Patho: Inflammation and Dysfunctional Wound Healing EX1
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Inflammation steps generally
Injury
Bleed
Stop bleed
Redness, pain, swell, heat, loss of function
heals
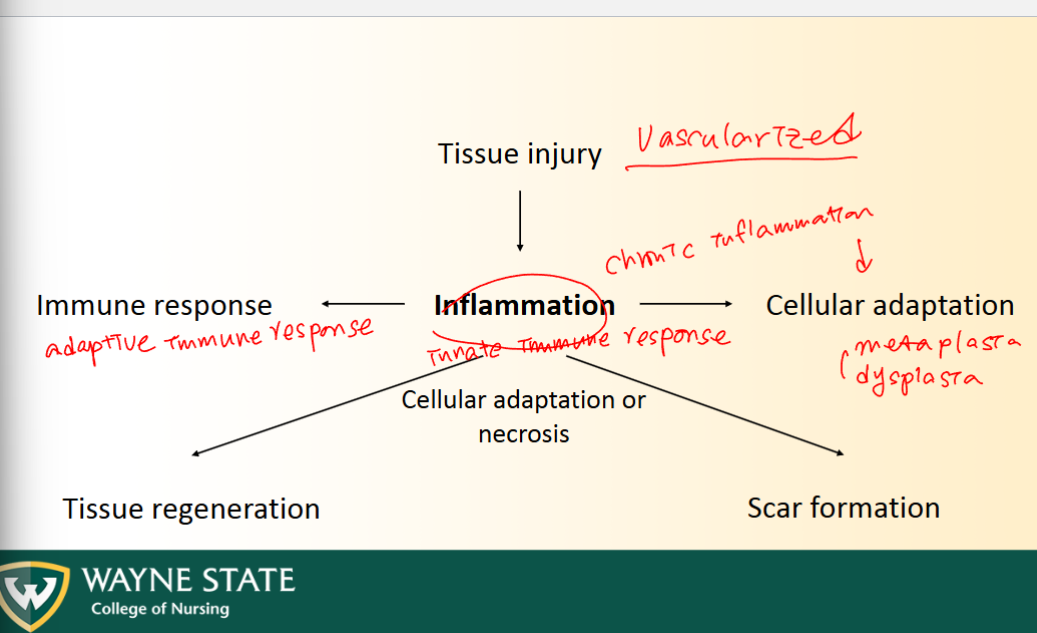
Inflammation Response types (Following VASCULARIZED Tissue Injury)
Inflammation (Innate immune response) lead to:
Immune response (adaptive immune response)
Tissue regeneration
Scar formation
Cellular adaptation (As a result of chronic inflammation)
Inflammation + Aims (3)
Nonspecific, protective, coordinated defense to tissue injury
Intensity proportional to injury
Aims of inflammation (3 aims)
Wall of injury
Prevent spread of injurious agent
Bring body’s defenses to region
2 Types inflammation
Acute: Occurs rapidly in reaction to injury
Rids body of offending agent
Enhance healing
Terminate quickly (few days max)
Chronic
Inflammation persists
INHIBITS HEALING (doesnt help)
Causes continual cellular and organ damage
Local vs Systemic Responses
Local
Vascular stage: dilation, permeability
Cellular stage: cellular chemotaxis
Systemic
White blood cell response
Acute phase response
Vascular Stage
Inflammatory mediators enable vasodilation + increased permeability
Histamine + Bradykinin
Increased permeability = fluids, WBCs, and platelets travel OUT to injury site (from vessel)
Vasodilation arterioles followed + enhanced capillary permeability = blood out to tissue = SWELLING
5 Cardinal Sings of Acute Inflammation
Rubor/ redness
Tumor/ swelling
Calor/ heat
Dolor/ pain
Loss of function
Edematous Fluid
Purulent Exudate (pus): edema fluid rich in protein from WBCs, debris, microbial organism
Transudate: Edema fluid contains mostly water filtrate of blood (little protein) like blister fluid
Cellular Phase: Chemotaxis
Movement of WBC following chemical gradient
Chemical signal from microbial agents, WBCs, endothelial cells ATTRACTS PLATLETS AND WBCs to injury
Margination: new WBCs arrive and line up along ENDOTHELIUM in area of inflammation
WBCs release inflammatory mediators to amplify or dampen inflammation, or attract more WBCs
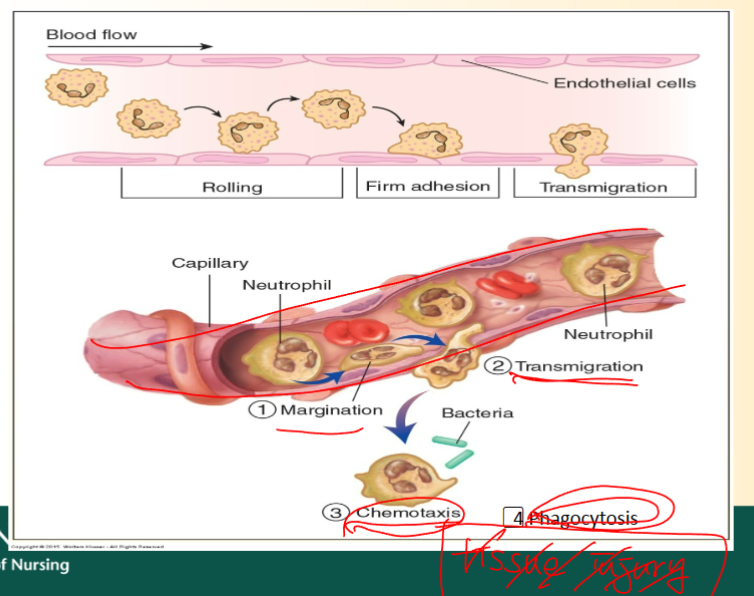
STEPS:
WBCs and other things release signal to recruit more
Margination: New WBCs(leukocytes) arrive and line up against endothelial wall
Rolling: Roll against wall to site of injury
Adhesion: adhere to endothelial receptors
Transmigration: WBCs squeex through endothlial lining into the cell/cells
Chemotaxis; WBCs follwo chemical gradient to specific injury site
Phagocytosis occurs at same time as chemotaxis, after they enter the cell
KNOW THIS 4 Chemotaxis stuff
Steps:
Margination
Transmigration (passing through endothelial
Chemotaxis
Phagocytosis
(Chemotaxis and phagocytosis happen simultaneously)
WBCs + 5 types
Major inflammation player
Neutrophils (granulocyte)
Lymphocytes (agranulocyte)
Eosinophils (granulocyte)
Basophils (granulocyte)
Monocytes/Macrophages (agranulocyte)
Granulocytes
Contain cytoplasmic granules = enzymes + mediators to fight infection
Neutrophil, basophil, eosinophil
PHILS = Gran
Neutrophil
First responder (24-48 hr)
Begin phagocytosis
Short life 10hr-few day
Bone marrow release more as they die
Likely to find in blood test with MRSA or other BACTERIAL
Viral = cold, flu, chicken pox and stuff not bacterial
Monocytes/ Macrophages
Activated after 24-48hr
Mono turn INTO MACRO (engluf pathogens)
Life span = long (weeks to months)
PREDOMINANT CELLS at injury site
CBC w/ differnetial
Used in diagnosis of infection and inflammation
Measures TOTAL NUMBERS WBCS and calculates percentages of wbc types
Mainly Neutrophil = bacterial infection
Mainly lymphocytes = viral infection
Inflammatory Mediators
Chemical proteins released when inflammation occurs
Released from Plasma,
MADE IN LIVER: Acute phase proteins, coagulation factors
Released from cells (WBC, mast cell, platlets, etc.)
Prostaglandins: pain fever
Leukotrienes: pain and swelling
Histamine: sneezing, eye tearing, sinus inflammation, etc.
Tumor necrosis factor (TNF-alpha): promotes immune response + necrosis of tumor cells
Interleukin: IL1 producing fever
Cytokines
Inflammatory mediators released by WBCs + AMPLIFY or DAMPEN inflammation
Tumor necrosis factor (TNF-alpha)
Interleukins(ILs)
Acute Phase Proteins
Inflammatory mediators made and released by LIVER
Stimulate, modulate, deactivate reaction
C-reactive protein
Fibrinogen
Serum amyloid A
ALL INCREASE with inflammation
Lab tests for inflammation
C-reactive protein (CRP)
Erythrocyte sedimentation rate (ESR) (indirectly shows fibrinogen levels) (ALSO LIVER ONE, along with serum amyloid A duh)
Leukocytosis (high WBC count)
ALL INCREASE with inflammation
Systemic Responses to inflammation (symptoms)
Fever
Pain
Malaise (generalized feeling poor health)
Lymphadenopathy (swollen lymph nodes)
Anorexia
Sleepy
Anemic
Weight loss
Fever
Inflammatory processes activate PROSTAGLANDINS + reset HYPOTHALAMIC TEMPERATURE REGULATING CENTER (raise the level to increase total body temp)
Higher body temp = WBC efficiency increase
Fever risks
Fever above 102 = BAD
Use antipyretics (aspirin, ibuprofen, etc.)
Inhibit prostaglandin formation + reduce fever
Reye’s syndrome = liver failure and encephalopathy (brain dysfunction)
Salicylate for children with viral infections
NO APIRIN: for children as an antipyretic agent
What causes chills with fever
Hypothalamic temperature control center is RAISED to higher baseline (normal is 98.6)
SO, body temp is lower than NEW BASELINE = feeling cold
Vasoconstriction + shiver to preserve/ generate heat
Lymphadenopathy
Enlargement of lymph nodes due to inflammation
Lymphocytes: mature in lymph node during inflammation = swollen + tender lymph nodes
LYMPHOCYTES = WBC
Acute Inflammation Outcomes (3)
Complete Resolution: Most desired
Injured cells replaced by same type
Vascular permeability returns
Mediators + debris, and WBCs are inactivated or destroyed
Healing by Connective tissue
Severe tissue damage + large inflammation
Fibrous (scar tissue) replaces (NOT TEH SAME TYPE)
Chronic inflammation: DOES NOT GO AWAY
Healing depends on cell type injured + severity
Cell regeneration: 3 types
Labile: continually divide + replace eliminated cells (skin, hair, nails, GI mucosal lining, bone marrow, cancer, etc.)
Stable: in a resting stage until STIMULATED, then enter cell cycle (bone cells, hepatocytes)
Permanent: do NOT enter cell cycle and DONT regenerate (neurons, cardiac, myocytes)
Cell cycle phases
G1: Synthesis of components needed for DNA
Synthesis: DNA replication
G2: Preparation for mitosis
M: Mitotic phase
CIRCULAR OVERALL
G0 phase: resting phase where cells STOP dividing, can last days to decades
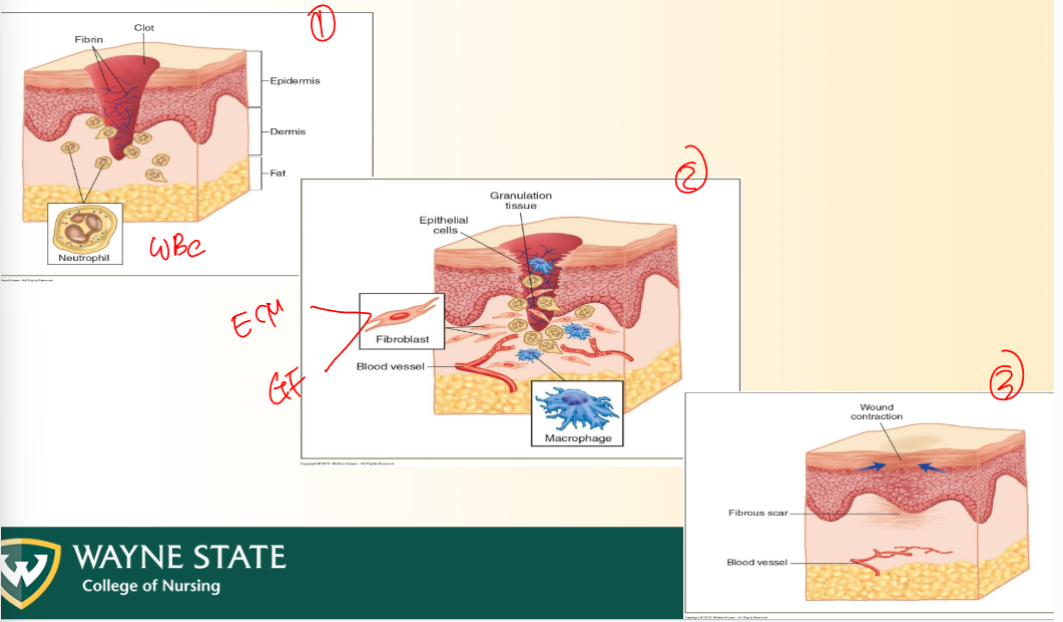
3 phases of wound healing
Inflammation
Vascular phase: vasodilate + permeability
Cellular phase: macrophages, phagocytes, etc.
WBCs: NBELm/m
Proliferation, Granulation tissue formation, Epithelization
Fibroblasts = extracellular matrix or growth factors
Proliferation = phase following initial inflammation where new tissue is formed
Granualtion tissue: highly vascularized, new CT, fibroblasts, and and extra cellular matrix (INTIAL PHASE where CT and BLOOD VESSELS froma round wound)
Epithelization = Growth of EPITHELIAL CELLS over a wound
Granulation b4 epithelization
Wound contraction + remodeling
KNOW DIAGRAM PLS
Skin Wound healing (3 processes)
Primary intention:
Clean laceration requires simple re-epithelialization when edges are approximated (closed together withs stiches or som)
No scar tissue formed
Secondary intention
Wound with LARGE GAP in tissues; some of the tissue has been gouged out (ulcer)
Scar tissue formed
Tertiary intention:
Wound with large gap missing tissue has been CONTAMINATED + needs DRAINAGE TUBE for healing
MAY need skin graft
Factors for wound healing: 10
Nutrition: proteins, carbs, etc.
Oxygenation + circulation
Immune strength
Diabetes: reduces phagocytic ability + circulation
Corticosteroid use: anti-inflammatory delay healing
Immunosuppressant agents
Contamination
Surgically inserted devices
Obesity
Age
Wound complications for healing (7)
Keloid: hyperplasia of scar tissue
Contractures: inflexible shrinkage of wound tissue that pulls edges toward center
Dehiscence: opening wound suture line
Evisceration: opening of wound with extrusion of tissue + organs
Stricture: abnormal narrowing of tubular body passage from scar tissue
Fistula: abnormal connection between 2 epithelium lined organs/vessels
Adhesion: internal scar tissue between tissues or organs
Anaplasia
Cancer cells that divide rapidly and have little resemblance to normal cells
Neoplasm:
Abnormal mass of tissue that forms when cells grow + divide excessively instead of dying
NOT always cancerous
Benign vs Malignant Neoplasia
Benign
Non cancerous
Well differentiated: generally look like cells they should be replacing; but TOO MANY OF THEM
Cell proliferation (increase in number) is EXCESSIVE
Can not regulate proliferation rate
Malignant:
Cancerous
Poorly differentiated: nonfunctional, non-resembling cells they are growing on/replacing
More poorly differentiated = faster growth
Excessive cell proliferation, cant control= ANAPLASIA
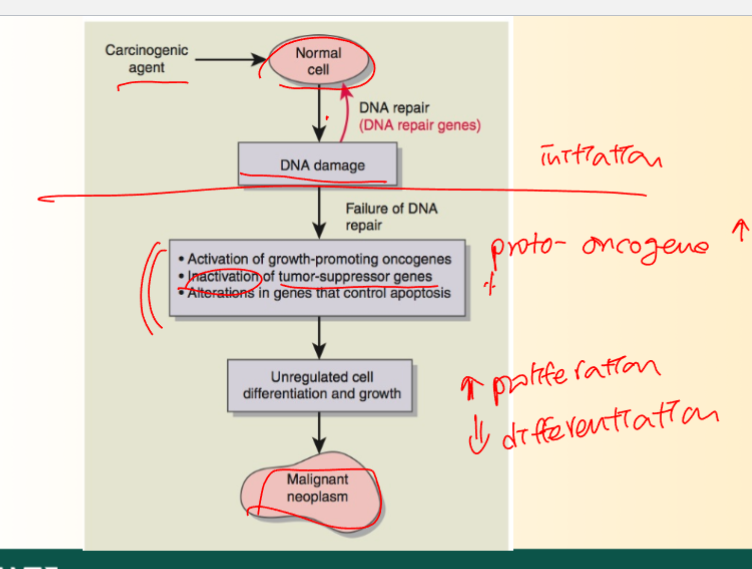
Carcinogenesis (3 Phase)
Normal cells change to cancerous cells
Initiation: exposure of cells to carcinogenic agent + DNA damaged
Promotion: start of unregulated growth (MUTATED not MALIGNANT YET)
Proliferation INCREASE, Differentiation DECREASE
Progression: tumor cells acquire malignant phenotype (NOW MALIGNANT, becomes a tumor mass)
Invade surrounding tissue
GF: VEGF (Increased vascular endothelial growth factor)
Alter overall tissue function
GROWTH RATE = EXPONENTIAL: because the cancerous cells keep dividing, and then those divide, and so on
Cancer Associated Gene (3)
Proto-oncogene:
Genes that promote proliferation
When mutated, stimulate constant, unrelenting proliferation + cell cycle
Tumor suppressor gene: stops proliferation
When defective/deactivated, lose ability to inhibit cell proliferation
Cancer then starts
p53 gene = tumor suppressor
Apoptotic + anti-apoptotic gene: genes regulating apoptosis either promoting or stopping
Unregulated = bad duhS
LOOK AT THIS
KNOw it
Mechanism allowing viruses to cause cancer
The initiation stage is caused by carcinogens that damage the DNA of our cells.
Some viruses act as carcinogens by entering the body and causing cell mutations, which begins the process of carcinogenesis.
Identify several cancer causing viruses
HPV (human papilloma viruses): causes cervical cancer
Epstein barr virus
Hepatitis B virus
Human herpes virus 8