Imaging Capstone
1/151
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
152 Terms
xray circuit
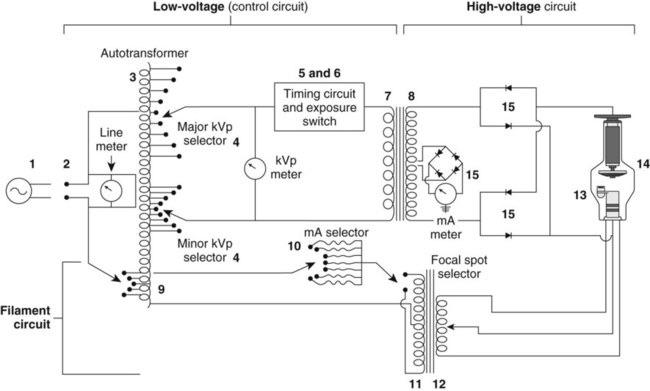
main power supply
wall outlet at 220 V
line compensator
reduce fluctuations in power source
autotransformer
self induction
single coil- variable makes small changes to voltage
mA selector
sets mA sent to filament, more heat means more xrays
what mA selector controls
heat/current for thermionic emission
step down transformer
mutual induction
more turns on primary side
increase current/amperage
Thermionic emission
rectifiers
change AC to DC
xray tube housing
lead, prevents leakage and off focus radiation emitted not aimed at pt
gas envelope
creates air-free vaccuum
prevents from corrosion and oxidation
extends tube life
cathode
negative
creates free electrons through thermionic emission
filament and focusing cup
filaments
tungsten
heat passes through heating filament emitting a cloud of electrons- space charge source-
2 dual focus
small filament
small heat capacity- small mA
higher spatial resolution
small exposures and small body parts
large filaments
can handle larger mA
lower spatial resolution- electron stream larger
for larger mA and larger body parts
focusing cup
hold filaments
focuses electron stream to small area on target increasing spatial resolution
negative to repel electrons toward anode
tungsten is good why
high atomic number, high melting point, readily dissipates heat
space charge effect
limited number of electrons that can be created at the cathode.
once cloud is full saturation, no more room for more electrons to boil off
number of electrons increases with increasing mA and time
anode
Positive- attracts charged electrons
Absorbs electrons and creates xray photons
Rotating anode allow higher heat capacity and larger focal track- induction motor
anode material
tungsten and renium
rotor
turns in xray tube
stator
electromagnets inducing turn of rotor
actual focal spot
on target
effective focal spot
projected or useful focal spot
on patient
anode heel effect
Variation in beam quantity-intensity- across the x-ray field
where is intensity the lowest, why?
anode side (80% as strong)
Photons created deeper in the anode have to pass through the “heel” and lose intensity due to absorption in the target material
where is intensity the highest
cathode side (120% as strong)
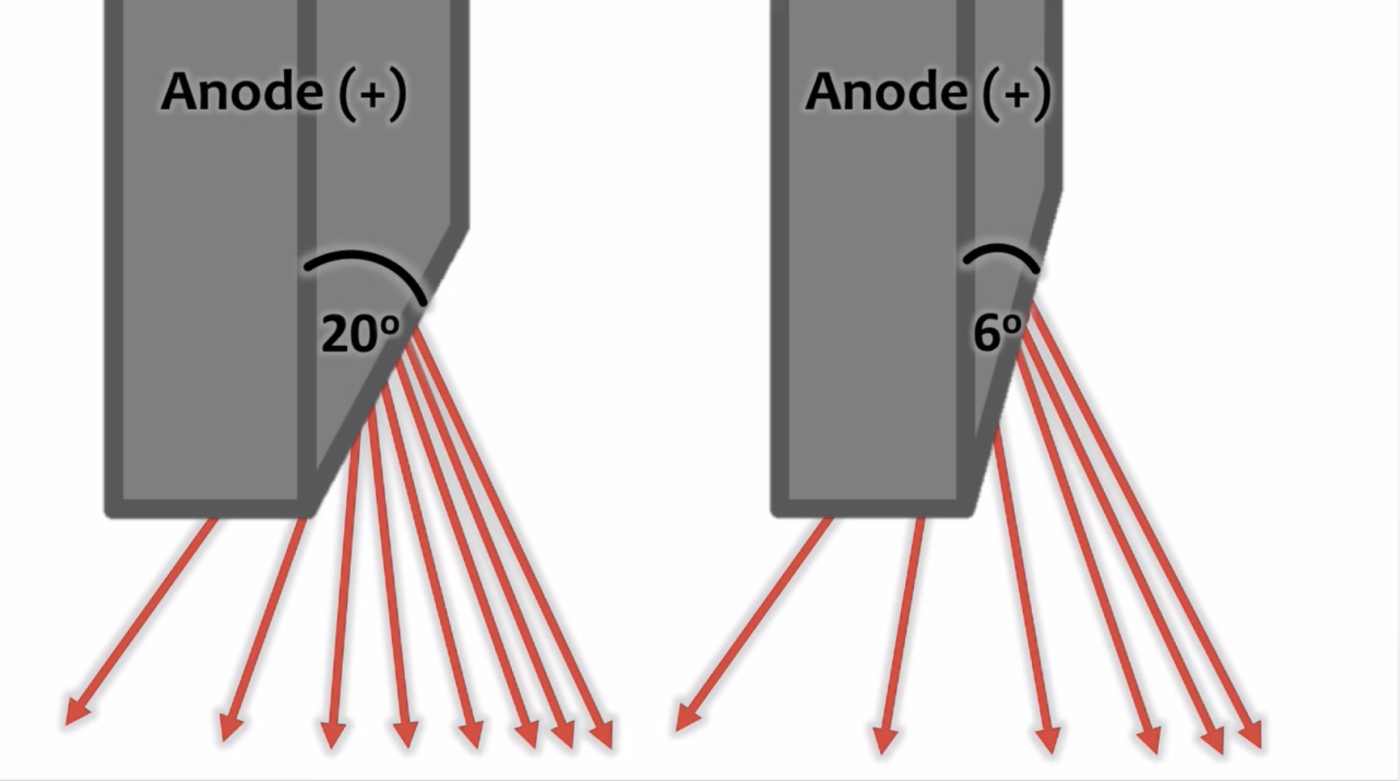
what happens to uniformity as anode angle decreases
decreases
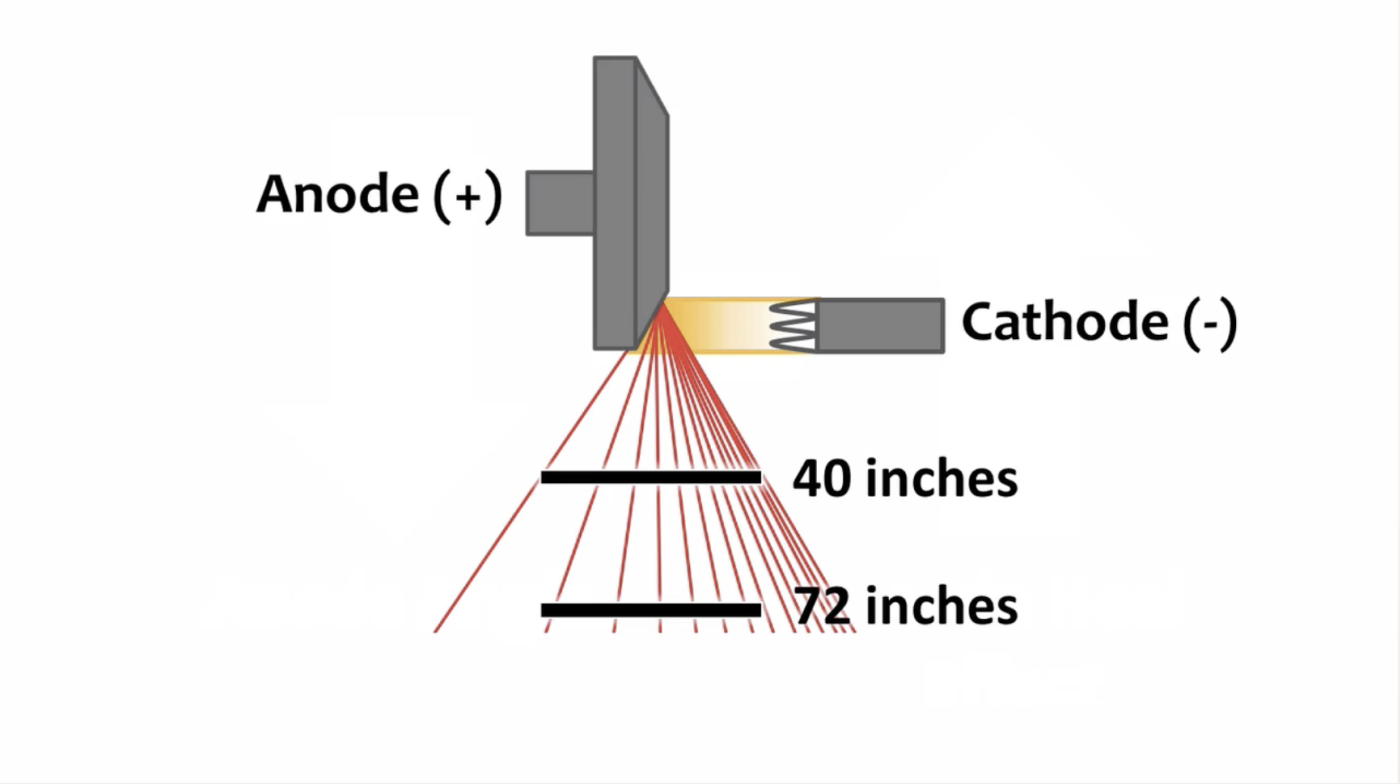
increase anode heel effect with SID
decrease the SID

why does increased SID decrease anode heel effect
Larger SID allow IR to be exposed to more of the center of the beam creating a more even exposure
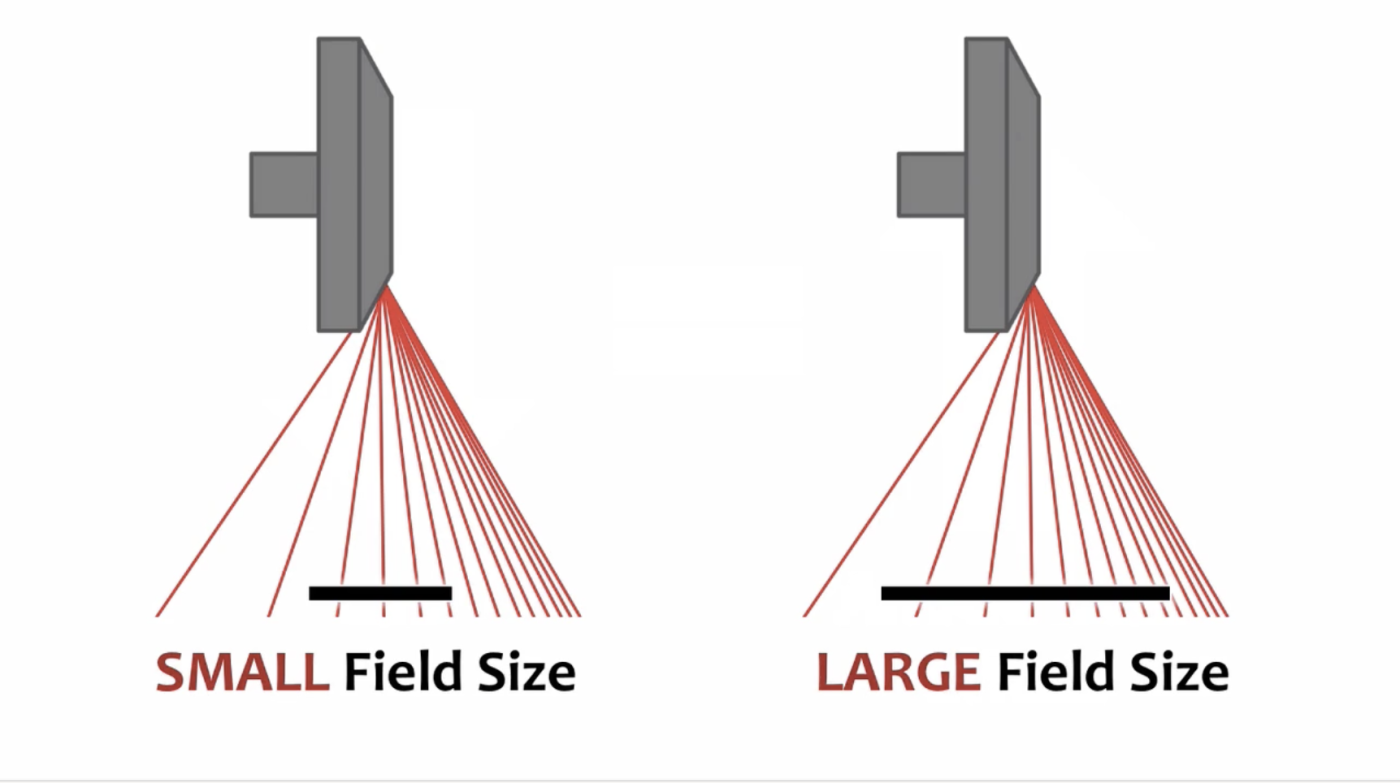
increase anode heel effect with field size
increase field size
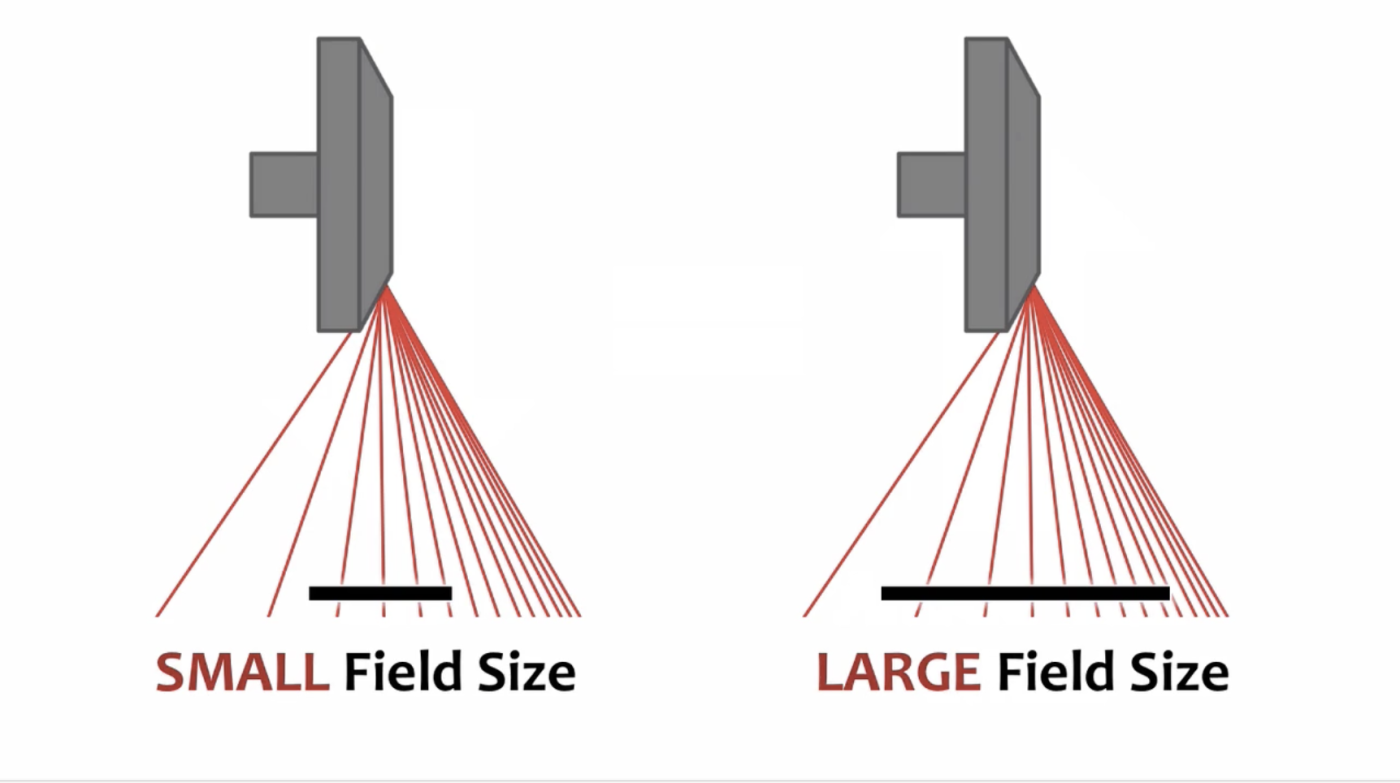
why does increased field size increase anode heel effect
Larger field size exposes IR to high and low intensity
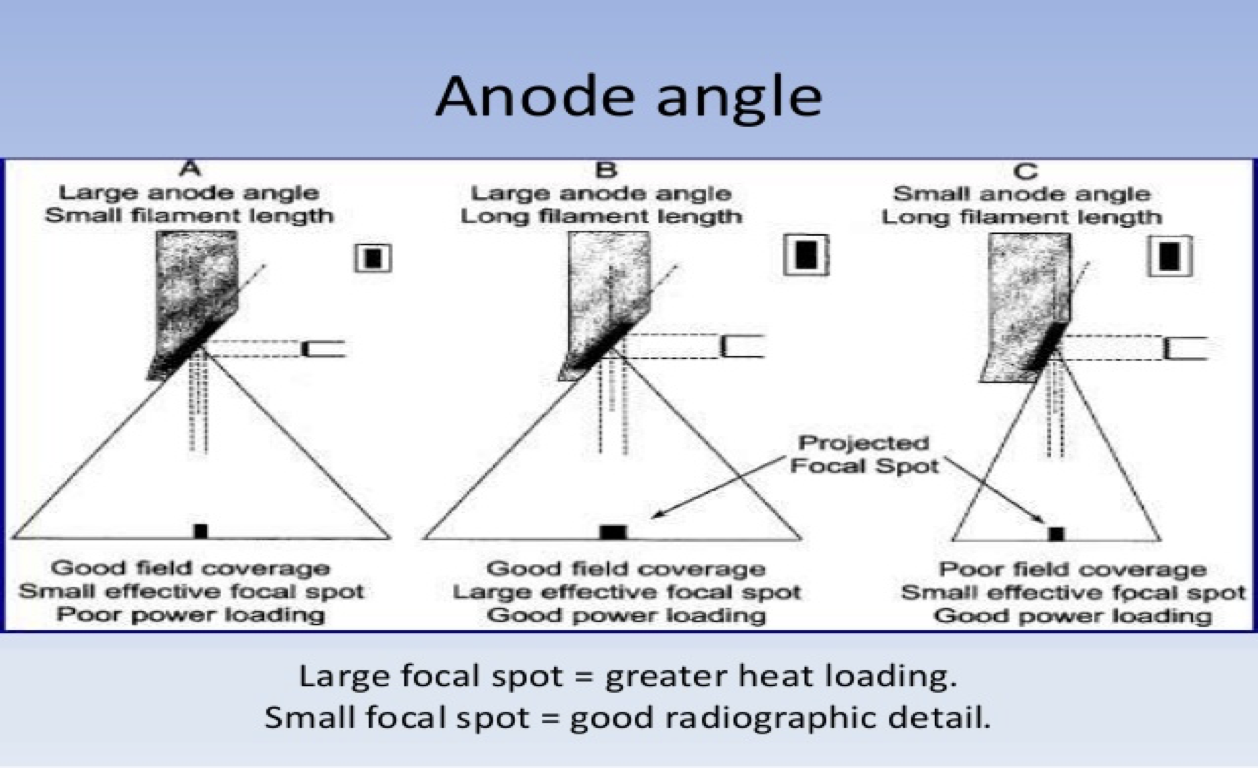
line focus principle
Relationship between the actual focal spot on the target and the effective focal spot- toward the patient
effective focal spot size vs actual
always smaller
smaller anode angle does what
reduces the size of the effective focal spot size
Allows for best resolution while keeping the actual focal spot large to increase heat capacity
off focus radiation
Electron interactions in the tube away from the anode focal spot
These photons can leave as leakage radiation- a form of scatter
how much of the beam do off focus radiation make up
1%
how to reduce off focus in primary beam
Shuttering-collimation can reduce off-focus radiation in primary beam
off focus radiation affects spatial resolution, T/F
true, decreases
off focus radiation affects contrast resolution T/F
true, decreases
what affects heat capacity
time—- smaller = better capacity
mA— smaller = better capacity
mAs— smaller = better capacity
filament size— larger = better capacity
focal spot— larger = better capacity
anode angle— larger = better capacity
rotating anode/speed— faster = better capacity
change mAs how much to see a noticeable difference
30%
mA is
and quantity relationship
direct, tube current- amount of electrons flowing through the tube- higher mA/current= higher quantity
exposure time and quantity relationship
direct, time electrons are in the tube and being created – increase time= increase quantity
kVp and quantity relationship
direct
filtration and quantity relationship
indirect, increases average energy- increase filtration= decrease quantity
distance and quantity relationship
indirect, inverse square law- increase distance decrease quantity hitting the IR
how much change in kVp before see change in receptor exposure
10%
kVp and quality relationship
direct, increase kVp= increases quality/energy/penetration= decrease patient dose
filtration and quality relationship
increase filtration= increase quality/ average energy= decreases patient dose
brems interaction
electrons interact with nucleus of target material
The closer electron get to nucleus the more energy the electron loses= the more energy the photon has
Energy is not lost- photon takes on the energy the electron loses
what xrays always in the beam
brems bc has no minimum or maximum energy
characteristic xrays
Electron interaction with k-shell electron- ionization
Photon energy= cascade effect= binding energy of k-shell- binding energy of electron that fills the void
cascade effect
when an electron fills the void of a ionized electron
remnant radiation
attenuated beam- what is remaining in the beam after it passes through matter
attenuation and what contributes to it
reduction in intensity due to absorption and scatter in matter- transmission/penetration, absorption, scatter
what is attenuation dependent on
Part thickness- more mass, more scatter, more attenuation
Tissue density- more dense areas with more mass attenuate more
Atomic number- different structures in body attenuate differently- higher atomic number increases attenuation
Beam energy- lower energy will penetrate less and attenuate more
Pathologies- additive vs destructive
compton interaction
Most common- occurs at all energy levels- main interactions at high energy levels
Outer shell interaction
Ionization- electron knocked out is Compton electron
Remaining photon has decreased energy and scatter away in different direction
what doses does compton contribute to
occupational and pt
Ionized free electron is absorbed in tissue contributing to pt dose
scatter effect on image
Scatter adds noise/fog to image
photoelectric interaction
Main interaction at low energy levels
Inner shell interaction
Ionization- electron is removed making the atom unstable- ejected electron is photoelectron- gets absorbed by tissue and cells
Cascade effect occurs creating characteristic photon- which gets absorbed in the surrounding tissue
what does photoelectric contribute to
Increases patient dose- does not affect occupational dose- increases image quality- differential absorption/attenuation
photoelectric effect on image quality
increases
types of distortion
size and shape
shape distortion caused by
Angle of tube
Angle of part
Angle of IR
motion
shape distortion caused by
Angle of tube
Angle of part
Angle of IR
motion
CR is
cassette based
sampling frequency
CR- pixels samples per mmm as laser scans imaging plate. affects spatial resolution
steps of the reader/digitizer
Steps 1: rollers extract plate from housing
2: helium neon laser light passes though focusing lenses and reflects off a mirror to read plate in a back and forth (raster pattern)
(left to right line by line- like we read)
3: phosphor release energy stored in the form of light photons when hit by the laser- photostimulable luminescence
4: Photomultiplier tube collects and amplifies the light photons making them brighter
5: light sent to ADC- converted to digital image
6: plate exposed to bright white fluorescent light to release and erase any remaining latent image
raster pattern
left to right line by line
photostimulable luminescence
phosphor release energy stored in the form of light
Photomultiplier tube
collects and amplifies the light photons making them brighter
indirect radiology uses
Uses a TFT or CCD
main conversion of indeirect
Converts x-ray photons to light and then to an electrical charge
Scintillation layer made of
phosphors (absorption layer)- Cesium Iodide or Gadolinium Oxysulfide
how is light emitted in indirect and why is that not ideal
xrays photons are converted into light- emitted isotropically- potential for loss of light or information decreasing spatial resolution
photodiode/photodetector
light to electrical signal
TFT- array/matrix of detector elements
Each DEL contains an active element- the pixel,
storage capacitor- stores electrical charge, and
switch- releases the charge leaving each DEL to send to computer for processing
active element in DEL
pixel
what does switch do in TFT
releases the charge leaving each DEL to send to computer for processing
CCD scintillatoin layer
coupled to a sensor chip by lens or fiber optics
CCD chip
converts light photons to electrical signal and sends to computer for processing
increase phophor size effect on image quality
decrease in resolution- loss of light/image
increase phophor thickness effect on image quality
decrease in resolution- loss of light/image
direct does what
Converts x-rays directly to electrical charge
Non-scintillation
Direct Absorbing and conversion layer
photoconductor- Amorphous selenium
how does A:Se work
High voltage charge is applied across the surface before exposure, this causes the selenium atoms to release electrons in response
FOV
diameter of the area being imaged
matrix
arrangement of squares- rows and columns- collection of pixels
pixel pitch
space between pixels- center of one to center of adjacent smaller pitch= smaller pixels
pixels
picture element- each square represents a shade of gray
pixel size equation
FOV/matrix
spatial resolution
sharpness of recorded detail-lp/mm
Ability of system to differentiate between adjacent structures
Measure of the smallest detail that can be recorded
spatial resolution measured in
lp/mm
MTF
modular transfer function- measure of the systems ability to transfer object information to the receptor
smaller FOV means
decrease in pixel size
larger matrix means
more pixels-smaller pixel size
smaller pixels means
better spatial resolution
what affects spatial resolution in digital
Pixel size
Pixel pitch
Pixel denisity
Sampling frequency-CR- pixels samples per mmm as laser scans imaging plate
Fill factor- ratio of light sensing area to size of entire dell
DQE- measure of effectiveness of imaging device to convert incident photons to electrical signal
fill factor
ratio of light sensing area to size of entire DEL
DQE
detective quantum efficiency- measure of effectiveness of imaging device to convert incident photons to electrical signal