Exam 1 - Oral Path
1/134
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
135 Terms
How is the formation of the oral and maxillofacial region described?
A complex process
What occurs during development of the oral and maxillofacial region?
Tissues develop and merge
How do oral clefts develop?
Result from disruption of the orchestrated development and merger of tissue processes
Medial nasal processes
Merge with each other to form central part of the upper lip
Occurs during weeks 6 and 7
Maxillary processes
From 1st pharyngeal arch
Merge with nasal prominences to form lateral portions of the upper lip
Occurs during weeks 6 and 7
Primary Palate
Only hard palate
Formed from the merging of medial nasal processes
Forms the intermaxillary segment
Gives rise to premaxilla (triangular bone bearing the four incisors)
Secondary Palate
90% hard and soft palates
Formed from merging of maxillary processes from 1st pharyngeal arch
Components of the Intermaxillary Segment
Labial: Philtrum
Upper jaw: carries four incisors
Palatal: forms primary triangular palate
Palatal shelves
Medial projections of maxillary processes
Growth toward one another
Fusion of palatal shelves begins by week 8 in a cranio-caudal direction
Simultaneous fusion with primary palate and nasal septum
When does complete fusion of the palatal shelves occur?
Week 12
What is the cause of cleft lip?
Defective fusion of medial nasal processes with maxillary process
What is the consequence of a failure of the palatal shelves to fuse?
Cleft palate
Incidence of Cleft Lip And/Or Palate
Cleft lip and cleft palate together
Either Cleft palate or Cleft lip separately
Causes of Syndromic Clefts
Single-gene syndromes
Autosomal dominant
Autosomal recessive
X-linked inherited
Chromosomal anomalies
Idiopathic
Do oral clefts follow a simple Mendelian inheritance pattern?
No, they have heterogeneous causes
What are the three contributing factors to oral clefts?
Heterogenous causes:
Major genes
Minor genes
Environmental factors
Causes of Oral Clefts
Genes
Environmental factors
Maternal alcoholism
Maternal tobacco use
Anticonvulsant therapy
Lateral facial cleft
Lack of fusion of the maxillary and mandibular processes
From the commissure to the ear
Uncommon
What are lateral facial clefts associated with?
Accessory mandible
Absent parotid gland
Peripheral facial weakness
Oblique facial cleft (rare)
Form upper lip to the eye
Due to failure of fusion of lateral nasal process with the maxillary process
Median cleft of the upper lip
Due to failure of fusion of the medial nasal processes
Clefting
One of the most common major congenital defects
Cleft lip
More prevelant unilaterally
Complete Cleft Lip
From the lip to the nostril
Involves the alveolus
Usually between lateral incisor and the cuspid
tooth can be absent in the cleft area (especially the lateral incisor)
Supernumerary teeth may be seen
Incomplete CL
Nose not involved
Severity of Cleft Palates
Depends on structures involved:
Hard and soft palates
Only soft palate
Cleft (bifid) uvula
Less Severe Cleft Palate
Submucous Palatal Cleft
Intact mucosa
Defect of muscles of soft palate
Frequent notch in bone along posterior margin of hard palate
Bluish midline discoloration
Best identified by palpation with blunt instrument
Can be associated with cleft uvula

Key features of Pierre Robin Sequence (or anomalad)
Cleft palate: palatal shelves fail to fuse
Mandibular micrognatia: constraint of mandibular growth in utero
Glossoptosis → airway obstruction due to posterior displacement of tongue (tongue fails to descend)
Can Pierre Robin sequence be isolated?
Yes, it may be isolated or occur with other syndromes/anomalies
What clinical difficulty is common in Pierre Robin sequence?
Respiratory difficulty, especially in the supine position → can cause asphyxia
Treatment of orofacial clefts
Mutlidisciplinary approach:
Pediatrician
Oral and maxillofacial surgeon
Otolaryngologist
Plastic surgeon
Pediatric dentist
Orthodontist
Prosthodontist
Speech pathologist
Geneticist
Leukodema
Common oral mucosa condition
Considered an anatomical variation
Unknown cause
More prevalent in African Americans
More common and severe in smokers
Less pronounced with smoking cessation
Benign condition
Clinical Manifestations of Leukoedema
Mucosa appearance:
• Diffuse, gray-white, milky, opalescent
• Folded surface with wrinkles or whitish streaks
• Lesions do not rub off
Distribution:
• Typically bilateral in oral mucosa
• May extend to labial mucosa
• Can involve floor of mouth

Diagnosis of Leukoedema
White appearance diminishes or disappears with eversion of the cheek
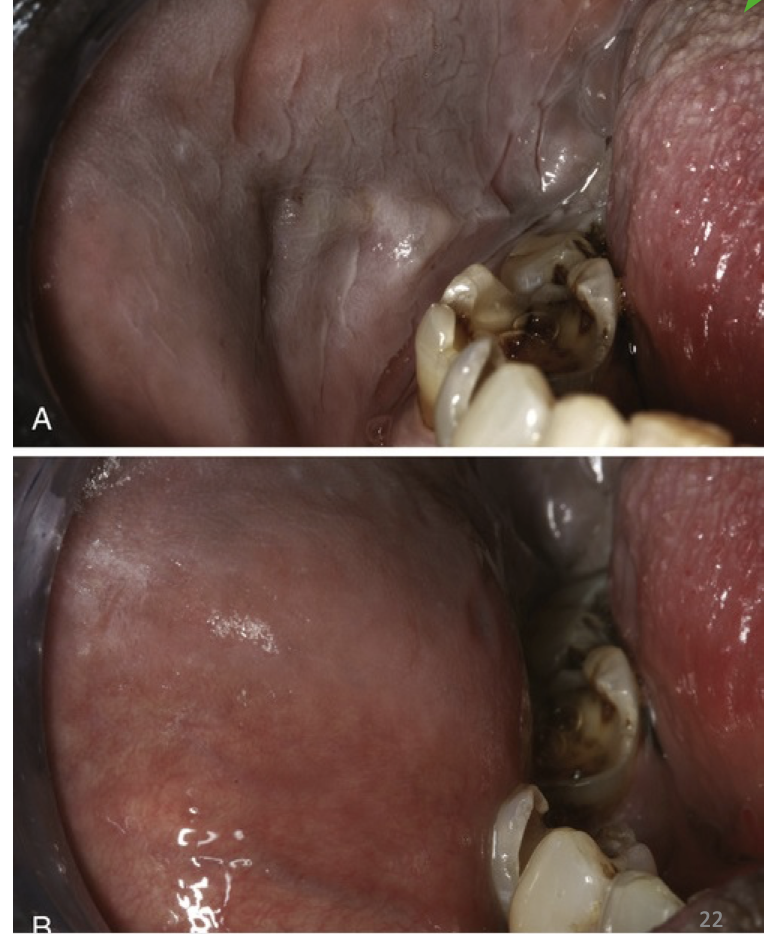
Differentials of Leukoedema
Leukoplakia
Candidiasis
Lichen planus
Ankyloglossia
Developmental condition
Characterized by a short and thick lingual frenum
Leads to limitation of tongue movement
More common in neonates
Clinical Manifestations of Ankyloglossia (Mild cases)
Little clinical significance
Clinical Manifestations of Ankyloglossia (Severe cases)
Fusion of tongue to floor of mouth
Possible fusion of frenum to tip of tongue
Slight clefting of tongue tip
Speech difficulties (usually minor)

Treatment of Ankyloglossia
Mild cases: no treatment necessary
Frenotomy: for infants with specific breast-feeding problems
Frenuloplasty: postponed until 4–5 years old in children
Indicated in children and adults with functional or periodontal difficulties → increases tongue mobility
Fissured Tongue (Scrotal Tongue)
Relatively common
Multiple grooves or fissures on the dorsal lingual surface
Cause: unknown
Contributing factors: age & environment
Clinical Features of Fissured Tongue
Multiple grooves or furrows
Severe cases:
Numerous fissures covering entire dorsal surface
Tongue papillae divided into multiple separate “islands” (associated with geographic tongue)
Symptoms:
Usually asymptomatic

Treatment of Fissured Tongue
Benign condition → no treatment needed
Prophylaxis: prevent accumulation of debris → encourage patients to brush the tongue
Varicosities
Abnormally dilated, tortuous veins
Rare in children, common in elderly
Associations:
Leg varicosities ↔ tongue varicosities
Smoking
Cardiovascular disease
Most common type of Varicosities
Sublingual varix
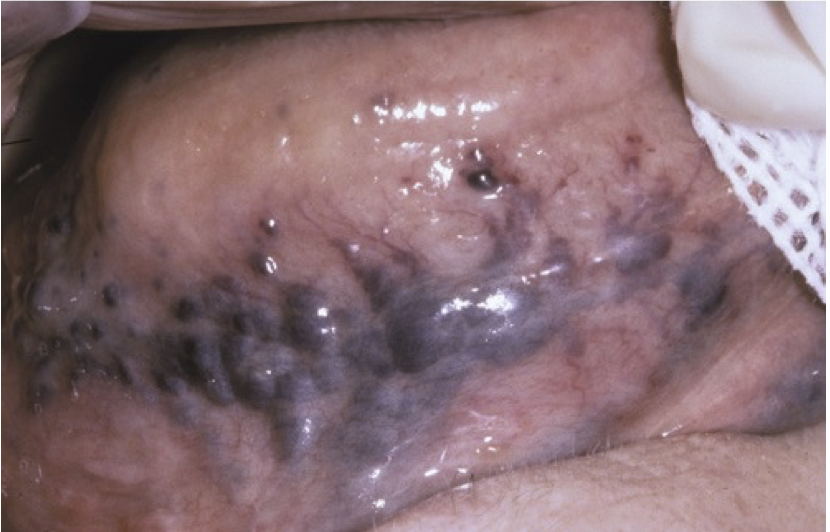
Clinical manifestations of Varicosities
Multiple lesions
Purple papules (elevated)
Located on ventral & lateral borders of tongue
Symptoms:
Usually asymptomatic
Thrombosis may occur
Solitary Varices
Less common than sublingual varices
Locations:
Lips
Buccal mucosa
Often noticed after thrombosis
Thrombosed varix:
Firm
Nontender
Blue-purple nodule (isolated)

Treatment of Varicosities
Asymptomatic cases: no treatment required
Solitary varices: surgical removal (laser treatment)
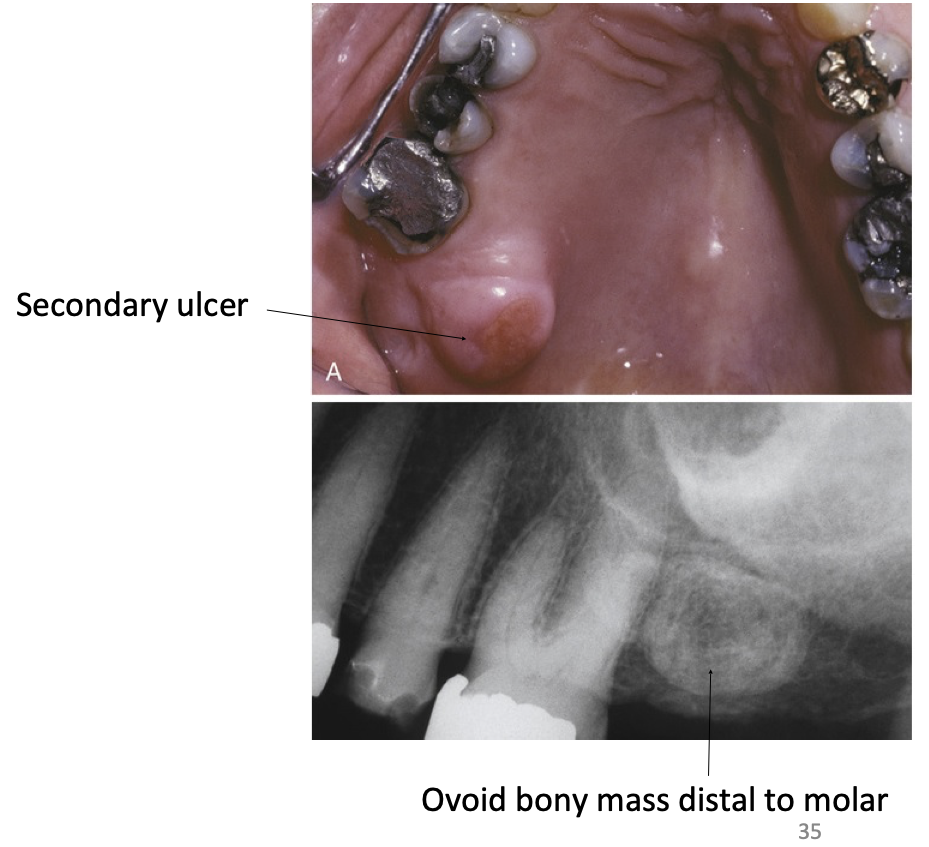
Exostoses
Benign bony protuberances arising from cortical plate
Location: jaws frequently affected → related to stresses from teeth function
Best-known forms:
Torus palatinus
Torus mandibularis
Clinical Manifestations of Exostoses
More frequent in adults
Buccal exostoses:
Bilateral row of bony nodules
Located on facial aspect of maxillary and/or mandibular alveolar ridge
Symptoms:
Usually asymptomatic
Surface mucosa may ulcerate

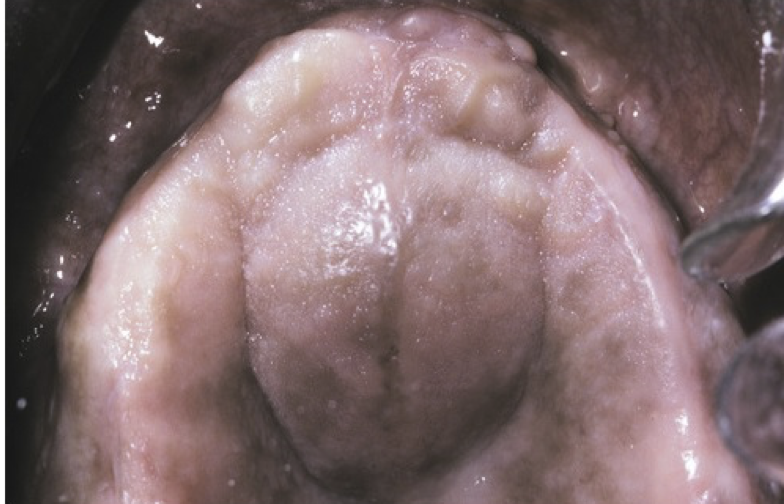
Clinical Manifestations of Palatal Exostoses
Location: Lingual aspect of maxillary tuberosities
Bilateral or unilateral
More common in males
Patients with buccal or palatal exostoses may also present palatal or mandibular tori
Cyst
Pathologic cavity
Filled with fluid
Lined by epithelium
Many developmental cyst are considered fissural cysts
Slow increase in size
Palatal Cysts of the Newborn
Prevalence: mostly in neonates
Appearance: White or yellow-white papules
Location:
Often along midline
Near junction of soft and hard palate
Lesion pattern: Single or clusters (2–6 lesions)
Symptoms: Asymptomatic
Treatment:
No treatment necessary
Self-healing

Nasolabial Cyst
Location: Upper lip, lateral to midline
Clinical Manifestations of Nasolabial Cyst
Swelling of upper lip, lateral to midline
Elevation of the ala of the nose
Obliteration of the maxillary mucolabial fold
Pain: uncommon, occurs if secondary infection develops
Rupture: may occur → drains into oral or nasal cavities
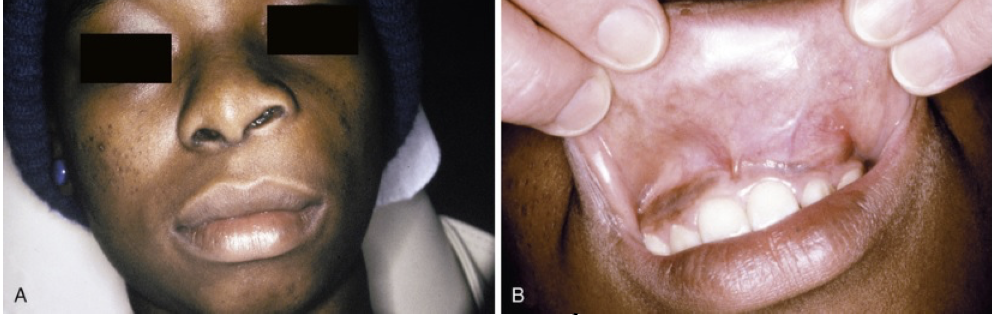
Treatment and Prognosis of Nasolabial Cyst
Complete surgical excision
Recurrence is rare
Nasopalatine duct cyst
Most common nonodontogenic cyst of the oral cavity
Clinical Manifestations of Nasopalatine Duct Cyst
Swelling of anterior palate
Drainage
Pain
Many cases are asymptomatic
Discovered on routine radiographs
Radiographic Features of Nasopalatine Duct Cyst
Appearance:
Well-circumscribed radiolucency
Located in or near midline of anterior maxilla
Between apices of central incisors
Shape:
Usually oval or round
May appear as inverted pear shape
Borders: sclerotic margins commonly present
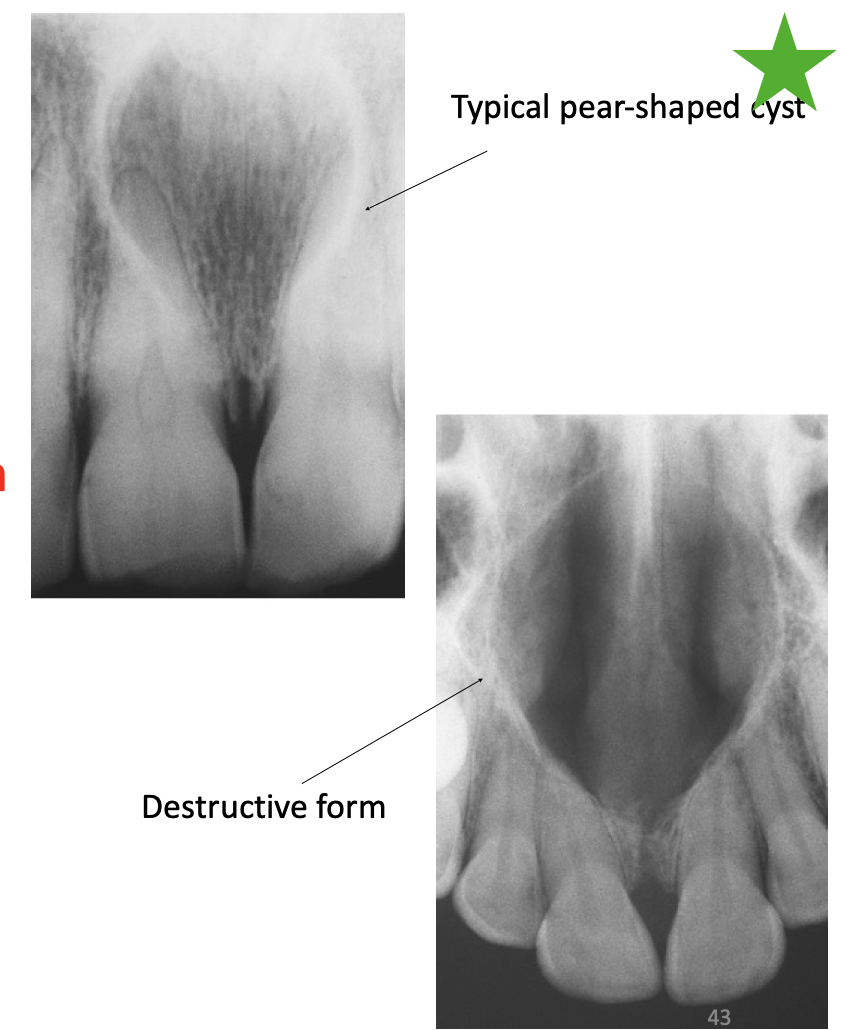
Treatment & Prognosis of Nasopalatine Duct Cyst
Treatment:
Surgical enucleation
Biopsy recommended
Prognosis:
Recurrence is rare
Malignant transformation is very rare
Thyroglossal Duct Cyst
Remnant of epithelium from the thyroglossal tract
Develops classically in the midline
Often adjacent to the hyoid bone
Clinical Manifestations of Thyroglossal Duct Cyst
Midline swelling
Painless in most cases
Movable and fluctuant
Complications:
Secondary infections may occur
If located at the base of the tongue, can cause laryngeal obstruction
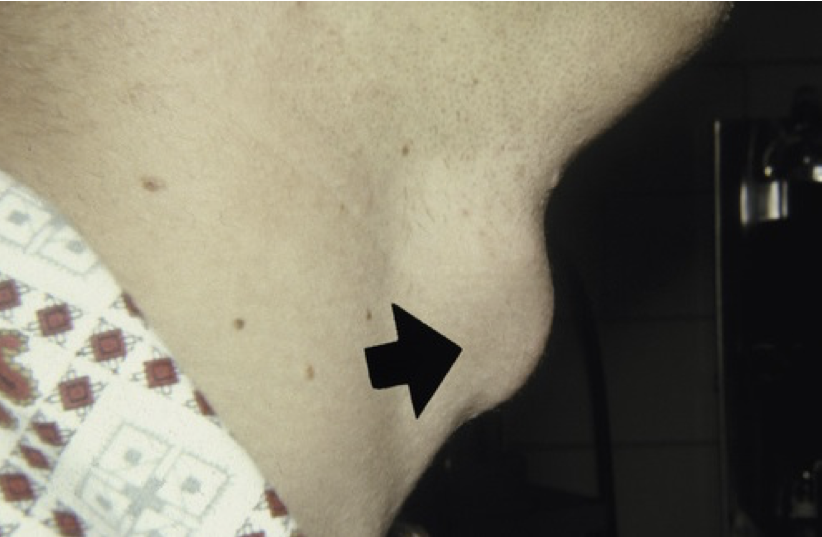
Treatment of Thyroglossal Duct Cyst
Sistrunk procedure → complete removal of:
Cyst
Midline segment of hyoid bone
Portion of muscular tissue along the thyroglossal tract
Environmental Alterations of Teeth
Developmental tooth defects
Post-developmental structure loss
Discolorations of teeth
Localized disturbances in eruption
Environmental Effects on Tooth Development
Ameloblasts (cells forming enamel) are highly sensitive
External stimuli → significantly alter enamel structure
Severity of defect is directly proportional to intensity/duration of factors
Two categories of factors:
Systemic
Local
Does enamel remodel after its initial formation?
No enamel does not remodel (unique to enamel)
Abnormalities of enamel development remain permanently etched on the tooth surface
What are the 3 major steps in enamel development?
Matrix formation – proteins are laid down
Mineralization – minerals deposited, most original proteins removed
Maturation – final mineralization and removal of protein remnants
Effects of time on enamel defects
Timing of ameloblastic damage impacts location and appearance of enamel defect
Final enamel is a record of insults received during tooth development
Position of enamel in permanent tooth provides rough estimate of time of damage
What are the two main classifications of enamel defects?
Hypoplasia: quantitative defect
Opacities: qualitative defect
What characterizes enamel hypoplasia?
Pits, grooves, or larger areas of missing enamel
What characterizes enamel opacities?
Diffuse or demarcated defects
Enamel thickness is normal
Appear as variations in translucency
Diffuse opacities
Increased white opacities without clear boundaries from normal enamel
Demarcated opacities
Areas with decreased translucence and increased opacity
Sharp boundary with adjacent enamel
Porosity determines color (white, cream, yellow, or brown)
Environmental Enamel Hypoplasia
Cause: Systemic influences during tooth development
Characteristic pattern:
Rows of pits or diminished enamel
Bilateral and symmetrical enamel loss
Defects’ location corresponds to developmental stage of affected teeth
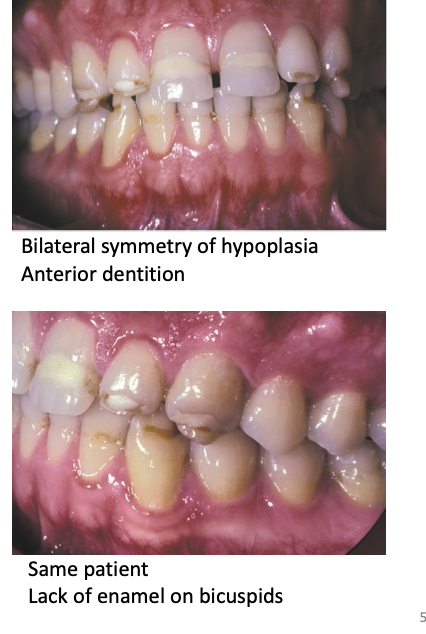
Turner Hypoplasia
Pattern of enamel defects in permanent teeth
Cause: Periapical inflammatory disease of the overlying deciduous tooth
Usually affects only one tooth (“Turner tooth”)
Determinants: timing & severity of insult → appearance of defect
Most frequent: Permanent bicuspids → close relation with overlying deciduous molars
Less frequent: Anterior teeth → crown formation usually complete before apical inflammation develops in caries-resistant anterior deciduous teeth
Clinical signs of Turner Tooth
Extensive enamel hypoplasia
Lack of significant enamel
Irregular dentin surface
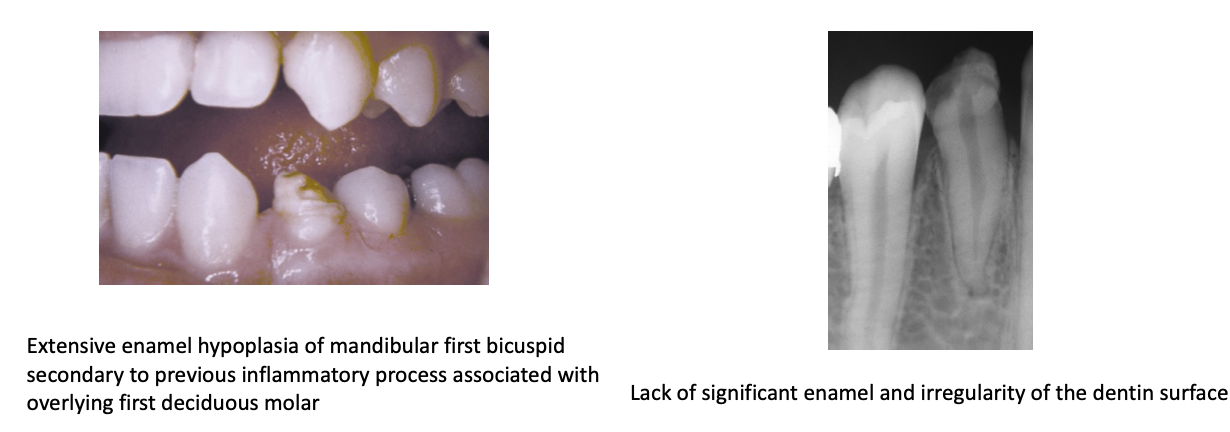
Turner tooth
Cause: Traumatic injuries to deciduous teeth
Most affected: maxillary central incisors
Factors determining degree of damage of permanent teeth
1 Stage of tooth development
2. Length of time infection is not treated
3. Virulence of microorganisms
4. Host resistance to infection
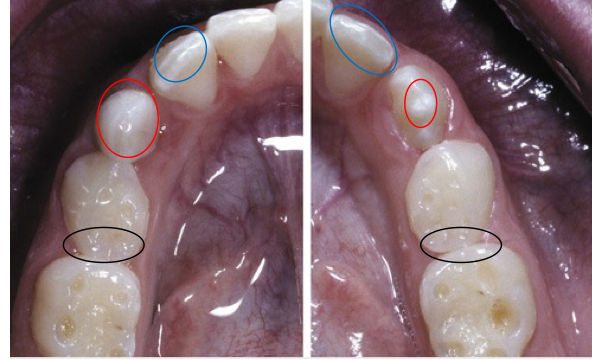
Molar-Incisor Hypomineralization
Hypomineralization affecting one or more molars
Appearance of enamel:
White, yellow, or brown areas
Sharp demarcation with normal enamel
Yellow/brown enamel:
Increased porosity
Posteruptive enamel loss
Incisor involvement correlates with number of molars affected
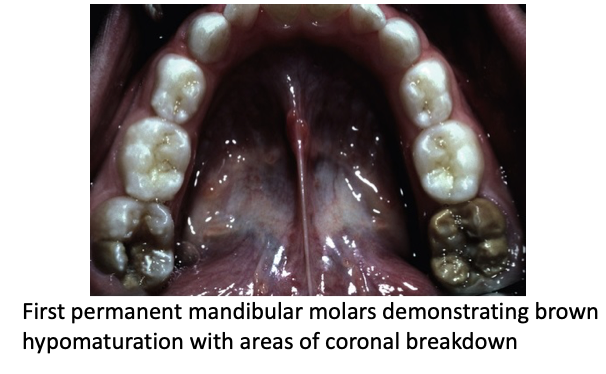
Clinical consequences of molar-incisor hypomineralization
High dental sensitivity
Difficulties with oral hygiene
Higher caries risk
Problems with dental anesthesia
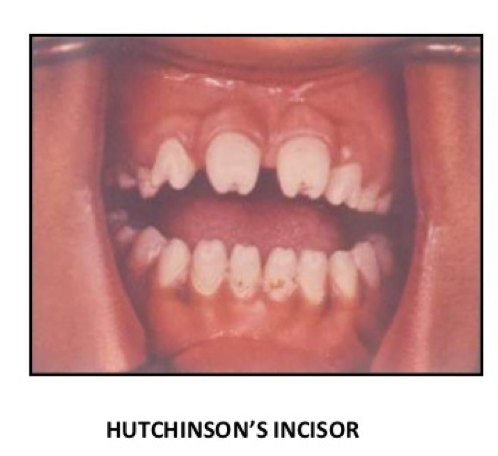
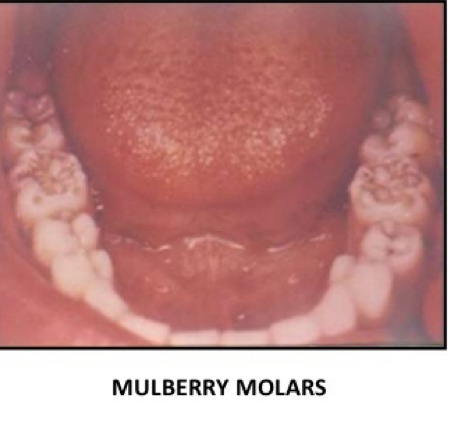
Syphilis hypoplasia
Rare nowadays:
Hutchinson teeth (anterior teeth)
Mulbery teeth (posterior teeth)
Hutchinson teeth
Affects anterior teeth
Crowns shaped like straight-edge screwdrivers
Greatest circumference at middle one-third of crown
Mulberry molars
Affects posterior teeth
Constricted occlusal tables → bumpy surface of mulberries
Treatment & Prognosis of Hypoplasia
Most cases: No treatment required
Dental microabrasion → effective for most dental fluorosis cases
Treatment of caries where present
Cosmetic approaches:
Acid-etched composite resin restorations
Labial veneers
Full crowns
Post-Developmental Tooth Structure Loss
Tooth structure is lost after formation
Common causes: caries & traumatic fractures
Causes of Post-Developmental Destruction of Enamel Surface of the Crown
Abrasion
Attrition
Erosion
Abfraction
Causes of Post-Developmental Destruction of Root (dentin/cementum surfaces)
External resorption
Internal resorption
Tooth wear (Tooth surface loss)
Physiologic
Normal process
Age dependent
Pathologic
Functional problems
Esthetic concerns
Dental sensitivity issues
Causes of tooth wear
Multifactorial: combination of more than 2 factors
Attrition
Abrasion
Erosion
Abfraction
Attrition
Loss of tooth structure due to tooth-to-tooth contact during occlusion and mastication
Some degree is normal
Pathologic attrition:
Functional problems
Esthetic concerns
Factors that accelerate tooth destruction:
Poor-quality or absent enamel
Premature contacts (edge-to-edge occlusion)
Intraoral abrasives, erosion, and grinding habits
Clinical Manifestations of Attrition
Teeth affected: Both deciduous and permanent
Affects predominantly opposed dental surfaces in contact
Most frequent locations: Incisal and occlusal surfaces
Characteristic finding: Large, flat, shiny wear facets
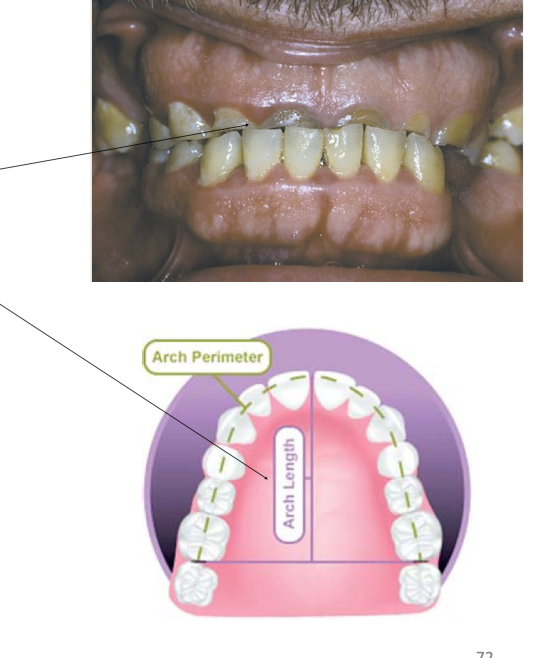
Loss of interproximal contact points: due to vertical movement of teeth → leads to shortening of arch length
Pulp exposure and dentin sensitivity are rare
Slow tooth structure loss allows for apposition of reparative secondary dentin within pulp cavity
Abrasion
Wearing away of tooth structure or restoration due to mechanical action of an external agent
Most common cause: Inadequate tooth brushing
Abrasive toothpaste
Heavy pressure
Horizontal brushing stroke
Other causes:
Pencils
Toothpicks etc
Clinical Manifestation of Abrasion
Toothbrush abrasion:
Horizontal cervical notches on buccal surface of exposed radicular cementum & dentin
Well-defined margins
Smooth, hard surface
If acid is present: lesions become rounded & shallower
Other manifestations: rounded or V-shaped notches on incisal edges of anterior teeth → associated causes:
Thread biting
Use of pipes or bobby pins

Erosion
Loss of tooth structure caused by a nonbacterial chemical process
Also called dental corrosion
Causes:
Chelating agents (primary cause)
Acidic agents
Involuntary or voluntary regurgiation (eating disorders)
Clinical Manifestations of Erosion
Not correlated with functional wear patterns
Loss usually linked to known abrasives (dietary/chemical sources)
Areas most affected (not protected by serous secretions)
Anterior maxillary teeth: facial (buccal) & palatal surfaces
Mandibular posterior teeth: facial (buccal) & occlusal surfaces
Cupped Lesion
Classic pattern of dental erosion
Central depression of dentin surrounded by elevated enamel
Seen on:
Occlusal cusp tips
Incisal edges
Marginal ridges
Erosion of Posterior Teeth
Findings:
Extensive loss of occlusal surface
Edges of metallic restorations stand above tooth structure
Progression:
Rapid dentin destruction
Concave depression of dentin
Surrounded by elevated rim of enamel

Erosion of buccal cusps
Loss of entire buccal cusps
Replacement by ski slope-like depressions from lingual cusp to buccal cementoenamel junction

Erosion of palatal surfaces
Palatal surfaces affected
Exposed dentin with a concave surface showing peripheral white line of enamel

Area-Specific Causes of Erosion
Facial surfaces of maxillary anterior teeth: dietary sources of acids
Incisal portion of anterior teeth (both arches): environmental sources (suggested)
Palatal surfaces of maxillary anterior teeth + occlusal surfaces of posterior teeth (both arches): regurgitation of gastric secretions