irreversibile cell injury and cell death
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
54 Terms
what is the "point of no return"?
it is the point where the injury to the cell is no longer reversible, and will lead to cell death
irreversible cell injury leads to....
cell death
what are the 2 types of cell death?
1. death by swelling- necrosis/oncosis
2. death by shrinking- apoptosis
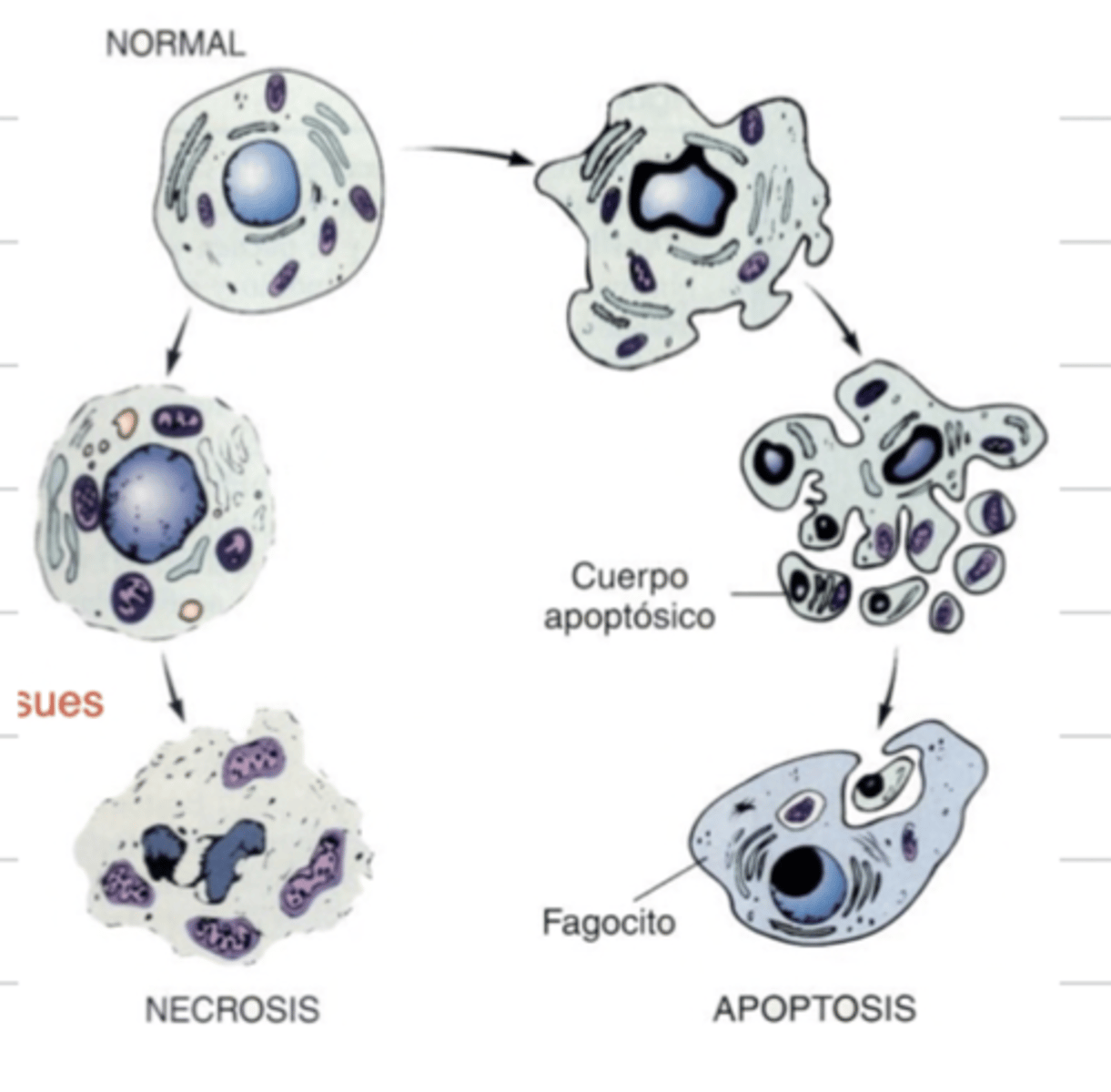
death of a cell by swelling is called....
necrosis/oncosis
death of a cell by shrinking is called....
apoptosis
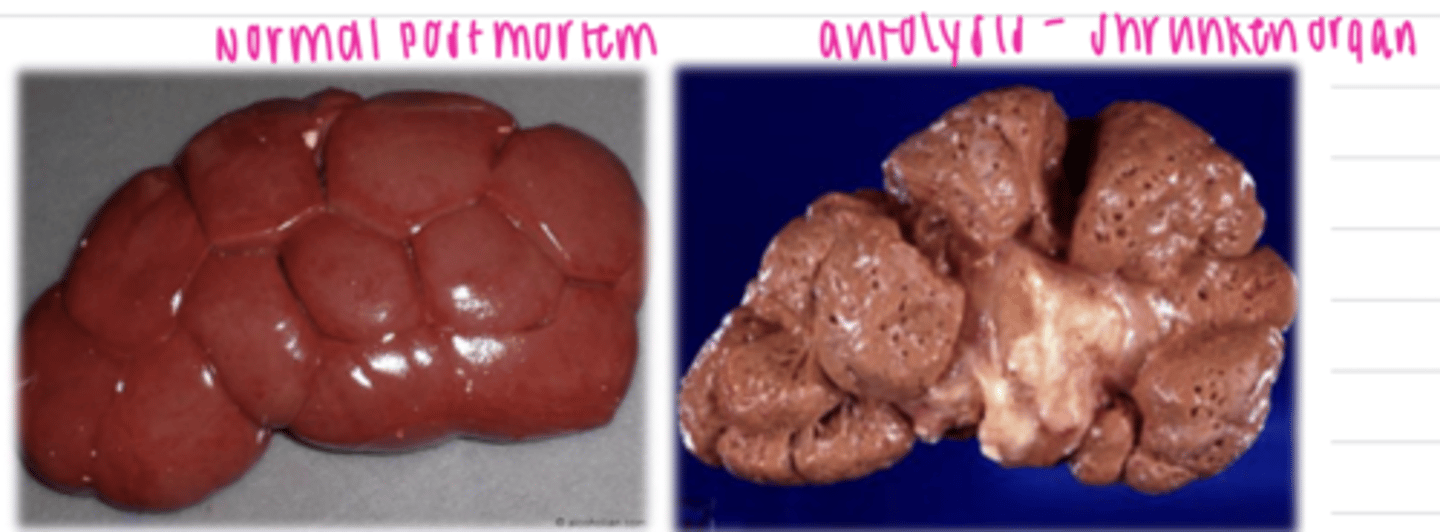
what is the difference between necrosis and autolysis?
necrosis is pathological and is the death of living cells
autolysis is physiological, and is the post-mortem degeneration of cells
autolysed organs appear....
shrunken
what are the possible ways that the nucleus can change after cell death?
-pyknosis: shrunken, dark, homogenous, round
-karyorrhexis: ruptured, dark fragments in cytoplasm
-karyolysis: pale due to dissolution of chromatin
-absence of nucleus: later stage of karyolysis
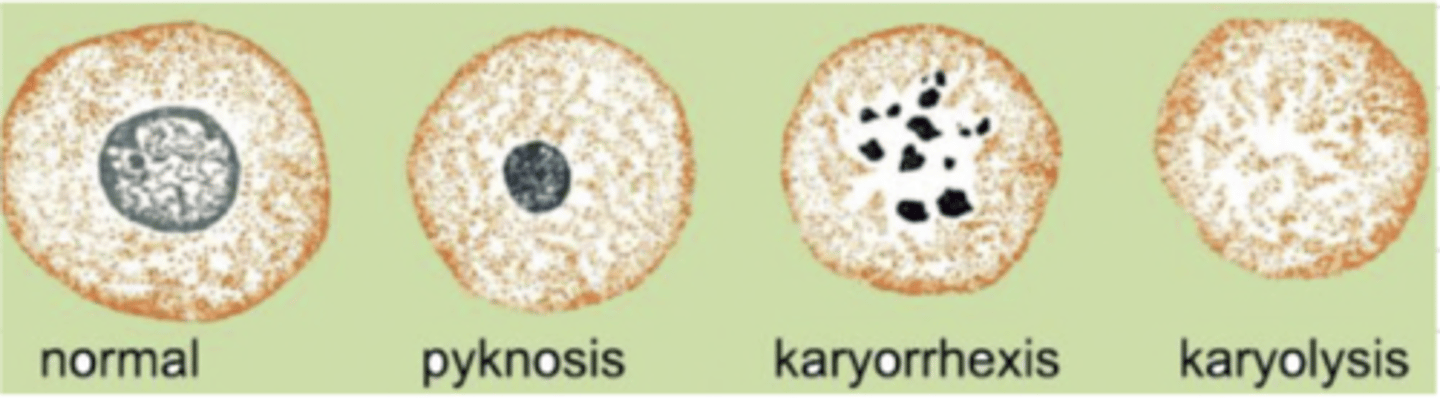
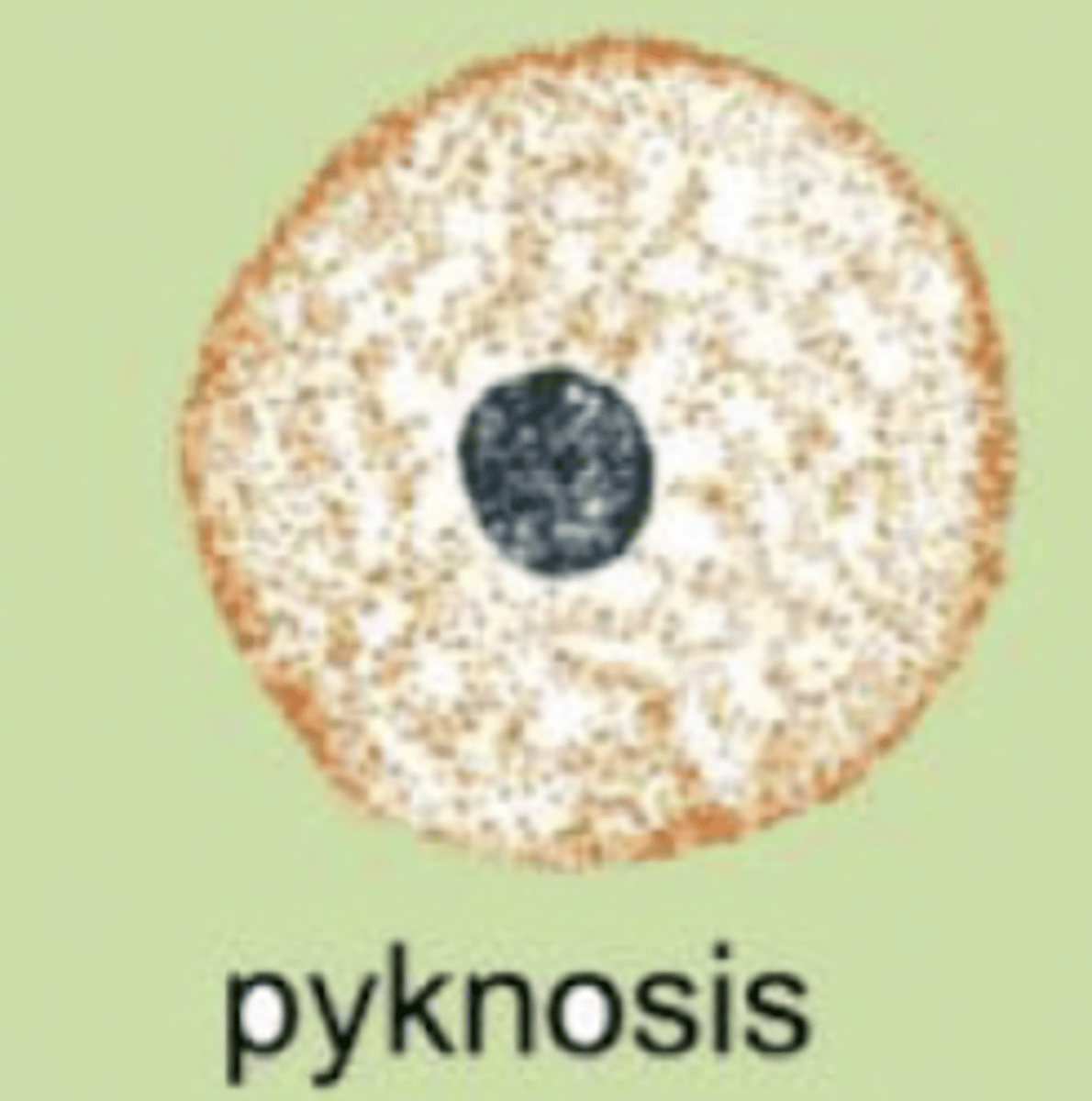
what is pyknosis?
the condensation of chromatin in the nucleus of a cell due to cell death. the nucleus appears shrunken, dark, homogenous, and round
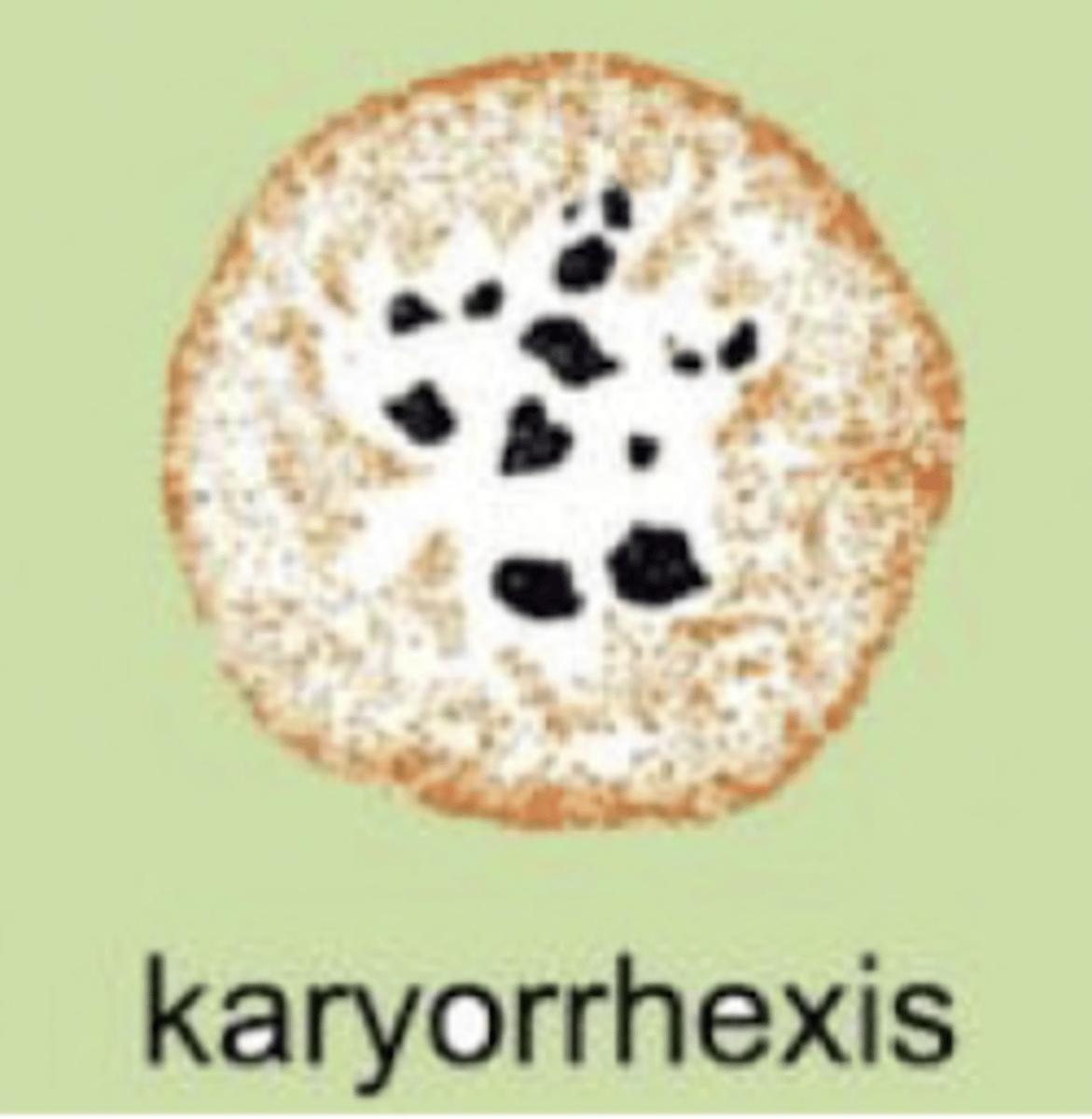
what is karyorrhexis?
the fragmentation of the chromatin after cell death. the cell has fragments irregularly floating within the cytoplasm
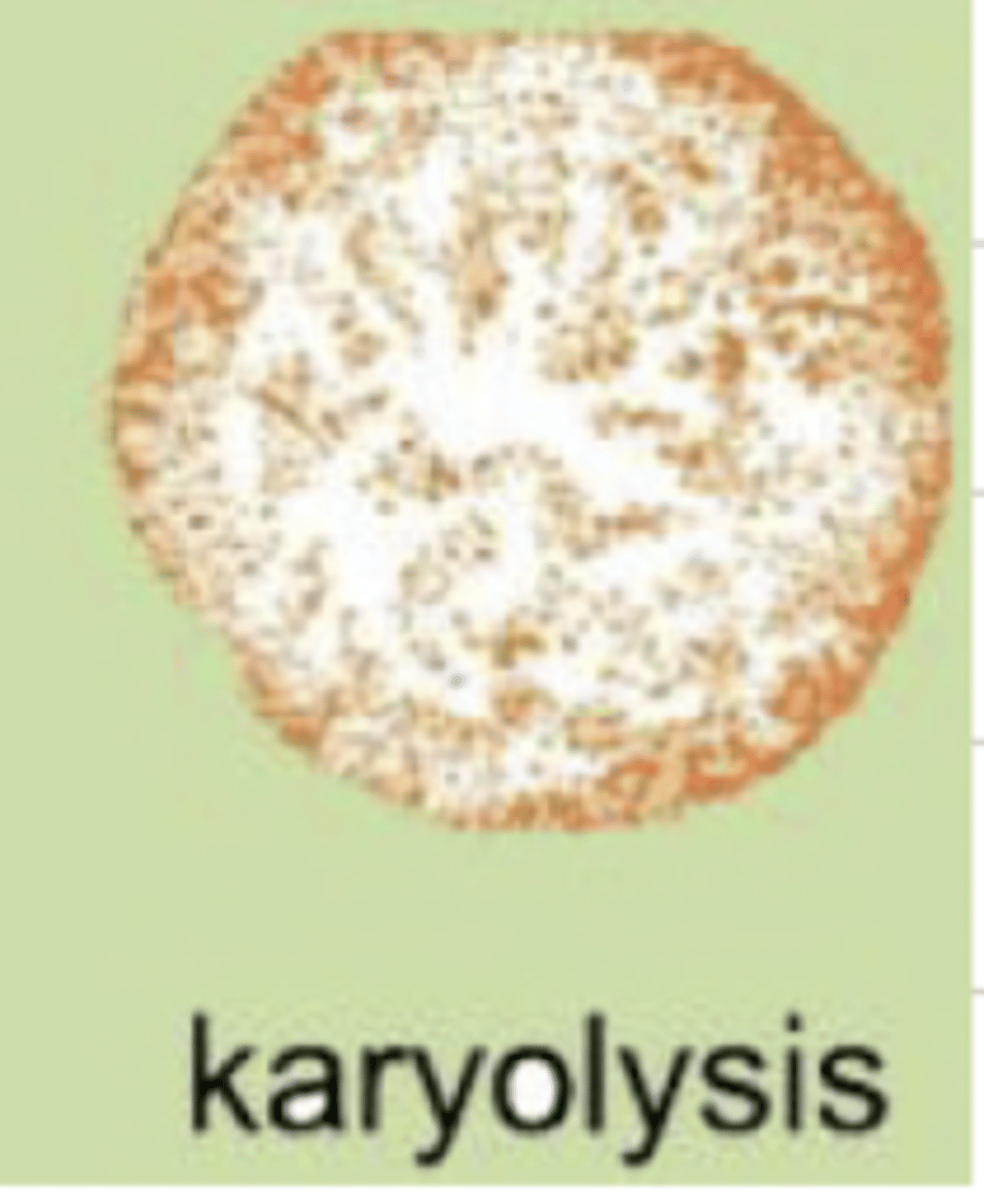
what is karyolysis?
the dissolution of chromatin after cell death. the nucleus is pale and will disappear completely
what are the 2 instances that tell us the cell has reached a point of no return?
1. inability to restore mitochondrial function
2. obvious cell membrane damage
if an injured cell cannot restore mitochondrial function and has obvious cell membrane damage, we say that it has reached the ...
point of no return
what are the effects of free radicals?
-peroxidation of membrane lipids
-oxidative changes of proteins
-DNA damage
what occurs when a cell has obvious membrane damage?
there will be an influx of Ca2+, which activates enzymes (ATPases, endogenous phospholipases, proteates, endonucleases), including arachidonic, acid, which attracts an immune response, causing inflammation
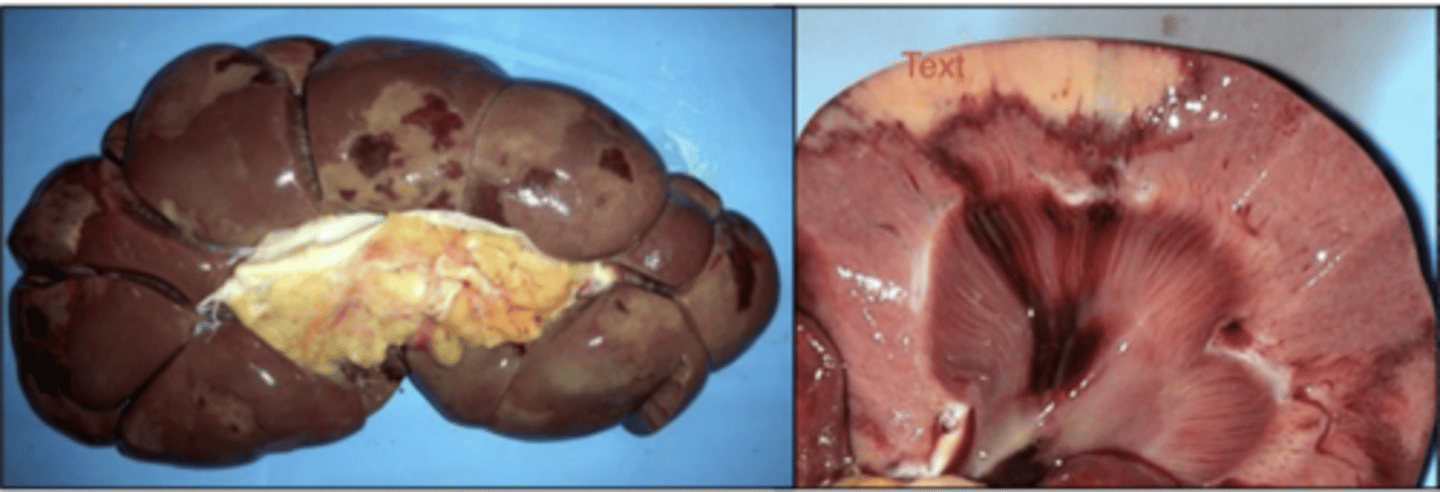
what are the causes of coagulative necrosis?
hypoxia, ischemia, toxins
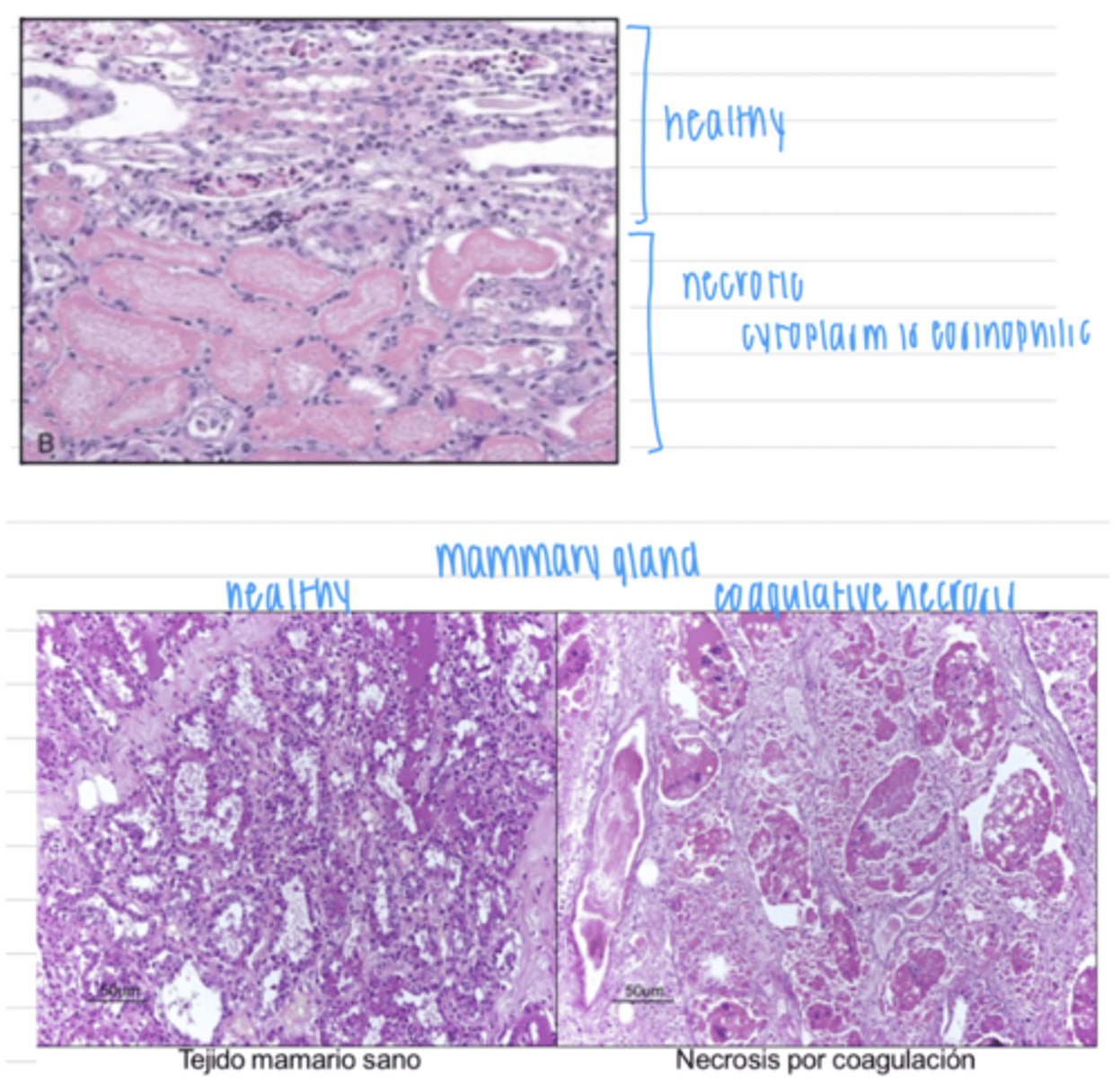
describe coagulative necrosis
necrosis caused by ischemia, hypoxia, or toxins, where the organ and cell structures are preserved by coagulation of proteins. the color and texture changes, but the structure stays the same. proteins are denatured.
the necrotic tissue will be phagocytized and lysed in a few days, and a scar will replace the dead tissue
which type of necrosis leaves the tissue structure completely normal?
coagulative necrosis
in coagulative necrosis, proteins are denatured, which causes what microscopic appearance?
pyknotic, karyorrhetic, or absent nucleus
eosinophilic cytoplasm
what is the consequence of a tissue that has died by coagulative necrosis?
it will be phagocytized and lysed in a few days, with a scar replacing the dead tissue. the animal can survive.
coagulative necrosis is typical in what organs?
liver, kidney, muscle
it can be found anywhere, except nervous tissue
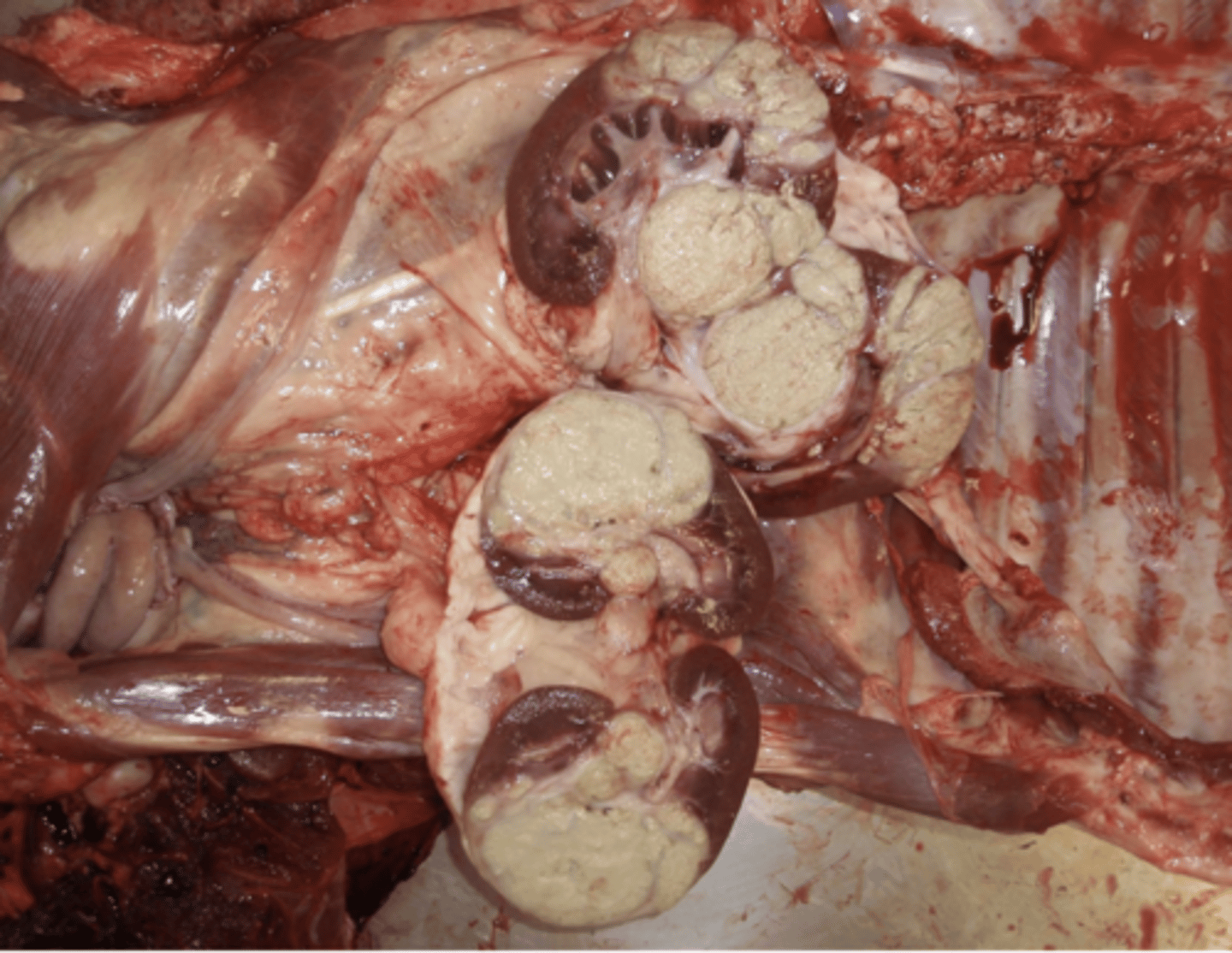
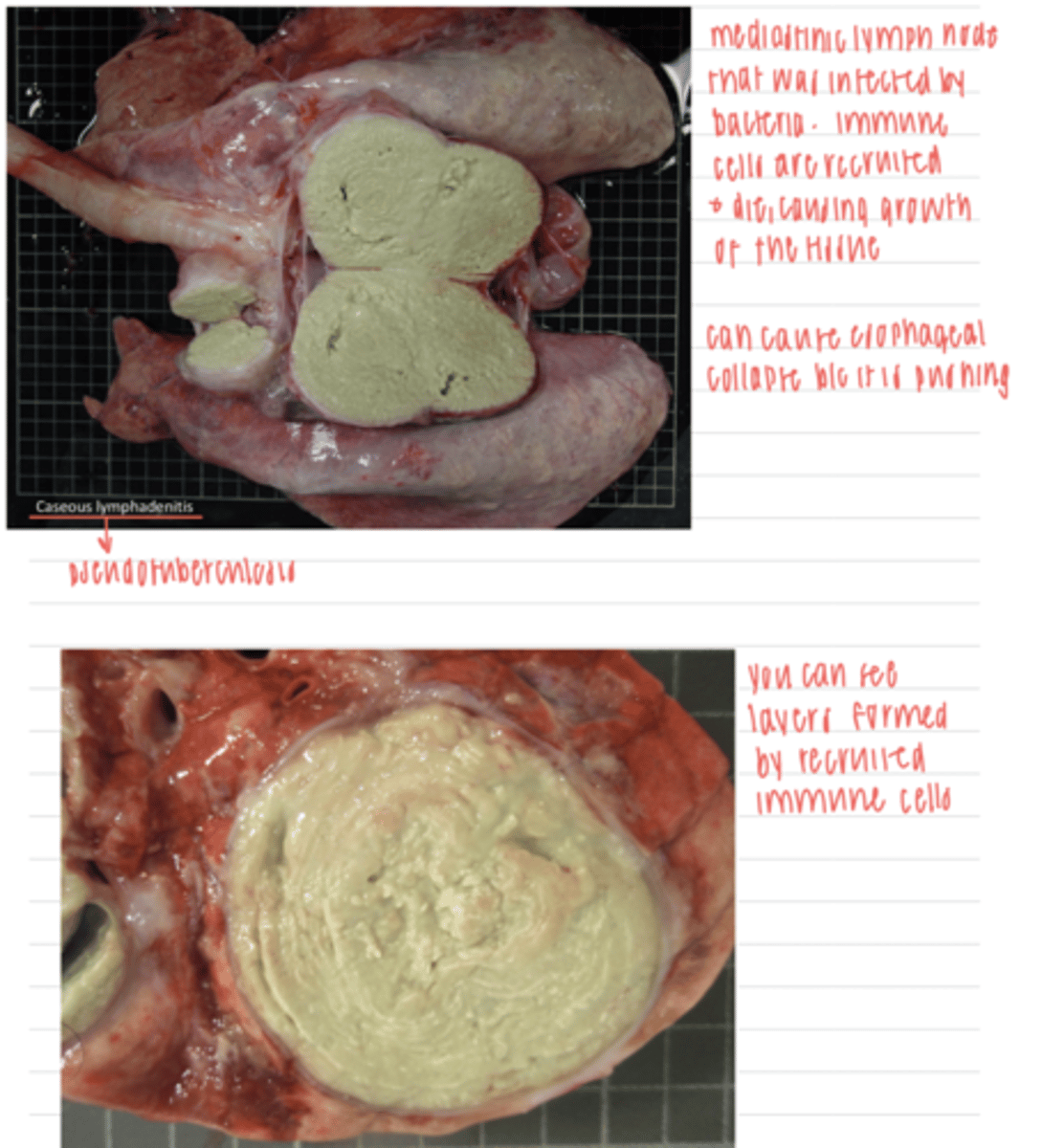
caseous necrosis is typical of what disease?
tuberculosis
what type of necrosis leaves the tissue granular and friable?
caseous necrosis
which is more chronic- coagulative or caseous necrosis?
caseous
caseous necrosis is common in what tissues?
lungs, lymph nodes
can be seen in any tissue
can any tissue undergo coagulative necrosis?
no- nervous tissue cannot
can any tissue undergo caseous necrosis?
yes
how does a tissue that underwent caseous necrosis appear?
grossly:
surrounded by an external fibrous capsule
yellow
sometimes hard
microscopically:
foci of nuclear and cytoplasmic remains
dead leukocytes
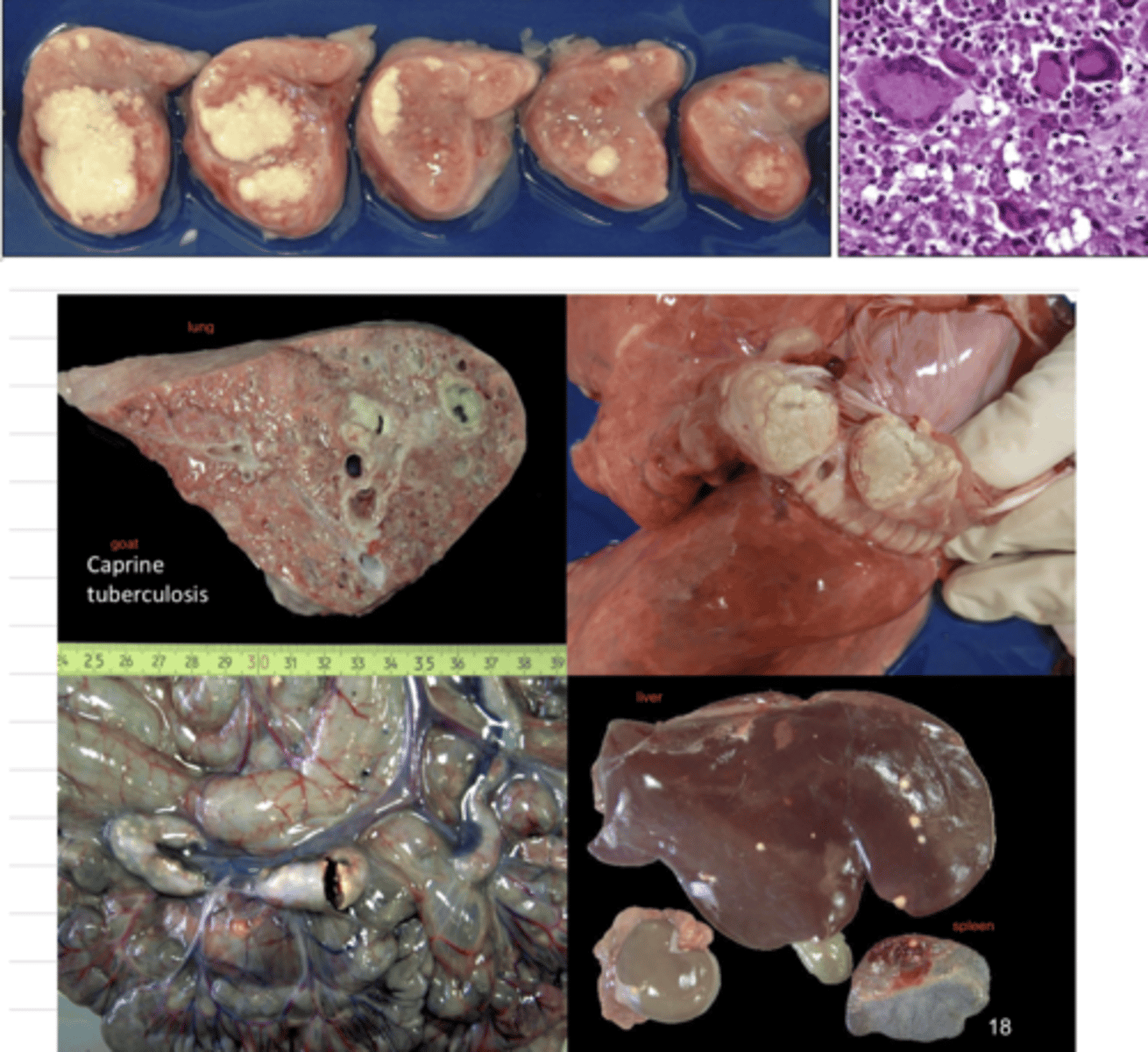
which type of necrosis leaves the tissue with a cheese-like appearance?
caseous necrosis
what type of necrosis does this describe:
In the development of this lesion, bacteria wall degradation plays a key role, causing a foci of _________ necrosis, surrounded by granulomatous inflammatory cells and a external capsule of fibrous tissue
caseous necrosis
how does a caseous necrosis lesion change over time?
more immune cells are recruited and die, causing growth of the tissue. the tissue also hardens because it accumulates calcium ("dystrophic calcification")
in the CNS, what type of necrosis will be observed due to hypoxia?
liquefactive necrosis
in the CNS, what is the cause of liquefactive necrosis?
hypoxia
what happens to the tissue that dies by liquefactive necrosis?
in the CNS, the spaces that are left will fill with lipidic remains and fluids
in other tissues, it will become an abscess, which can even become caseous if the liquid is lost or hardens
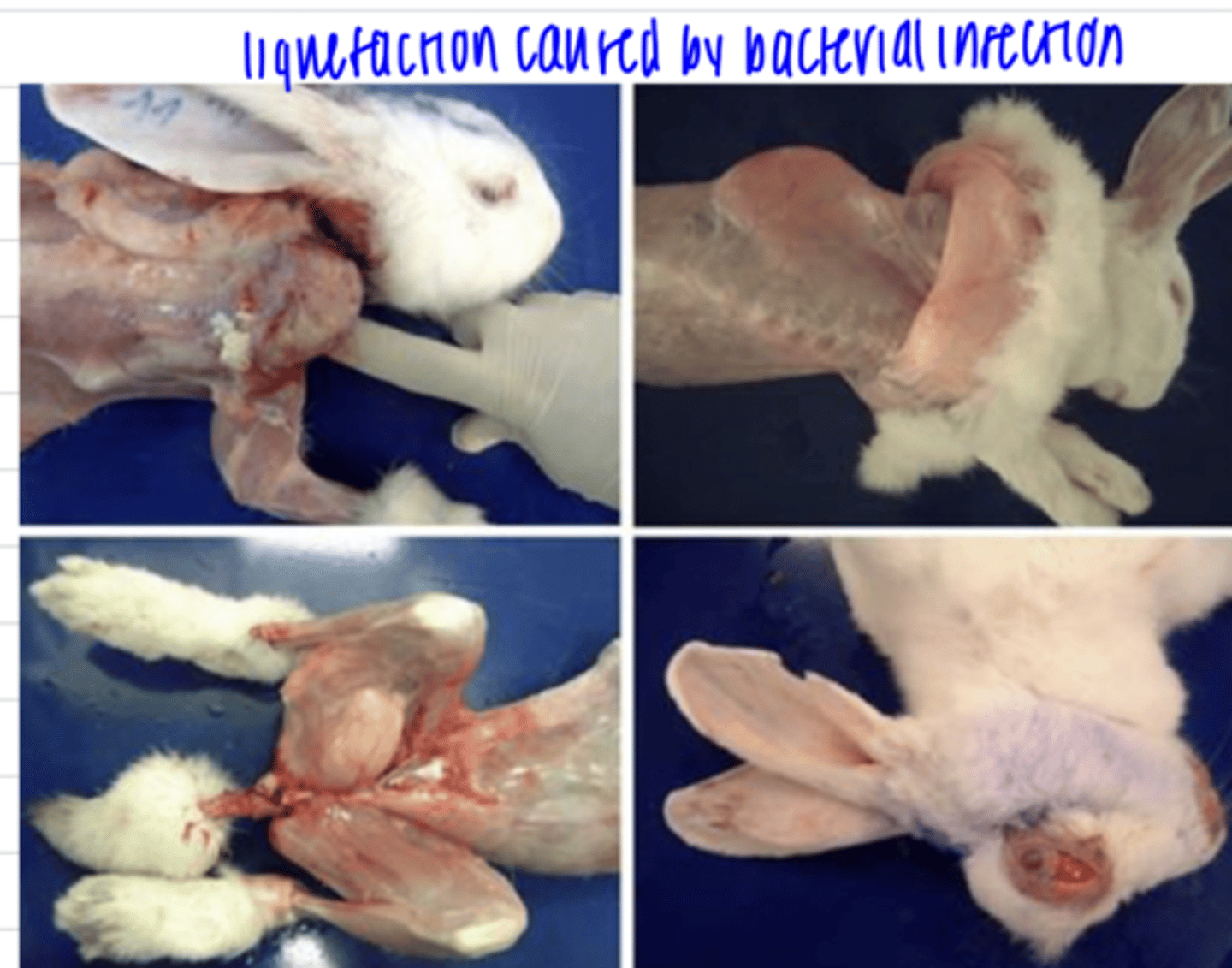
what is the cause of liquefactive necrosis?
pyogenic bacteria infection
OR if it is in the brain, hypoxia

pyogenic bacteria infections can cause ______ necrosis
liquefactive
what is wet gangrene?
lesion produced when a tissue with coagulative necrosis is further degraded by saprophytic bacteria that have contaminated it from the environment. the bacteria cause putrifaction of the tissue, leaving a soft, moist, red-brown-black tissue.
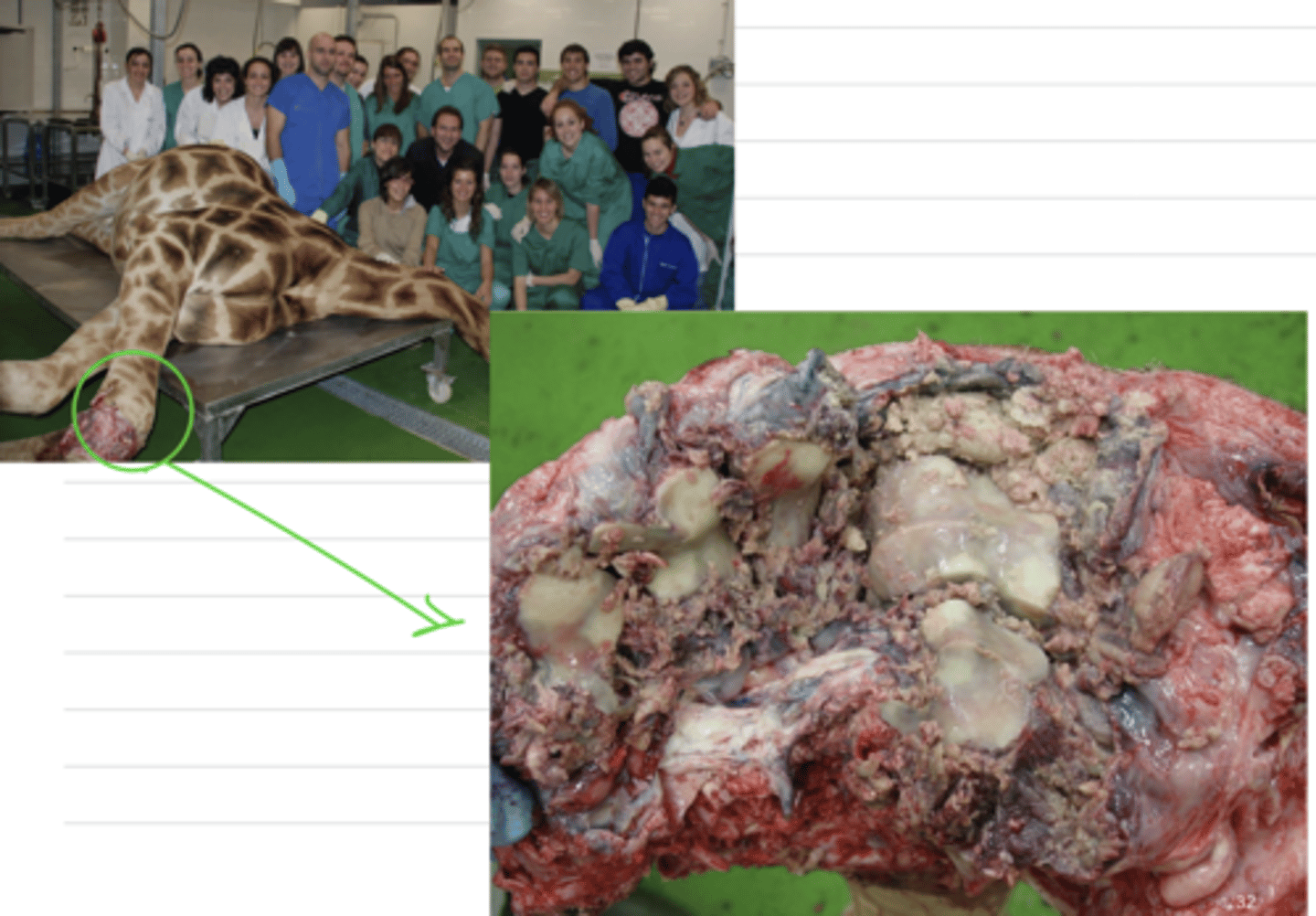
when saprophytic bacteria infect a tissue that already has coagulative necrosis, this produces _______
wet gangrene
what is the appearance of a tissue with wet gangrene?
soft, moist, red-brown to black, sometimes with gas bubbles

what is the danger of wet gangrene?
it can spread to other parts of the body if it is not separated.
we must remove the necrotic tissue and clamp it to prevent the spread of the toxins into the blood.
dry gangrene results from.....
loss of blood flow to a specific part of the body, caused by toxins or cold. the tissue will mummify/solidify.
which type of gangrene is produced by the effect of bacteria?
wet gangrene
gas gangrene
how does dry gangrene appear?
shriveled, dry, brown-black
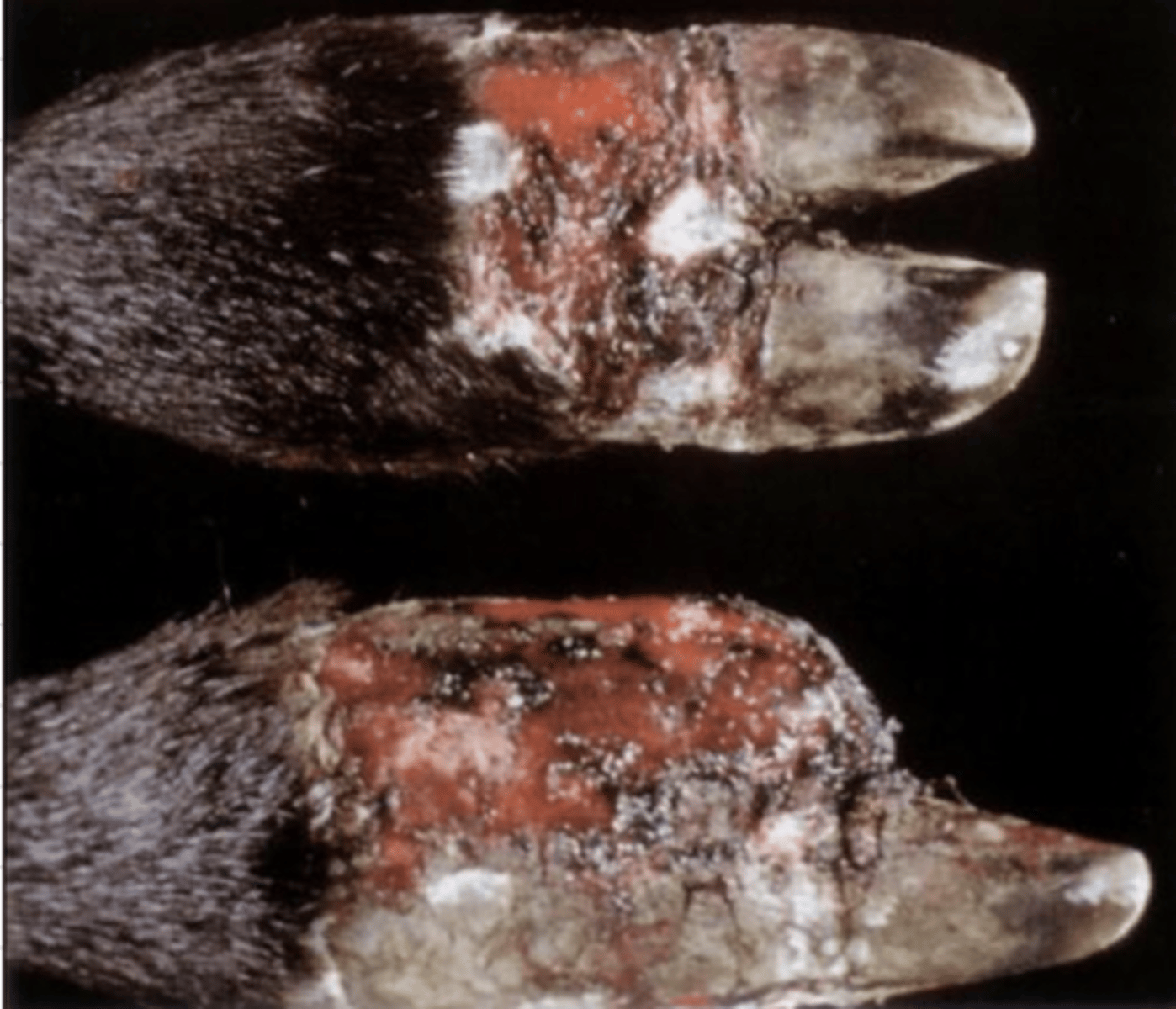
what is the cause of dry gangrene?
loss of blood flow to a specific part of the body due to toxins or cold
some toxins cause vessel constriction, leading to lack of blood flow
intense cold can cause freezing and cell damage by forming crystals
in what type of gangrene are the tissues depleted of water?
dry gangrene
what causes gas gangrene?
gas-producing (anaerobic) bacteria infecting necrotic tissue
when gas-producing (anaerobic) bacteria infects necrotic tissue, what is the result?
gas gangrene
how does gas gangrene appear?
grossly:
dark red-black
gas bubbles and fluid
microscopically:
coagulative necrosis
serohemorrhagic exudate
gas bubbles

in which organ is fat necrosis the most common?
pancreas- due to pancreatic lipases
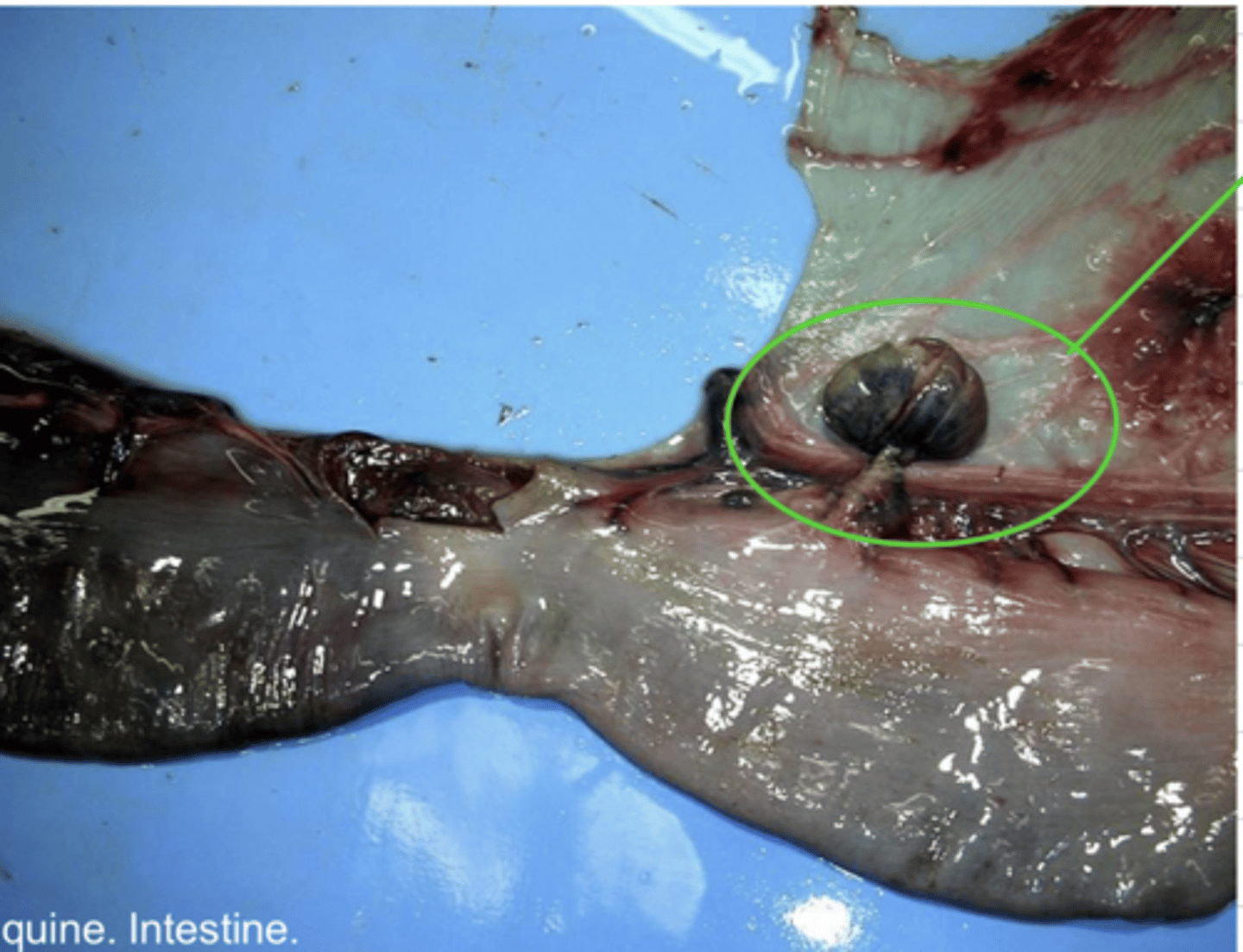
what are the 2 types of fat necrosis?
1. traumatic fat necrosis- this is where adipose tissue is crushed (common in pelvic fat and subcutanenous tissue)
2. abdominal fat necrosis- this occurs in cattle, the cause is unknown. in the mesentery, omentum, and retroperitoneum. can cause intestinal stenosis if it involves fat surrounding the intestines.
traumatic fat necrosis is common where in the body?
pelvic fat
subcutaneous tissue
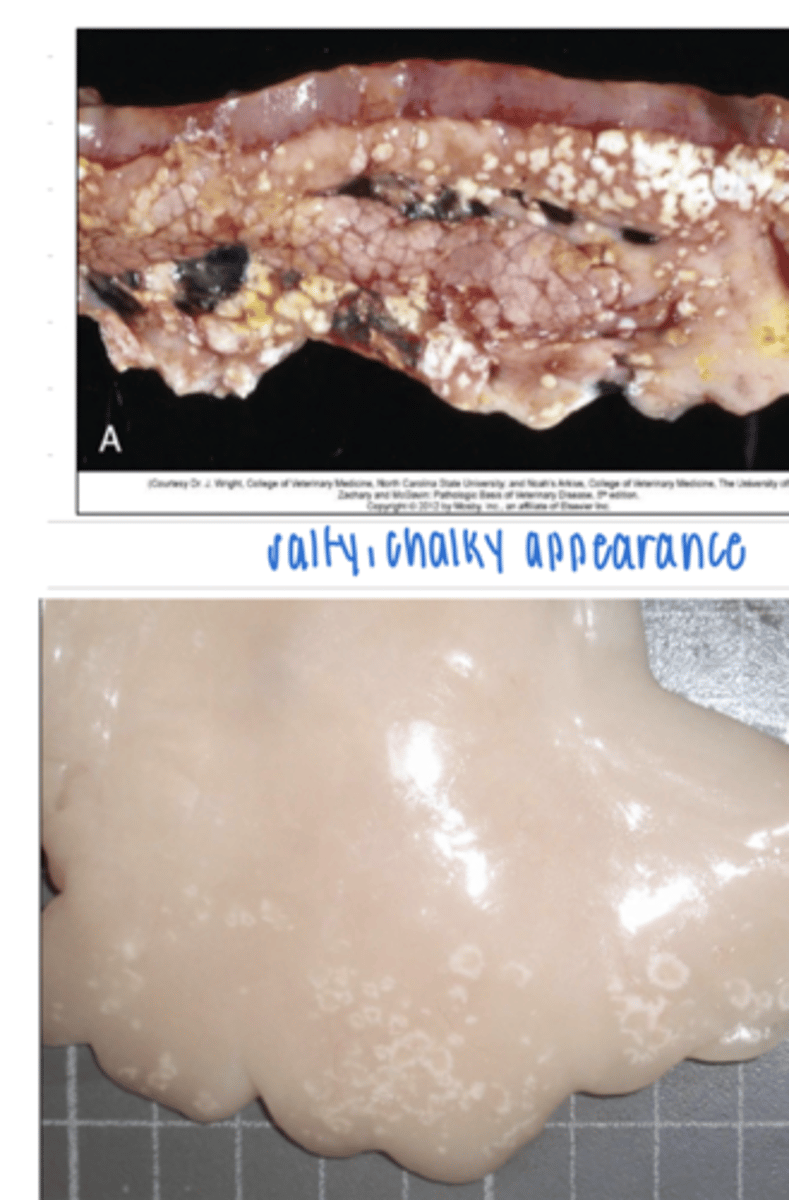
how does fat necrosis appear?
grossly:
dry, salty
microscopically:
if there is saponification, necrotic adipocytes are basophilic
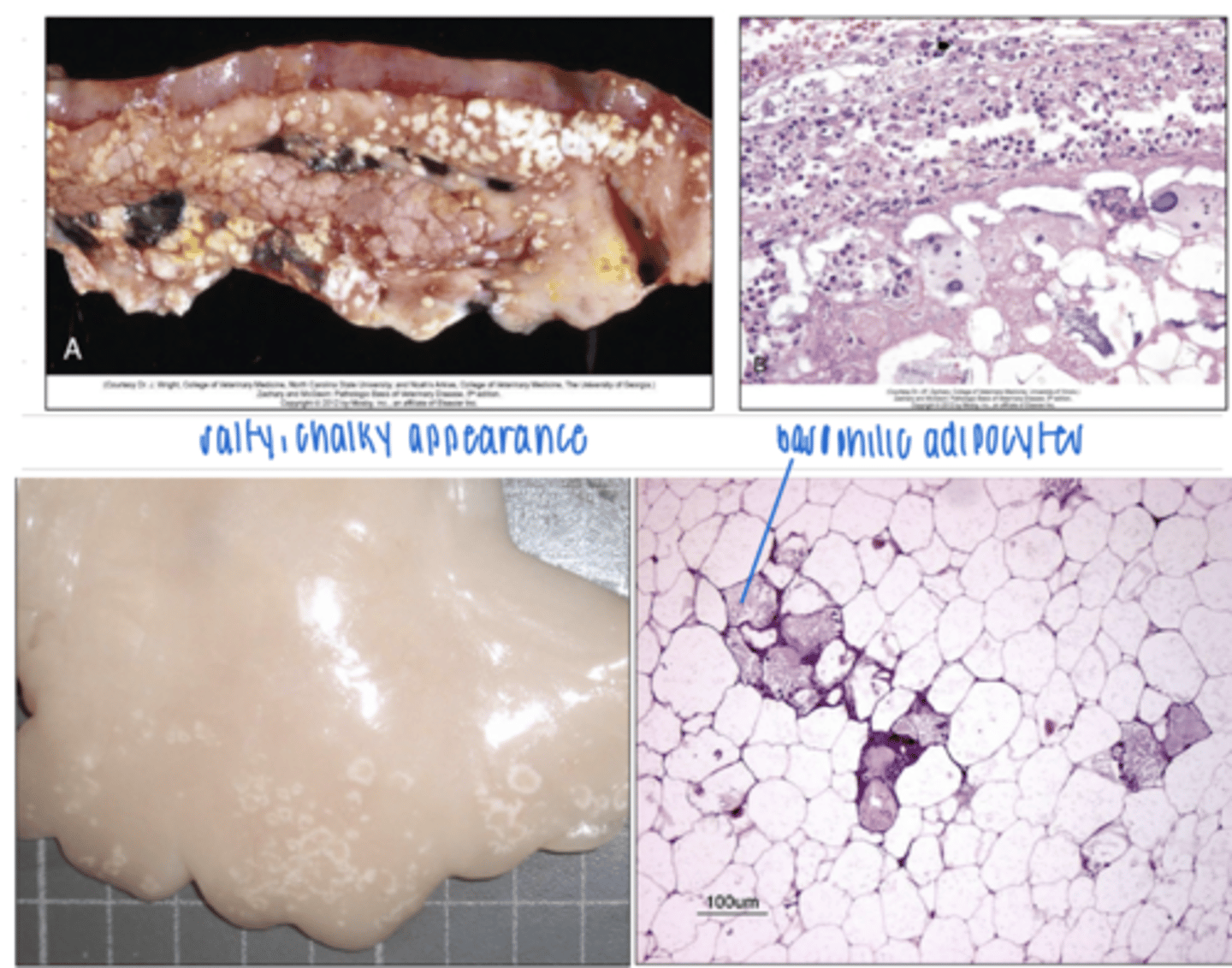
what type of necrosis has a dry and salty appearance?
fat necrosis
what are the consequences of necrosis?
inflammation
irritation and sequestrum if it cannot be degraded