ICCM - Quiz 1
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
what are the components to a preceptor presentation?
one-liner
past medical history
review of systems
physical exam
differential diagnosis
plan (meds, labs, imaging)
unstable angina diagnosis
history - pain at rest or a change in character of pain
additional - normal troponin, normal or minimal changes on EKG (potential ST depression or T wave inversion on EKG)
NSTEMI diangosis
positive troponin
additional - symptoms, no ST elevation on EKG, potential ST depression or T wave inversion on EKG
STEMI diangosis
ST elevation on EKG (2 continuous leads)
additional - positive troponin, symptoms, compensatory EKG changes
ACS medications
nitroglycerin
aspirin
heparin
ticagrelor - brand name is brilinta (alternative is clopidegrel)
ACS treatment
STEMI - cath lab within 90 min
unstable angina and NSTEMI - cath lab, but not immediately
nitroglycerin dosage for ACS
0.4 mg sublingual
repeat every 5 minutes for up to three doses
aspirin dosage for ACS
325 mg uncoated chewable
heparin IV bolus dosage for ACS
60 units/kg
max 4000 units
heparin IV drip dosage for ACS
12 units/kg
max 1000 units/hour
ticagrelor (brilinta) dosage for ACS
180 mg PO
clopidogrel dosage for ACS
300-600 mg loading dose
75mg PO QD after
what are the symptoms for atrial fibrillation?
palpitations, chest pain, dizziness, SOB
what are the two most common causes of atrial fibrillation?
CHF and sepsis
what are other causes of atrial fibrillation?
alcohol (holiday heart)
PE
pericarditis
myocarditis
valvular abnormalities
endocarditis
what trial supports that there is equal mortality to rhythm control vs rate control?
AFFIRM trial
what does the AFFIRM trial support?
equal mortality to rhythm control vs rate control in treatment for atrial fibrillation
the RACE II trial supports that when you rate control you should aim for a heart rate of what?
less than 110 bpm
what trial supports that you should aim for a heart rate of less than 110 bpm when rate controlling?
RACE II
what medications are used to rate control?
diltiazem or metoprolol
diltiazem dosage for rate control atrial fibrillation
bolus - 5, 10, 15, or 20 mg
drip - 5 mg/hour
what is happening during atrial fibrillation and what do you see on EKG?
multiple foci in the atria are firing, leading to the an irregularly irregular rhythm seen on EKG

what are you at risk for with atrial fibrillation?
stroke
what are the risk factors for atrial fibrillation?
hypertension
coronary artery disease
congestive heart failure
alcohol abuse
cocaine use
what arrhythmias are included in supra-ventricular tachycardia?
sinus tachycardia
atrial flutter
AVNRT - atrioventricular nodal reentrant tachycardia
AVRT - atrioventricular reentrant tachycardia (ex. WPW)
what does an EKG look like for supra-ventricular tachycardia?
regular narrow complex tachycardia

what is happening with the electrical conduction of the heart in sinus tachycardia?
follows normal pathway
heart rate >100 bpm
what is happening with the electrical conduction of the heart in atrial flutter?
dominant ectopic foci with an atrial rate of 250-350 bpm
what is happening with the electrical conduction of the heart in AVRT?
re-entry circuit through an accessory pathway (bundle of Kent)
what is happening with the electrical conduction of the heart in AVNRT?
re-entry circuit within or near the heart's AV node
what is the step-wise treatment for supra-ventricular tachycardia?
IV fluids
vagal maneuvers (valsalva, cough)
adenosine
which SVT would IV fluids treat?
sinus tachycardia
which SVT would vagal maneuvers treat and why?
AVRT or AVNRT
works by stimulating the vagus nerve -> blocking the AV node -> slowing down heart rate
which SVT would adenosine treat and why?
AVRT or AVNRT
works by producing a transient AV node block -> slowing down heart rate
which SVT would adenosine diagnose and why?
atrial flutter
works by slowing the conduction and can reveal the characteristic flutter waves on EKG, but won't break the rhythm/treat
why is adenosine considered diagnostic and therapeutic?
diagnostic - atrial flutter
therapeutic - AVRT and AVNRT
adenosine dosage for SVT
6, 12, 12 mg rapid IV push
what are the two types of ventricular tachycardia?
monomorphic
polymorphic
what does an EKG look like for ventricular tachycardia?
wide complex tachycardia
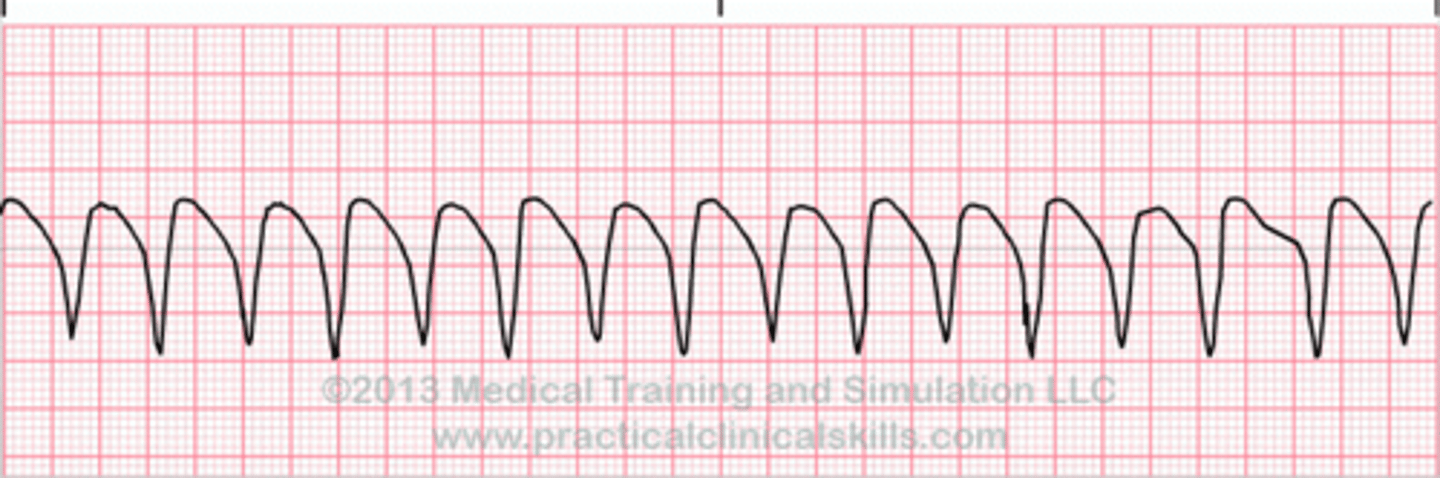
what are the treatment options for ventricular tachycardia for a patient with a pulse?
cardioversion
IV amiodarone
IV lidocaine
what is the treatment for ventricular tachycardia for a patient without a pulse?
defibrillation
what voltage is used to defibrillate a patient in ventricular tachycardia without a pulse?
300 joules (max)
amiodarone dosage for ventricular tachycardia
bolus - 150 mg IV over 10 minutes
drip - 1 mg/min for 6 hours
lidocaine dosage for ventricular tachycardia
bolus - 1 mg/kg IV
drip - 1-1.5 mg/kg at rate of 1-3 mg/min
T/F - amiodarone and IV lidocaine are equal mortality for treatment of ventricular tachycardia
true
what are the inferior EKG leads and artery associated?
II, III, aVF
RCA
what are the anterior EKG leads and artery associated?
V1-V4
LAD
what are the lateral EKG leads and artery associated?
I, aVL, V5, V6
LCfx
after an anterior STEMI what rhythm will a patient go into?
ventricular fibrillation
pulseless ventricular tachycardia
after an inferior STEMI what rhythm will a patient go into?
3rd degree heart block
normal PR interval for EKG
120s - 200 ms
normal QRS interval for EKG
< 120 ms
normal male QTc interval for EKG
< 440 ms
normal female QTc interval for EKG
< 460 ms
what does a prolonged QTc put a patient at risk for?
torsades de pointes
what labs and imaging should be obtained for all chest pain patients?
labs - CBC, CMP, magnesium, and troponin
imaging - EKG and chest x-ray
what is the dose for morphine and ondansetron (zofran) in the ED?
4 mg
gram positive bacteria list
staphylococcus
streptococcus
enterococcus
clostridium
listeria
bacillus
corynebacterium
gram negative bacteria list
escherichia
vibrio
salmonella
haemophilus
moraxella
pseudomonas
bartonella
pasturella
proteus
neisseria
klebsiella
enterobacter
helicobacter
yersinia
campylobacter
shigella
brucella
francisella
treponema
anaerobe bacteria list
bacteroides
eikenella
fusobacterium
eubacterium
atypical bacteria list
chlamydia
legionella
mycoplasma
what is unique about legionella
confirmatory diagnostic test - urine antigens
hyponatremia and elevated LFTs
what is the #1 cause of UTIs?
E. coli
what is the #2 cause of UTIs?
staphylococcus saprophyticus
what are 95% of blood culture contaminants?
staph epidermidis
staph hominis
staph haemolyticus
what are the different types of staphylococcus?
staph aureus
staph saprophyticus
staph epidermidis
staph hominis
staph hemolyticus
what are the different types of streptococcus?
alpha hemolytic - strep pneumoiae, strep viridans
beta hemolytic - group A (strep pyogenes), group B (strep agalactiae)
what are the different types of clostridium?
clostridium difficile
clostridium botulinum
clostridium perfringens
what are the different types of bacillus?
bacillus anthraces
bacillus cereus (reheated rice)
what are the non-STI chlamydias?
chlamydia pneumoniae
chlamydia psittaci
what is the history of penicillins?
discovered in 1928 by Dr. Fleming
a mold, Penicillium notatum, inhibited the growth of bacteria
what is the mechanism of action of penicillins?
inhibit bacterial cell wall synthesis
penicillin G (IM)
covers gram pos, gram neg, anaerobes
100% covers syphilis (treponema pallidum) and strep pyogenes
amoxicillin and ampicillin
covers gram pos, gram neg, anaerobes
100% covers strep pyogenes (not 100% for syphilis)
nafcillin, oxacillin, methacillin
covers gram pos ONLY
made to cover staph - good for MSSA
beta-lactamase inhibitors
covers gram pos, gram neg, anaerobes
amoxicillin/clavulanic acid (augmentin)
ampicillin/sulbactam (unasyn)
piperacillin/tazobactam (zosyn)
what is the MRSA and pseudomonas coverage for beta-lactamase inhibitors?
MRSA - no coverage from augmentin, unasyn, or zosyn
pseudomonas - no coverage from augmentin or unasyn; 95% coverage from zosyn
hospital medicine
ED - range of acuity
clinical decision unit - observed for further treatment
general floor - admitted to the hospital
step-down - intermediate level of care
critical care - patients who require close monitoring and management
inpatient roles and responsibilites
admitting, consulting, rounding, notes, physical exam, evaluating changes in patients, writing orders, charting
rounding team
physician, APPs, pharmacy, RT, students, nursing
inpatient evaluation
detailed charts - vitals, labs, PMHx, previous hospitalization, outpatient notes, consulting, nursing report
observe trends, abnormalities, and actionable findings to determine care
inpatient HPI
CC, risk factors, emergency room course, hospital course, PMHx, meds and allergies, social and family Hx, ROS
note formatting
H&P and consult H&P
consult or daily progress note
discharge summary and death summary
inpatient physical exam evaluation
five required systems - general, HEENT, respiratory, cardiovascular, abdomen, perivascular and extremities/pulses
other - MSK, skin, GU, lymphatic, psychosocial
general - normal and abnormal
normal - alert and oriented to person, place and time; in no acute distress
abnormal - lethargic, laying in bed and minimally responsive. Appears in respiratory distress with tachypnea and increased work of breathing
HEENT - normal and abnormal
normal - normocephalic, atraumatic, non-icteric sclera, EOM grossly intact, PERRL(A)
abnormal - pupils unequal; right 2mm with reaction to light and left 6mm without reaction to light
respiratory - normal and abnormal
normal - slear to auscultation bilateral without wheezes, rhonchi, or rales; no use of accessory muscles
abnormal - bilateral expiratory wheezing throughout all lung fields, diminished in bilateral bases. Tachypnea with RR ~30bpm and use of accessory muscles
cardiovascular - normal and abnormal
normal - regular rate and rhythm, no murmur gallops or rubs noted
abnormal - irregular irregular rhythm with HR ~ 130bpm. grade IV systolic ejection murmur heard best at left sternal boarder
abdomen - normal and abnormal
normal - soft, non-distended, non-tender to light and deep palpation, normo-active bowel sounds in all 4-quadrants
abnormal - distended, firm abdomen with diffuse TTP worse in RLQ with rebound tenderness present. Bowel sounds hypoactive in all 4 quadrants
perivascular - normal and abnormal
normal - no pedal edema, dorsalis pedis 2+ bilateral
abnormal - 3+ bilateral lower extremity pitting edema. Absent left popliteal pulse with cyanotic left foot
inpatient orders
admission order set - pre-built in orders that are common for admission
may need to add or remove some of the orders within the set
DVT prophylaxis in hospitalized medical adults
non-pharm - intermittent pneumatic compression
pharm options - lovenox 40mg SQ QD or SQ heparin (5000 units SQ BID or TID if obese or cancer patient (no renal dose is needed)
high-risk patient groups for DVT
patients at highest risk of VTE include patients who are critically ill, patients with cancer or stroke, and patients with multiple risk factors for VTE including pregnancy, heart failure, myocardial infarction, old age (>75 years), previous VTE, prolonged immobility, renal failure, obesity, and inherited or acquired hypercoagulable states
DVT prophylaxis in cancer patients
lovenox 40mg SQ QD
renal dose adjustment is needed
stress ulcer ICU
ulceration of the upper gastrointestinal (GI) tract (esophagus, stomach, duodenum) that occurs due to hospitalization and is common in critically ill patients
can be occult or overt
high risk groups for stress ulcers
mechanical ventilation for more than 48 hours
bleeding diathesis (thrombocytopenia (platelet <50,000)
elevated international normalized ratio >1.5 or a partial thromboplastin time >2 times the control value
GI ulceration or bleeding within the past year
traumatic brain or spinal cord injury
severe burns >35 percent of the body surface area
two or more minor risk factors (eg, sepsis, intensive care unit stay >1 week, occult GI bleeding ≥6 days, glucocorticoid therapy)
nonsteroidal anti-inflammatories or antiplatelet agents
stress ulcer prophylaxis in the ICU
first-line - PPIs (pantoprazole (protonix) 40mg PO daily)
second-line - H2 blockers (famotidine (pepcid) 20mg PO daily)
PPI MOA
block acid secretion by irreversibly binding to and inhibiting the hydrogen-potassium ATPase pump that resides on the luminal surface of the parietal cell membrane
H2 blocker MOA
antagonize the H2 receptors on the parietal cell, resulting in diminished gastric acid secretion
patient oral presentation
introduction - brief 1-liner, present HPI for new patients
data - vitals, pertinent physical exam, emergent/concerning labs
assessment and plan - principal problem and any secondary problems
use SOAP note format