5. Diseases of the conjunctiva
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
139 Terms
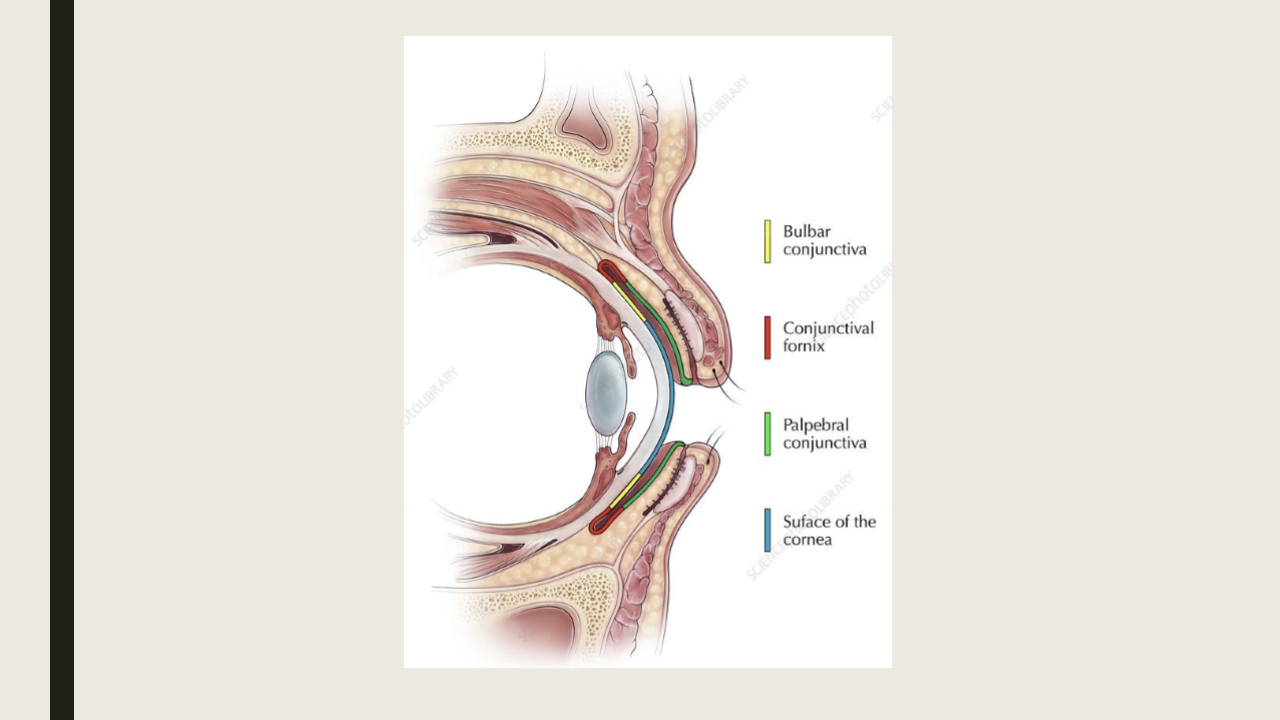
What is the conjunctiva?
The transparent mucus membrane that lines the inner surface of the eyelids and surface of the globe to the limbus.
Why is the conj highly vascularized?
Contains anterior ciliary arteries and palpebral arteries. Also has lymphatic system to drain the preauricular and submandibular lymph nodes.
What are the 3 divisions of the conj?
Palpebral: starts at MCJ and attaches to posterior tarsal plate
Forniceal: loose and redundant conj that folds on itself
Bulbar: covers anterior sclera and is continuous
What are the types of discharged associated with conj infection/inflammation.
Watery: composed of serous exudate and tears seen with viral or allergic conjunctivitis
Mucoid: stringy or ropy seen wit chronic allergic conjunctivitis or dry eye
Purulent: associated with eyes stuck shut in the morning
Mucopurulent: chlalmydial or acute bacterial conjunctivitis
Moderately purulent: acute bacterial conjunctivitis
Severe purulent: Gonococcal conjunctivitis
What are the three main conjunctival tissue reactions?
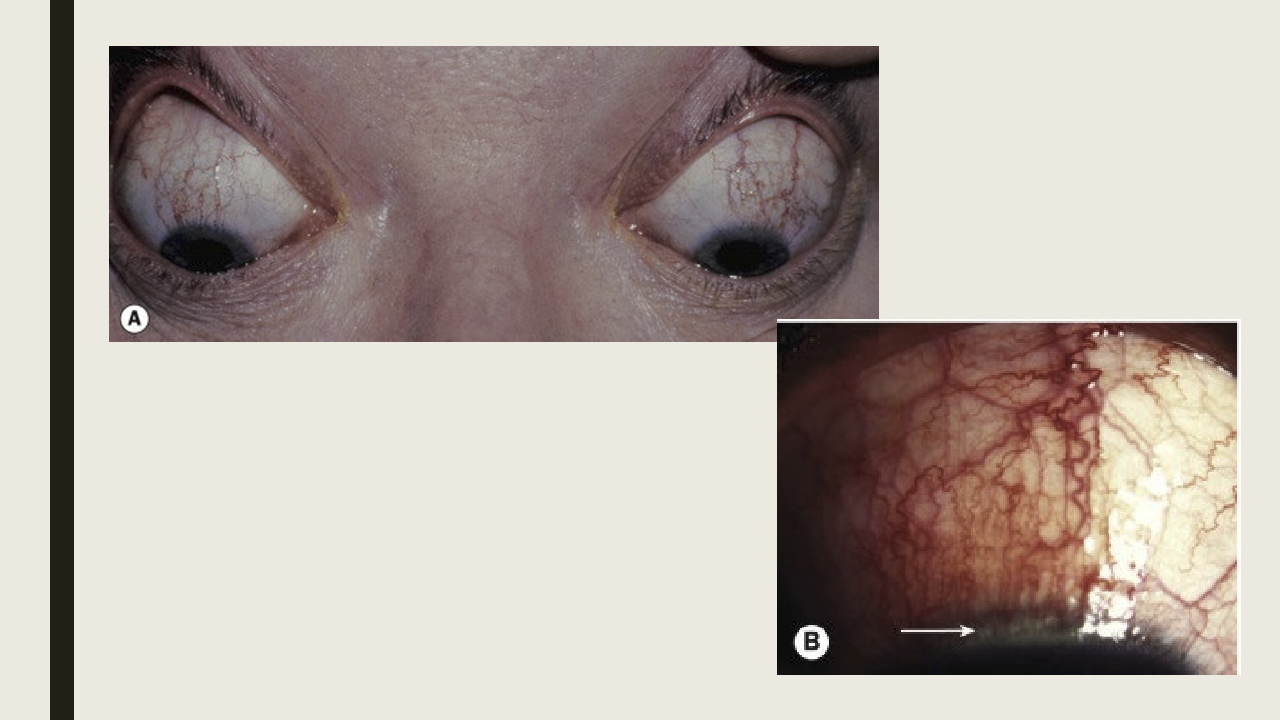
Hyperemia/injection: redness of the conjunctiva
Hemorrhage: area of bleeding seen with viral and occasionally bacterial conjunctivitis
Chemosis: area of conj swelling: acute represents hypersensitivity while chronic is associated with orbital outflow constriction

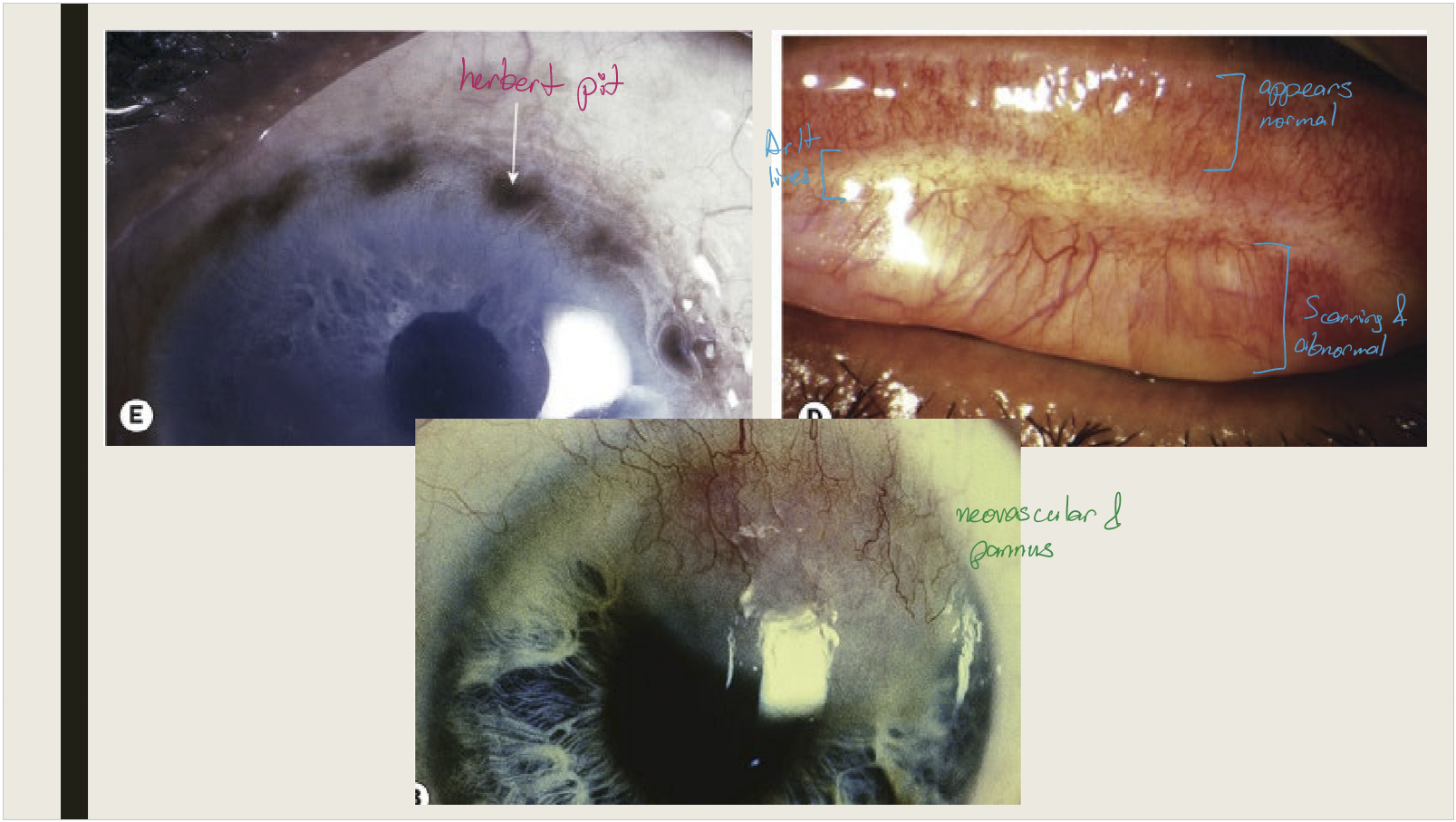
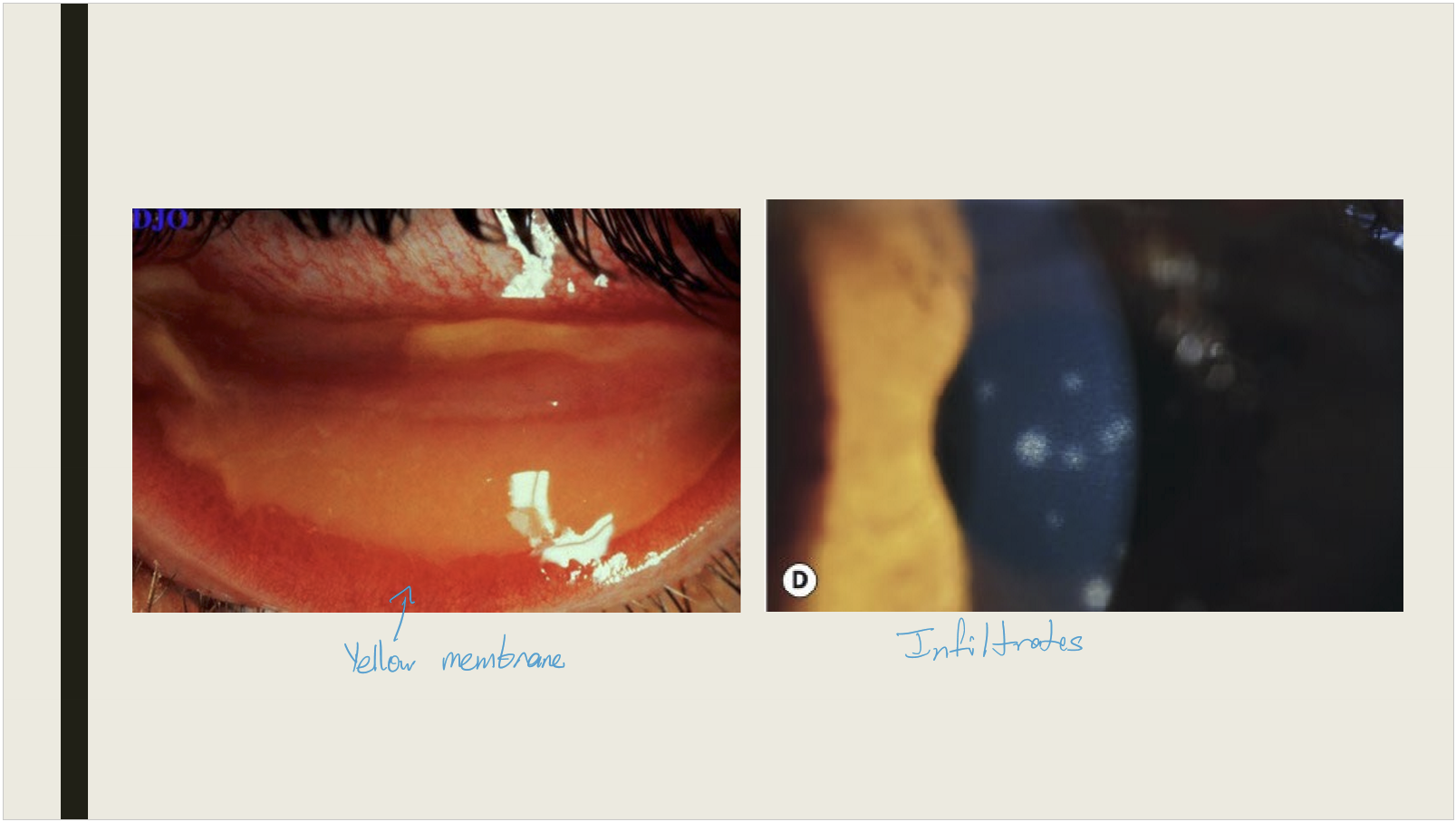
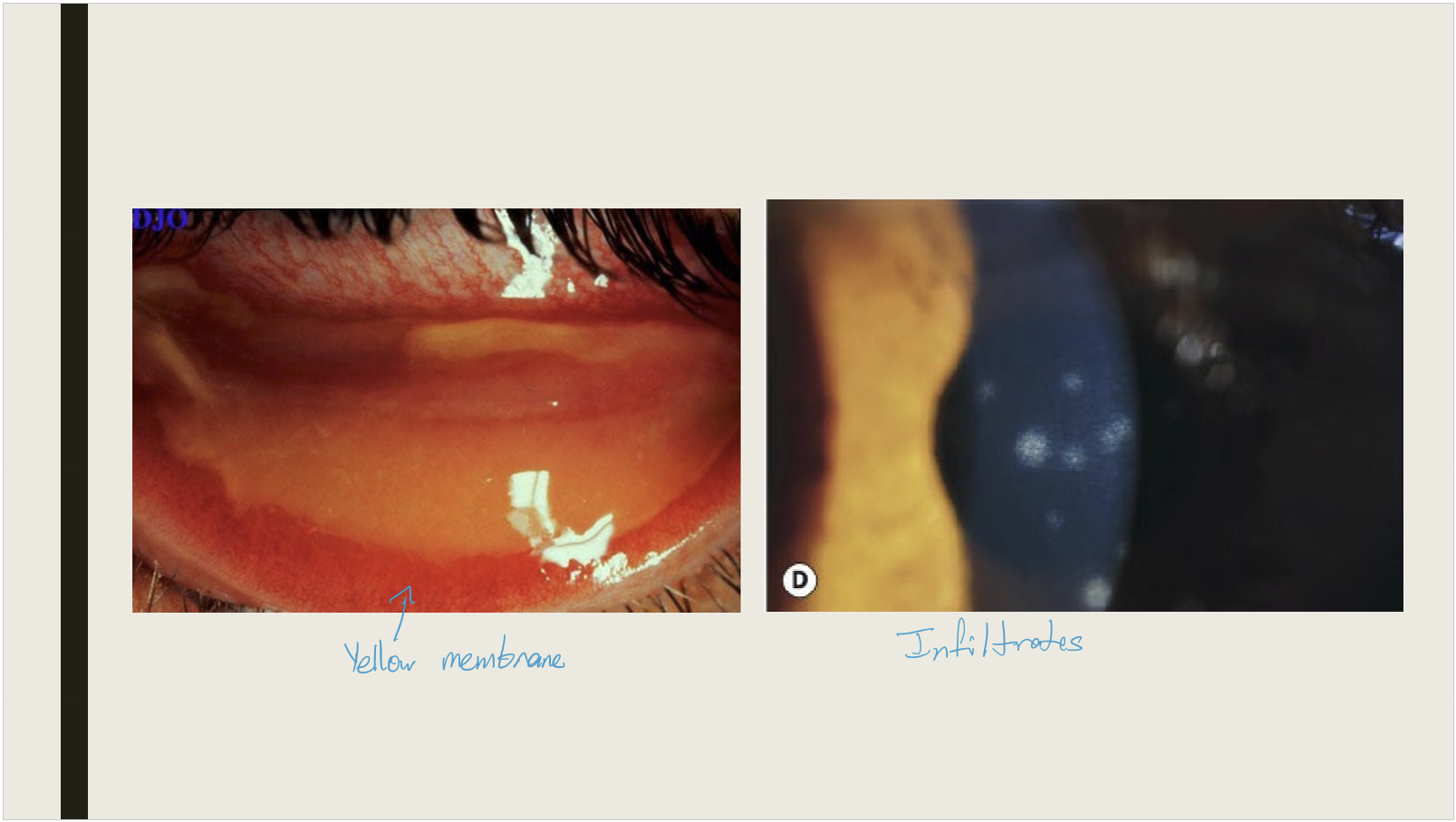
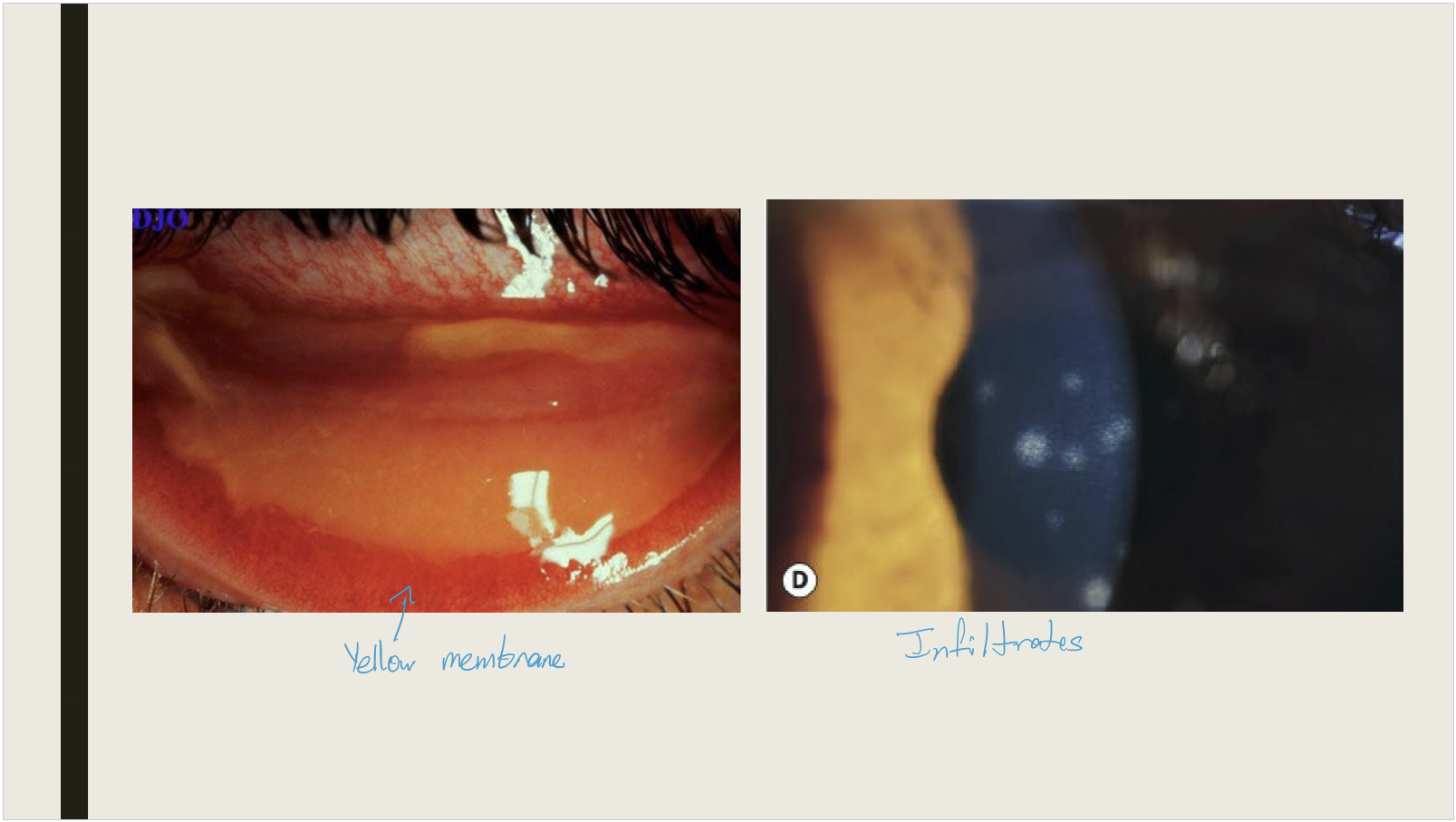
What membranes can form on the conjunctiva?
Pseudomembrane: coagulated exudate that adheres to the inflamed conj epithelium. Can peel without bleeding
Membrane: coagulated exudate that adheres to the inflamed conj. Contains more fibrin and blood vessels. Bleeding will occur if pull membrane away.
What are key conjunctival reactions associated with chronic inflammation and scarring?
Infiltration:
Linked to chronic inflammation and papillary response
Loss of conjunctival detail
Commonly affects the superior tarsal plate
Subconjunctival Scarring:
Frequently seen in trachoma
Severe scarring leads to loss of goblet cells and accessory lacrimal glands
Can result in entropion (inward turning of the eyelid)
What conditions are commonly associated with conjunctival follicles?
Viral infections
Chlamydial infections
Parinaud oculoglandular syndrome
Hypersensitivity to topical medications
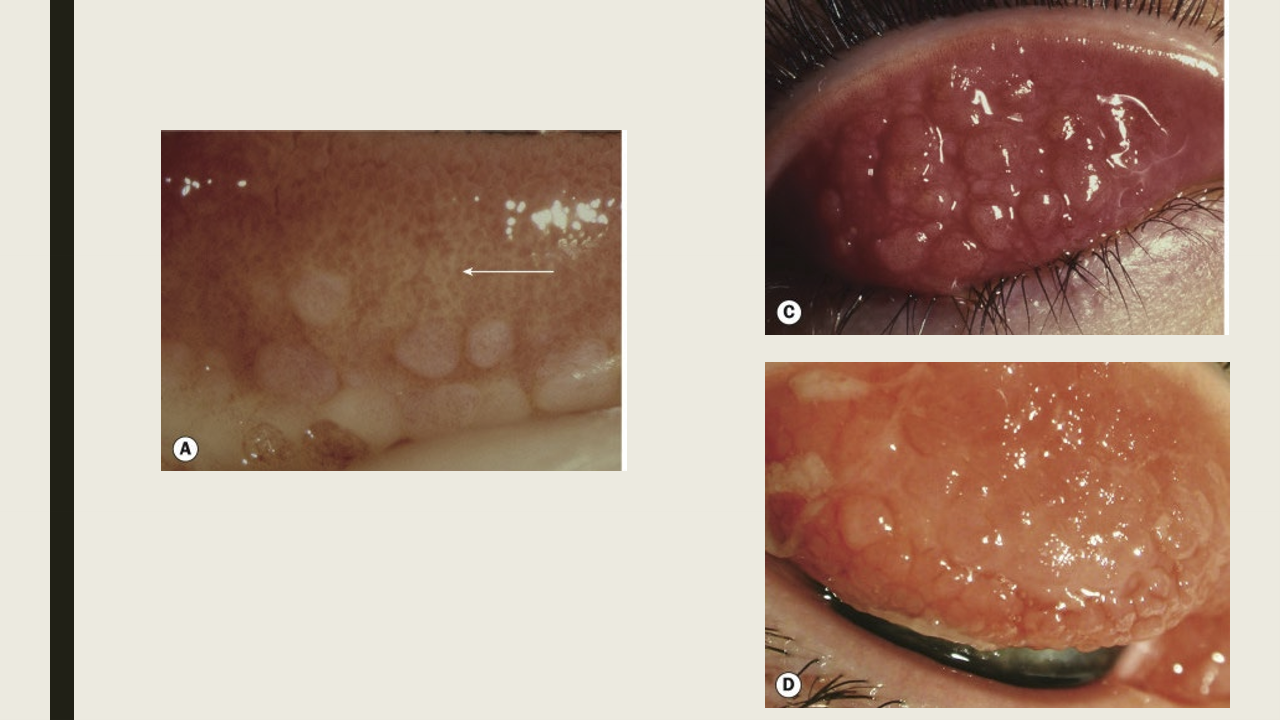
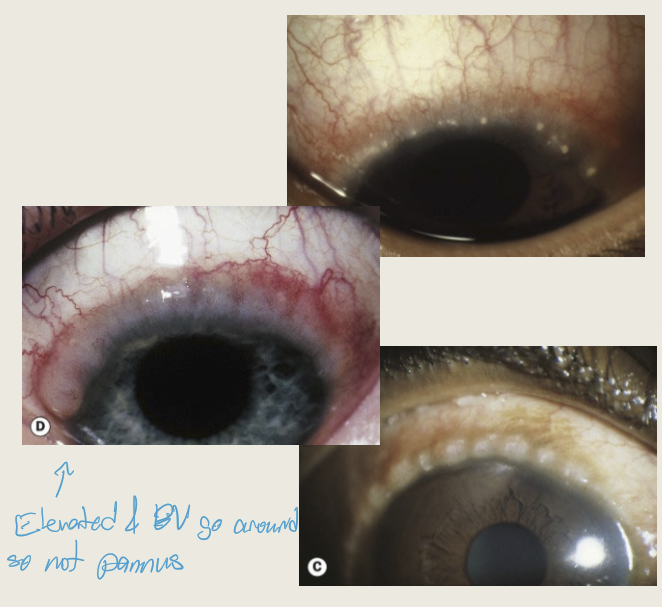
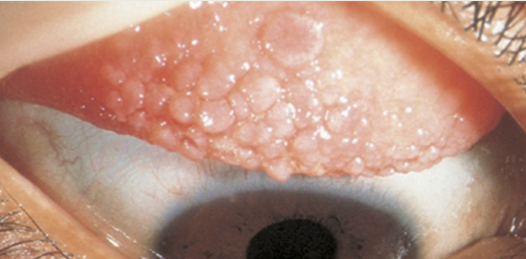
How do conjunctival follicles present?
Translucent lesion resembling a "grain of rice"
Elevated appearance
Blood vessels run around the lesion
Commonly found in the fornices
What conditions are conjunctival papillae commonly seen with?
Bacterial infections
Allergic reactions
Chronic marginal blepharitis
Contact lens wear
Superior limbal keratoconjunctivitis
Floppy eyelid syndrome

What are the presentations of the conjunctival papillae?
May be present on the palpebral or bulbar
They have vascular core
Micropapillae will have mosaic pattern of red dots
Macropapillae (<1mm) and giant papillae (>1mm) develop with chronic inflammation
Limbal papillae will look gelatinous

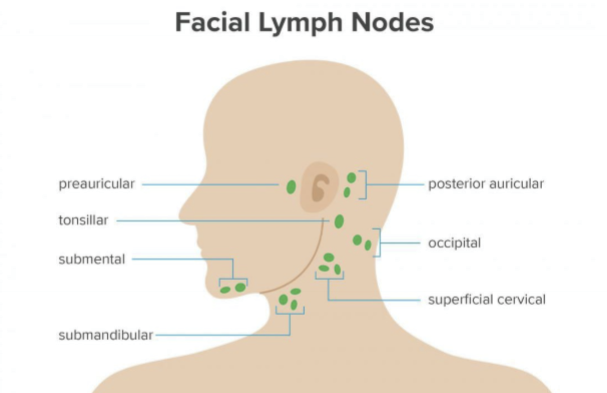
What conditions are commonly associated with conjunctival lymphadenopathy?
Viral infections
Chlamydial infections
Severe bacterial infections
Parinaud oculoglandular syndrome
Which lymph nodes are commonly involved in conjunctival lymphadenopathy?
Preauricular site is commonly affected. Lateral 1/3 of the eye drains into the preauricular lymph node.
Which bacteria commonly cause acute bacterial conjunctivitis?
Streptococcus pneumoniae
Staphylococcus aureus
Haemophilus influenzae
Moraxella catarrhalis
Neisseria gonorrhoeae
Neisseria meningitidis
What are symptoms & presentations of acute bacterial conjunctivitis?
Symptoms: redness, grittiness, burning, and discharge
Presentation: Unilateral and becomes bilateral within 1-2 days. Lid edema and redness, Conj hyperemia, mucuopurulent discharge, PEE, no lymphadenopathy.
What are the treatments for acute bacterial conjuinctivitis?
Culture as needed, to help ID causative agent
Topical antibiotics
Systemic antibiotics: used for gonococcal, H. influenza, and meningococcal
What causes adult chlamydial conjunctivitis?
Chlamydial trachomatis, serological variants D-K.
How is Chlamydial trachomatis transmitted?
Sexually transmitted
Affects 5-20% of sexually active adults (1.8 million cases in US in 2018)
10% of infections will result from eye to eye contact
How does adult chlamydial infections present?
Males may have urethritis= most are asymptomatic. Females may have urethritis which will cause painful urination and progress to pelvic inflammatory disease and can to lead to infertility.
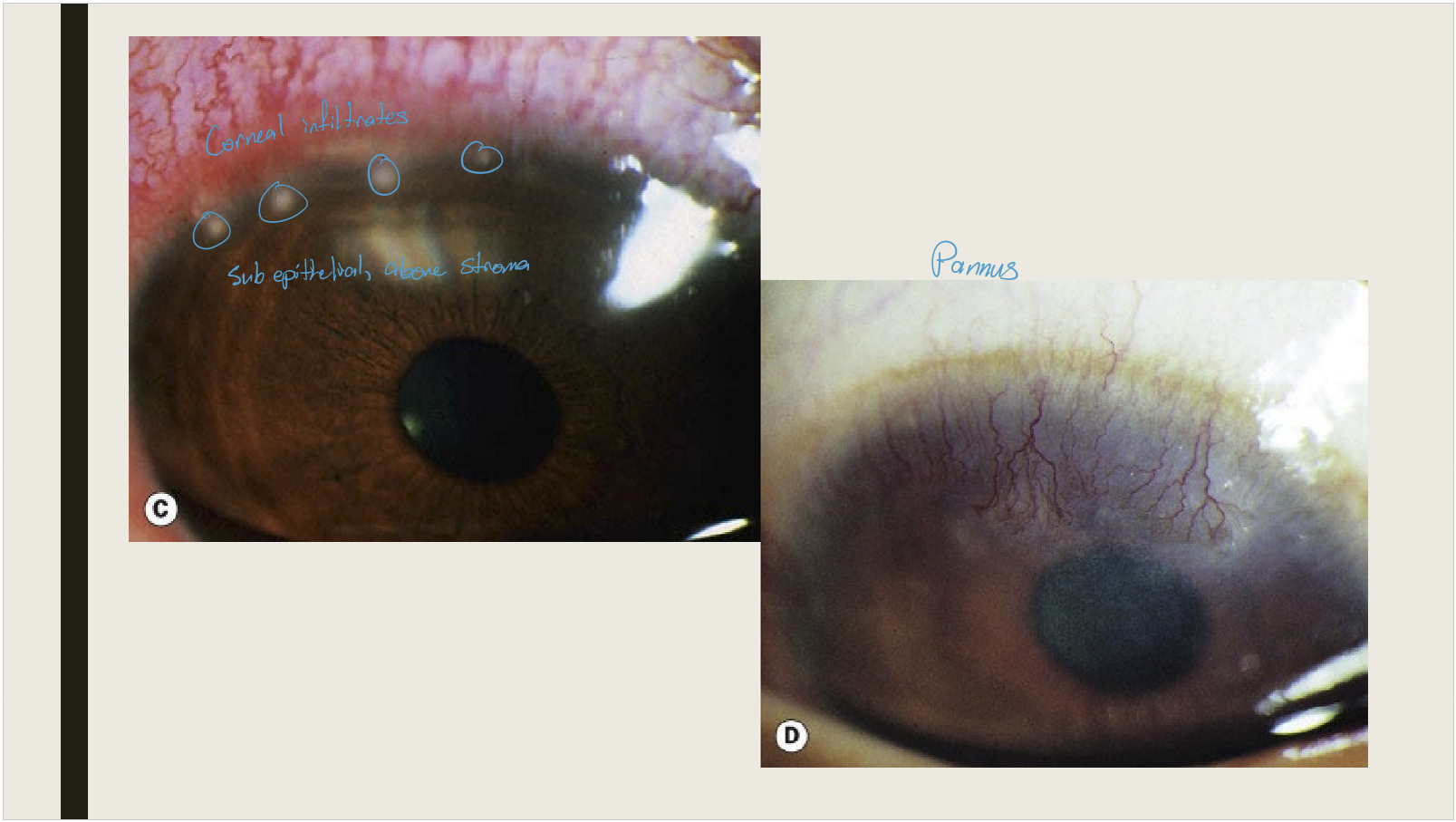
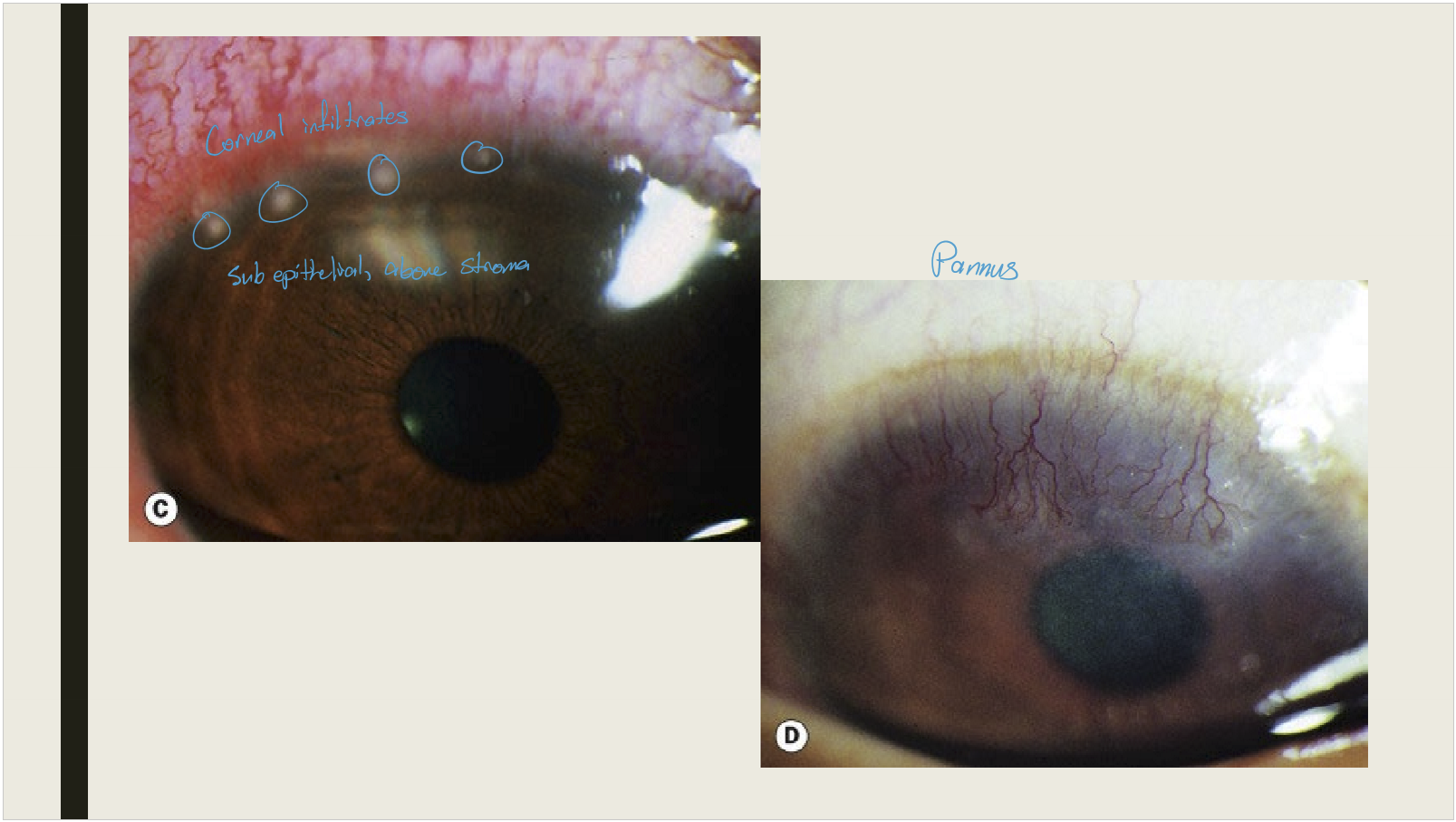
How does Adult chlamydial conjunctivitis present?
Water or mucopurlulent discharge
Large follicles prominent in the inferior fornix or superior tarsal plate
PEE
Peripheral subepithelial corneal inflitrates: may have 2-3 week delay of onset
Tender preauricular lymphadenopathy
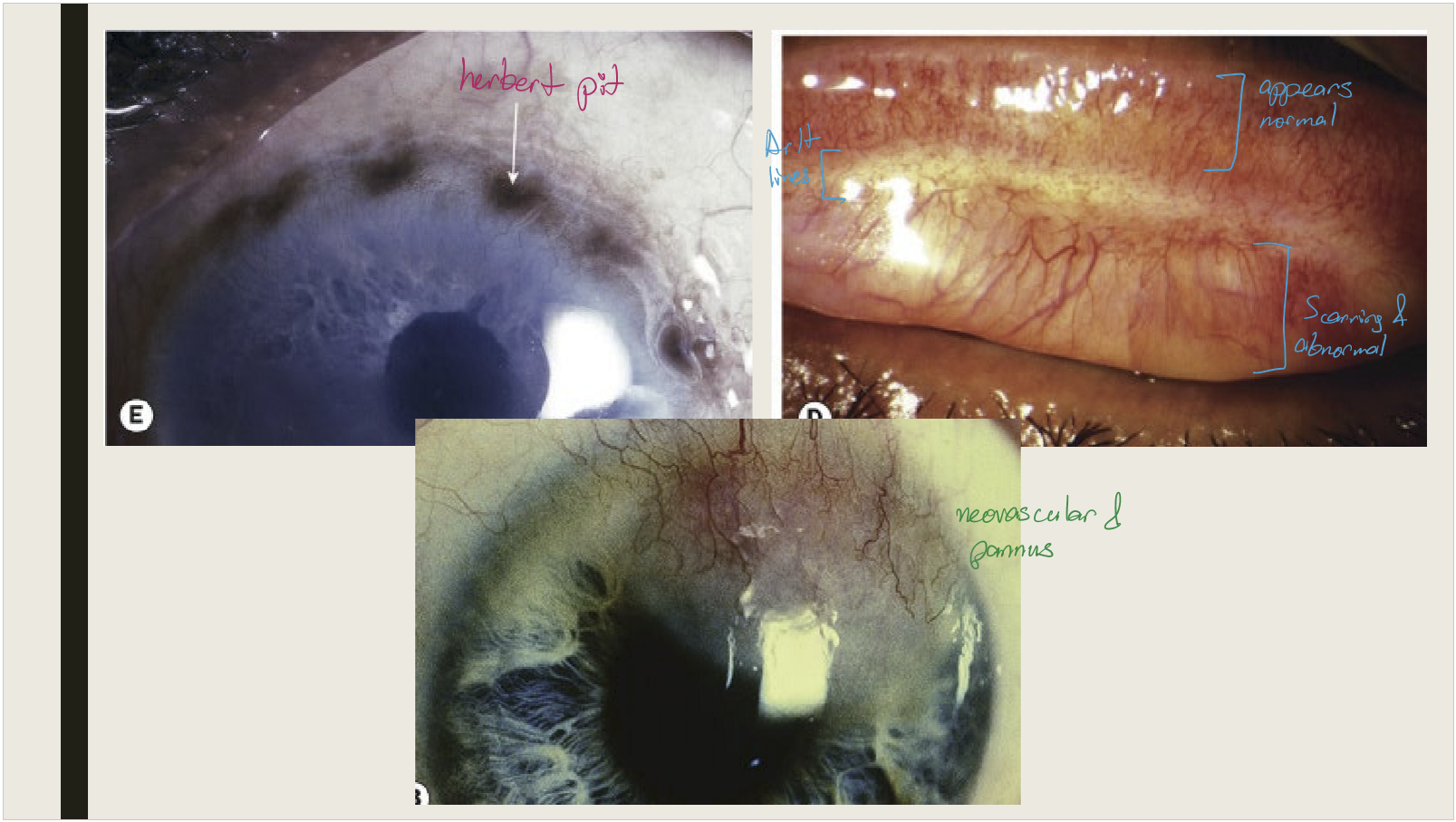
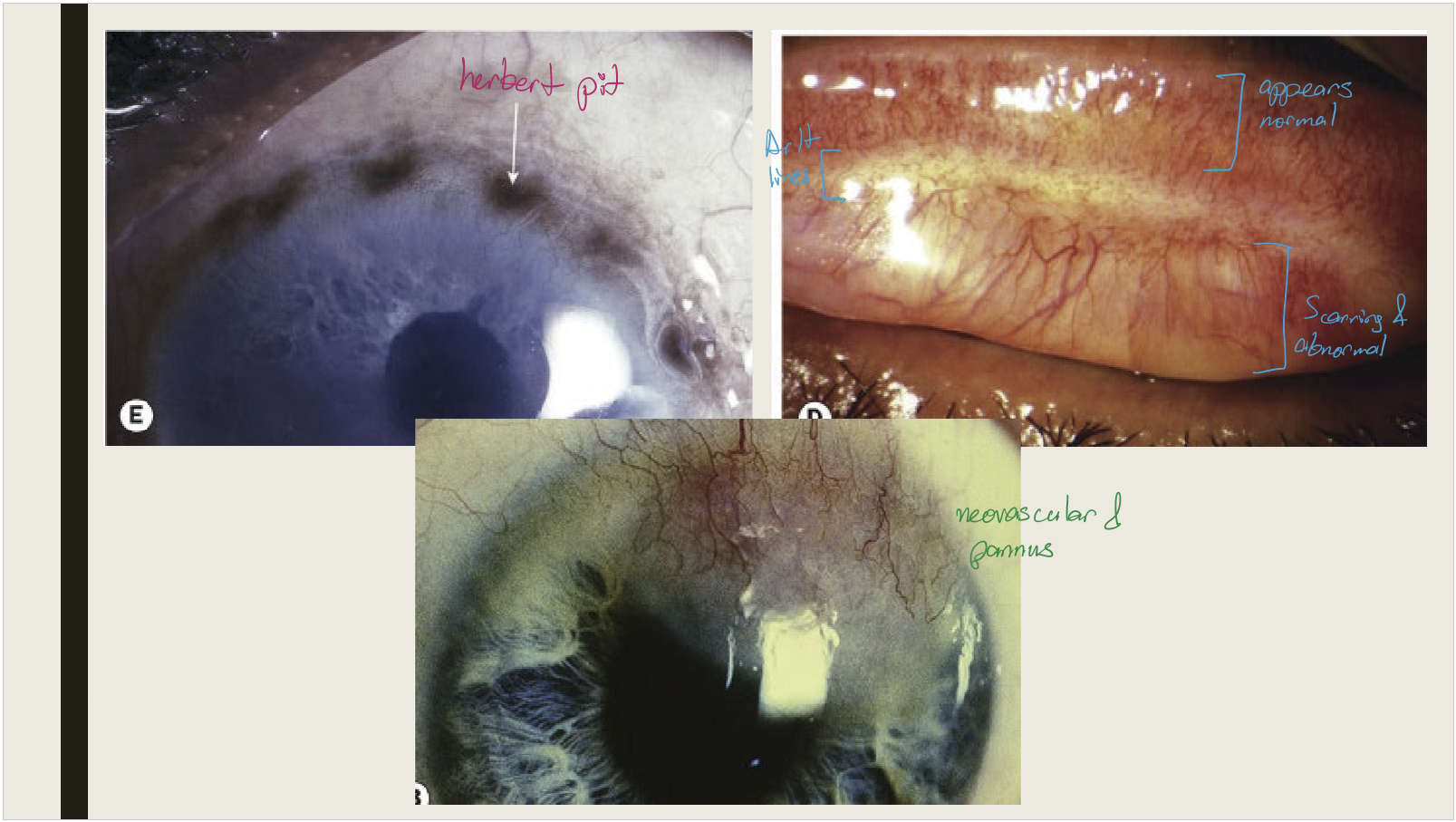
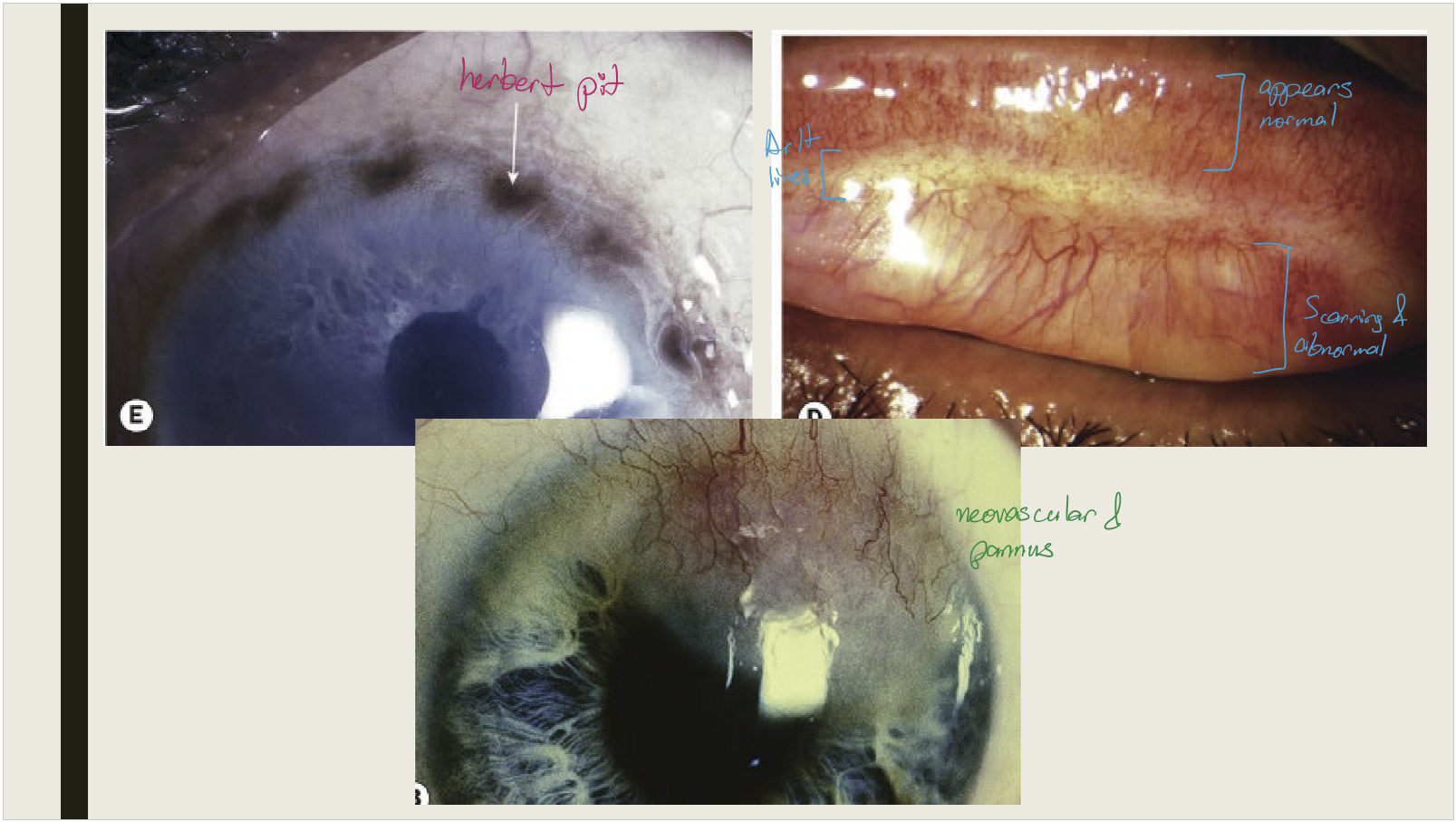
Con scarring and corneal pannus is seen with chronic infections
What are the treatments for Adult chlamydial conjunctivitis?
Culture
Refer to genitourinary specialist
Systemic antibiotics
Topical antibiotics
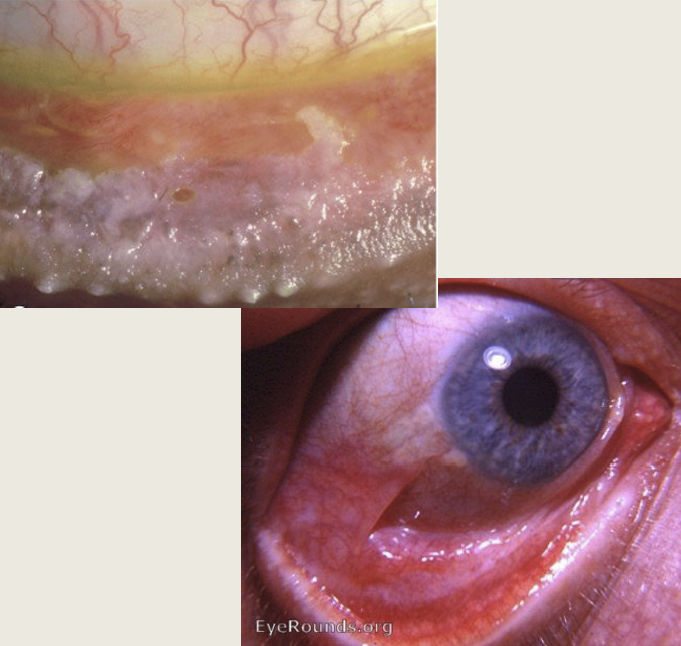
What is Trachoma?
The leading cause of preventable irreversible blindness in the world. Related to poverty, overcrowding, and poor hygiene.
What causes trachoma?
Chlamydial trachomatis serological variants A, B, Ba, C
What stages does trachoma have?
Active and cicatricial trachoma.
What age group is most commonly affected by active trachoma?
Pre-school children
What type of conjunctival reaction is seen in active trachoma?
Mixed papillary + follicular reaction, mucopurulent discharge, superior epithelial keratitis, pannus formation
What conjunctival reaction is absent in children under 2 with active trachoma?
Follicular reaction
In what age group is cicatricial trachoma more common?
Middle-aged individuals
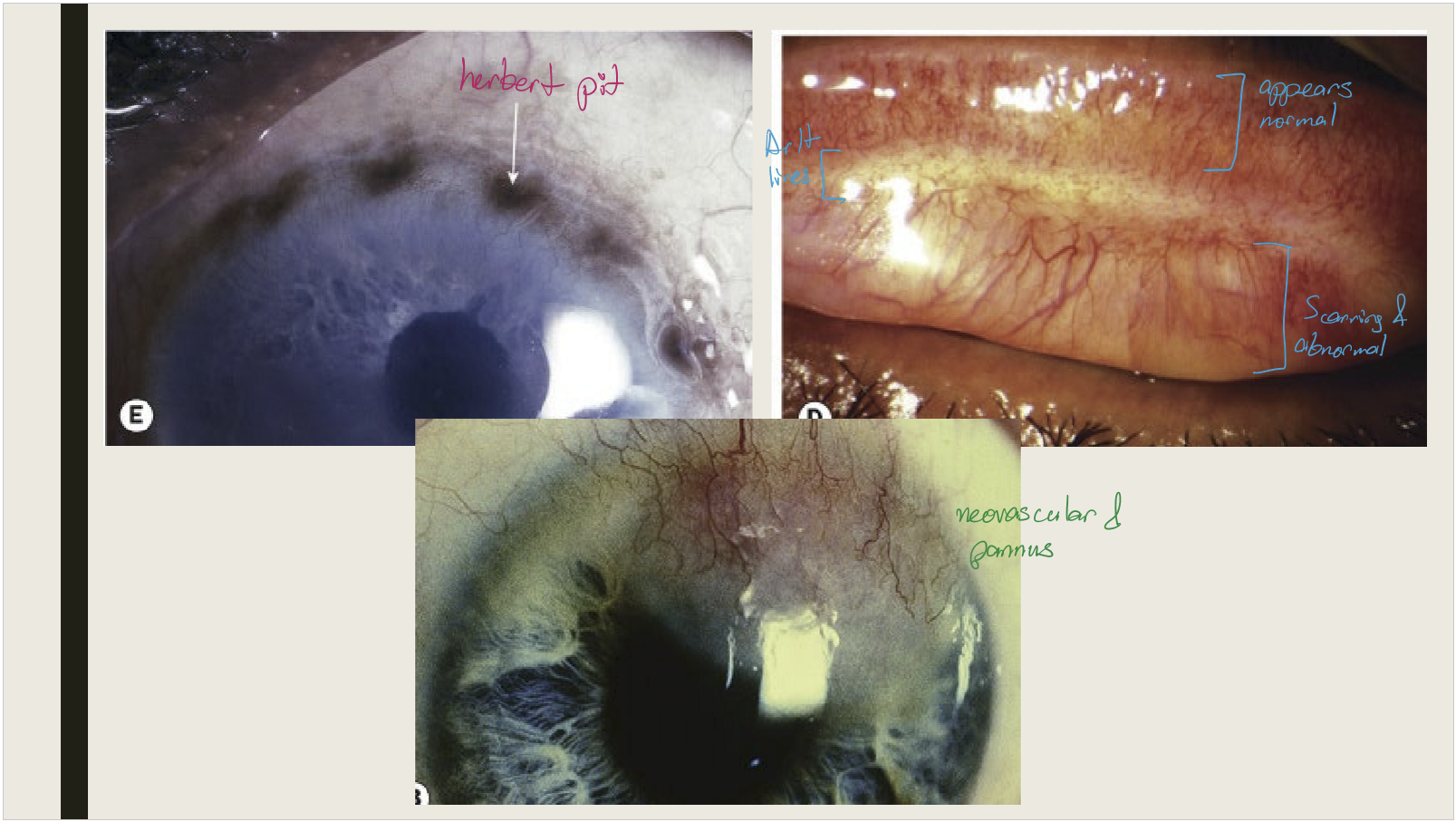
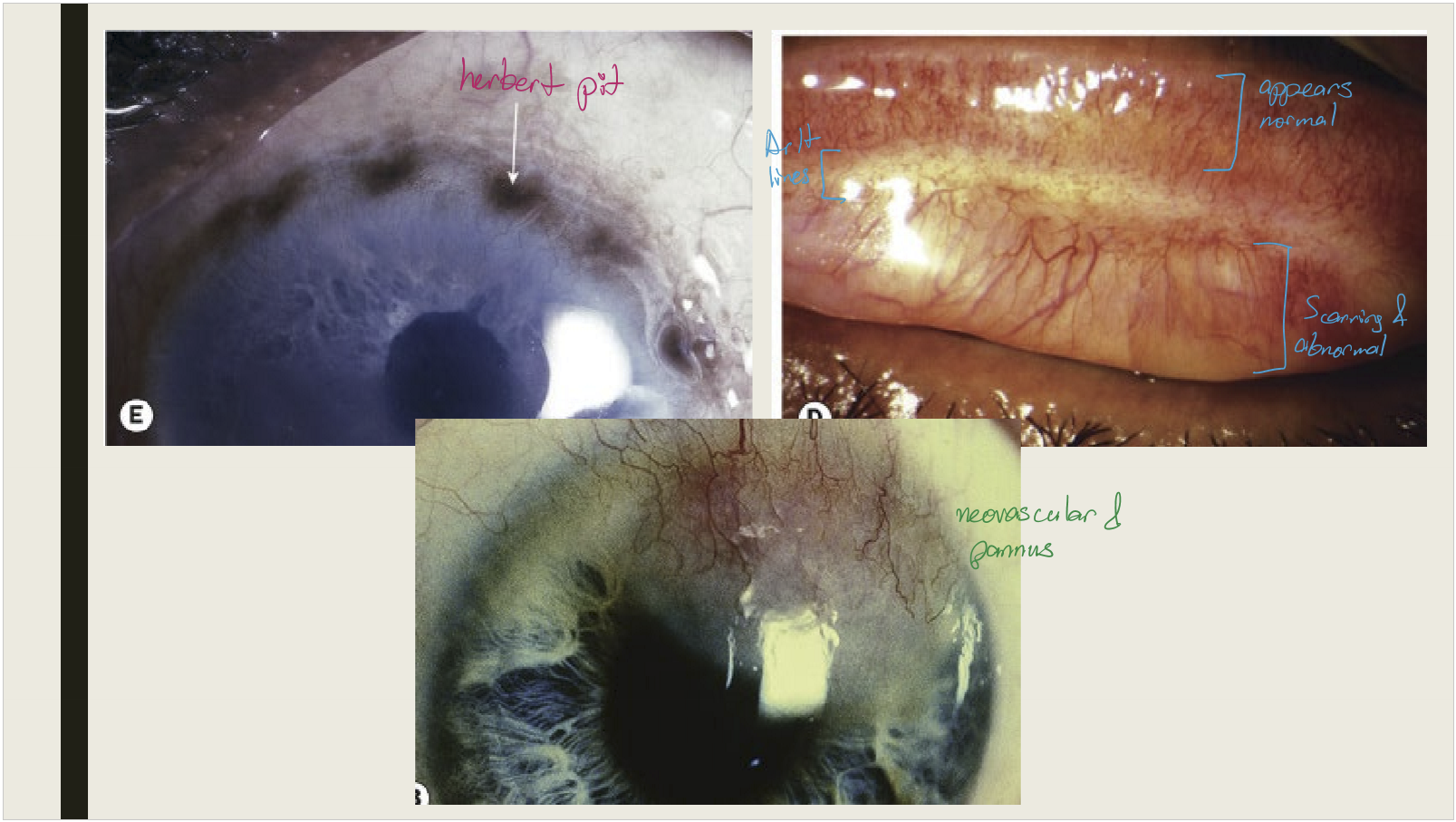
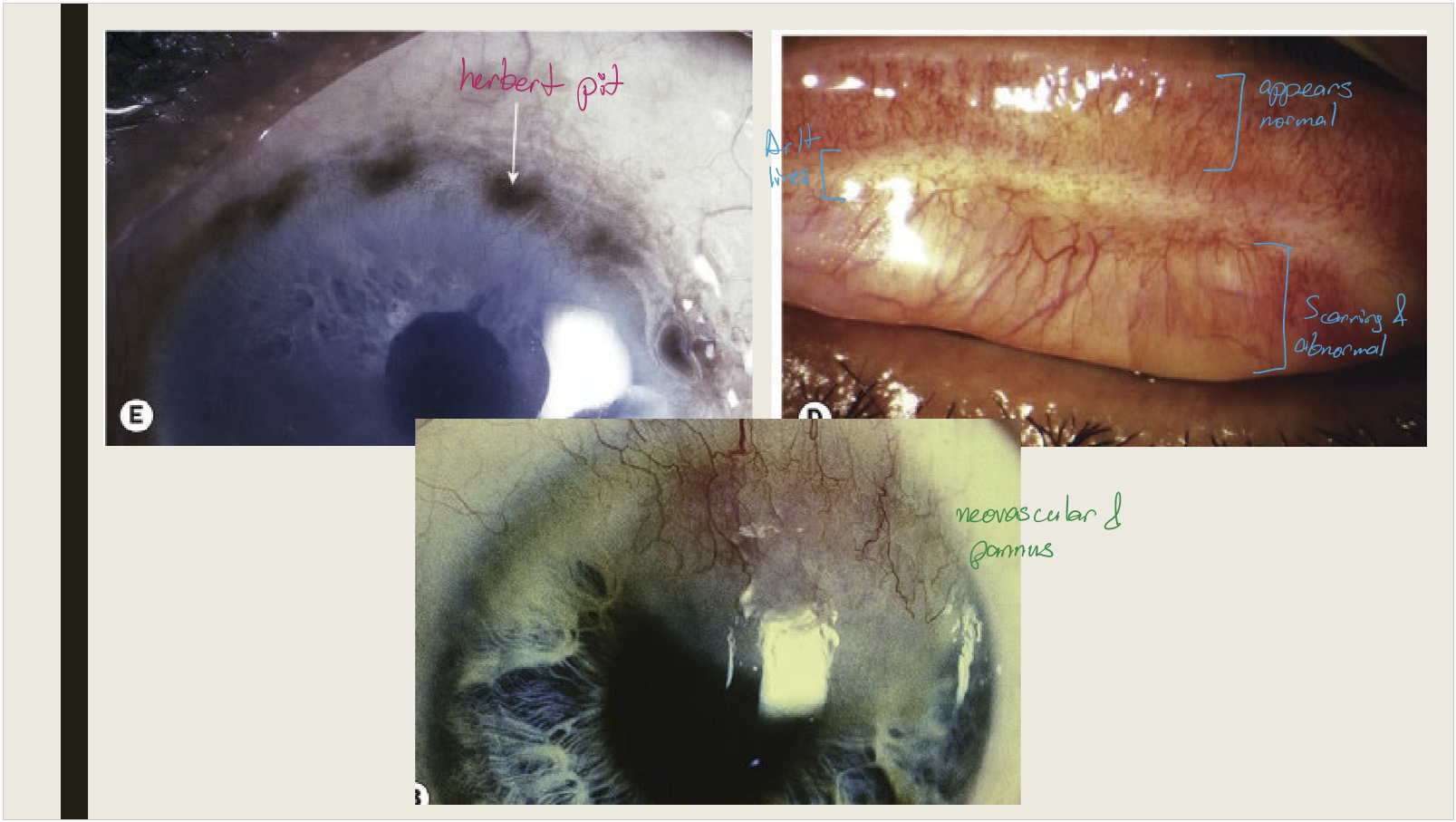
What conjunctival changes occur in cicatricial trachoma?
Conjunctival scarring
Mild infection: linear or stellate scarring
Severe infection: broad confluent scared (Arlt lines)
Superior tarsal effected more then other areas of conjunctiva
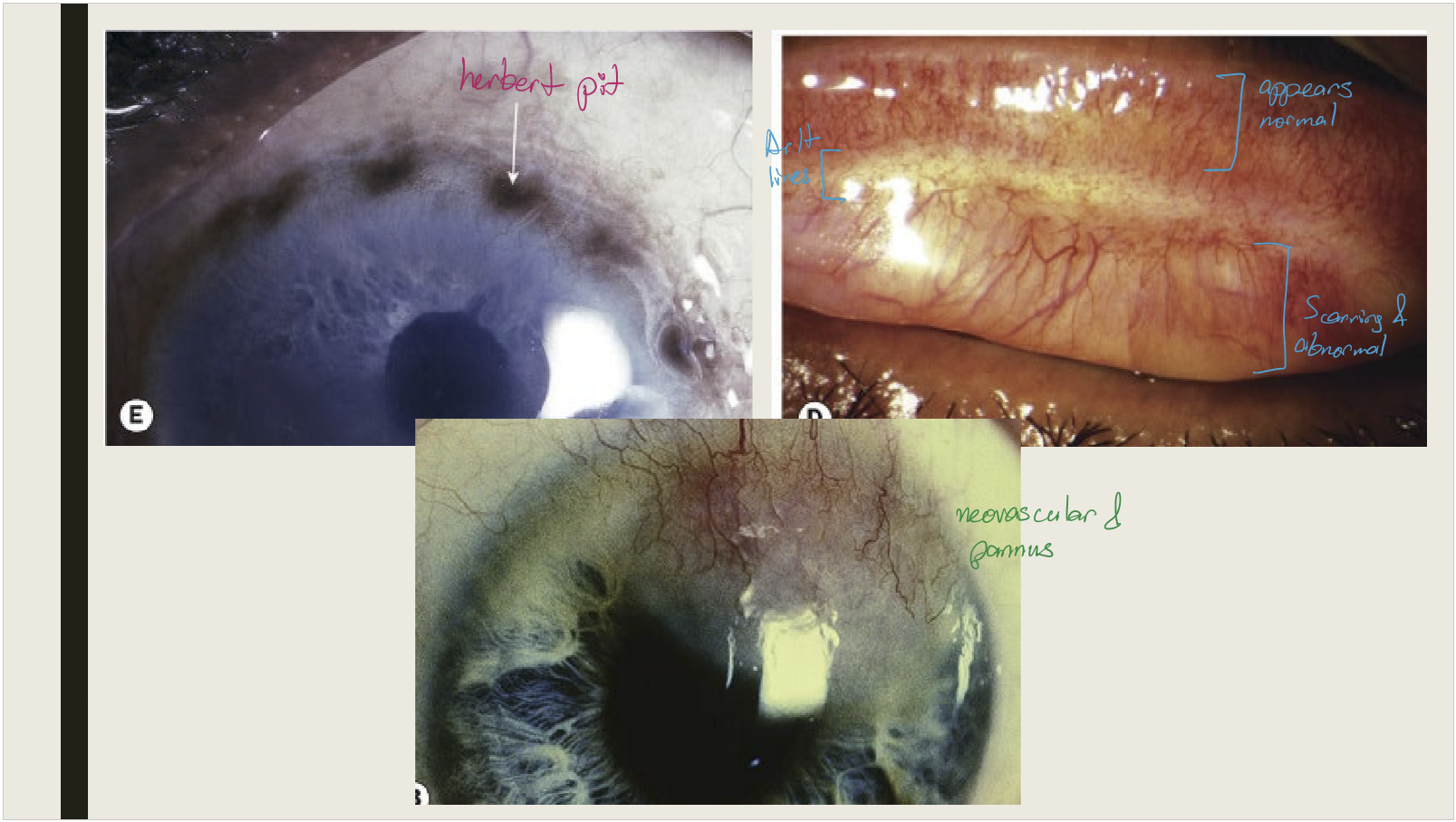
What happens to superior limbal follicles after they resolve in cicatricial trachoma?
They leave shallow pits (Herbert pits)
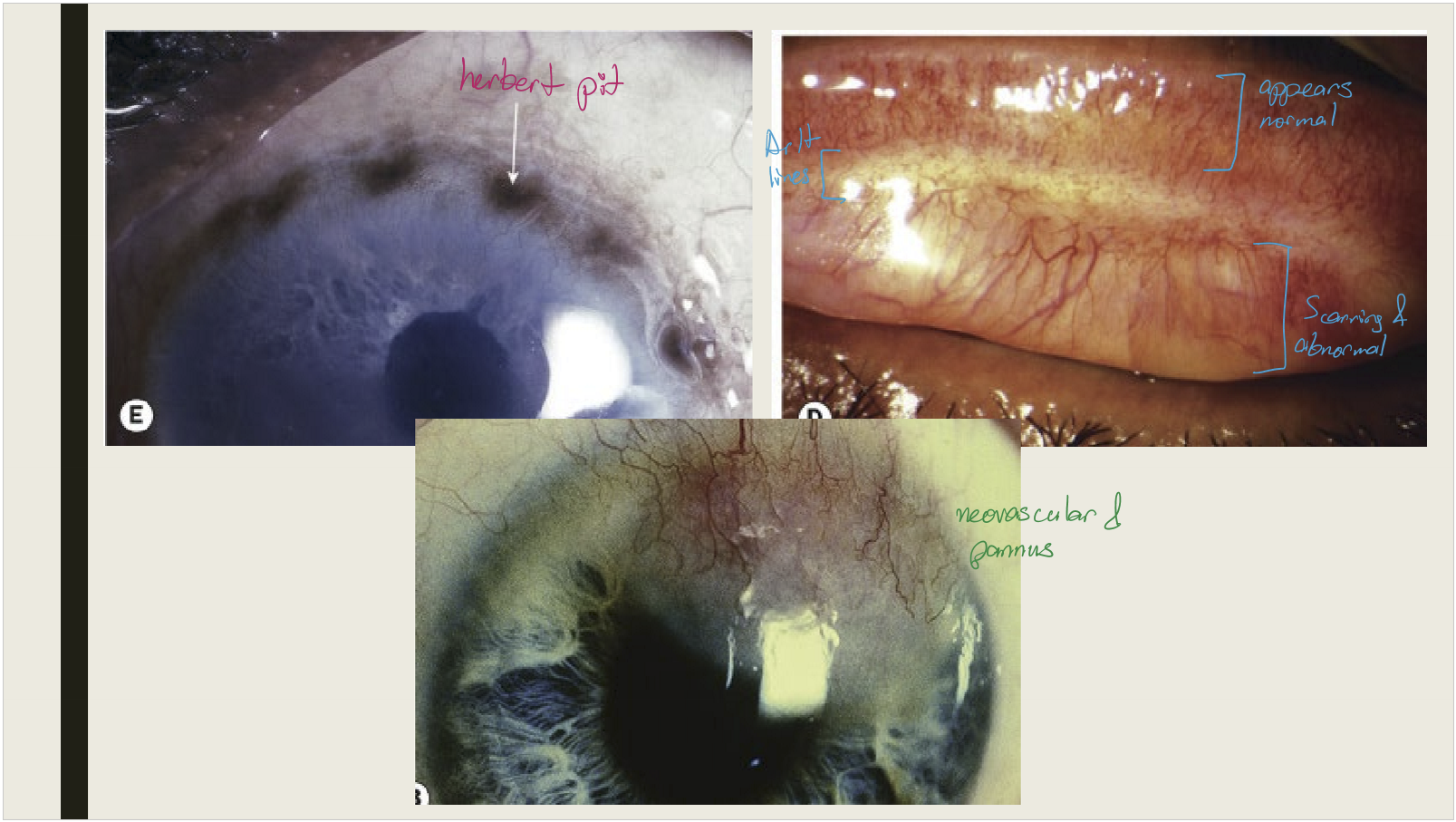
What are the corneal and eyelash changes seen in cicatricial trachoma?
Corneal opacification with vascularization; trichiasis and distichiasis
Why can cicatricial trachoma lead to dry eye?
Goblet cell destruction
How is trachoma treated?
Antibiotics:
Topical for trachomatous inflammation–follicular
Topical + systemic for trachomatous inflammation–intense
Facial cleanliness: all stages
Environmental improvement: clean water & sanitation
Surgery: for trichiasis/entropion (restores lid closure)
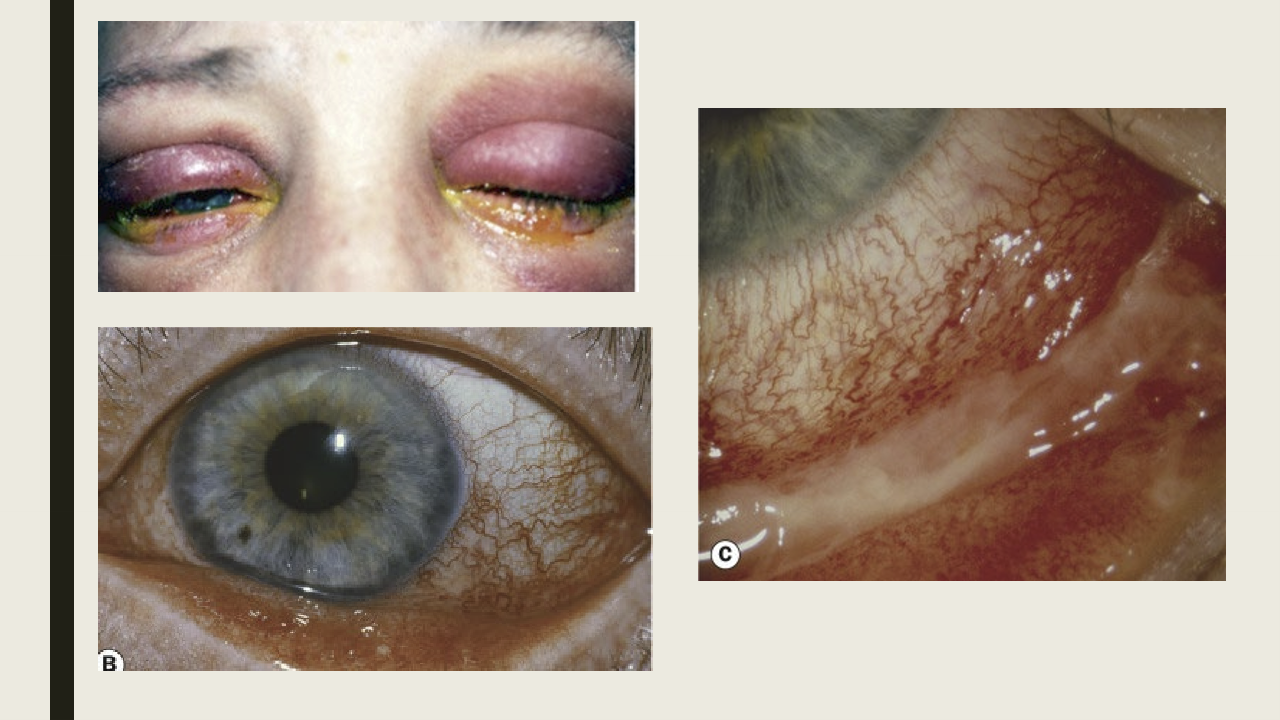
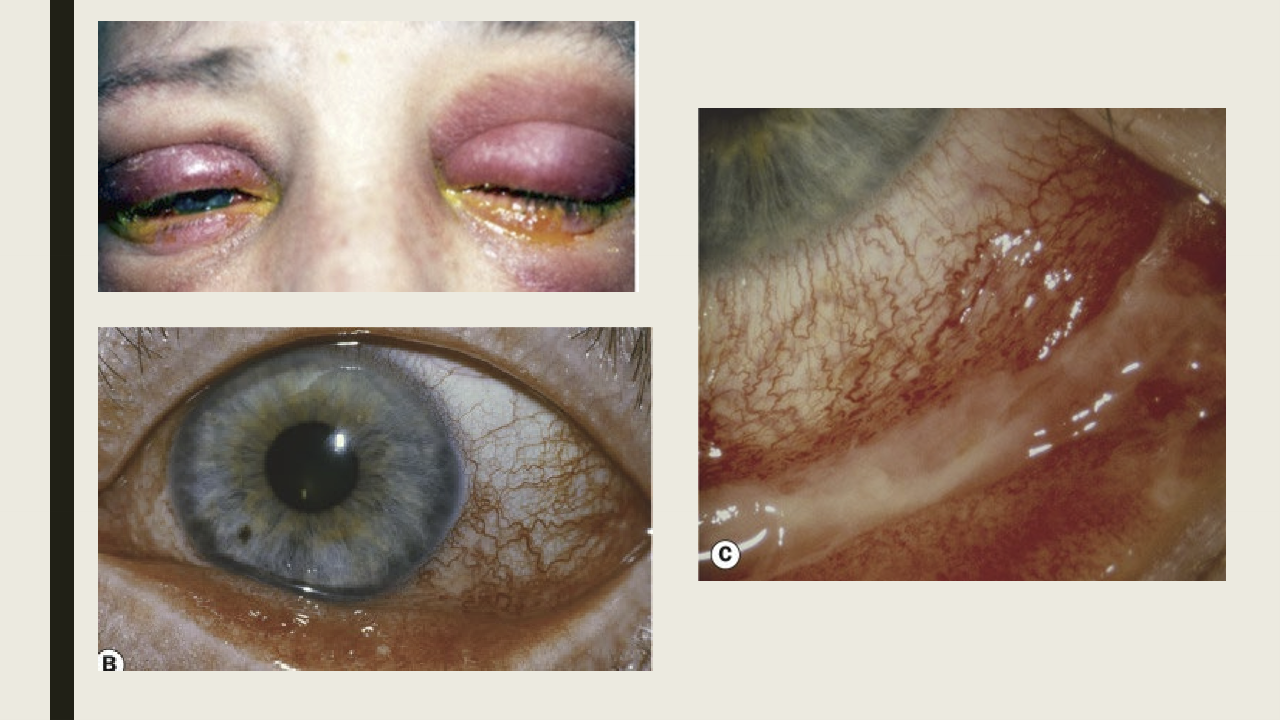
What causes adult gonococcal conjunctivits?
Neisseria gonorrhea, a sexually transmitted disease with 583,405 cases in the US in 2018.

What are the symptoms of gonococcal conjunctivits?
Severe mucopurulent discharge, returns quickly once wiped away. Rapid onset of 12-24 hours.

What are the presentations of adult gonococcal conjunctivitis?
Lid edema
Chemosis
Papillary conjuctival reaction
Corneal involvement: Infiltrate, ulceration, and perforation
Can invade an intact corneal epithelium
Very stinky, smells awful

What are the treatments for adult gonococcal conjunctivits?
Culture
Intramuscular antibiotics
If corneal is involved, hospitalization with IV antibiotics
Topical antibiotics
Management with primary care physicians or infectious disease
What is neonatal conjunctivitis/ ophthalmia neonatorum?
Conjunctivitis seen in the first month of life.
What causes neonatal conjunctivitis?
Chlamydia trachomatis
Neisseria gonorrhea
Herpes simplex (HSV-2)
Staph and strep species
Chemical: silver nitrate after birth prevent infection is super toxic to eye

What are the presentation for neonatal conjunctivits?
Discharge:
Chlamydial → mucopurulent
Gonococcal → purulent
Eyelid edema: severe with gonococcal
Vesicles on eyelid/periorbital skin: herpes
Conjunctival hyperemia: common in all
Keratitis: gonococcal, herpes

What are the treatments for neonatal conjunctivits?
Culture: helps determines the causative agent
Antibiotics: topical for mild conj or oral for moderate to severe conj
IV antiviral bc too young for oral antiviral

What is adenoviral conjunctivitis?
A highly contagious condition that affects the respiratory or ocular secretions.
How long does viral shedding occur for adenoviral conjunctivitis?
7 days shedding while asymptomatic
7 days shedding while symptomatic
7 days after symptoms, but not as severe
What are the four types of adenoviral conjunctivitis?
Non-specific acute follicular conjuncivitis
Pharyngocojunctival fever
Epidemic keratoconjuinctivitis (EKC)
Chronic/relapsing adenoviral conjunctiviits (not discussed)
What is non-specific acute follicular conjunctivitis?
Most common form of adenovrial conjunctivitis
Have associated sore throat or cold
What are the presentations of non-specific follicular conjunctivitis?
Irritation, foreign body sensation
Follicular conjunctival reaction
Conj hyperemia
PEE
Preauricular lymphadenopathy
What are the treatments for non-specific follicular conjunctivitis?
Palliative care. Artifical tears and cold compresses; wash pillows and stuff. Education that it is like a cold in eyes, steroids will make it worse, antibiotic does not help.
Who is commonly affected by pharyngoconjunctival fever?
Children
What are the symptoms and presentations of pharyngoconjunctival fever?
Have associated pharyngitis (sore throat) and fever
follicular conj reaction
conj hyperemia
Rhinitis: inflammation of the nasal mucous membranes
Preauricular lymphadenopathy
What are the treatments of pharyngoconjunctival fever?
Palliative care.
What causes epidemic keratoconjunctivitis (EKC)?
Adenovirus serotypes 8, 19, 37
What are the symptoms of EKC?
Ocular irritation/ foreing body sensation
Photophobia
Epiphora
Blurred vision d/t infltrates
What are the presentations of EKC?
Discharge-clear or yellow
Eyelid swelling
Bulbar and palpebral conj hyperemia
Conj chemosis (swelling) with follicular reaction
Keratitis: epithelial microcysts are in early stage; punctate epithelial erosions seen day 7-10; inflitrates develop day 14 and may last from months to years
Membrane or pseudomembrane formations: can cause irritation
preauricular lymphadenopath
What infection-control measures are required for a patient with EKC?
Sterilize all equipment, disinfect room, and avoid using the same room until cleaned
Strict hand hygiene, avoid sharing instruments
What are the treatments for EKC?
Paliative treatment: cold compresses, artificial tears
Topical steroids: commonly prescribed when corneal involvement is seen
Povidone-iodine: off label use; Decrease duration of symptoms and signs; very toxic to eye; need to do within 24-48 hours
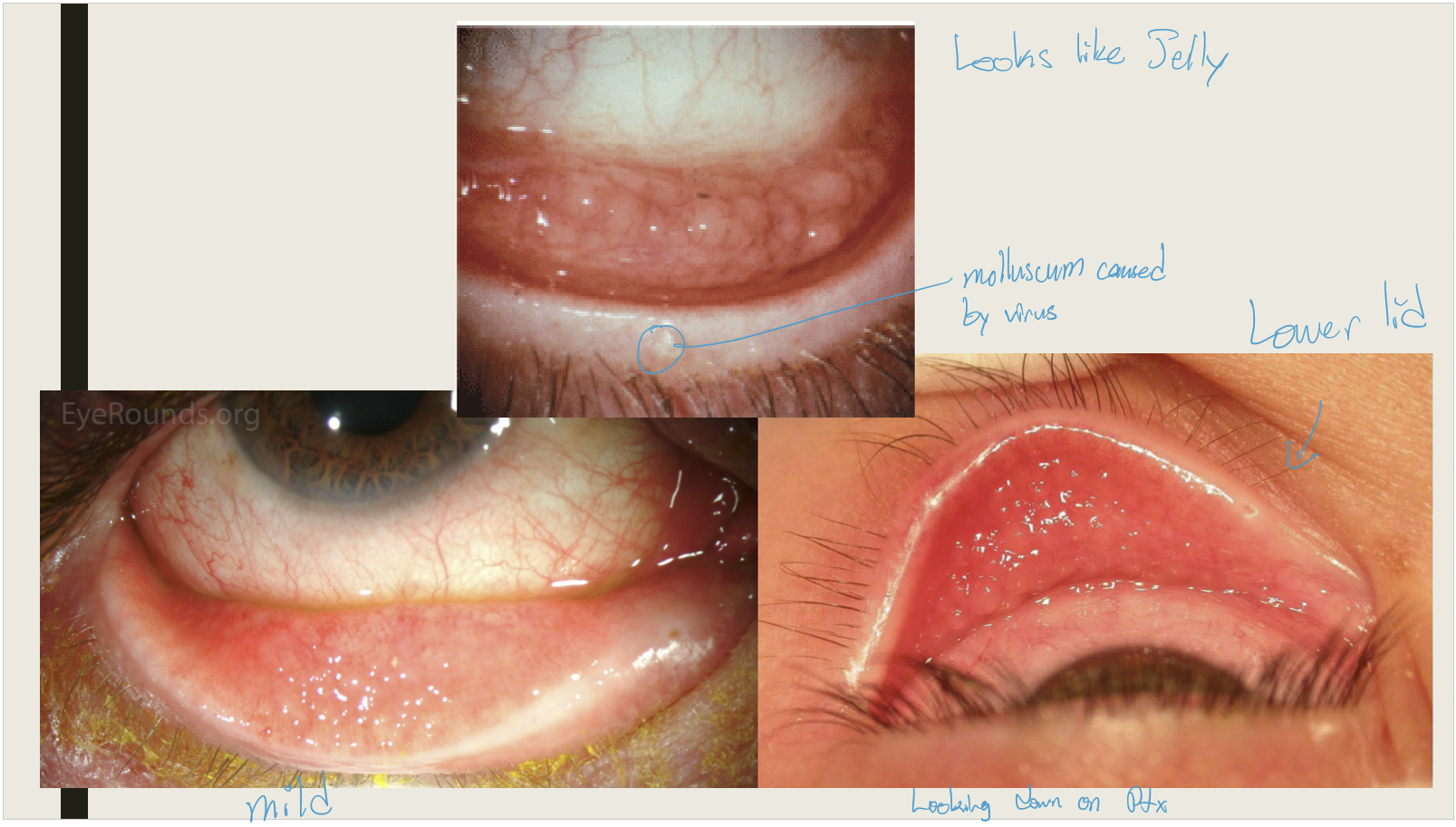
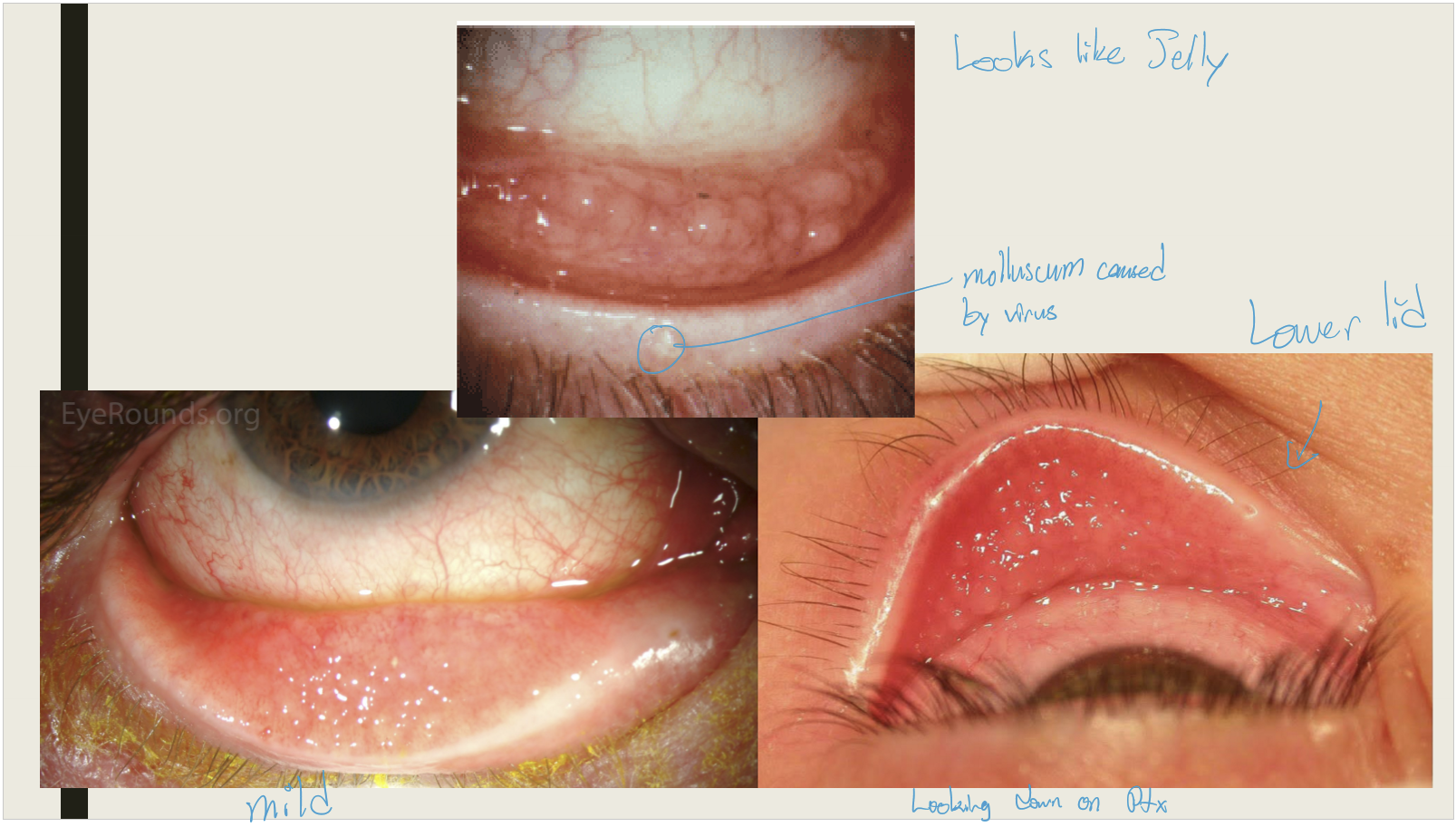
What virus causes molluscum contagiosum?
Poxvirus
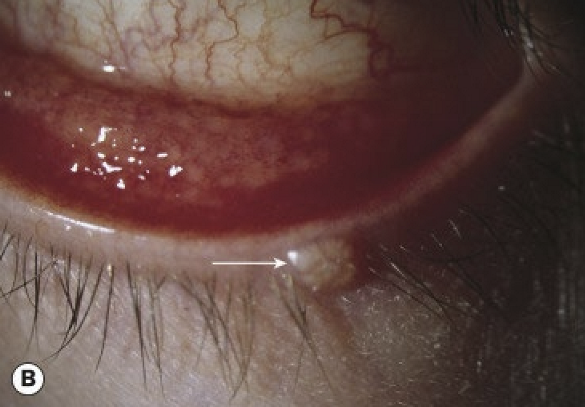
What is the typical age of incidence for molluscum contagiosum?
Most commonly affects children between 2–4 years of age. Molluscum lesions are typically seen along the eyelid margin.
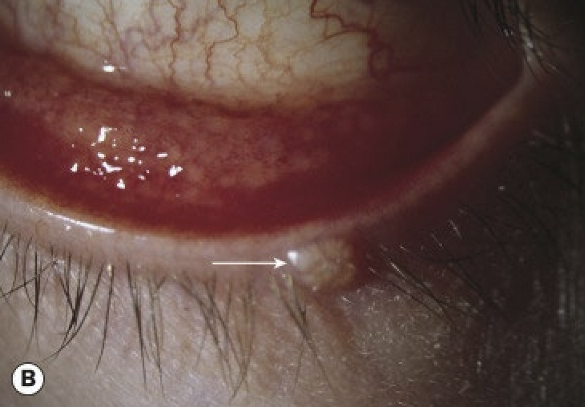
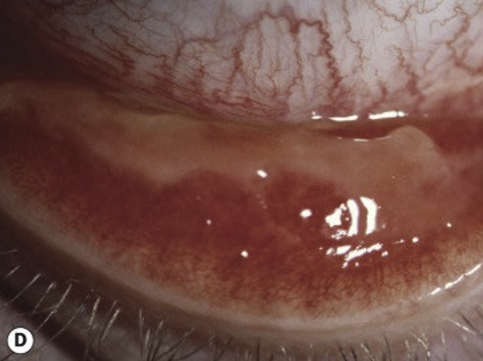
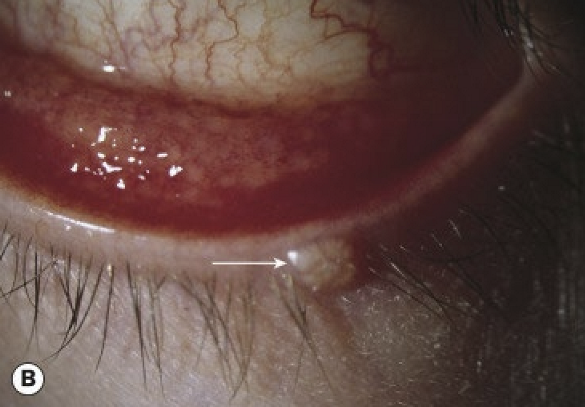
What are the symptoms and presentations of molluscum contagiosum conjunctivitis?
Chronic unilateral ocular irritation
Pale, waxy, umbilicated nodule on the lid margin
bulbar conjunctival nodule (seen with immunocompromised patients)
Epithelial keratitis and pannus can be seen in longstanding untreated cases
What are the treatments of molluscum contagiosum conjunctivitis?
Incision and drainage of the lid lesion
Cryosurgery of the lid lesion

Where does HSV1 remain dormant in and what causes it to be activated?
It lays dormant in the trigeminal ganglion and will reactive along any branch of the trigeminal nerve. Stress, fever, trauma, and UV light can activate it.
What are the symptoms and presentation of herpes simplex?
Redness
Pain
Photophobia
Unilateral follicular conj reaction
Conj hyperemia
What are the treatments for HSV?
Oral antiviral
What are the ocular symptoms and presentations of COVID-19?
Discharge
Epiphora
Photophobia
Follicular conj reaction
conj hyperemia
chemosis
What are the treatment for COVID-19
Palliative care: artificial tears and lid hygiene.
What are the types of allergic conjunctivitis?
Acute: more common in children
Seasonal: caused by pollen
Perennial: symptoms throughout the year; caused by dust mites, animal dander, and fungal allergens
What causes allergic conj?
Environmental allergy. Can be seasonal with symptoms being worse in spring and summer
What are the symptoms and presentations of allergic conjunctivitis?
Itching and watering
Papillary reaction
conj hyperemia
conj chemosis
What are the treatments for allergic conjunctivits?
Topical or oral anti-histamine
topical mast cell stabilizer
topical steroid
cold compresses: feels better, but doesn’t treat issue.
What is vernal keratoconjunctivitis (VKC)?
IgE and cell mediated immune response.
Who is affected by VKC?
Affects males more than females
Onset of symptoms around 5 yrs old, and symptoms improve with age
More common in hot dry climates
Peak incidence is in spring and summer
What are the symptoms of VKC?
Itching
Foreign body sensation
Thick mucoid discharge
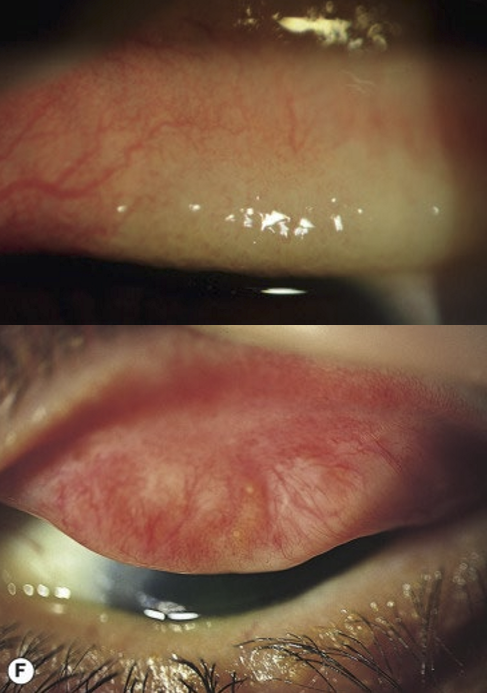
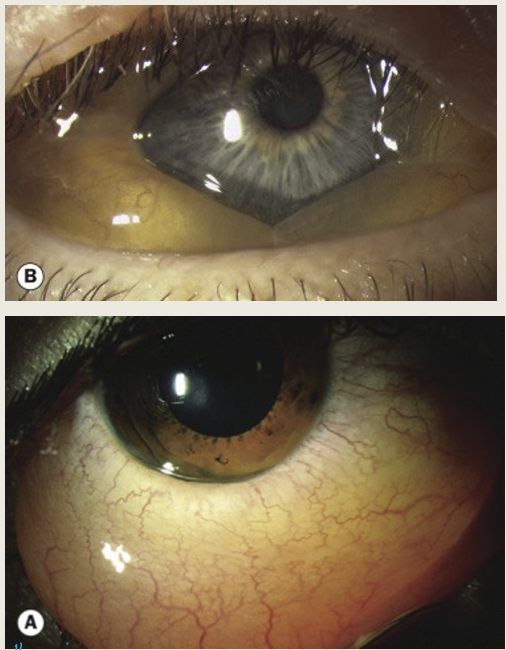
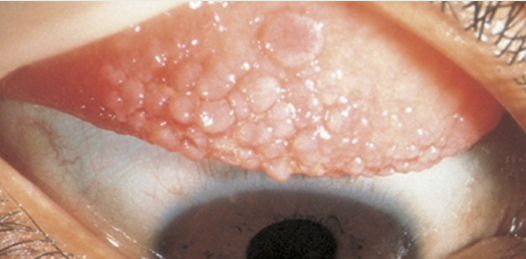
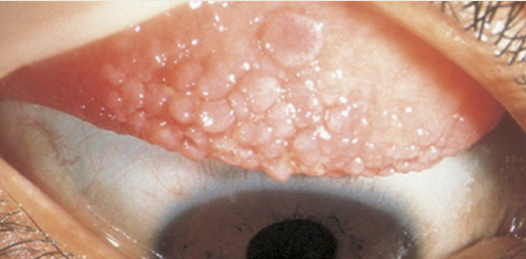
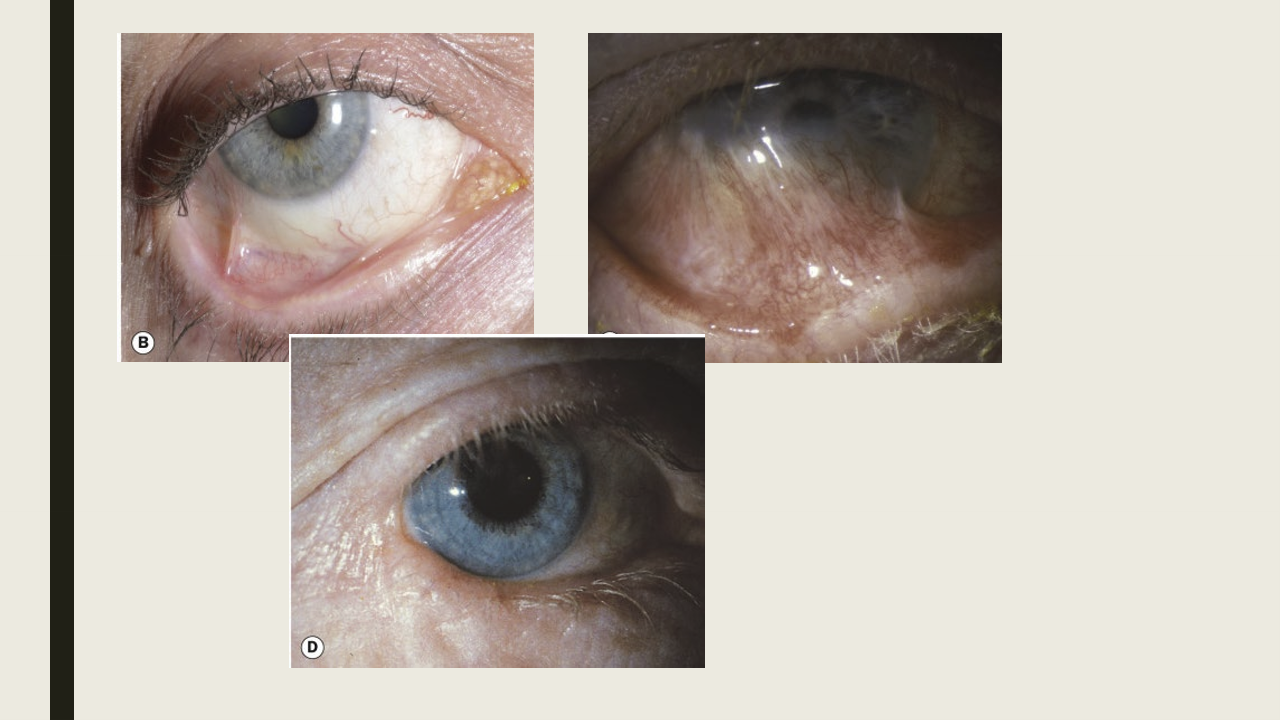
What are the conj presentations of VKC?
Macropapillae of superior tarsal plate, less than 1mm
Giant papillae of superior tarsal plate, larger than 1mm with mucus seen between giant papillae
Conj hyperemia
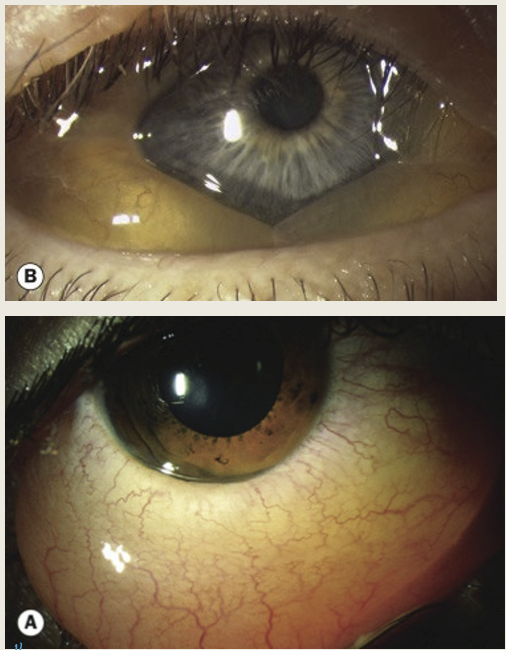
What are the limbal presentations of VKC?
Limbal papillae: gelatinous appearing papillae at the limubs
Horner-Trantas dots: focal white dots at the limbus. Dots are made up of degenerated epithelial cells and eosinophils
What are the corneal presentations of VKC?
Superior PEE, associated with sheets of mucus
Epithelial macroerosions d/t coalesced PEE, inflammatory mediators, and mechanical injury d/t superior tarsal papillae
Plaques and shield ulcers: plaques composed of fibrin and mucus and collect on macroerosions and form shield ulcers
Subepithelial scars: appear grey and oval, may affect vision
Pseudogerontoxon: can be seen with recurrent limbal disease, is white-grey band in anterior stroma of scarring, adjacent to area of previous limbal infection
Corneal neovascularization, tends to be superior
What are the treatments for VKC?
Topical steriods: most effective at any stages
Allergen avoidance
Palliative care- cold compresses and lid hygiene
Topcial antihistamine: good for mild cases
Topical antihistamine and mast cell stabilizer: good for moderate cases
Topical cyclosporine: anti-inflammatory
Systemic steroids: used only with sight threatening conditions
Surgical: amniotic membrane and keratectomy for severe corneal disease
What is atopic keratoconjuctivits (AKC)?
A chronic inflammation eye condition that combines type I and type IV reactions. It develops in adulthood, around 30-50 yrs old. Tends to be worse in winter. Males = Females
Who is at risk for AKC?
Individuals typically diagnosed with eczema, asthma, allergies. 5% were previously diagnosed with VKC.
What are the symptoms of AKC?
Itching
Tearing
Photophobia
Mucoid discharge
Tends to be worse than VKC
What are the presentations of AKC?
Conj: worse inferior
Papillary conj reaction
Conj hyperemia
Horner-trantas dots
Conj scarring and symblepharon formation (lead to a shorten fornix and keratinziation of the caruncle)
Cornea:
PEE inferior 1/3 of cornea
Persistent epithelial defects, may have associated corneal thinning
plaques
peripheral vascularization with stromal scarring, more common with AKC than VKC
Cataract: shield like anterior or posterior subcapsular cataract
What are the treatment for AKC?
Remove antigen
Palliative care: lid hygiene, cold compresses, artificial tears
Topical mast cell stabilizer, antihistamine or combination
Topical steriods and cyclosporine
Oral antihistamine or steroid
Bandage contact lens: persistent corneal defect
Surgical: amniotic membrane, keratoplasty (used for persistent corneal defect)
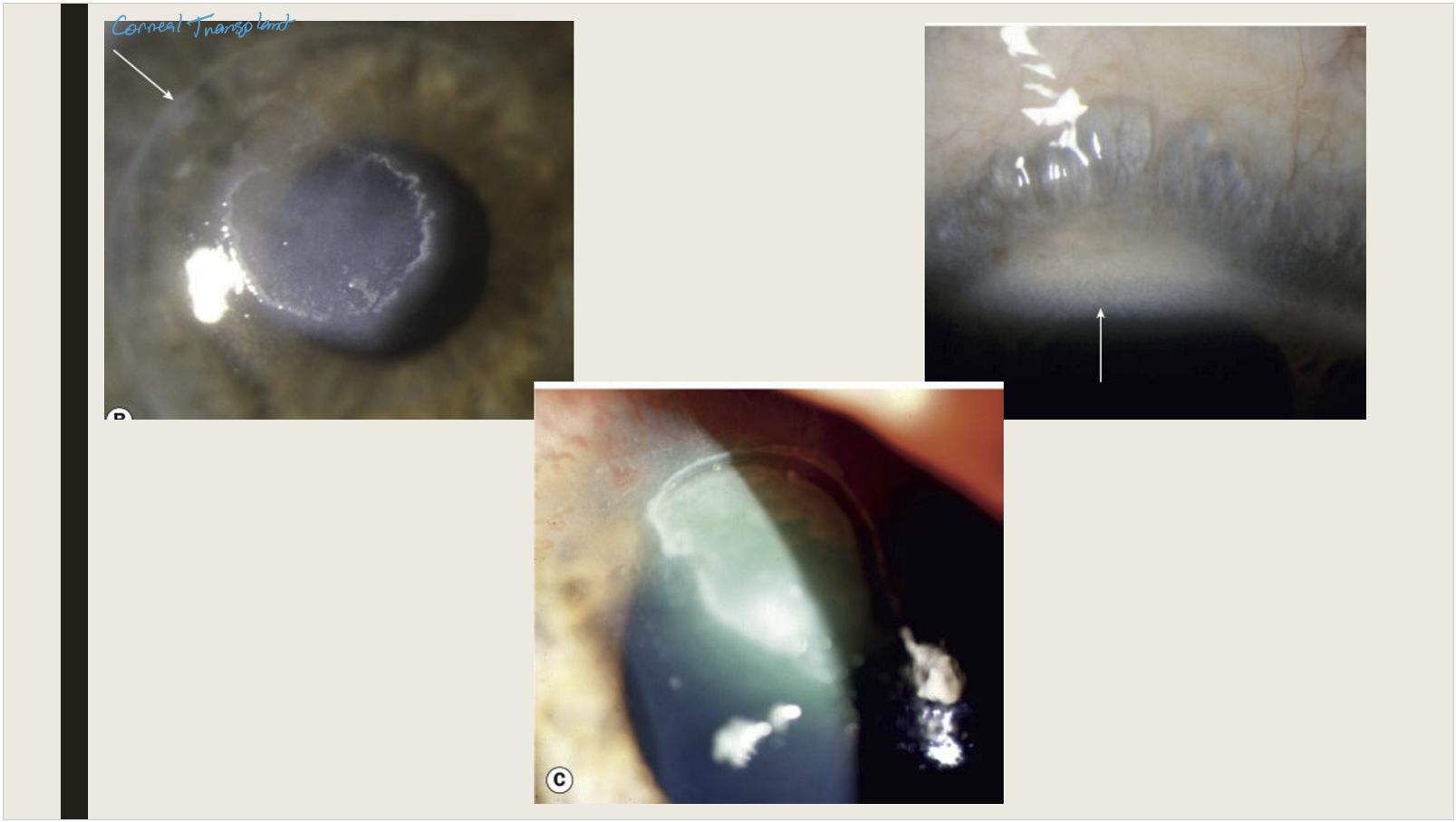
What causes Giant papillary conjunctivitis (GPC)?
Mechanical irritation:
CL: protein build up on lens
Ocular prosthetic
Exposed suture- commonly seen with corneal transplant
Scleral buckle- retinal detachment repair
Filtering bleb from trabeculectomy: glaucoma surgery
Mucus fishing syndrome
What are the symptoms of GPC?
Foreign body sensation
Redness
Itching
Mucus discharge
CL intolerance: symptoms may worsen after removal
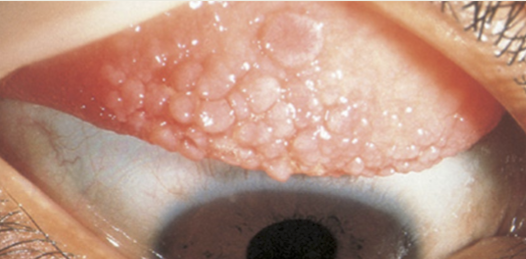
What are the presentation of GPC?
Conj hyperemia of the superior tarsal plate
Medium sized papillae (>0.3mm) on superior tarsal plate. can ulcerate in advanced cases
CL intolerance: excessive movement of CL, protein deposits on the CL
What are the treatments for GPC?
Discontinue CL wear until resolution (6wks) and stress importance of proper wear schedule and cleaning regimen
Proper cleaning regimen for ocular prosthetic
Topical mast cell stabilizers, antihistamines, and combination
Topical steriods
How can conjunctivitis be differentiated by follicles, papillae, and discharge?
Follicles + preauricular node →
• Herpetic signs present → HSV
• Herpetic signs absent → Adenovirus/ChlamydiaFollicles, no preauricular node → Toxic conjunctivitis, Molluscum, Pediculosis
Papillae + severe purulent → Gonococcal (GC)
Papillae + scant purulent → Bacterial (non-GC)
Papillae + watery → Allergy/Atopy
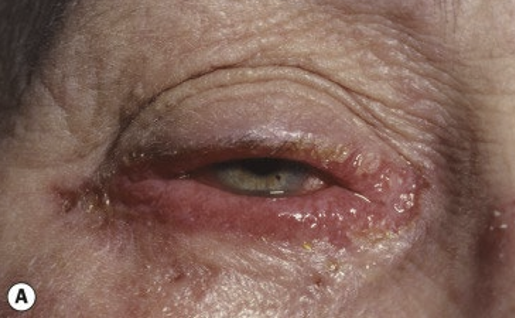
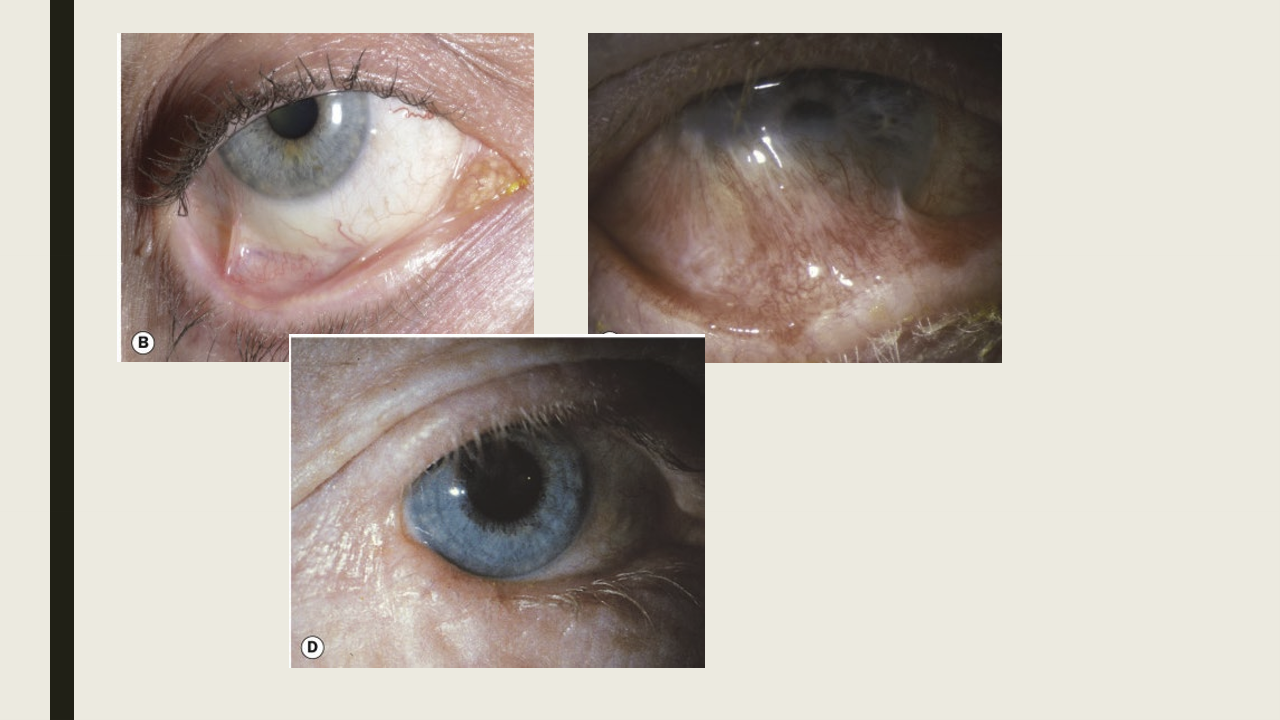
What is cicatrical pemphigoid/ mucus membrane pemphigoid?
A group of chronic autoimmune mucocutaneous blistering disease that affects con, nasopharynx, upper airways, gastrointestinal. Typically 2x females vs males.
What causes cicatricial pemphigoid?
Type II hypersensitivity, antibodies bind with complement at the basement membrane and recruit inflammatory cells.
What are the presentation of cicatricial pemphigoid?
Bilateral, but asymmetric condition.
Insidious onset
Conj:
papillary reaction
diffuse hyperemia and chemosis
flatenning of the plica and keratinization of the caruncle
conj fibrosis and shortening of inferior fornix
symblepharon-adhesions between the bulbar and palpebral conj
destruction of goblet cells and accessory lacrimal glands
Necrosis in sever cases
Cornea: PEE, vascularization, infiltrates, keratinization of cornea d/t limbal stem cell failure
Eyelid: aberrant lashes, blepharitis, keratinization of the lid margin, ankyloblepharon-connection of upper and lower lid at the lateral canthus
What are the treatments for cicatricial pemphigoid.
Systemic:
Oral antibiotic/anti-inflammatory
antimetabolites-chemotherapy drugs
oral steriods
Ocular treatment:
Artifical teras
topical steriods
blepharitis treatment (lid hygiene and tetracyclines)
Subconj injections: mitomycin-C or steroid
How are the complications of cicatricial pemphigoid treated?
Laser removal of aberrant eyelashes
punctal occlusion for severe dry eye
tarsorrhaphy when persistent epithelial defects are present
amniotic membrane for keatinization of the conj
entropion repair
keratoplasty or keratoprosthetic
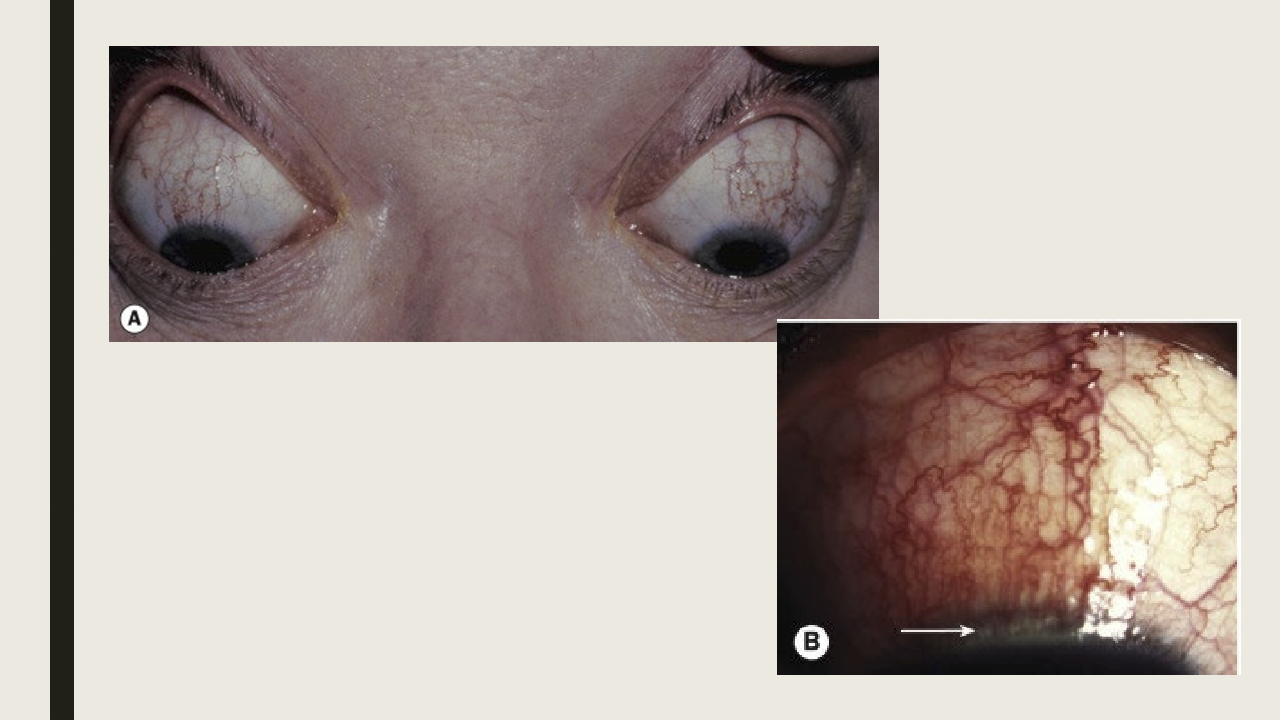
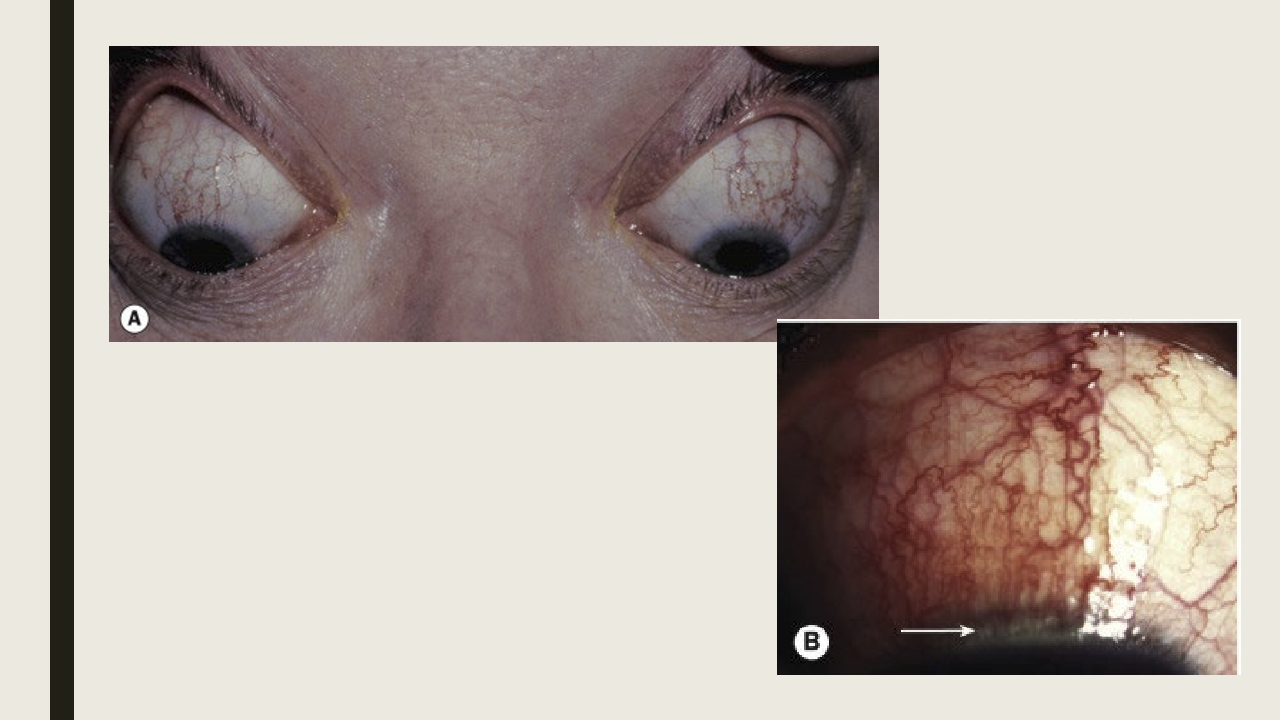
What is stevens-johnson syndrome?
An autoimmune reaction that causes painful rash and blistering of the skin and mucous membranes. Less than 5000 individuals in US have been diagnosed.

What are the symptoms and presentations of steven-johnson syndrome?
Prodromal phase: fever, malaise, muscle and joint pain
Skin rash that develops on the trunk and face, eventually skin will become necrotic and slough off
Bilateral conj hyperemia and purulent discharge
Subconj hemorrhage
PEE with epithelial defects
Conj membranes affected

What are the complications from stevens-johnson syndrome
Symblepharon
Lid margin keratinization
meibomain gland disease/dry eye
corneal opacificaion
Distichiasis
What are treatments for stevens-johnson syndrome?
Systemic: removal causative agent
Ocular:
Artifical tears and ointments
topical antiboitcs
removal of conj membranes
treatment of complications
What is Superior limbic keratoconjunctivitis (SLK)?
A bilateral condition where chronic inflammatory condition affects the superior bulbar conjunctiva, limbus and upper cornea. 50% association with TED.
What are the symptoms and presentation of SLK?
Foreign body sensation, photophobia, pain
Radial injection of only superior bulbar conj starting at the limbus
Papillary reaction of superior palpebral conj
Punctate staining of superior cornea, filaments may be present
What are the treatments for SLK?
Similar to dry eye treatment: artificial tears, topical anti-inflammatory medication, topcial cyclosporine, concurrent lid disease
Bandage contact lens
What causes subconjunctival hemorrhages?
Valsalva (coughing, sneezing, constipation, heavy lifting)
Systemic conditions: hypertension, bleeding disorders
Medicatino induced: antiplatelet or anticoagulant medication
Traumatic
Idiopathic

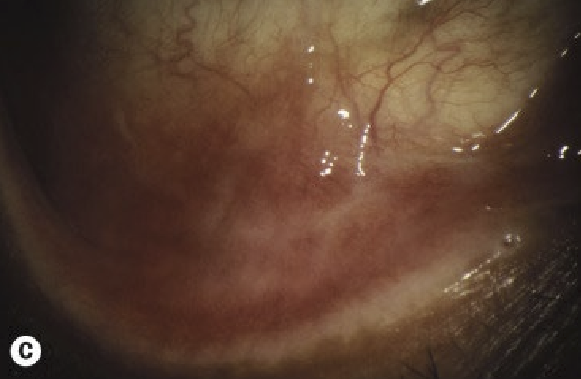
What are the symptoms and presentation of subconj hemorrhage?
Typically no symptoms, hay have irritation if hemorrahge is large
Collection of blood beneath of the conj
Tends to be sectoral but can be diffuse
Details of the sclera will be blocked by the blood

What are treatments for subconj hemorrhage?
Palliative care: artificial tears for irrataion
Check BP
Communicate with PCP if taking antiplatelet or anticoagulant meds
Lab work for recurrent subconjunctival hemorrhages: Prothrombin time, partial thromboplastin time, complete blood work with platelet
