Lecture 55: Skeletal Disease Processes 2
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
What is a benign, bony growth projecting outward from bone- typically originating at the periosteum?
exostosis
What is a bony growth at the margins of joints?
osteophyte
What is ossification of a tendon or ligament (forming abnormal bony projections) at the point of its insertion into the bone?
enthesophyte
What is uniform thickening of bone along the periosteal surface?
hyperostosis
What is a bony growth within the medullary cavity that can result in obliteration of the medullary cavity?
enostosis
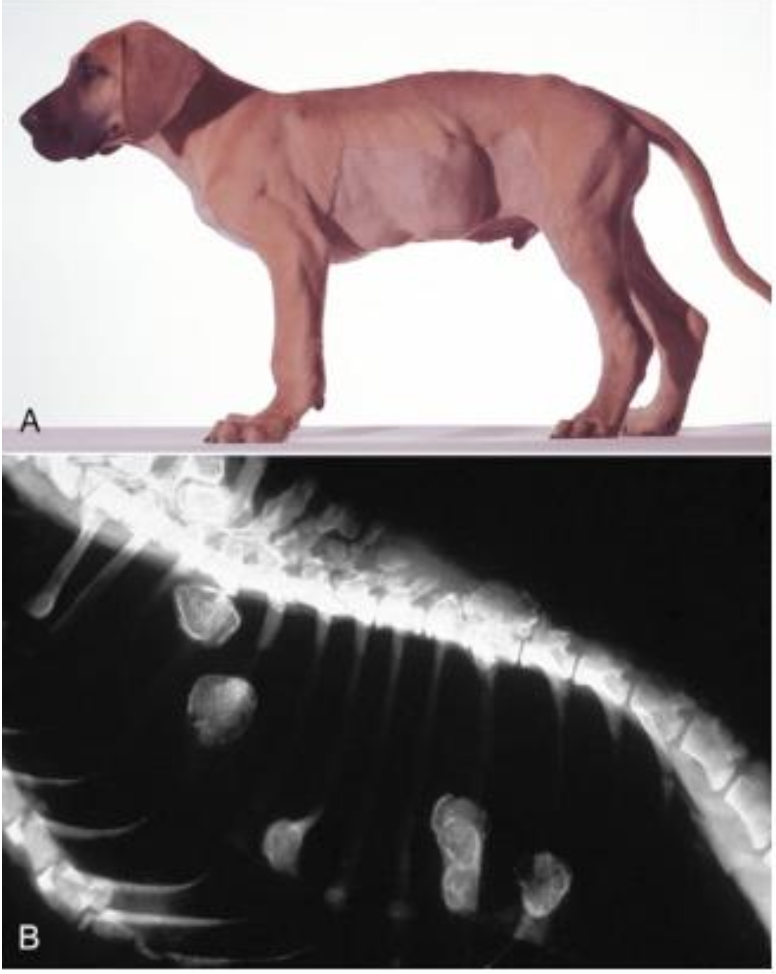
What is hypertrophic osteopathy?
Progressive, often bilateral, periosteal, new bone formation in the diaphyseal and metaphyseal regions, particularly of the distal limbs of dogs (most common) occurring as a secondary reaction to a primary space occupying lesion (usually intrathoracic neoplasm)

What has occurred in this canine tibia and fibula? note the dog also had an intrathoracic mass.
hypertrophic osteopathy
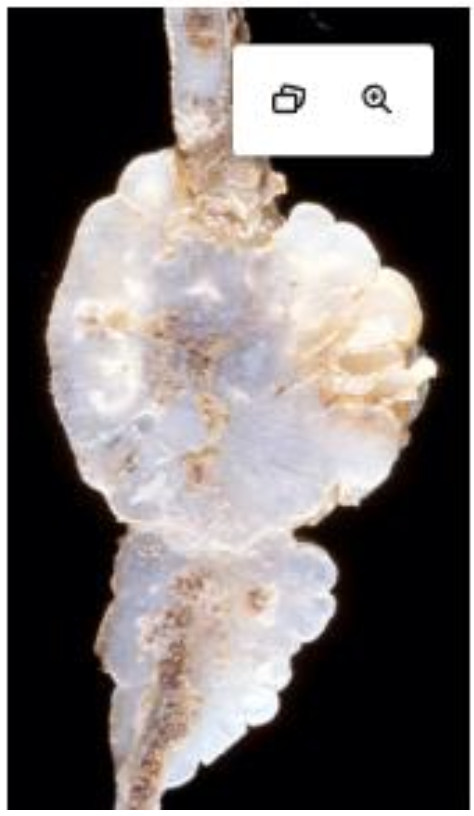
Where are osteochondromas located and in who?
adjacent to physes in young dogs and horses (mass usually stops growing when animal reaches skeletal maturity)
Where do osteochondromas NOT develop in dogs and horses?
on bones of intramembranous origins (ex. skull)
What makes osteochondromas in cats different?
they develop in mature animals and tend to be in flat bones instead of long bones

What is affecting this canine distal femoral metaphysis?
osteochondroma
What is this?
osteochondroma
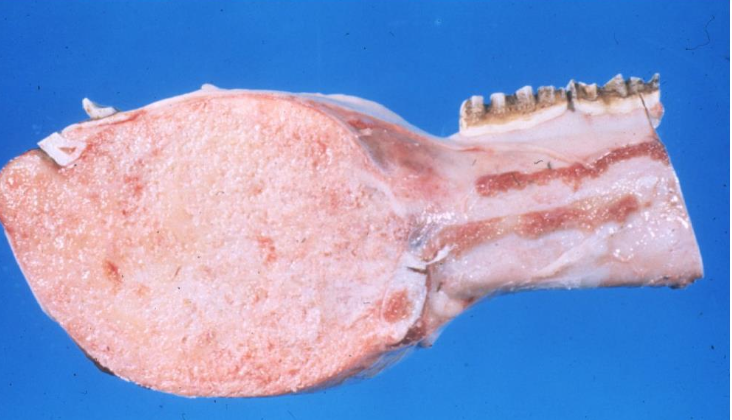
What are multilobular tumors of bone?
single, nodular, smooth-contoured, immovable masses that occur on flat bones of the skull and hard palate in middle aged/older dogs and cats

What is this mass on this canine skull? note the mass is firm and immovable.
multilobular tumor of bone
What are the benign neoplasms of hyaline cartilage often arising from flat bones of dogs, cats, and sheep? They have a blue-white appearance on cut section.
chondroma
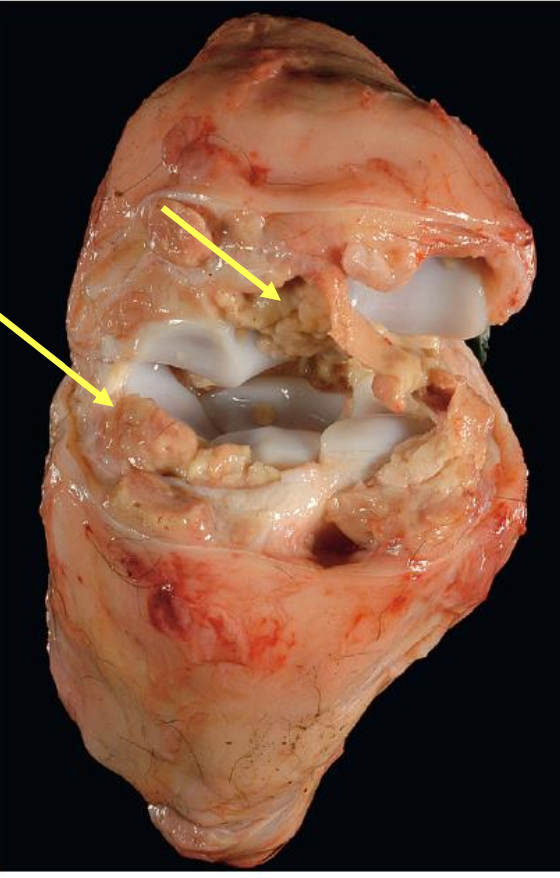
What are chondrosarcomas?
malignant neoplasms in which the neoplastic cells produce cartilaginous matrix but not osteoid or bone
Where are chondrosarcomas usually found?
flat bones in large breed dogs and sheep
dogs: nasal bones, ribs, and pelvis
sheep: ribs and sternum
What is affecting this feline rib? note the multilobulated white to gray mass with invasive destruction and loss of normal bone architecture.
chondrosarcoma
What are ossifying fibromas?
uncommon masses in the maxillae and mandibles of horses less than a year of age and cattle that can destroy adjacent cortical trabecular bone by expansile growth
What can be seen in this equine mandible?
ossifying fibroma
What bones does osteosarcoma have a predilection for in dogs and cats?
long bones (away from elbow - towards the knee)
ribs, vertebrae, bones of head etc

What is affecting this canine distal radius? note the reactive periosteal new bone formation and the large area of hemorrhage and necrosis.
osteosarcoma
What are the common skeletal sites of metastatic neoplasms in dogs? Where do they metastasize from?
rib shafts, vertebral bodies, and humoral/femoral metaphyses
mammary gland, liver, lung, and prostate
What is the difference between traumatic and pathologic bone fractures?
traumatic: normal bone broken by excessive force
pathologic: abnormal bone broken by minimal trauma or by normal weight bearing due to weakening from underlying disease
What two factors are important for callus formation during fracture repair?
hematoma and tissue necrosis → growth factors from hematoma and inflammation with necrosis begin process to stimulation proliferation of repair tissue (woven bone)
What is the primary (soft) callus in bone repair?
disorganized meshwork of woven bone formed by fibrous connective tissue and cartilage to bridge the gap, encircle the fracture site, and stabilize the area
What is the secondary (hard) callus?
more organized and stronger bone that replaces the primary callus at the fracture site
What are the 4 major steps of fracture repair?
hematoma formation
primary (soft) callus formation
secondary (hard) callus formation
bone remodeling (months to years): resolve callus and return to normal shape and architecture
What are the major complications of fracture healing?
inadequate blood supply
instability: excessive movement can result in too much fibrous tissue deposition that cannot act as a template for bone formation
infection
What is the difference between a stable and unstable fraction?
unstable: fractured edges improperly aligned, abundant external callus trying to stabilize region
stable: fractured edges adequately aligned, fracture stabilized by abundant cartilaginous callus that is replaced by bone
How can you tell if joint fluid is diseased?
normal joint fluid should be clear to pale yellow and viscous
diseased joint fluid has decreased viscosity and is more opaque
What are the common routes of infectious arthritis?
• Neonatal bacteremia secondary to omphalitis or oral-intestinal entry commonly leads to polyarthritis in lambs, calves, piglets, and foals.
• Bacteria can also reach the joint by direct inoculation (as in a puncture wound)
• Direct extension from periarticular soft tissue
• Extension from adjacent bone
What are the macroscopic lesions of septic/infection arthritis?
articular cartilage: eroded or ulcerated
synovial fluid: reduced viscosity and turbid due to neutrophils or fibrin
synovial membrane:
acute: hyperemia or mild edema
subacute: synovial hyperplasia
chronic: replacement of synovial membrane with granulation tissue and fibrosis
What is affecting this carpus of a calf? note the abundant yellow fibrin within the joint and the white glistening articular cartilage.
fibrinous synovitis

What is affecting this porcine stifle joint? note the villous hypertorphy of the synovial membrane.
chronic synovitis
What type of bacterial arthritis is expected with gram negative vs gram positive bacteria?
negative: fibrinous inflammation
positive: suppurative arthritis
What is a common cause of suppurative arthritis in cattle and pigs?
trueperella pyogenes
What is a common cause of acute serofibrinous polyarthritis in cattle?
histophilus somni
What is a cause of myocplasma (fibrinous) arthritis in pigs?
mycoplasma hyorhinis in pigs between 3-10 wks of age and mycoplasma hyosynoviae in pigs older than 3 months
What is a cause of myocplasma (fibrinous) arthritis in cattle?
mycoplasma bovis
What are the commonly seen lesions in goats with CAE (viral arthritis)?
chronic firbinous arthritis that can look like “rice grains” attached to synovium
carpal hygromas: fluid filled sac on dorsal aspect of joints (“big knee”)
What are the lesions commonly seen in nonerosive noninfectious - immune mediated polyarthritis?
joint pain, swelling, lameness in multiple joints
articular cartilage normal
synovial villous hyperplasia - minimal to marked
synovial fluid contains neutrophils with no bacteria
What concurrent sterile immune mediated diseases are associated with nonerosive noninfectious - immune mediated polyarthritis in dogs?
steroid responsive meningitis/arteritis, neoplasia, or SLE (systemic lupus erythematosus)