EMT Unit Exam Study (Airway, Ventilation and Respiratory)
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
118 Terms
Anatomy
Anatomy Answers
Physiology
The branch of biology that deals with the normal functions of living organisms and their parts.
Physiology Answers
Pathophysiology?
the disordered physiological processes associated with disease or injury.
Adult ventilation rates and adequate volumes?
Each breath should be delivered over 1 second with the minimum volume needed to produce chest rise. Initial ventilation rate for an adult should be 10 to 12 breaths per minute.
Beta Receptors?
Portions of the nervous system that, when stimulated, can cause an increase in the force of contraction of the heart, an increased heart rate, and bronchial dilation.
Alpha Receptors?
Portions of the nervous system that, when stimulated, can cause constrictions of blood vessels.
Alpha 1 Receptors?
Receptors found on vascular smooth muscle. Cause vascular restriction.
Stimulates blood vessels. Causes blood vessels to constrict; skin becomes pale, cool, clammy.
Alpha 2 Receptors?
Receptors found both in the brain and in the periphery (In the brain stem, they modulate sympathetic outflow).
Beta-1 Receptors?
Receptors located in the heart. When the receptors are stimulated they increase the heart rate and increase the heart's strength of contraction or contractility.
Stimulates the heart. Increases force of heart contraction.
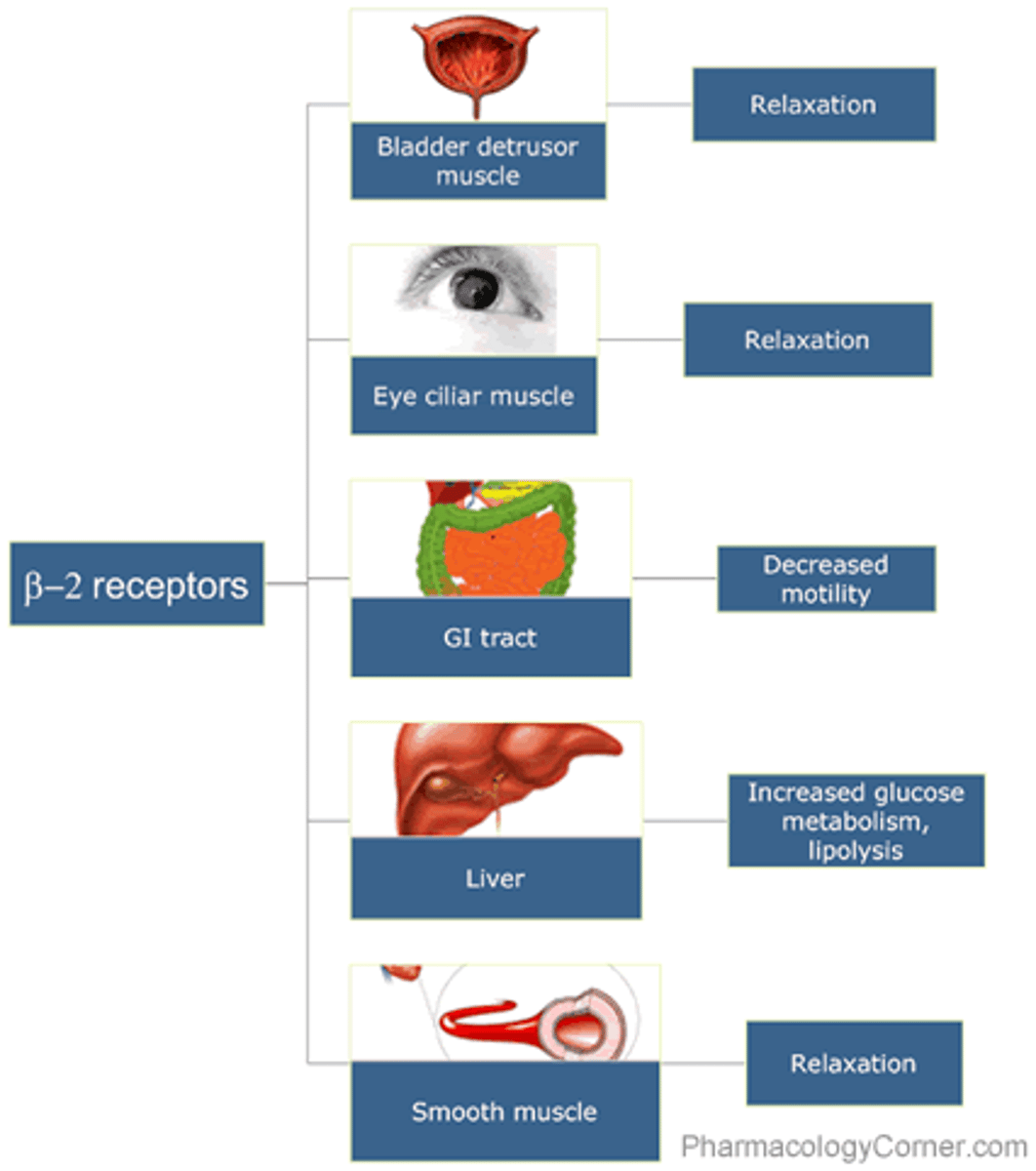
Beta-2 Receptors
Receptors located in the bronchioles of the lungs and the arteries of the skeletal muscles.
Stimulation of these receptors causes smooth muscle relaxation, which may result in peripheral vasodilation with subsequent hypotension and reflex tachycardia. Stimulation of theses receptors in the lungs causes bronchodilation, the desired clinical effect.
Stimulates the lungs. Causes bronchodilation.
Complications with tracheostomy tubes?
Cleaning or changing them.
1.Bleeding
2.Air trapped around the lungs (pneumothorax)
3.Air trapped in the deeper layers of the chest(pneumomediastinum)
4.Air trapped underneath the skin around the tracheostomy (subcutaneous emphysema)
5.Damage to the swallowing tube (esophagus)
6.Injury to the nerve that moves the vocal cords (recurrent laryngeal nerve)
7.Tracheostomy tube can be blocked by blood clots, mucus or pressure of the airway walls. Blockages can be prevented by suctioning, humidifying the air, and selecting the appropriate tracheostomy tube.
Treat by putting them in a comfortable position and providing suctioning to clear the obstruction. If unable to clear the airway consider ALS intervention. Once obstruction is clear oxygenate the patient.
Complications with hyperventilation?
Defined as overbreathing to the point that the level of arterial carbon dioxide falls below normal.
Can cause hypoxia or anxiety
The body is trying to compensate for acidosis, the buildup of excess acid n the blood or body tissues that results from the primary illness. Similarly, in an otherwise healthy person, blood acidity can be diminished by excessive breathing because it "blows off" too much carbon dioxide.
Dyspnea?
Shortness of breath or difficulty breathing.
Nocturnal dyspnea?
Severe shortness of breath, especially at night after several hours of reclining; the person is forced to sit up to breathe.
Hyperventilation?
Rapid or deep breathing that lowers the blood carbon dioxide level below normal.
Hypoxic drive?
The theory that the brain gradually accommodates high levels of carbon dioxide and then uses a "backup system" to control breathing based on low levels of oxygen, rather than high levels of carbon dioxide.
Frequently found in end-stage chronic obstructive pulmonary disease (COPD).
Breath Sounds: Wheezes?
A high pitched, whistling breath sound, characteristically heard on expiration in patients with asthma or chronic obstructive pulmonary disease.
Diseases:
1.Asthma
2.COPD
3.Congestive Heart Failure/Pulmonary Edema
4.Pneumonia
5.Bronchitis
6.Anaphylaxis
Signs and Symptoms:
1.Dyspnea
2.Productive or nonproductive cough
3.Dependent edema, Pink frothy sputum
4.Fever, Pleuritic chest pain
5.Clear or white sputum
6.Hives, Facial swelling, Stridor, nonproductive cough
Breath Sounds: Rhonchi?
Coarse breath sounds heard in patients with chronic mucus in the airways.
Diseases:
1.COPD
2.Pneumonia
3.Bronchitis
Signs and Symptoms:
1.Productive cough
2.Fever, Pleuritic chest pain
3.Clear or white sputum.
Breath Sounds: Crackles?
Rattling breath sounds signaling fluid in the air spaces of the lungs; formerly called rales.
Diseases:
1.Congestive Heart Failure (CHF)/Pulmonary Edema
2.Pneumonia
Signs and Symptoms:
1.Dependent edema, Pink frothy sputum
2.Fever, Pleuritic chest pain
Breath Sounds: Stridor?
A harsh, high-pitched, barking inspiratory sound often heard in acute laryngeal (upper airway) obstruction.
Diseases:
1.Croup
2.Epiglottis.
Signs and Symptoms:
1.Fever, Barking cough
2.Fever, Sore Throat, Drooling
Breath Sounds: Decreased or Absent Breath Sounds?
Apnea or the absence of spontaneous breathing.
Diseases:
1.Asthma
2.COPD
3.Pneumonia
4.Hemothorax
5.Pneumothorax
6.Atelectasis
Signs and Symptoms:
1.Nonproductive cough, dyspnea
2.Productive cough
3.Fever, pleuritic chest pain
4. Shock, respiratory distress
5.Dyspnea. pleuritic chest pain
6. Fever, decreased oxygen saturation
Asthma?
An acute spasm of the smaller air passages, called bronchioles, associated with excessive mucus production and with swelling of the mucous lining of the respiratory passages.
Be prepared to suction large amounts of mucus from the mouth and to administer oxygen.
Signs and Symptoms:
Wheezing on inspiration/expiration
Bronchospasm
Anaphylaxis?
An extreme, life-threatening, systemic allergic reaction that may include shock and respiratory failure.
In most cases, it can be treated with epinephrine (adrenalin).
Signs and Symptoms:
Flushed skin or hives (urticaria)
Generalized edema
Decreased blood pressure (hypotension)
Laryngeal edema with dyspnea
Wheezing or stridor
Bronchiolitis?
Inflammation of the bronchioles that usually occurs in children younger than 2 years and is often caused by the respiratory syncytial virus.
Signs and Symptoms:
Shortness of breath
Wheezing
Coughing
Fever
Dehydration
Tachypnea (increased breathing rate)
Tachycardia
Bronchitis?
An acute or chronic inflammation of the lung that may damage lung tissue; usually associated with cough and production of sputum and, depending on its cause, sometimes fever.
Signs and Symptoms:
Chronic cough (with sputum production)
Wheezing
Cyanosis
Tachypnea (increased breathing rate)
What is Chronic Obstructive Pulmonary Disease (COPD)?
A slow process of dilation and disruption of the airways and alveoli caused by chronic bronchial obstruction.
Often use accessory muscles to breathe, patients will exhale through pursed lips, digital clubbing (abnormal englargement of the ends of the fingers).
An umbrella term used to describe a few lung diseases such as emphysema and chronic bronchitis, an on going irritation of the trachea and bronchi.
Assist with a prescribed inhaler and allow them to sit upright if it is most comfortable.
Congestive Heart Failure (CHF)?
Occurs when the heart is unable to pump sufficient blood to meet the metabolic needs of the body; usually occurs as a complication of another condition.
Patients who are at risk have a history of hypertension and coronary artery disease and/ atrial fibrillation. It can lead to pulmonary edema.
Signs and Symptoms:
Dependent edema
Crackles (pulmonary edema)
Orthopnea
Paroxysmal nocturnal dyspnea
Difficulty breathing with exertion
Swollen legs and feet (pedal edema)
Common Cold?
Upper respiratory tract infection/viral rhinitis, enters through nose
Signs and Symptoms:
Cough
Runny or stuffy nose
Sore throat
Pathophysiology of Congested Heart Failure (CHF)?
A disease of the heart characterized by shortness of breath, edema, and weakness.
Patient may or may not smoke.
Damaged ventricles and failure of the heart as a pump.
An attempt by heart to compensate with an increased rate.
Enlarged left ventricle.
Backup of fluid into the body as the heart fails to pump adequately.
What how do you know if it is left side Chronic Heart Failure (CHF)?
Check the lungs you will be able to hear crackles on expiration.
What how do you know if it is right side Chronic Heart Failure (CHF)?
Check for edema (swelling) in the legs, ankles, and swelling within the abdomen such as the GI tract and liver.
Pathophysiology of COPD?
A slow process of dilation and disruption of the airways and alveoli caused by chronic bronchial obstruction.
Usually in long-term smokers.
Emphysema:
Destruction of the airways distal to the bronchiole.
Destruction of the pulmonary capillary beds.
Decreased ability to oxygenate the blood.
Lower cardiac output and hyperventilation.
Development of muscle wasting and weight loss.
Chronic Bronchitis:
Excessive mucus production with airway obstruction.
Pulmonary capillary bed undamaged.
Compensation by decreasing ventilation and increasing cardiac output.
Poorly ventilated lungs, leading to hypoxemia.
Increased carbon dioxide retention.
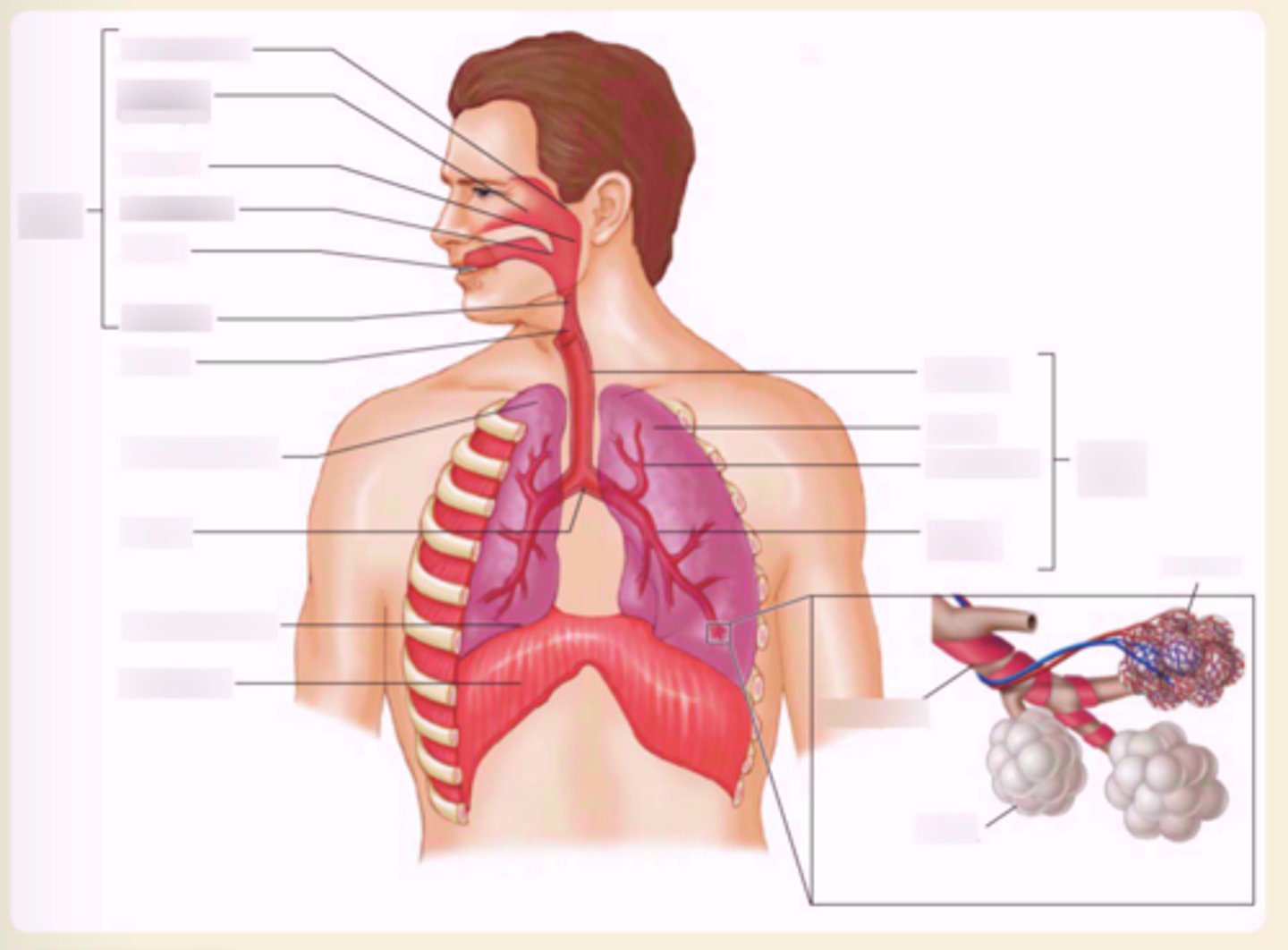
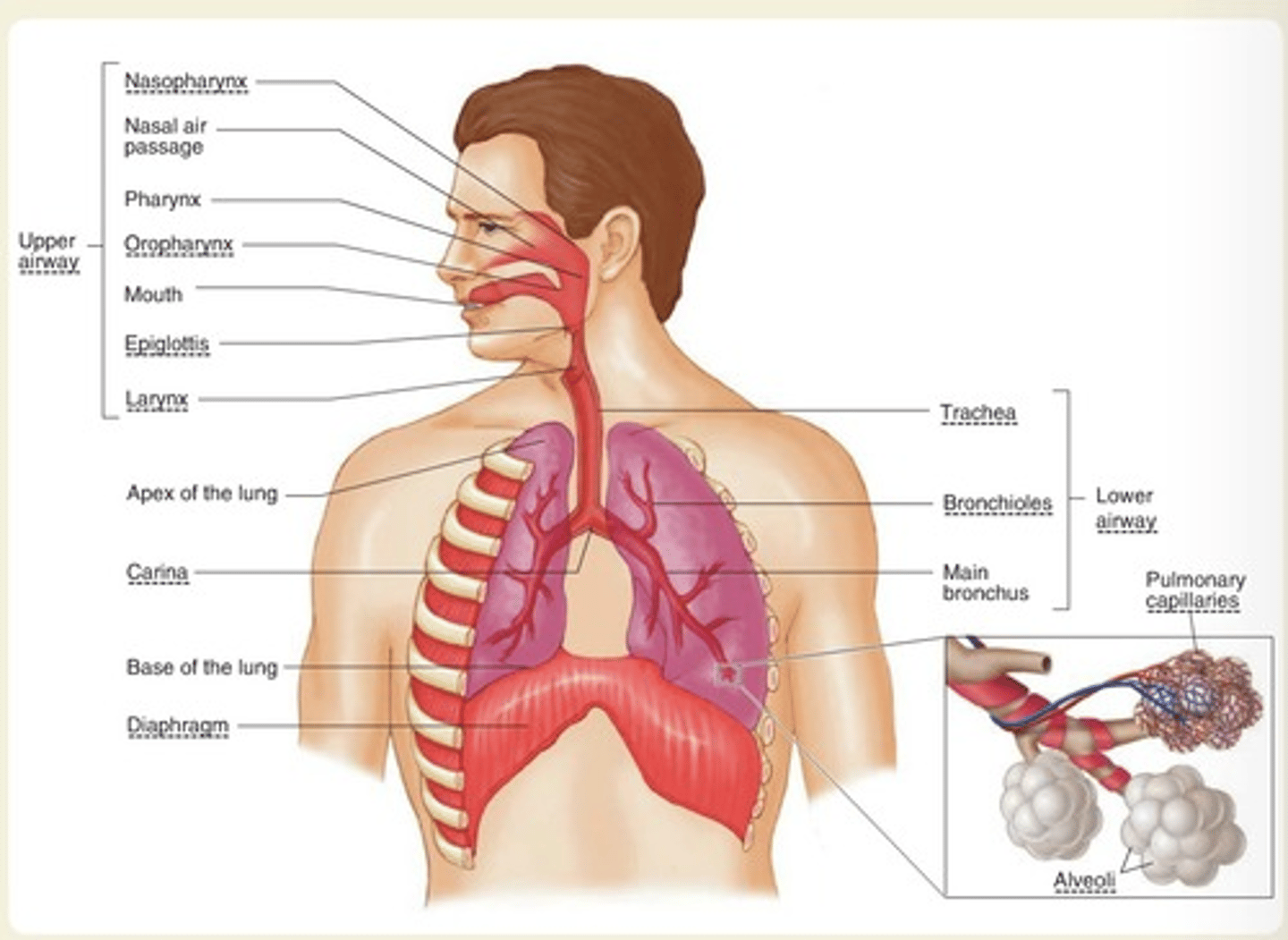
Pathophysiology of the upper airway?
To act as a conductor of air.
To humidify and warm or cool the inspired air.
To prevent foreign materials from entering the tracheobronchial.
To serve as an important area in speech and smell.
Upper airway consists of: Nose, oral cavity, pharynx, and larynx.
Pathophysiology of the lower airway?
Deliver oxygen to the alveoli.
Trachea, bronchioles, main bronchus
Croup?
An inflammatory disease of the upper respiratory system that may cause a partial airway obstruction and is characterized by a barking cough; usually seen in children.
Signs and Symptoms:
Fever
Barking cough
Stridor
Mostly seen in pediatric patients
Diphtheria?
An infectious disease in which a membrane forms, lining the pharynx; this lining can severely obstruct the passage of air into the larynx.
Signs and Symptoms:
Difficulty breathing and swallowing
Sore throat
Thick, gray buildup in throat or nose
Fever
Emphysema?
A disease of the lungs in which there is extreme dilation and eventual destruction of the pulmonary alveoli with poor exchange of oxygen and carbon dioxide; it is one form of chronic obstructive pulmonary disease.
Can present adventitious breath sounds such as crackles, rhonchi, and wheezes, or may have severely diminished breath sounds due to poor air movement.
Signs and Symptoms:
Barrel chest
Pursed lip breathing
Dyspnea on exertion
Cyanosis
Wheezing/decreased breath sounds
Epiglottitis?
A disease in which the epiglottis becomes inflamed and enlarged and may cause an upper airway obstruction.
Signs and Symptoms:
Dyspnea
High fever
Stridor
Drooling
Difficulty swallowing
Severe sore throat
Tripod or sniffing position
Tension pneumothorax?
A life-threatening collection of air within the pleural space; the volume and pressure have both collapsed the involved lung and caused a shift of mediastinal structures to the opposite side.
Results from the air in the alveoli space and causes everything to get pushed in a direction.
Signs and Symptoms:
Severe shortness of breath
Decreased/altered level of consciousness
Neck vein distension
Tracheal deviation (late sign)
Hypotension; signs of shock (late sign)
Pulmonary Embolus?
A blood clot that breaks off from a large vein and travels to the blood vessels of the lung, causing obstruction of blood flow.
Signs and Symptoms:
Sharp chest pain
Sudden onset
Dyspnea
Tachycardia
Clear breath sounds initially
Treat by providing supplemental oxygen (mandatory), place in a comfortable position, and assist with breathing if necessary.
Pulmonary emboli may cause cardiac arrest.
Tuberculosis (TB)?
A disease that can lay dormant in a person's lung for decades, then reactive; many strains are resistant to antibiotics. TB is spread by cough.
Signs and Symptoms:
Cough
Fever
Fatigue
Productive/bloody sputum
Respiratory Syncytial Virus (RSV)?
A virus that causes an infection of the lungs and breathing passages; can lead to other serious illnesses that affect the lungs or heart, such as bronchiolitis and pneumonia. RSV is highly contagious and spread through droplets.
Signs and Symptoms:
Cough
Wheezing
Fever
Dehydration
Influenza Type A (Flu)?
A virus that has crossed the animal/human barrier and has infected humans, recently reaching a pandemic level with the H1N1 strain.
Can lead to pneumonia or dehydration.
Signs and Symptoms:
Cough
Fever
Sore throat
Fatigue
Pertussis (Whooping Cough)?
An airborne bacterial infection that affects mostly children younger than 6 years. Patients will be feverish and exhibit a "whoop" sound on inspiration after a coughing attack; highly contagious through droplet infection.
Can identify if a patient looks dehydrated.
Signs and Symptoms:
Coughing spells
"Whooping" sounds
Fatigue
Pneumonia?
An infectious disease of the lung that damages lung tissue.
A secondary infection, meaning it begins after an upper respiratory tract infection such as a cold or sore throat.
If the oxygen exchange at the alveoli is markedly impaired, the lips, fingers, and nails may be blue or gray.
If in the lower part of the lungs near the abdomen they may have a fever, abdominal pain, and vomiting rather than dyspnea.
Signs and Symptoms:
Dyspnea
Chills, fever
Cough
Green, red, or rust-colored sputum
Localized wheezing or crackles
Pneumothorax?
A partial or complete accumulation of air in the pleural space.
Normally, the "vacuum" pressure in the pleural space keeps the lung inflated. When the surface of the lung is disrupted, however, air escapes into the pleural cavity and results in loss of negative vacuum pressure. The natural elasticity of the lung tissue causes the lung to collapse.
Signs and Symptoms:
Sudden chest pain with dyspnea
Decreased breath sounds (affected side)
Subcutaneous emphysema
Treat by providing supplemental oxygen and prompt transport to a hospital.
Automatic Transport Ventilator (ATV)?
A ventilation device attached to a control box that allows the variables of ventilation to be set. It frees the EMT to perform other tasks while the patient is being ventilated.
Aerobic Metabolism?
Metabolism that can proceed only in the presence of oxygen.
Anaerobic Metabolism?
The metabolism that takes place in the absence of oxygen; the principal product is lactic acid.
Ataxic Respirations?
Irregular, ineffective respirations that may or may not have an identifiable pattern.
Chemoreceptors?
Monitor the levels of O2, CO2, and the pH of the cerebrospinal fluid and then provide feedback to the respiratory centers to modify the rate and depth of breathing based on the body's needs at any given time.
What is an adequate tidal volume for an adult?
500mL
What respiratory emergency causes patients to rely on hypoxic drive?
Patients with COPD.
What lungs sounds are associated with Asthma?
Wheezes.
What lungs sounds are associated with Chronic Heart Failure (CHF)?
Crackles.
What lungs sounds are associated with Infection?
Rhonchi.
What lungs sounds are associated with Airway Obstruction?
Stridor.
Internal Respiration?
The exchange of gases between the blood cells and the tissues.
Dead Space?
The portion of the tidal volume that does not reach the alveoli and thus does not participate in gas exchange.
Compliance?
The ability of alveoli to expand when air is drawn in during inhalation.
Mediastinum?
Space within the chest that contains the heart, major blood vessels, vagus nerve, trachea, major bronchi, and esophagus; located between the two lungs.
Phrenic Nerve?
Nerve that innervates the diaphragm; necessary for adequate breathing to occur.
Intrapulmonary Shunting?
Bypassing of oxygen-poor blood past nonfunctional alveoli to the left side of the heart.
How do you treat and oxygenate a patient with COPD?
Do not overload them with oxygen but do not starve them, provide gentle slow respirations.
Administrate low-flow oxygen (2 L/min) is a good start, with adjustments to 3 L/min, the 4 L/min, and so on until the symptoms have improved.
What are the 3 rules for suctioning techniques?
1. Only on the way out.
2. Adult = 15 sec, Child = 10 sec, Neonate = 5 sec.
3. Only go in as far as you can see.
Sufactant?
A liquid protein substance that coats alveoli in the lungs, decreases alveolar surface tension, and keeps the alveoli expanded; a low level in a premature infant contributes to respiratory distress syndrome.
Visceral Pleura?
The membrane that covers the lungs.
Vital Capacity?
The amount of air that can be forcibly expelled from the lungs after breathing in as deeply as possible.
Diffusion?
A process in which molecules move from an area of of higher concentration to an area of lower concentration.
During inhalation what does oxygen do?
Moves from the atmosphere into the lungs, then crosses the alveolar membrane onto hemoglobin (blood).
What is Ventilation?
The simple movement of air into and out of the lungs.
What is Respiration?
The exchange of oxygen and carbon dioxide in the alveoli and tissue of the body.
What are Kussmaul Respirations?
Characterized as deep, rapid respirations commonly seen in patients with metabolic acidosis.
What are Cheyne-Stokes Respirations?
An irregular respiratory pattern in which the patient breathes with an increasing rate and depth of respirations that is followed by a period of apnea, or lack of spontaneous breathing, followed again by a pattern of increasing rate and depth of respirations.
Coronal Plane?
Divides the body into a frontal and back portion.

Transverse (Axial) Plane?
divides the body into a top and bottom portion.

Sagittal (Lateral) Plane?
Divides the body into right and left sides.

What are the parts of the upper airway?
Nasopharynx, Pharynx, Oropharynx, Epiglottis.
What are the parts of the lower airway?
Larynx, Trachea, Alveoli, Bronchioles, Main Bronchi, Carina, Diaphragm.
Pleural Space?
The potential space between the parietal pleura and the visceral pleura. It is described as "potential" because under normal conditions, the space does not exist.
Pleura?
The serous membrane covering the lungs and lining the thorax, completely enclosing a potential space known as the pleural space.
How do you get Minute Volume?
Respiratory rate x Tidal Volume.
What carries oxygenated blood to the heart?
Pulmonary veins.
What carries deoxygenated blood to the lungs?
Pulmonary artery.
What part of the heart do the pulmonary veins bring oxygenated blood to?
Left atrium then falls to the left ventricle.
What part of the heart receives deoxygenated blood?
The right atrium and falls to the right ventricle.
What brings deoxygenated blood back to the heart?
The inferior and superior vena cava.
What is oxygenated blood pushed out to the body through?
Through the Aorta and splits to the Artery (upper) and Aorta (lower).
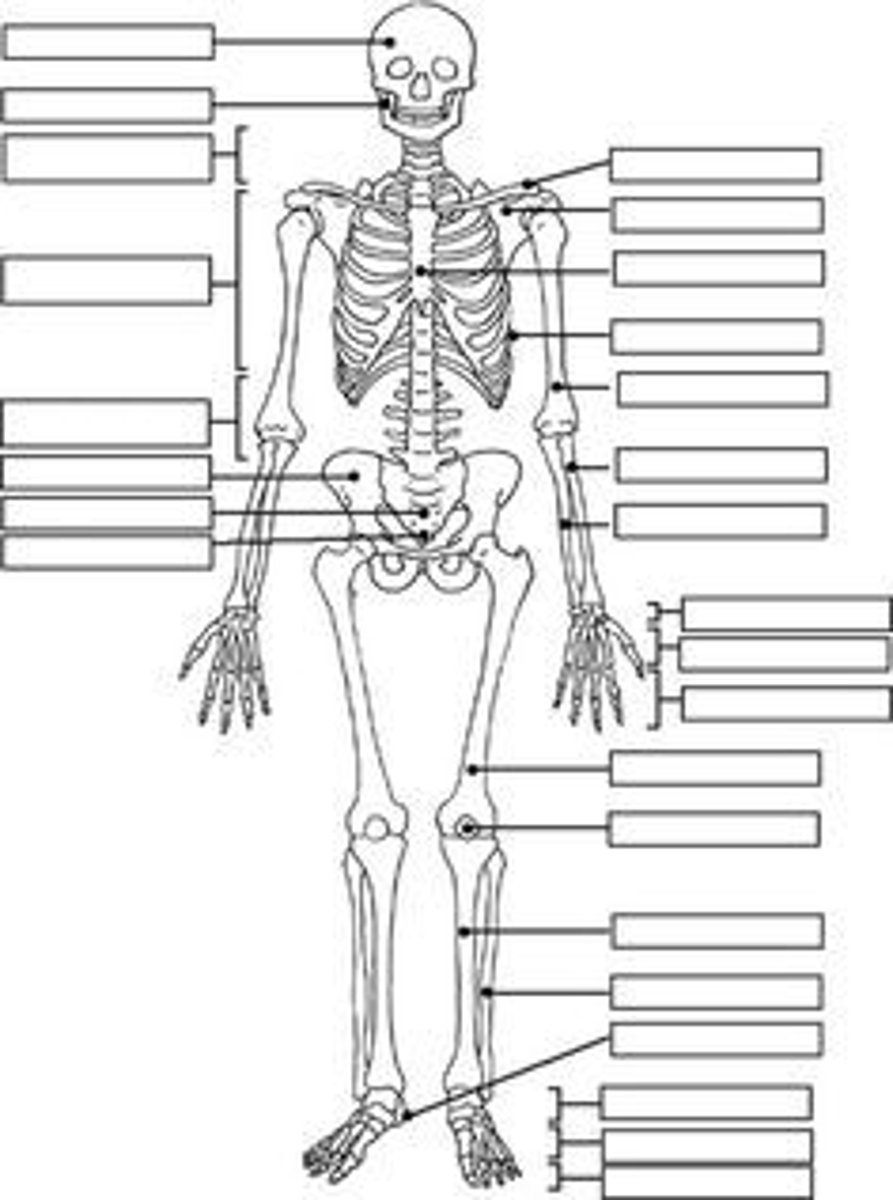
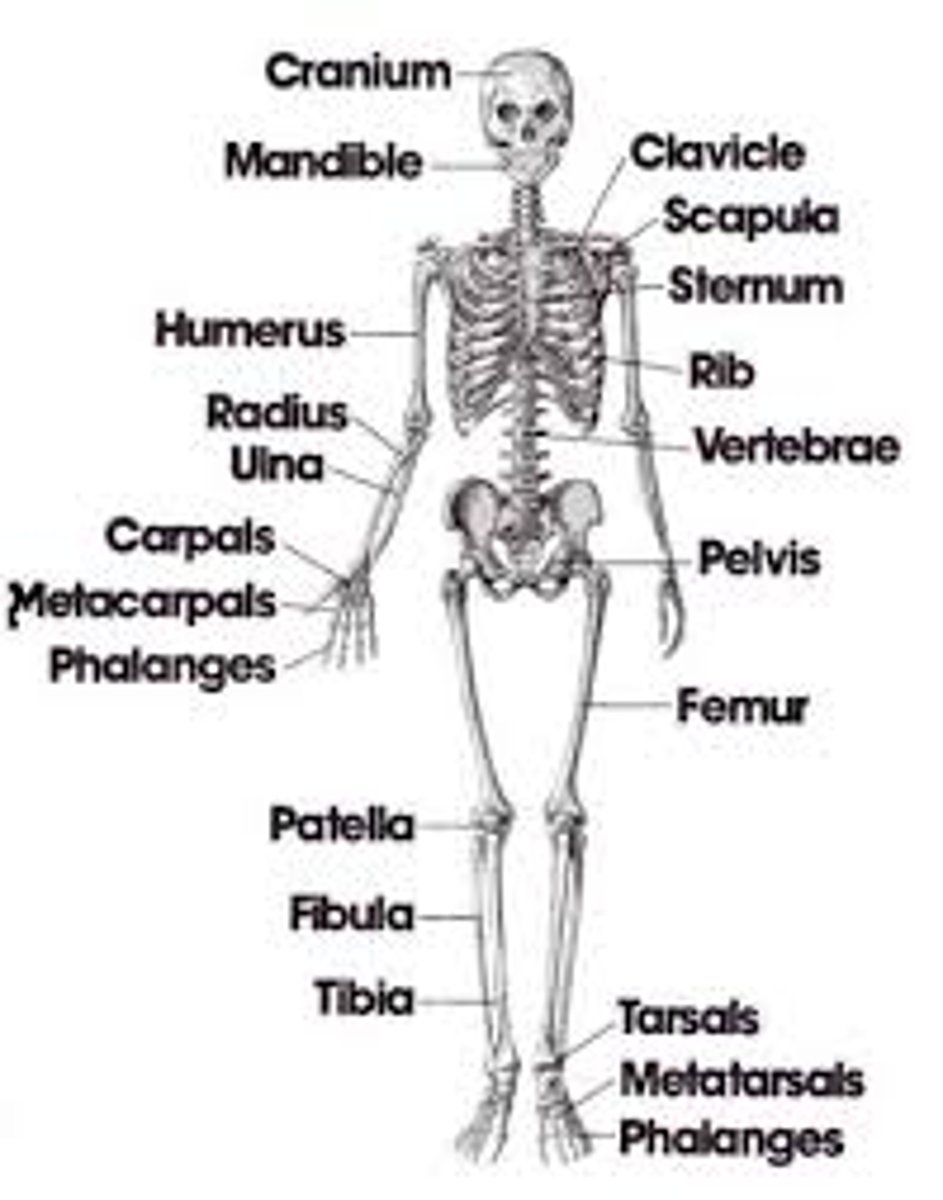
Where can someone check for pulses?
Carotid Artery (most common), Femoral Artery, Radial Artery (most common), Brachial Artery, Posterior Tibial Artery, Dorsalis Pedis Artery.
What does the Cerebrum do?
On one side of the brain controls activities on the opposite side of the body.
What does the Cerebellum do?
Coordinates the various activities of the body, particularly body movements.
What does the Brain Stem do?
Control center for virtually all body functions that are absolutely necessary for life. Cells in this part of the brain control cardiac, respiratory, and other basic body functions such as the regulation of consciousness.
What organs are in the Right Upper Quadrant?
Liver, Gallbladder, Bile Duct, and one of the Kidneys.
What organs are in the Right Lower Quadrant?
Appendix, and parts of the small and large intestine.
What organs are in the Left Upper Quadrant?
Stomach, Spleen, and one of the kidneys.
What organs are in the Left Lower Quadrant?
Parts of the large intestine and small intestine.
What does the Liver do?
Production of bile, assists with carbohydrate, protein, and fat metabolism of nutrients within the bloodstream, manufactures proteins for immune regulation and clotting, detoxification of blood, elimination of waste.
What does the Pancreas do?
Regulates glucose metabolism and other functions.
Exocrine: enzymes for protein, carbohydrate, and fat breakdown within the duodenum, Endocrine: insulin and glucagon.