Exam III Study Guide: Reproductive Physiology
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
What are the barriers to sperm cell transport in the female reproductive tract?
1. Cervix and cervical crypts: privileged pathways remove non-motile sperm. 2. Uterus and uterine glands create an immune reaction to sperm. 3. Oviduct/uterotubal junction: smallest portion of the female tract where uncapacitated sperm can get stuck.
What events are associated with the capacitation of sperm cells?
1. Cholesterol efflux increases membrane fluidity, altering surface proteins and making the membrane more permeable. 2. Sperm cell hyperactivation occurs, allowing more calcium to enter, causing rapid contraction of flagella for increased movement.
What is the makeup of the zona pellucida and how do sperm cells interact with it?
The zona pellucida consists of three proteins: ZP-1 (structural support), ZP-2 (reacts with acrosome-reacted sperm), and ZP-3 (contains receptor JUNO that binds sperm protein ligand IZUMO, inducing the acrosome reaction). Acrosin in sperm vesicles allows penetration and release of male genetic material.
What is the purpose of the zona block and how does it occur?
The zona block prevents polyspermy. Cortical granules release the enzyme ovastacin, which cleaves ZP-2, altering the zona pellucida structure and hardening it to prevent further sperm binding.
Describe the process of sperm interaction with the oocyte after penetrating the zona pellucida.
After penetration, the sperm binds to the oocyte's plasma membrane via Izumo1 and Juno, triggering membrane fusion. This allows the sperm's nucleus to enter the oocyte, causing a calcium increase that initiates the cortical reaction and the completion of the oocyte's second meiotic division, leading to fertilization.
What is the difference between facultative and obligate delayed implantation?
Facultative delayed implantation is influenced by environmental factors (e.g., nutrition), while obligate delayed implantation occurs as a regular phase in the reproductive cycle.
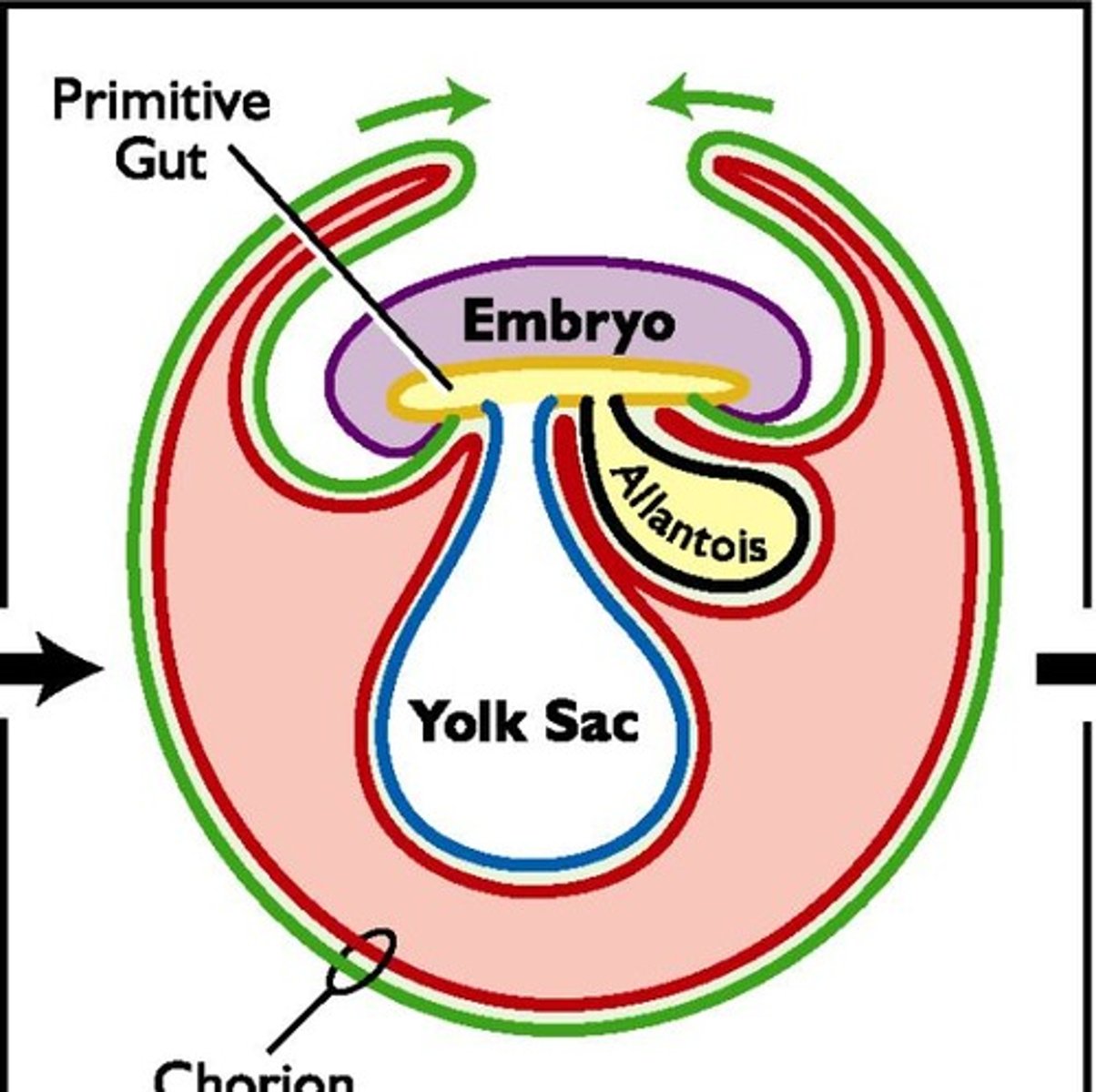
What are the stages of embryonic development after fertilization?
After fertilization, a zygote forms, then divides to create a morula, which compacts and forms a blastocyst through osmotic pressure. The blastocyst hatches from the zona pellucida and begins embryonic development, starting with the primitive gut and undergoing gastrulation to form three germ layers: ectoderm, mesoderm, and endoderm.
How does maternal recognition of pregnancy occur in sows, cows, and humans?
Sow: Estradiol from the conceptus causes PGF2a secretion into the uterine lumen, preventing luteolysis. Cow: IFN-t from the conceptus blocks oxytocin receptors, maintaining progesterone levels. Human: Chorionic gonadotropin supports ovarian progesterone production.
What are the classifications of placentation and examples of each type?
Types include: Diffuse (pigs, horses), Cotyledonary (ruminants), Zonary (dogs, cats), Discoid (rats, primates). Histological attachment types: Epitheliochorial (ruminants), Endotheliochorial (dogs, cats), Hemochorial (humans, rats).
What functions does the placenta perform?
The placenta facilitates nutrient transfer from mother to fetus, waste removal from fetus to mother, provides protection, and produces hormones like progesterone and chorionic gonadotropin.
What physiological events lead to parturition?
Maturation of the fetal HPA axis increases fetal cortisol, triggering hormonal shifts that decrease progesterone and increase estrogen. Rising estrogen enhances uterine sensitivity, promotes oxytocin receptor expression, and increases PGF2α production, leading to uterine contractions and cervical dilation. The Ferguson reflex activates oxytocin release, amplifying contractions until delivery.