Week 7: Scaffa Chapter 17: Health Professional Well-Being
1/127
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
128 Terms
Well-Being
A state in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community
Oftencited characteristics include building and maintaining positive and fulfilling relationships, receiving and providing emotional support, experiencing positive emotions, pursuing personal growth, engagement, and accomplishment, and participating in spiritual or other activities that provide meaning
Triple Aim
Proposes that health-care systems pursue three aims:
Improving the health of populations
Enhancing the patient experience of care
Reducing the per capita cost of health care
Possible fourth aim would be improving the work life and well-being of healthcare professionals and staff
Burnout
A psychological syndrome that involves a prolonged response to chronic interpersonal stressors on the job that results in feelings of being overextended and depleted of one's emotional and physical resources
Consists of emotional exhaustion, depersonalization, cynicism, and a reduced sense of personal accomplishment
Produces significant personal suffering for health-care providers in the form of broken relationships, alcohol and substance abuse, depression, and suicide
Physical Symptoms of Burnout
Chronic fatigue
Headaches
Muscle pain
Insomnia
Hypertension
Gastrointestinal disorders
Psychological Manifestations of Burnout
Feelings of helplessness, anxiety, and depression
Difficulties with concentration, memory, and decision-making
Behavioral Manifestations of Burnout
Absenteeism
Poor work performance
Aggression
Defensiveness
Social withdrawal
Substance use
Risk-taking behavior
Coping Strategies Used by OTs for Burnout
Self-awareness and self-monitoring
Spending time with family and friends
Striving for a personal and work-life balance
Maintaining a sense of humor
Burnout: Stage 1
A compulsion to prove oneself
Burnout: Stage 2
Working harder to meet ones' own high expectations
Burnout: Stage 3
Neglecting basic personal self-care needs
Burnout: Stage 4
Displacement and the inability to recognize and deal with the source of one's distress
Burnout: Stage 5
Revision of values and the dismissal of once-important relationships and activities
Burnout: Stage 6
Denial of emerging problems, intolerance, cynicism, and aggression
Burnout: Stage 7
Withdrawal, isolation, loss of hope or direction, escape through alcohol or drug use
Burnout: Stage 8
Behavioral changes obvious to family and friends and increasing feelings of worthlessness
Burnout: Stage 9
Depersonalization and a loss of emotional connectedness to self and others
Burnout: Stage 10
Pervasive feeling of inner emptiness that may lead to addictive behaviors, such as gambling, overeating, compulsive sexual behavior, and drug and alcohol abuse
Burnout: Stage 11
Depression, loss of meaning, apathy, and hopelessness
Burnout: Stage 12
Burnout, total mental and physical collapse, potential for suicide need for immediate medical and psychological attention
Emotional Exhaustion
Characterized by feeling overextended and overwhelmed by job demands
Results in higher health-care costs due to staff turnover and lower job productivity
Known to be the primary product of compassion fatigue and can lead to difficulties with creating a genuine empathic relationship with clients, which in turn can negatively affect the delivery of services
Depersonalization
Is exemplified by detachment, indifference, and cynicism
Reduced Sense of Personal Accomplishment
Manifested by feelings of inadequacy, perceptions of failure, and decreased confidence
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Control of Hazards and Exposures
Chemicals
Physical agents
Biological agents
Psychosocial factors
Human factors
Risk assessment and risk management
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Organization of Work
Fatigue and stress prevention
Work intensification prevention
Safe staffing
Overtime management
Healthier shift work
Reduction of risks from long work hours
Flexible work arrangements
Adequate meal and rest breaks
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Built Environment Supports
Healthy air quality
Access to healthy, affordable food options
Safe and clean restroom facilities
Safe, clean and equipped eating facilities
Safe access to the workplace
Environments designed to accommodate worker diversity
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Leadership
Shared commitment to safety, health, and well-being
Supportive managers, supervisors, and executives
Responsible business decision-making
Meaningful work and engagement
Worker recognition and respect
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Compensation and Benefits
Adequate wages and prevention of wage theft
Equitable performance appraisals and promotion
Work-life programs
Paid time off (sick, vacation, caregiving)
Disability insurance (short- & long-term)
Workers’ compensation benefits
Affordable, comprehensive healthcare and life insurance
Prevention of cost shifting between payers (workers’ compensation, health insurance)
Retirement planning and benefits
Chronic disease prevention and disease management
Access to confidential, quality healthcare services
Career and skills development
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Community Supports
Healthy community design
Safe, healthy and affordable housing options
Safe and clean environment (air and water quality, nose levels, tobacco-free policies)
Access to safe green spaces and non-motorized pathways
Access to affordable, quality healthcare and well-being resources
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Changing Workforce Demographics
Multigenerational and diverse workforce
Aging workforce and older workers
Vulnerable worker populations
Workers with disabilities
Occupational health disparities
Increasing number of small employers
Global and multinational workforce
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: Policy Issues
Health information privacy
Reasonable accommodations
Return-to-work
Equal employment opportunity
Family and medical leave
Elimination of bullying, violence, harassment, and discrimination
Prevention of stressful job monitoring practices
Worker-centered organizational policies
Promoting productive aging
Issues Relevant to Advancing Worker Well-Being Through Total Worker Health: New Employment Patterns
Contracting and subcontracting
Precarious and contingent employment
Multi-employer worksites
Organizational restructuring, downsizing and mergers
Financial and job security
Primary Work Setting for OT practitioners (25.8%)
Long-term care (LTC) or skilled nursing facilities (SNFs)
Next Two Most Common Employment Sites for OT Practitioners after LTCs and SNFs
Hospital settings (23.9%)
Schools (19%)
School Employees in California were Reported to be at Risk for injury from hazards such as:
Chemical spills
Ergonomics
Infectious disease
Poor indoor air quality
Trips, slips, and falls
Risk Factor
Any attribute, characteristic or exposure of an individual that increases the likelihood of developing a disease or injury
Ex: underweight, unsafe sex, high blood pressure, tobacco and alcohol consumption, and unsafe water, sanitation and hygiene
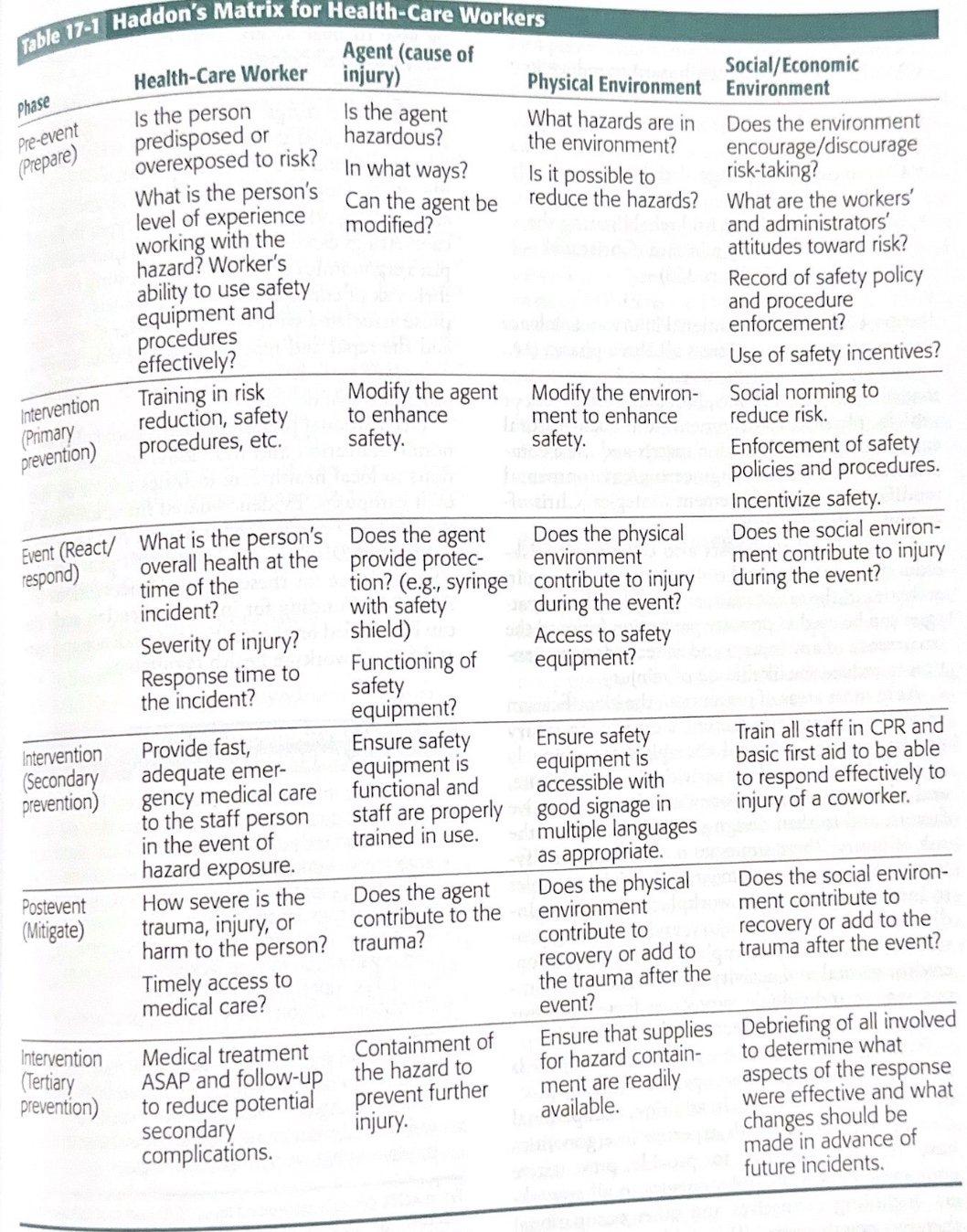
Haddon’s Matrix
Developed by William Haddon Jr.
A matrix that conceptualizes injury as occurring in three phases in interaction with human factors, an agent or vehicle, and physical and sociocultural environment
Pre-injury event
Injury event
Post-injury event
Pre-Injury Event Phase
Primary prevention efforts are appropriate
Ex: Speed limit enforcement to reduce motor vehicle crashes
Injury Event Phase
Secondary prevention is the focus
Ex: Shortening emergency response times and improving the efficacy of rehabilitation
Haddon’s Matrix for Health-Care Workers
Hazard
The potential to cause harm, or a condition or activity that if not controlled could result in illness or injury
Typically fall into four broad categories
Physical
Chemical
Biological
Psychological
Physical Hazards
Include such things as radiation, noise, and poor working conditions
Chemical Hazards
May be naturally occurring or human-made, such as vapors and gases from industry and tobacco smoke
Biological Hazards
Take the form of allergens, blood, bacteria, viruses, and other microbiological organisms
Psychological Hazards
Are typically occurrences that induce unreasonably high levels of stress, such as exposure to violence
Haddon’s Categories of Injury Prevention Strategies (Haddon Ten)
Preventing the initial creation of a hazard
Reducing the amount of energy a hazard contains
Preventing the release of existing hazards
Modifying the rate or distribution of a hazard
Separating the hazard, by time or space, from the person
Using material barriers to prevent exposure to a hazard
Modifying qualities of a hazard to reduce its impact
Increasing the person’s resistance to damage from a hazard
Countering the damage already done as quickly as possible
Stabilizing, repairing, and rehabilitating the damage produced by a hazard
Injury Prevention and OT
Occupational therapists are uniquely equipped to analyze daily activities in work, leisure, and self-care; to identify potential risk and protective factors; and to then design strategies to reduce the risk of injury
Strategies OTs use may include modifying environmental, equipment, and activity variables to increase safety in the workplace, decreasing individual risk factors for injury, and increasing protective factors
Evidence-Based Workplace Interventions
Ergonomic interventions (training, rest breaks, forearm supports, specially designed glasses, workstation redesign) increase work comfort
Ergonomic workstation redesign and training reduce days lost, pain prevalence and intensity, and injury rate among health-care workers
Changes in the workplace design, equipment, and organization reduce sickness absence in several occupational classifications
Participatory ergonomics reduces pain among workers
Web-based monitoring at work only may not be better than no intervention to reduce pain. Adding strengthening and relaxation exercises to a web-based monitoring program may have a positive effect on pain and on stress.
Infectious Agents Include
Bacteria, fungi, viruses, and parasites that have the ability to spread an infection or infectious disease
According to the NIOSH (2017a), health-care workers are at risk from the following infectious agents:
Blood-borne pathogens (BBPs)
Ebola
Influenza
Middle East respiratory syndrome (MERS)
MRSA
SARS
TB
Sharps Injuries
Include needlesticks
Can transmit BBPs such as HIB, hepatitis B virus, and hepatitis C virus
How do sharps injuries impact a worker’s well-being?
Stress of undergoing immediate and long-term testing
Waiting for results
Being treated if infected
What financial impact does the health-care system face from sharps injuries?
Additional staffing to cover missed work
Testing expenses
Preventative or curative treatment regimens
The time and cost of injury investigation and documentation
What is the primary prevention strategy regardless of the infectious agent?
Education regarding specific risk-reduction techniques
The appropriate use of safety supplies and equipment
The consistent reporting and reviewing of data on infection rates at the institution or in the community, as well as at state, national, and global levels
Isolation Procedures
Hand hygiene
Eye protection
Hand Hygiene
A simple but very effective prevention strategy to decrease the transmission of infectious agents, but studies show that some healthcare providers practice hand hygiene les than half of the times they should
Workers have the right to:
Working conditions that do not pose a risk of serious harm
Receive information and training (in a language and vocabulary the worker understands) about workplace hazards, methods to prevent them, and the OHSA standards that apply to their workplace
Review records of work-related injuries and illnesses
File a complaint asking OSHA to inspect their workplace if they believe there is a serious hazard or that their employer is not following OSHAs' rules. OSHA will keep all identities confidential
Exercise their rights under the law without retaliation, including reporting an injury or raising health and safety concerns with their employer or OSHA. If a worker has been retaliated against for using his or her rights, the worker must file a complaint with OSHA as soon as possible but no later than 30 days.
Stress
The source of this can include exposure to infectious diseases, productivity demands, insufficient staffing, role ambiguity, complex authoritarian management systems, ethical dilemmas and moral distress that arise from being involved in decisions that have an impact on people’s health and well-being, and burnout
Can lead workers to leave their respective professions
Adverse Effects of Occupational Stress
Psychological
Ex: irritability
Behavioral
Ex: difficulty sleeping, attendance issues
Physical
Ex: headache
Moral Distress
Tension that arises when a moral agent (e.g., a practitioner) is unsure of the best course of action to take or encounters a barrier that prohibits doing what is known to be right
Expectations that were Linked to the Highest Level of Moral Distress Include:
Being expected to obtain as many billable units as possible per client regardless of individual client needs
Being unable to provide optimal therapy services because of limited insurance coverage or insurance cutoffs reported
Being expected to treat and/or write documentation for more clients than time allows
Recommended Risk-Reduction Strategies for Health-Care Workers Include
Organizational change interventions
Stress management interventions
Organizational Change Interventions Recommended by the CDC
Involvement of employees in all aspects of planning and evaluating the intervention with a focus on team processes
Use of interdisciplinary health-care teams
Multipronged interventions that include risk assessment
OSHA Suggestions for Organizational Change Interventions
Address work-related stressors such as inadequate work space, unreasonable work load, lack of readily available resources, inadequate and unsafe equipment
Recognize and take action on legitimate concerns regarding overbearing physicians and supervisors
Establish employee assistance programs and organizational change programs
Provide greater flexibility with job assignment, hours, and alternative job arrangements
Suggestions from OSHA for Stress Management Interventions
Educate employees about job stress
Establish and maintain stress-management programs
Provide readily available counseling from a nonjudgmental source
Provide group therapy for specific job-related stressors (e.g., death of patients)
Use of relaxation exercises and biofeedback until stress source is identified
Impact of Burnout on Individual Health-Care Professionals Includes
Increase in anxiety
Increase in depression
Increase in disrupted sleep
Increase in substance abuse
Increase in marital discord
Increase in early retirement
Increase in suicide rates
Stressors in the Health-Care Work Environment that Lead to Burnout Include
New payment and health-care delivery approaches
Electronic health records
Publicly reported quality of care metrics
Excessive workloads
Inadequate staffing
Decreased autonomy and lack of control over work processes
Specific Stressors Related to Occupation Therapy Include
Staff shortages
Work overload
Role ambiguity
Lack of recognition and support from colleagues
Low visibility of the occupational therapy profession
Resilience
Patterns of positive adaptation during or following significant adversity or risk
Is protective against compassion fatigue and burnout
A dynamic, adaptive process throughout the life span that can be learned
Internal Factors that Contribute to Resilience
Personality traits such as optimism
Beliefs such as self-efficacy
Skills such as adaptive coping
External Factors that Contribute to Resilience
Refer to environmental resources (material and energy) and the access to and stability of those resources over time
Social Factors that Contribute to Resilience
Include feelings of connectedness to the people around us
For health-care workers, includes mutual trust and connectedness to colleagues
Resilient Health-Care Worker
One who has the ability to maintain personal and professional well-being in the face of ongoing work stress and adversity
Two Complementary Types of Behaviors that Resilience Consists of
Preventive
Corrective
Preventive Behaviors
Those activities someone engages in that protect from burnout and help the person resist adversity
Corrective Behaviors
Those activities a person engages in that help the individual cope effectively with stressful conditions
Compassion Satisfaction
The joy and fulfillment a person derives from helping other people
The more a person has, there is less risk of burnout
Compassion Fatigue
An emotional state with negative psychological and physical consequences that emanate from acute or prolonged caregiving of people stricken by intense trauma, suffering, or misfortune
A direct result of a caregiver ignoring the symptoms of personal stress combined with inattention to personal emotions over time
If not addressed, can become burnout
Signs and Symptoms of Compassion Fatigue
Trouble sleeping/exhaustion
Increased emotional reactivity/hypersensitivity to emotional material
Hypervigilance or heightened sensitivity to potential threats to self
Diminished interest in regular activities
Reduced ability to feel empathy
Anger and irritability
Absenteeism (work, family event, social events) or poor work skills
Difficulty separating work life from personal life
Job Engagement
The antithesis of burnout
Is conceptualized as an energetic state of involvement with personally fulfilling activities that enhance one's sense of professional efficacy
Characteristics of Job Engagement
Pleasurable engrossment with work tasks (similar to the concept of flow)
Enthusiasm
Persistence
A sense of professional efficacy, satisfaction, and success with work
Action Collaborative on Clinician and Resilience
Initiated by the National Academy of Medicine (NAM) in 2017
Designed to address health-care provider well-being and prevent burnout
Goals for the Action Collaborative on Clinician Well-Being and Resilience
Improve baseline understanding of challenges to clinician well-being
Raise the visibility of clinician stress and burnout
Elevate evidence-based, multidisciplinary solutions that will improve patient care by caring for the caregiver
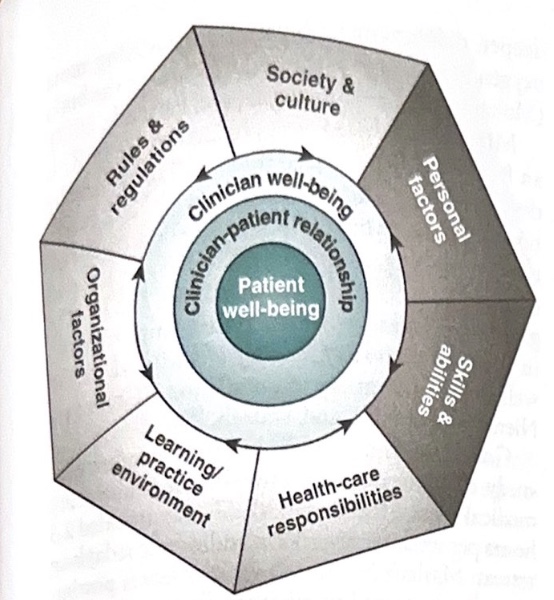
Clinician Well-Being Model
Depicts the individual and organizational/environmental factors that affect clinician well-being and resilience
A holistic model that captures the relationship between the patient and the clinician and the complex interaction of factors that affect professional well-being and thereby have an impact on patient care
Purpose is to guide research on clinician well-being and the development of effective intervention strategies at individual, organizational, and systems levels
Clinician Well-Being Model: The Three Concentric Circles in the Center of the Diagram
Form the nucleus
Represent (from the inside outward) patient well-being, the clinician-patient relationship, and clinician well-being
Clinician Well-Being Model: Individual and External Factors that Affect Clinician Well-Being and Resilience
Encircle the nucleus
Individual factors:
Health-care role
Personal factors
Skills and abilities
Environmental factors:
Sociocultural factors
Regulatory, business, and payer environment
Organizational factors
Learning/practice environment
Stanford (University) Physician Wellness Model
Identifies personal resilience, efficiency for practice, and a culture of wellness as determinants of well-being, the interaction of which promotes professional fulfillment
Similar to the NAM model in that it emphasizes the interaction of internal (personal resilience) and external factors (efficiency of practice and culture of wellness) that affect clinician well-being
Professional Fulfillment in Stanford (University) Physician Wellness Model
Happiness or meaningfulness, self-worth, self-efficacy, and satisfaction at work
Prevention and Intervention Programs to Reduce Burnout and Enhance Resilience
Can be directed at the individual, the worksite or organization, the community or system, or some combination of these
Four Levels of Salazar and Beaton’s (2000) Ecological Approach that Addresses the Context in Which Occupational Stress Occurs
Microsystem
Consists of the individual and immediate work environment
Organizational system
Includes the physical structures, organizational culture, and policies and procedures
Periorganizational system
Societal influences on the worker and the organization
Extraorganizational system
Includes customs, cultures, traditions, and government policies that affect the worker and the organization
Professional Self-Care
Attending to one’s own health and wellness needs
Engaging in behaviors and activities that increase energy, lower stress, and contribute to health and well-being
Basic Recommendations for Professional Self-Care
Restful sleep
Good nutrition
Adequate physical activity
Coping
Conscious, volitional efforts to regulate emotion, cognition, behavior, physiology, and the environment in response to stressful events or circumstances
Strategies can be problem-focused or emotion-focused
Problem-Focused Coping
Involves planning and engaging in specific behaviors to overcome or solve the problem causing the distress
Emotion-Focused Coping
Addresses the feelings associated with stressful situations and can be active or avoidant
Ex (active):
Positive reappraisal
Relaxation techniques
Emotional support from others
Use of humor
Prayer or meditation
Avoidant Emotion-Focused Coping
Involves avoiding distress through denial, distraction, behavioral disengagement or escape (use of substances)
Mindfulness
The awareness that emerges through paying attention, on purpose, and nonjudgmentally to the unfolding of experience moment by moment
Practices include sitting and walking meditations, breath training, and body scans
Breath Training
Modifies shallow or quick breathing into deeper, diaphragmatic breathing, providing more oxygen to all tissues of the body, including the brain
Mindfulness-Based Stress Reduction (MBSR)
Originally developed for persons with chronic medical conditions
An 8-week evidence-based intervention that teaches mindfulness meditation, diaphragmatic breathing, and other relaxation techniques
Consistently demonstrated improvements in depression, anxiety, quality of life, and overall well-being in a variety of populations
Yoga
An ancient practice that originated in India
Means unity and refers to the union of mind and body and the union of individual and universal consciousness
Ultimate aim is self-awareness
Benefits of Yoga
A more positive outlook on life
Increased efficiency at work and job satisfaction
Enhanced self-confidence, self-sufficiency, and sociability
Healthier interpersonal relationships
More effective responses to life challenges