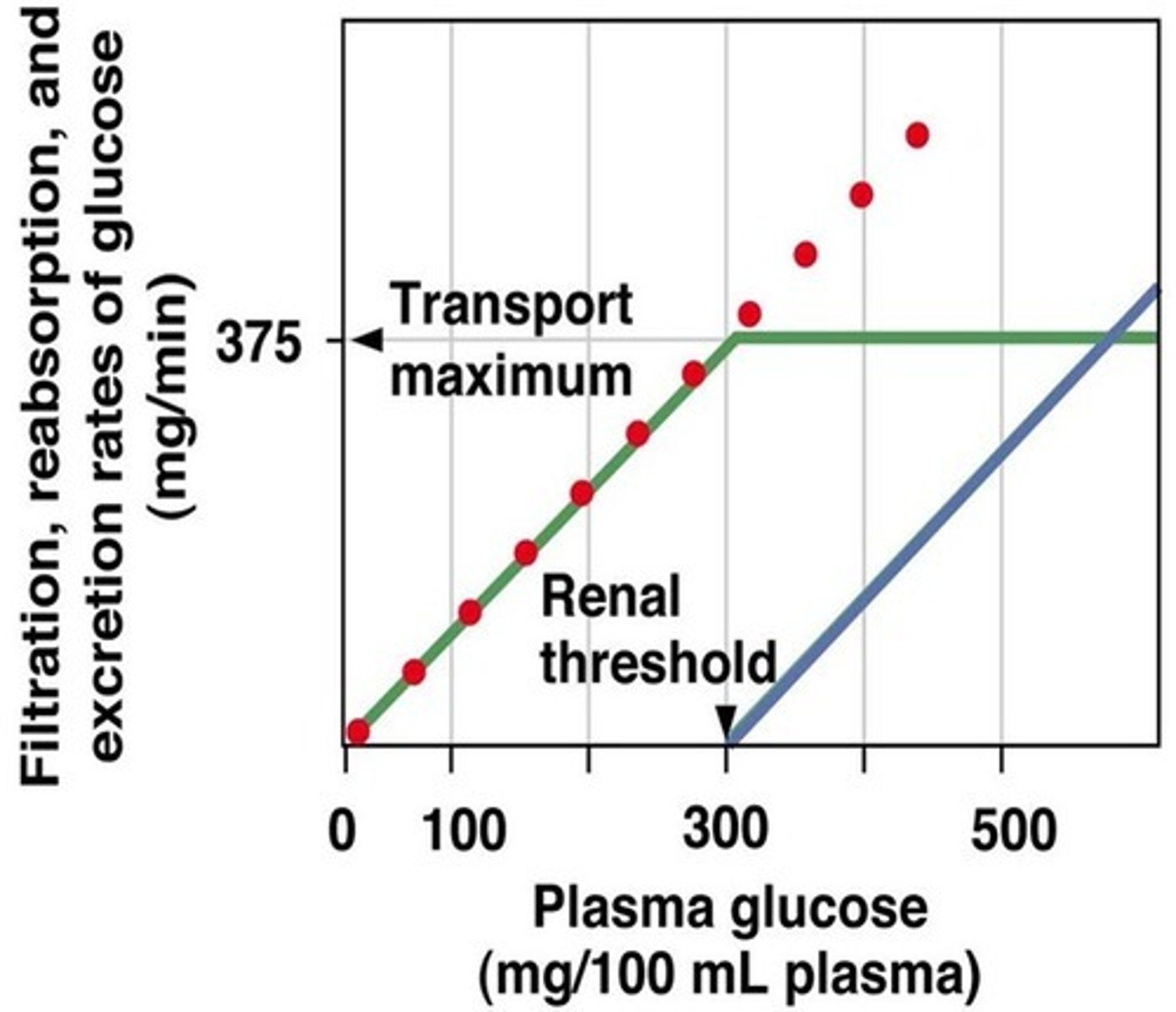
What is the renal threshold?
↑ [solute] → no further ↑ in transport & reabsorption
solute excreted
300
![<p>↑ [solute] → no further ↑ in transport & reabsorption</p><p>solute excreted</p><p>300</p>](https://knowt-user-attachments.s3.amazonaws.com/eb468b6a-5f98-4698-a5e2-886918954e53.jpg)
What is the relationship between filtration and GFR?
Glucose
direct relationship
↑ [glucose] → ↑ GFR of glucose
the more there is, the more you filter
![<p>direct relationship</p><p>↑ [glucose] → ↑ GFR of glucose</p><p>the more there is, the more you filter</p>](https://knowt-user-attachments.s3.amazonaws.com/277f8737-8c2e-4ea7-bda2-d60cb04b8c30.jpg)
What is the relationship of reabsorption to Tmax (transport maximum)?
Glucose
Tmax is at 375 mg/min
Below Transport maximum:
↑ [glucose] → ↑ reabsorption rate
- if you have high [glucose] but you are below transport max, then you will have reabsorption
Above Transport max:
↑ [glucose] → constant reabsorption rate
- if you have high [glucose] but you have reached transport max, then you have constant reabsorption rate (you are saturated on transporters)
![<p>Below Transport maximum:</p><p>↑ [glucose] → ↑ reabsorption rate</p><p>- if you have high [glucose] but you are below transport max, then you will have reabsorption</p><p>Above Transport max:</p><p>↑ [glucose] → constant reabsorption rate</p><p>- if you have high [glucose] but you have reached transport max, then you have constant reabsorption rate (you are saturated on transporters)</p>](https://knowt-user-attachments.s3.amazonaws.com/e9eebad6-7777-49e0-999d-9e3279941be1.jpg)
How is excretion related to Tmax (transport maximum)?
Glucose
renal threshold: 300 plasma glucose
Below renal threshold: glucose is reabsorbed!
↑ [glucose] → no excretion of glucose
Above renal threshold: glucose is NO LONGER reabsorbed! It reached threshold. It stays in filtrate.
↑ [glucose] → ↑ excretion of glucose
- Glucosuria
↑↑ [glucose] in blood → diabetes mellitus
Faulty glucose transporters → genetic
![<p>Below renal threshold: glucose is reabsorbed!</p><p>↑ [glucose] → no excretion of glucose</p><p>Above renal threshold: glucose is NO LONGER reabsorbed! It reached threshold. It stays in filtrate.</p><p>↑ [glucose] → ↑ excretion of glucose</p><p>- Glucosuria</p><p>↑↑ [glucose] in blood → diabetes mellitus</p><p>Faulty glucose transporters → genetic</p>](https://knowt-user-attachments.s3.amazonaws.com/54544562-f564-40c8-a4b1-e09e6ce011c1.jpg)
Summary of filtration, reabsorption and excretion of glucose
filter glucose at all plasma conc.
reabsorb glucose up to renal threshold
excrete glucose above renal threshold
What is passive reabsorption into capillaries?
follow [solute] gradients
net filtration favors reabsorption!
PC - peritubular capillary hydrostatic pressure (filtration), 10 mm Hg
πC - capillary colloid osmotic pressure (absorption), 30 mm Hg
NFP = PC - πC
10 - 30
NFP: 20
What is secretion?
addition of solute to filtrate
moves against its conc. gradient
Interstitial fluid to cell: basolateral cell surface
- Active transport: Primary, secondary and tertiary active transport
Cell to lumen: apical cell surface
- Facilitated diffusion
Where does most secretion occur?
proximal tubules
What is renal clearance?
clearance of a substance = mass of substance excreted per time/plasma [substance] conc.
volume of plasma from which substance is removed per unit time
- proportion of substance removed from the plasma
So how well someone filters out a substance
What is the renal clearance equation?
Cs = Us x V/Ps
Cs = clearance of S
Us = urine conc. of S
V = urine vol. per unit time
Ps = plasma conc. of S
UsV = amt in the urine
ex: Cs = 5 L/hr
The substance is removed from 5L of plasma in 1 hour
What is inulin?
a polysaccharide not normally found in the body
What does inulin clearance = ?
inulin clearance = GFR
- inulin is filtered, but not reabsorbed or secreted
What can inulin be used to do?
be used to monitor glomerular filtration rate
- give inulin intravenously to maintain Pin (Plasma concentration of Inulin)
PIN = 4 mg/L
UIN= 300 mg/L
V = 0.1 L/hr
CIN = ?
CIN = (300 mg/L * 0.1 L/hr) / 4 mg/L
CIN = 30 mg/hr / 4 mg/L
CIN = 7.5 L/hr
7.5 L of plasma is cleared of inulin in 1 hour (CIN = GFR)
Can creatinine be used as a viable alternative to inulin?
yes. constant production: constant plasma conc.
but a small amount is secreted.
meaning that clearance would be higher because it is secreted (added to the filrate)
With inulin, clearance = GFR...what does that mean?
no reabsorption, no secretion
With glucose, clearance = 0, what does that mean?
total reabsorption
With urea, clearance < GFR, what does that mean?
about 50% is reabsorbed
reabsorption
clearance is lower than GFR
With penicillin, clearance > GFR, what does that mean?
secretion
clearance is higher than GFR
What is micturition?
urination
Detrusor muscle (bladder): normal state is relaxed in order to fill
Sympathetic system inhibits contraction - keeps it relaxed
smooth muscle
Internal urethral sphincter: normal state is passively contracted
Sympathetic system
smooth muscle
External urethral sphincter: normal state is tonically contracted
Somatic motor system
skeletal muscle
What is the micturition state?
Urinary bladder and urethra
Stretch reflex: Detrusor stretch receptors
- Integration in the spinal cord (spinal reflex)
1. Parasympathetic stimulation of detrusor muscle
2. Increased pressure will open internal urethral sphincter
3. Inhibition of somatic control of external urethral sphincter
4. Micturition
What is the voluntary control of micturition?
Prevent micturition: learned reflex, conscious control
1. Micturition center in the brainstem and cerebral cortex:
- inhibit parasymp. system and promote sphincter contraction.
2. Continued stimulation of stretch receptors
- can only delay mict. temporarily
- max bladder content = 500-600 ml
- at full capacity or at will, promote micturition
Additional promotion of micturition is done by what?
valsava maneuver
- voluntary contraction of abdominal walls and expiratory muscles
- compression of detrusor muscle stimulates micturition reflex