Normal Labor and Delivery
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
Labor Definition
Onset of uterine contractions of sufficient frequency, intensity, and duration to result in effacement and dilation of the cervix
Effective uterine contractions
Last 45-90 seconds, increasing in duration as labor progresses
Create 40-100 mmHg
Occur every 2-4 minutes
Duration of labor depends on:
Parity
Size and position of fetus
Shape and capacity of pelvis
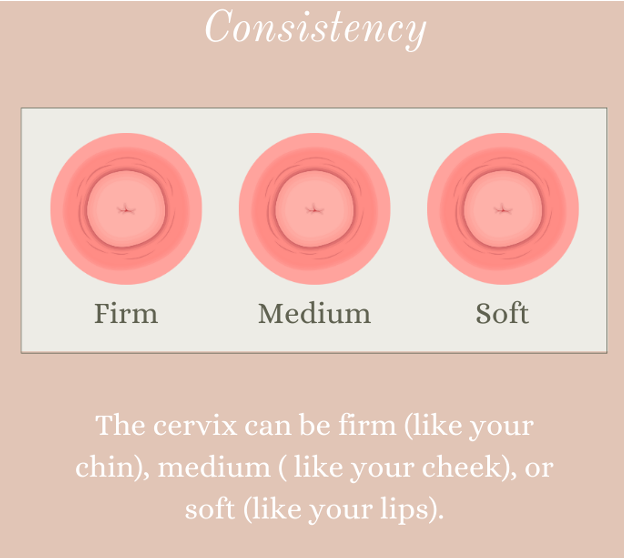
Consistency of cervix
Firm: cannot push baby out
Efficiency of uterine contractions
Assessment of patient in labor
Digital vaginal exam
Assessment of cervix
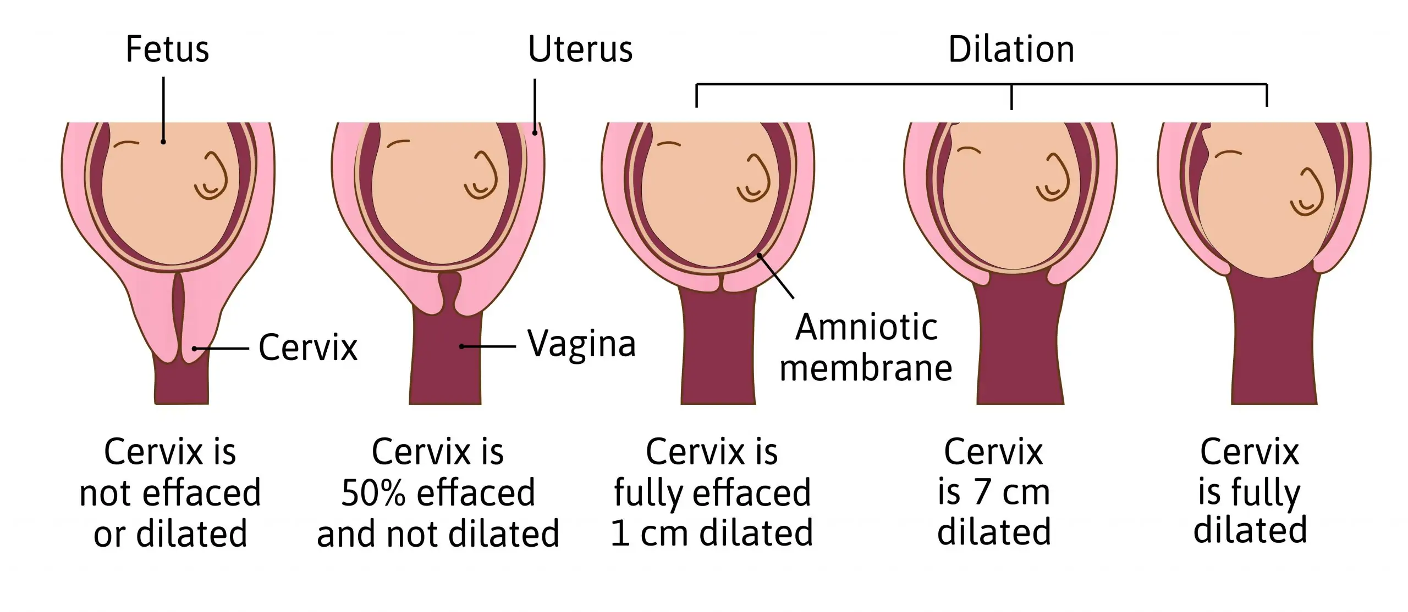
Effacement: thinning
Dilation: opening
Consistency: soft
Position of cervix
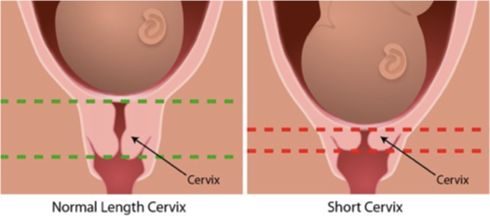
Effacement
Thinning and shortening of cervical canal
Normal length: 3-4 cm
Measured in percentages
Cervix thins out and softens → length is reduced
Determine by palpating cervix with finger and estimating length from internal to external os
Need 50-60% effacement before cervix can open effectively
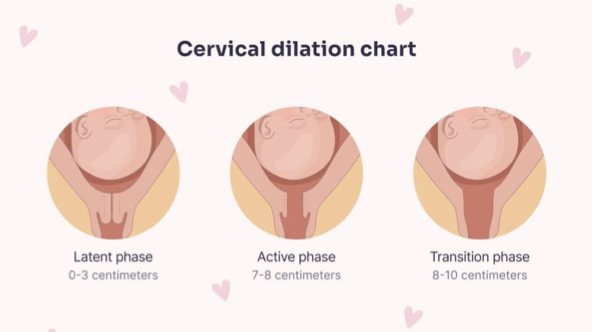
Dilation
Opening of the cervix to accomodate the baby
Describes the size of the opening of the cervix at the external os
Measured in cm (1-10)
Ranges from closed (-) to fully dilated (10 cm)
Determine by sweeping the examining finger from the margin of the cervix on one side to the other side
Phases
Latent: 0-3 cm
Active: 7-8 cm
Transition: 8-10 cm
Effacement and Dilation
Consistency
Ranges from firm to soft
Soft: indicated onset of labor
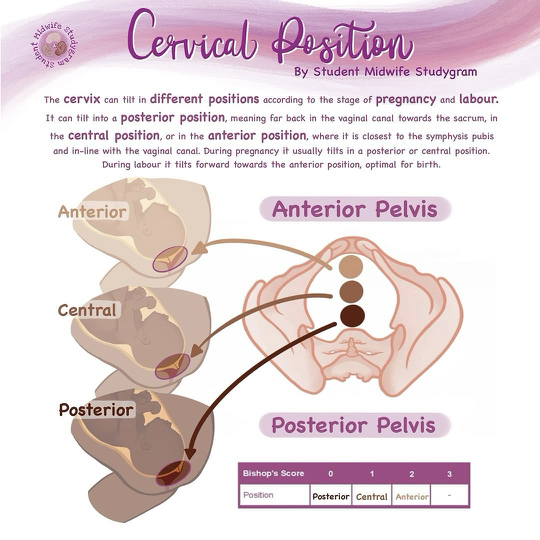
Position
Describes location of cervix with respect to fetal presenting part
Classified as posterior, mid-position, anterior
Progresses from posterior to anterior in labor
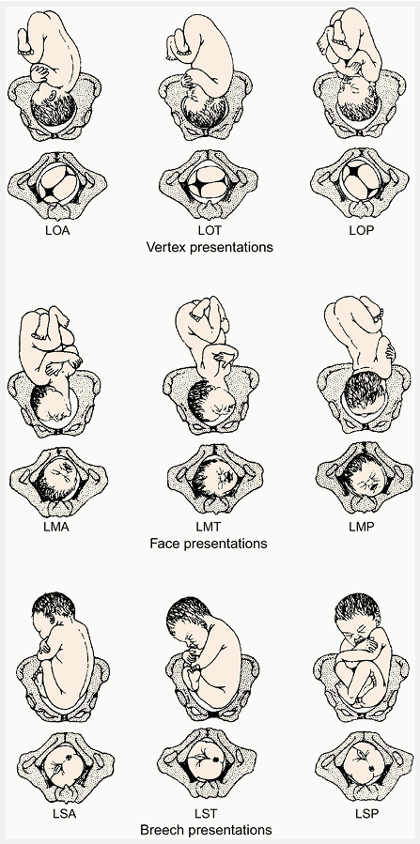
Position
Relation of presenting part to fetus to right or left side of birth canal and its direction anteriorly, transversely, or posteriorly
Most common is occiput anterior
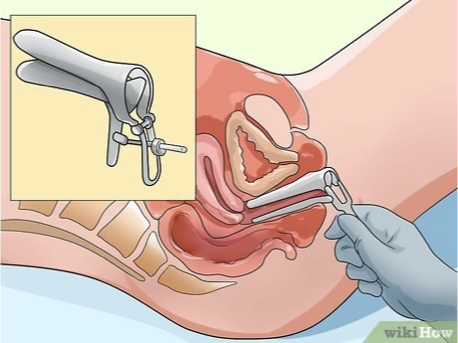
Sterile speculum exam for:
Suspected rupture of membranes
Preterm labor
Signs of placenta previa
Rupture of membranes
Premature rupture of membrane (PROM): happened on its own
Preterm premature rupture of membranes: happens when baby is premature (< 36 weeks)
Artificial rupture of membranes (AROM): provider manually ruptures membranes
4 ways to test rupture of membranes
Pooling
Sterile speculum inserted into the vagina to evaluate for the presence of amniotic fluid pooling
Nitrazine paper test
Check pH → (+) if paper turns blue
Ferning test
Swab collected and evaluated under microscope: (+) if there is a fern like pattern (salt content of amniotic fluid)
AmniSure
Immunoassay test that detects specific proteins found in amniotic fluid → highly accurate
Pooling, Nitrazine paper test, and Ferning test usually done together
Complications → chorioamnionitis
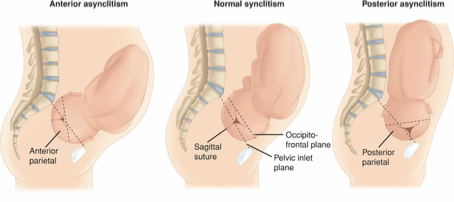
Synclitism
Optimal fetal head position during labor
Head is not tipped to either side
Bi-parietal diameter (widest part of the head) is parallel to the plane of the pelvis
Sagittal suture is midway between the maternal symphysis pubis and the sacrum
Affects how the baby moves through the birth canal
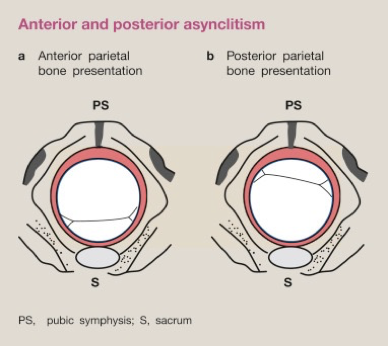
Asynclitism
Fetal head is tipped towards one shoulder laterally, causing it to engage with the pelvis in an uneven, lateral, or oblique angle
Anterior: anterior parietal bone is closer to pelvis, making the sagittal suture closer to the sacrum
Posterior: posterior parietal bone is deeper in the pelvis, making the sagittal suture closer to the pubic symphysis
Severe cases can impede fetal descent
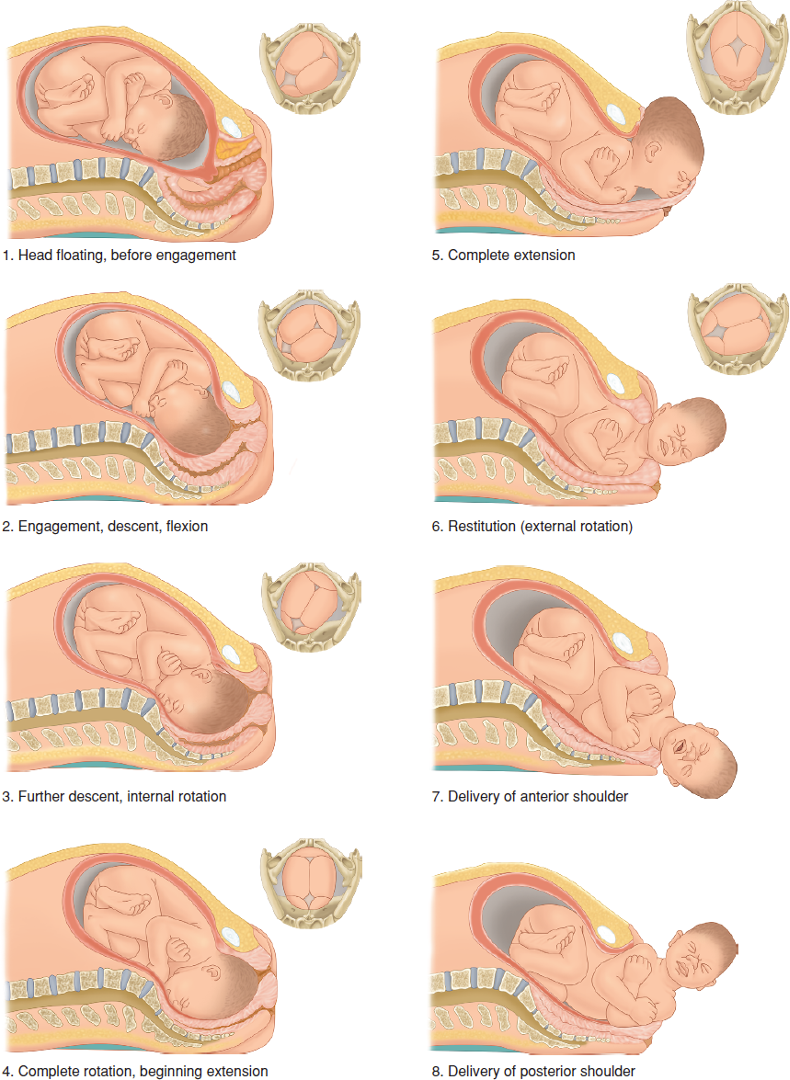
Cardinal Movements of Labor
Engagement
When widest diameter of fetal presenting part has passed through pelvic inlet
In most, the bony presenting part is at level of the maternal ischial spines when head becomes engaged
Descent
Flexion of head
Partial flexion exists before labor → further flexion occurs with descent
Internal rotation
Extension
External rotation
Expulsion
True Labor Contractions
Regular and get stronger
Stronger with walking
No change laying down
Back and abdominal pain
Cervix thins and dilates
No effect with sedation
False Labor Contractions
Contractions irregular and short
No change if walking
Goes away laying down
Lower abdominal pain
No cervical change
Sedation helps
First stage of labor: onset
Onset of labor until full effacement and dilation
Body getting ready for birth
Usually the longest stage of labor
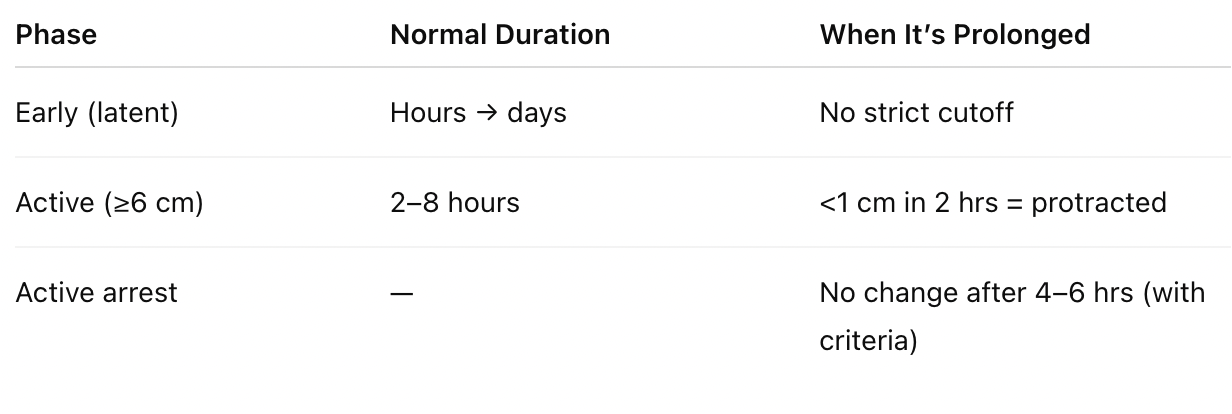
Latent phase
Effacement and early dilation (0-3-4 cm)
Contractions mild to moderate, irregular, and gradually increasing in frequency and intensity
Strong period cramps or lower back pain
Timing depends on history of vaginal birth
Nulli: 6-20 hours
Multi: 2-12 hours
Normal for early labor to stop and start for a stretch of days
Prolonged
Nullips: > 20 hours
Multips: > 14 hours
Active phase
Rapid, progressive cervical dilation
Cervix dilates from 6-10 cm
Contractions are strong, more regular, and closer together: usually every 2-4 minutes
Cervix progresses about 1 cm dilation every 2 hours
Duration
Nulli: 4-8 hours
Multi - 2-5 hours
Prolonged active phase
< 1cm dilation over 2 hours (especially after 6 cm)
May prompt: position changes, hydration, pain management, possible augmentation of labor (Pitocin)
Active phase arrest
Cervix is >= 6 cm
Membranes are ruptured
No cervical changes despite
4 hours of adequate contractions OR
6 hours of inadequate contractions with Pitocin
Medications given
Antiemetics: metoclopramide
If GBS (+): penicillin
Pain control
Non-pharmacological: walking, swaying, side lying, lunging, birthing ball or peanut ball, breathing and relaxation, songs
Pharmacological
Systemic analgesics (IV/IM): opioids (fentanyl, morphine), nitrous oxide
Epidural analgesics: blocks pain from uterine contractions and cervical dilation, no longer restricted by cervical dilation
Labor Augmentation
Prostaglandins (Misoprostol): ripens cervix if it is not favorable (cannot give Pitocin to a firm cervix)
Pitocin: stimulates uterine contractions
Second stage of labor: delivery
Complete dilation of the cervix to the delivery of the infant
Have intense pushing and delivery of the baby with strong uterine contractions
Contractions every 2-3 minutes lasting 60-90 seconds
Duration
Nulli: 3 hours
Multi: 2 hours
Longer durations may be normal if progress continues and fetal status is reassuring
Crowning
Widest part of baby’s head remains visible at the vaginal opening between contractions and birth is imminent
Pronounced molding of fetal head
Further extension under pubic arch
Full crown of head emerges
Perineum ready to slip over fetal nose, mouth, and chin
Controlled birth necessary to avoid sudden compression on fetal head and trauma to maternal tissues (provider may support perineum)
Molding
Changes to the newborns head during labor
Shaping and overlapping of bones in the fetal skull as the baby passes through the birth canal → reduces diameter of the head
Physiological adaptation to help the baby’s head fit through the maternal pelvis
More extreme if infant rotated to posterior position during labor and birth (occiput posterior)
Results in elongated or cone-shaped head
Usually resolves in hours to days after birth as the cranial bones return to their normal position; no treatment needed
Benign; no treatment needed
Positions
Upright: uses gravity, improves pelvic dimensions
Hands and knees
Pain and sensations
Strong rectal pressure
Stretching or burning at crowning
Epidural may reduce urge to push
Third stage of labor: placenta
Separation and expulsion of placenta
Uterus globular and more firm (contracting to prevent postpartum hemorrhage)
Sudden gush of blood
Umbilical cord protrudes farther out of vagina
Duration
5-10 minutes from delivery of infant
Prolonged if > 30 minutes
Examining placenta
Examine to see if all lobes and membranes are present (cotyledons)
Examine for placental abnormalities
Cord blood samples may be taken
Involution of uterus → contracts to size of grapefruit after placenta delivers
Fourth stage of labor: postpartum
The hour or two after delivery when the tone of the uterus is re-established as the uterus contracts again, expelling any remaining contents
Episiotomy
Intentional surgical incision in perineum made during the second stage of labor to enlarge the vaginal opening for birth
Not routine anymore
Indicated if
Non-reassuring fetal heart rate requiring rapid delivery
Operative vaginal delivery
Shoulder dystocia
Rigid perineum preventing delivery
Breech delivery
Not recommended for routine prevention of perineal tears, for convenience, for tradition, or to shorten second stage
Mediolateral
Midline and extends diagonally
Lower risk of anorectal injury
More challenging repair
More painful d/t increased tissue damage and involvement of muscle
Preferred in situations with higher risk of severe tears, such as operative deliveries (forceps or vacuum) or larger babies
Midline
Midline straight downward
Higher risk of tears extending into anal sphincter or rectum
Easier repair
Good healing/less pain
Rare dyspareunia
Small blood loss
Good anatomic result
Preferred in low risk deliveries where the risk of severe tearing is minimal
Risks and complications
Increases blood loss
Higher rates of 3rd-4th degree lacerations
Postpartum pain
Dyspareunia
Infection
Evidence shows that spontaneous tears heal better then routine episiomities
Repair immediately after with absorbable sutures
Uterine Hemostasis
Physiologic: uterine muscle fibers contract to constrict blood vessels where the placenta was attached
Uterine massage: manual massage helps stimulate contractions and expel clots
Controlled cord traction: gentle pulling on the umbilical cord while applying counter pressure to the uterus (facilitates delivery of the placenta without causing uterine inversion)
Early cord clamping
Cord is clamped and cut within seconds of delivery
Shortens third stage of labor but may decrease neonatal blood volume
Delayed cord clamping
Cord is clamped 1-3 minutes after delivery or until pulsations stop
Benefits for baby: increased iron stores and improved hemoglobin levels