Clostridioides difficile
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
29 Terms
Clostridioides difficile
Most frequent infectious cause of healthcare-associated diarrhea in hospitalized patients (North America and Europe)
true
T/F: Exposure to any antimicrobial is the single most important risk factor for CDI.
Toxin A
Enterotoxin strain of C. diff
Toxin B
Cytotoxin strain of C. diff
BI/NAP1/027
Which strain of C.diff is associated with severe CDI, has higher rates of relapse, produces toxin A and B (produces 16x more toxin A and 23x more toxin B), and is fluoroquinolone-resistant?
fluoroquinolone
BI/NAP1/027 is _____-resistant
1. Antibiotic use
2. Advanced age: ≥65
3. Immunocompromised: cancer, HIV
4. GI surgery or manipulation of the GI tract: tube feeding
5. Gastric-acid suppression medications (long-term PPI use)
6. Hospitalization/healthcare exposure
Risk factors for C. diff
- Fluroquinolones
- Clindamycin
- Penicillins and combinations (broad spectrum): Zosyn, Unasyn, Augmentin
- Cephalosporins: generations 2-4
- Carbapenems
Antibiotics that are frequently associated with C. diff
- Macrolides
- Penicillins (narrow spectrum)
- Cephalosporins: 1st gen
- SMX-TMP
- Sulfonamides
Antibiotics that are occasionally associated with C. diff
- Aminoglycosides
- Tetracyclines
- Tigecycline
- Chloramphenicol
- Metronidazole
- Vancomycin
Antibiotics that are rarely associated with C. diff.
Diarrhea
Abdominal discomfort
Fever
Colitis
Fulminant disease
Clinical presentation of C. diff
Malaise
Abdominal pain
Nausea
Anorexia
Watery diarrhea
Low-grade fever
Evidence of colitis
Severe abdominal pain
Perfuse diarrhea
High fever
Evidence of fulminant disease
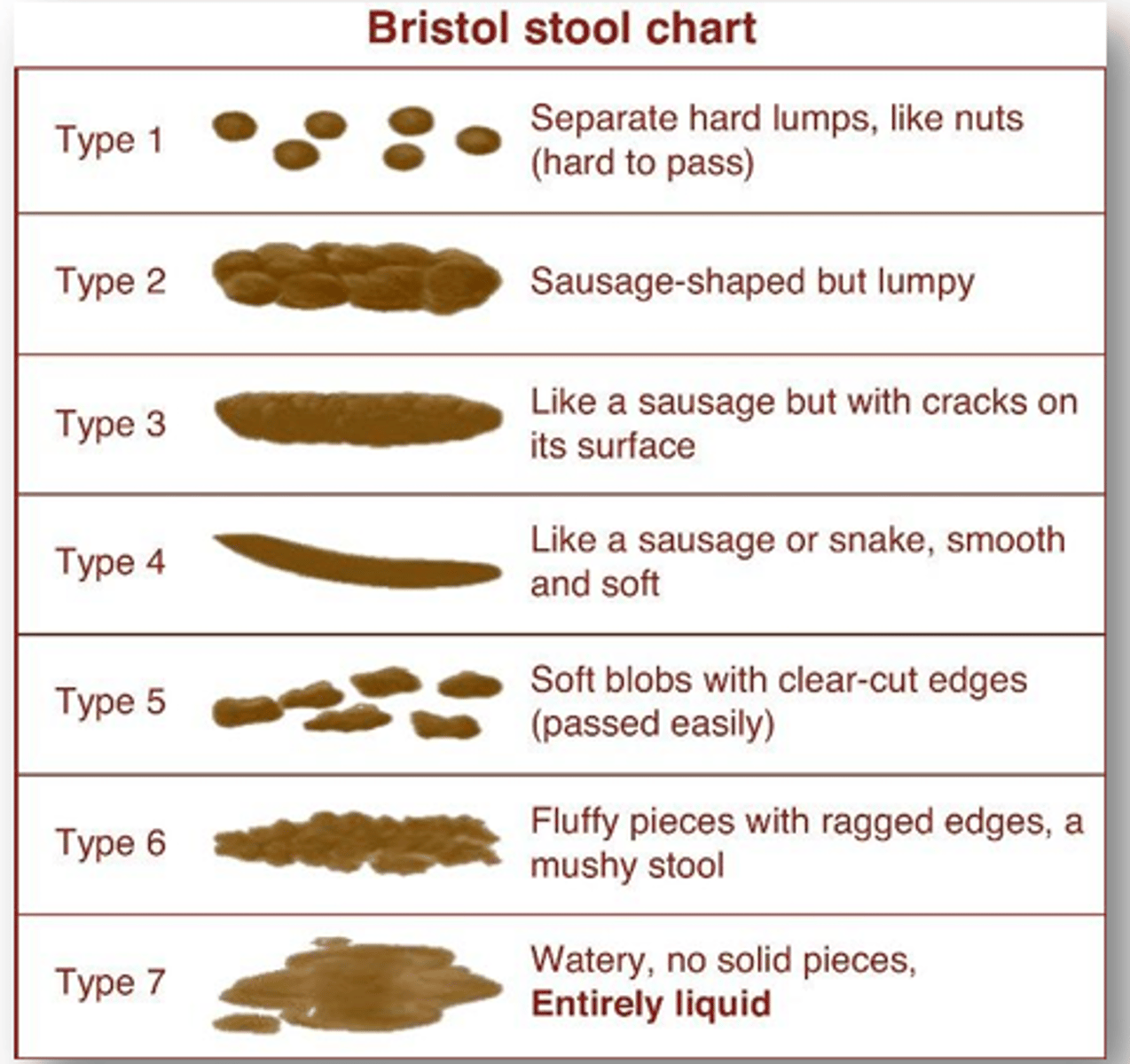
1. Unexplained and new-onset ≥3 unformed stools in 24 hours
2. Stool culture for C. diff
3. Detection of toxin A or B
4. WBC count: marked leukocytosis
5. Endoscopic exam
Diagnosis of C. diff
Colonization:
- NO clinical symptoms present
- Positive C. diff test and/or its toxin
(more common)
Infection:
- Clinical symptoms present
- Positive C. diff test and/or its toxin
How to differentiate between C. diff colonization and C. diff infection?
WBC ≤ 15,000 cells/ml
SCr < 1.5 mg/dL
Which WBC count and SCr level indicate non-severe C.diff?
WBC > 15,000 cells/ml
SCr ≥ 1.5 mg/dL
Which WBC count and SCr level indicate severe C.diff?
Macrolides
Fidaxomicin (Dificid) should NOT be used in patients with an allergy to _____.
Preferred: Fidaxomicin (Dificid) 200 mg BID x 10 days
Alternative 1: Vancomycin (Firvanq) 125 mg PO QID x 10 days
Alternative 2 (if the 2 above are unavailable): Metronidazole (Flagyl) 500 mg PO TID x 10-14 days
Treatment recommendation for initial episode, non-severe C. diff
- WBC ≤ 15,000 AND SCr < 1.5
Preferred: Fidaxomicin 200 mg BID x 10 days
Alternative 1: Vancomycin 125 mg PO QID x 10 days
Treatment recommendation for initial episode, severe C. diff.
- WBC > 15,000 AND SCr ≥ 1.5
Vancomycin 500 mg PO/NGT QID PLUS Metronidazole 500 mg IV Q8H
*If ileus, consider adding rectal instillation of: Vancomycin 500 mg in 100 ml of NS Q6H
Treatment recommendation for initial episode, fulminant
- Hypotension or shock, ileus, megacolon
1. Preferred: Fidaxomicin 200 mg PO BID x 10 days OR Fidaxomicin 200 mg PO BID x 5 days, followed by once every other day x20 days
2. Alternative: Vancomycin tapered and pulsed
- Vanco 120 mg PO QID x10-14 days, then BID x 7 days, then daily x 7 days, then every 2-3 days x2-8 weeks
Treatment of the first recurrence of C. diff (within 90 days)
Vancomycin 125 mg PO QID x 10 days
Could also use Dificid
For the treatment of the first recurrence of C. diff, what is the treatment if Metronidazole was used for the first episode?
Bezlotoxumab (Zinplava) 10 mg/kg IV once during administration of standard treatment regimen
Adjunctive treatment for recurrence of C. diff.
1. Fidaxomicin 200 mg PO BID x 10 days OR 200 mg PO BID x 5 days followed by once every other day x20 days
2. Vancomycin tapered or pulsed OR Vancomycin 125 mg PO QID x 10 days, THEN Rifaximin 400 mg PO TID x 20 days
3. Fecal microbiota transplantation (FMT): used if patient has C. diff >2 times (total of 3 episodes)
Treatment of the second or subsequent recurrence of C. diff
Bezlotoxumab (Zinplava)
- single dose of 10 mg/kg IV over 60 min
A human monoclonal antibody that binds to C. diff Toxin B and neutralizes its effect
- NOT effective if given without the standard treatment of C. diff
- Precaution in CHF patients (exacerbates HF)
- AEs: nausea, pyrexia, headache
Fecal Microbiota Transplantation (FMT)
Investigational treatment for recurrent CDI (RCDI) and failure of appropriate treatment
- administered via nasoduodenal tube or enema
- FDA alert for enteropathogenic E. coli (EPEC) and Shiga-toxin-producing E. coli (STEC)
glove use
The only CDI prevention recommendation with the highest strength of recommendation and quality of evidence; decreases the risk of transmission
true
T/F: For hand hygiene, soap and water are preferred over alcohol-based hand hygiene products.