Exam 2
1/153
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
154 Terms
Responsibility of an EKG technician
Is to generate a correct and readable EKG tracing. This Learning Objective is an overview of situations that might require changes to the usual EKG procedures in order to achieve that goal.
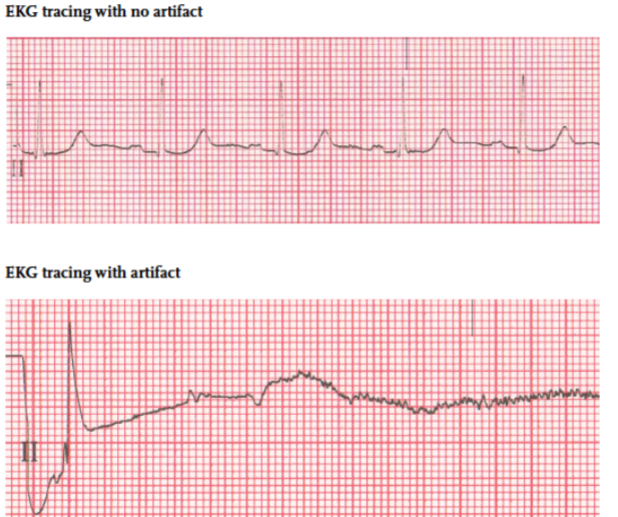
Artifact
interference or distortion that appears on an EKG tracing - may be caused by
Environmental factors
Defective equipment
Patient conditions
These patient conditions/situations may require changes to standard EKG testing:
• Pregnancy beyond the sixth month
• Limb amputation or injury
• Presence of scar tissue/broken skin
• Situations in which the patient’s age or health condition affects the position of the heart
EKG procedures may also have to be adapted for patients under Transmission-Based Precautions:
Disposable lead wires may be used
Testing may take place in a specially ventilated room
There may be different or additional procedures required for disinfection of EKG equipment after testing
EKG technicians should always follow any special infection prevention measures noted in the patient’s record or required by the facility
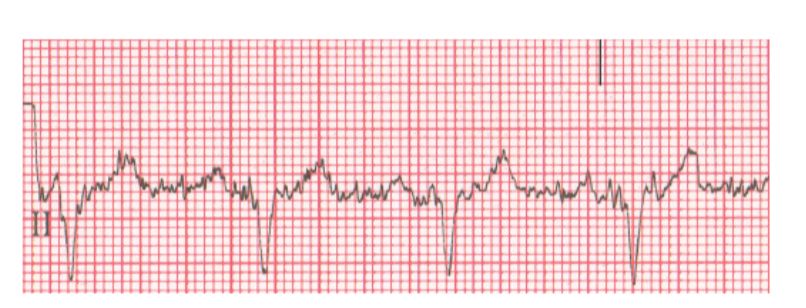
somatic tremor
EKG artifact usually caused by patient tremors or shivering.
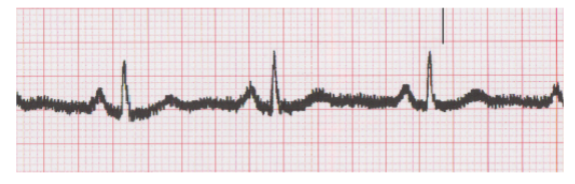
wandering baseline
EKG artifact in which the normally flat baseline moves up and down across the tracing.

abrade
in electrocardiography, to lightly scrub the outer layer of the skin to remove debris that can interfere with electrode contact.
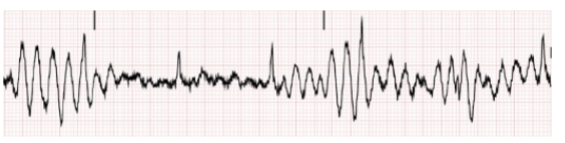
electrical interference
in electrocardiography, a type of artifact caused by the presence of other appliances or equipment in the area surrounding the EKG machine
broken recording
EKG artifact that occurs when the signal is compromised by frayed or faulty lead wires
Remember these points about addressing somatic tremor artifact:
Patients with Parkinson’s disease or other medical problems may need to be positioned with their hands palms-up under their buttocks to reduce tremors
Placing limb electrodes on the torso may reduce artifact in patients with tremors
Blankets can help stop tremors in patients who are cold, as can increasing the room temperature
Pillows may be used to make a patient more comfortable and less likely to tremble or move
Anxious or nervous patients should be reassured and given time to relax
Remember these points about addressing wandering baseline artifact:
Movement of muscle groups like those used for breathing can cause wandering baseline, so it can be helpful to remind patients to remain still and breathe normally
Placing the electrodes for the limb leads on the wrists and ankles can help eliminate wandering baseline caused by breathing irregularities
Loose electrodes or poor electrode contact are common causes of wandering baseline. The following skin preparation techniques can improve electrode contact:
Remove sweat or moisture with towel, paper towel, or gauze pads.
Remove skin oil or substances like lotion with soap and water.
Gently abrade the skin using dry gauze or a special skin abrading product.
Remove body hair as needed to increase contact between skin and electrodes (use only medical clippers)
Remember these points about addressing electrical interference artifact:
Turn off other electrical appliances in the area
Plug the EKG machine in to a different outlet
If an extension cord is being used, discontinue use of extension cord
Make sure the machine is properly grounded (three prongs on the cord, plugged in to a three-prong outlet)
Turn off fluorescent lights
Mobile phones can cause electrical interference, so any phones in the room should be removed from the immediate testing area
Making a habit of double-checking all of the following will help ensure accurate, artifact-free EKG tracings:
Fresh, in-date electrodes adhering properly to the patient’s skin
Electrodes in the correct locations and attached to the correct lead wires
Lead wires properly connected to the electrodes and to the machine
Lead wires not frayed or damaged in any way
dextrocardia
a rare heart condition that causes the heart to develop pointing to the right side of the chest instead of the left side.
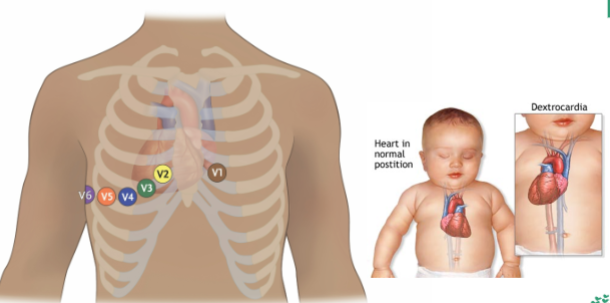
Remember these points about dextrocardia:
It is a rare heart condition that causes the heart to develop pointing to the right side of the chest rather than to the left side
The patient is usually aware of this condition or it is noted in the chart
If the electrodes are placed in the standard, left-sided positions, the EKG will not be accurate
Remember these points about electrode placement for patients with limb amputation or injury:
A patient who has had a limb amputation or who has an injury that limits access to a limb requires adapted electrode placement
The key for adaptations is that the electrode for the corresponding, unaffected limb should be placed in a mirror position

Remember these points about electrode placement for patients who have undergone mastectomy or who have scars on/injury to the chest wall
Avoid placing electrodes on scar tissue, which can be fragile and may be injured when the electrode is removed
Electrodes should be placed as close as possible to the standard locations
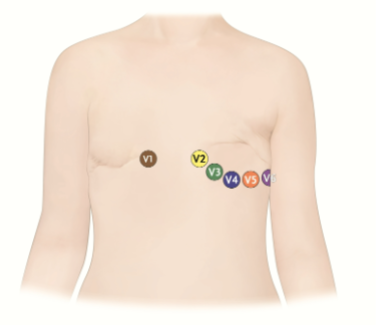
Remember these points about electrode placement for patients with large breasts:
Move breast tissue away from the electrode site as much as possible so the electrodes are placed on the chest wall
Explain the process to the patient and get the patient’s consent before making any contact
The patient can lift her own breast tissue or the technician can use the back of a hand to move the tissue
Electrodes should be placed as closely as possible to the standard position and should not be placed on top of breast tissue
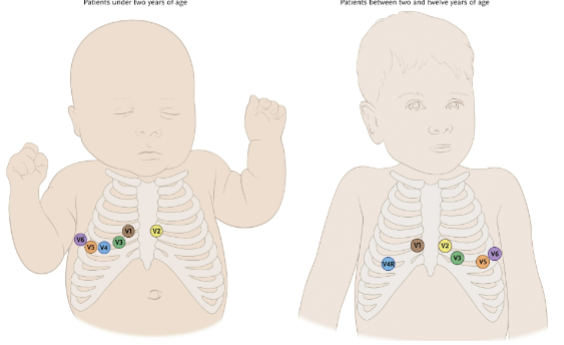
Electrode placement for pediatric patients differs from placement for adult patients:
Children under two years of age require right-sided placement
Children between two and twelve require adapted placement as shown in the next slide
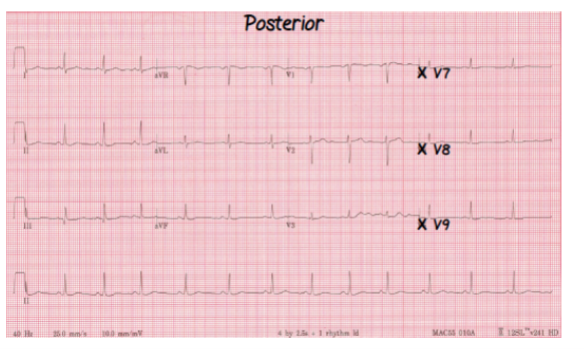
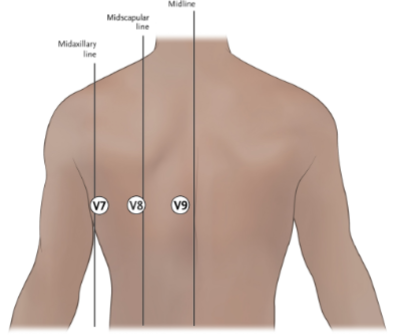
Remember these points about posterior EKGs:
Sometimes a doctor will ask to have an EKG repeated using posterior leads
This can help to diagnose a particular type of heart attack (inferior wall myocardial infarction)
Patient health conditions or circumstances might require changes to positioning:
Respiratory or heart problems might make it difficult for patients to tolerate supine position. Semi-Folwer’s position will likely be more comfortable for these patients.
Patients who are six months or more pregnant should not be placed in the supine position. Pillows can be used to tilt these patients to the left, taking pressure off the vena cava.
Cardiac output in an essential measure of the function of the heart:
Cardiac output is the amount of blood, measured in liters, that the heart pumps each minute
Cardiac output per minute = amount of blood pumped with each heartbeat (stroke volume) multiplied by the number of heartbeats per minute
If cardiac output is low, the patient’s health will suffer
Low output can be caused by electrical and mechanical problems
These requirements have to be met in order for the heart to pump blood through the body:
Electrical system of the heart working properly
Mechanical components (muscle and valves) healthy
Enough blood to pump through an intact vascular system
cardiac conduction system
the pathway of electrical impulses that controls the heart’s pumping action.
intrinsic rate
the normal firing rate (expressed in beats per minute) associated with a part of the heart’s electrical conduction system.
sinoatrial node
part of the electrical conduction system of the heart, located in the upper part of the right atrium and acting as the primary pacemaker of the heart, with an intrinsic rate of 60–100 BPM; also called the SA node or sinus node
pacemaker
something that regulates the heart’s contractions; natural pacemakers are part of the cardiac conduction system, with the sinoatrial (SA) node acting as the primary pacemaker when the heart is functioning normally. An artificial pacemaker is a battery-powered device that creates electrical impulses to stimulate the heart
atrioventricular node
part of the electrical conduction system of the heart, located at the bottom of the right atrium, behind the tricuspid valve, with an intrinsic rate of 40–50 BPM.
atrioventricular (AV) junction
part of the electrical conduction system of the heart, located between the AV node and the bundle of His.
bundle of His
part of the electrical conduction system of the heart, located in the upper part of the interventricular septum, with an intrinsic rate of 40–50 BPM; also called AV bundle.
bundle branches
part of the electrical conduction system of the heart; they divide from the bundle of His and carry the electrical impulse to the walls of the ventricles.
Purkinje fibers
part of the electrical conduction system of the heart; they divide from the bundle branches and have an intrinsic rate of 20–40 BPM.
irritable
in reference to the cardiac conduction system, more likely to initiate an electrical impulse at the wrong time or in the wrong location.
Remember these points about the cardiac conduction system:
The SA node is the primary pacemaker of the heart.
Other areas of the conduction system can initiate an impulse if it fails.
Lack of oxygen or other problems in the heart could cause another area to initiate an impulse, as well
isoelectric line
on an EKG tracing, the straight line between upward and downward movements (also sometimes called the baseline)
wave
on an EKG tracing, movement upward or downward from the isoelectric line; a positive wave moves upward and a negative wave moves downward.
segment
on an EKG tracing, the isoelectric area between two waves.
interval
on an EKG tracing, a wave and a segment taken together.
complex
several EKG waves considered together.
morphology
the shape and direction of waves, complexes, and segments on an EKG tracing.
normal sinus rhythm
cardiac rhythm produced when the electrical system of the heart is functioning normally.
P wave
in normal sinus rhythm, the first positive deflection (upward movement) seen on an EKG tracing; corresponds to the contraction of the atria.
QRS complex
an EKG complex that includes the Q, R, and S waves and corresponds to the contraction of the ventricles; appearance in EKG tracings can vary widely.
T wave
an EKG wave that follows the QRS complex and corresponds to the relaxation of the ventricles.
PR interval
on an EKG tracing, the interval from the beginning of the P wave to the beginning of the QRS complex.
QRS interval
the length of time associated with a complete QRS complex on an EKG tracing; normal measurement is less than 0.12 seconds
R-R interval
on an EKG tracing, the interval between the R wave of one complex and the R wave of the next complex
ST segment
on an EKG tracing, the segment between the J point (the end of QRS) to the beginning of the T wave
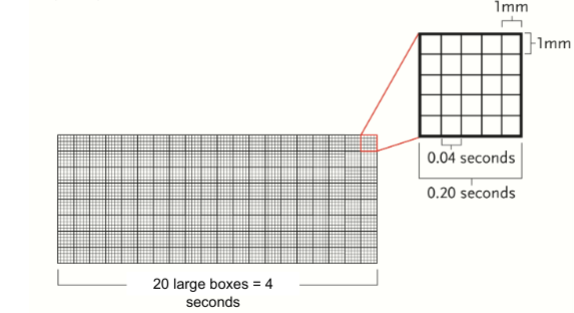
EKG Graph Paper
heart rhythm
the overall pattern of the heartbeat.
heart rate
the speed at which the heart is beating.
These six steps are required to analyze an EKG tracing
Determine heart rate (in BPM)
Examine the rhythm for regularity (clear pattern or lack of pattern)
Note presence or absence of P wave before each QRS, and note qualities of P wave
Measure length of PR interval
Measure length of QRS interval
Identify (name) the rhythm
six-second method
method used to determine heart rate from an EKG tracing that involves identifying a six-second section of the EKG and counting the number of QRS complexes in that section, then multiplying by 10.
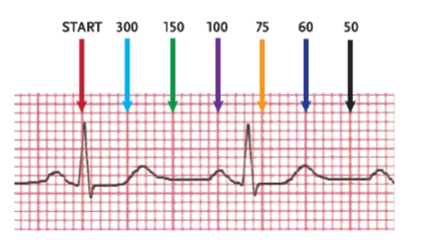
large block method
method used to determine heart rate from an EKG tracing that involves counting the numbers of large blocks between two consecutive R waves and dividing that number into 300, which is the number of large blocks in a one-minute EKG strip; also called the 300 method
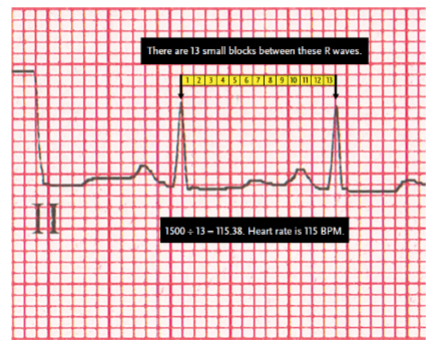
small block method
method used to determine heart rate from an EKG tracing that involves counting the small blocks between two consecutive R waves and dividing that number into 1500, which is the number of small blocks representing the passage of one minute; also called the 1500 method.
Remember these points about the six-second method
Involves counting the number of complete QRS complexes in a six-second section of EKG tracing and multiplying that number by 10 to determine rate
It is the least precise method of determining heart rate
It is the only method that can be used with irregular rhythms
Remember these points about the large block method:
Involves counting the large blocks between two consecutive R waves, then referring to a chart for the corresponding heart rate
Can also be used without the chart, by dividing the number of large blocks between R waves into 300
Sometimes called the 300 method
Remember these points about the small block method:
• Involves counting the small blocks between two consecutive R waves and dividing 1500 by that number
• 1500 is used because there are 1500 small blocks in a one-minute EKG strip
regular rhythm
general category of heart rhythm in which QRS complexes occur in a pattern that looks the same each time and repeats with consistent timing (for example, every 0.8 seconds).
irregular rhythm
general category of heart rhythm in which QRS complexes may look alike or different from each other, and do not repeat with consistent timing
regularly irregular rhythm
general category of heart rhythm in which QRS complexes may or may not look alike but are irregular in a clear, repeating pattern
calipers
a tool with adjustable points, used to measure intervals on EKG tracings.
Remember these points about measuring the PR interval:
It is measured from the beginning of the P wave (where it leaves the isoelectric line) to the beginning of the QRS complex
It can be measured using calipers or a scrap of paper and a pen or pencil
Normal range for the PR interval is 0.12-0.20 seconds
Remember these points about measuring the QRS complex:
Measurement is taken from the point where the first wave of the complex leaves the isoelectric line to the point where the last wave begins to flatten out
Not all QRS complexes show all of these waves, so it can take practice to perfect finding these measurements
Calipers or paper may be used, as with the PR interval measurements
Normal range for the QRS duration is less than 0.12 seconds
Values between 0.10 and 0.12 may be considered slightly prolonged, but not abnormal
escape beat
a heartbeat created when a part of the heart’s electrical conduction system other than the SA node initiates the electrical impulse that causes the heart to beat
escape rhythm
a rhythm in which a part of the heart’s electrical conduction system other than the SA node initiates all electrical impulses that cause the heart to beat (i.e., acts as the heart’s primary pacemaker)
ectopic focus
a situation in which an irritable area in the cardiac conduction system begins to generate an impulse even though the SA node may be working normally
dysrhythmia
difficult or abnormal heart rhythm; includes rhythms that are too fast, too slow, or originate in an area of the heart other than the SA node; sometimes commonly called arrhythmia
sinus rhythm
a cardiac rhythm originating in the sinus (SA) node.
atrial rhythm
a cardiac rhythm originating in the atria instead of the SA node.
junctional rhythm
a cardiac rhythm originating in the cells near the bundle of His or in the area of the AV junction rather than in the SA node.
ventricular rhythm
a cardiac rhythm originating in the ventricles rather than in the SA node; marked on an EKG tracing by a widened QRS complex
heart block
a type of cardiac rhythm caused when the AV node or AV bundle delays the electrical impulse from the SA node too long; also called AV block.
underlying rhythm
the basic rhythm of a patient’s heart, separate from any abnormal beats or complexes
Organization of the Cardiac Conduction System

These are ways in which abnormal beats or rhythms may occur:
If the SA node fails to generate an impulse and another area generates it, this creates a late beat called an escape beat
When this happens regularly it is called an escape rhythm
Irritable sites in the heart may generate electrical impulses, even when the SA node is working normally
This is known as an ectopic focus (ectopic pacemaker)
Remember these points about dysrhythmias:
A rhythm might be too fast, too slow, or originate in a part of the heart other than the SA node
Five areas in the heart can generate a rhythm and a rhythm is named for the area where it originates
Sinus rhythms begin in the sinoatrial node
Atrial rhythms originate in the atria
Junctional rhythms originate in the AV junction
Ventricular rhythms originate in the ventricles
Heart blocks (AV blocks) are caused by problems in the conduction of electrical impulses between the atria and the ventricles
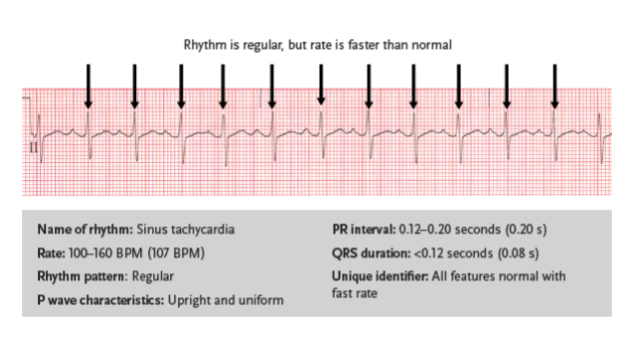
sinus tachycardia
a fast sinus rhythm with normal characteristics but with a rate of 100–160 BPM
Can be caused by medications, stress, or the body’s need for additional oxygen
Fever, exercise, fear, and low blood volume can also be causes
Can be especially dangerous for patients with a history of coronary artery disease
Treatment depends on the cause
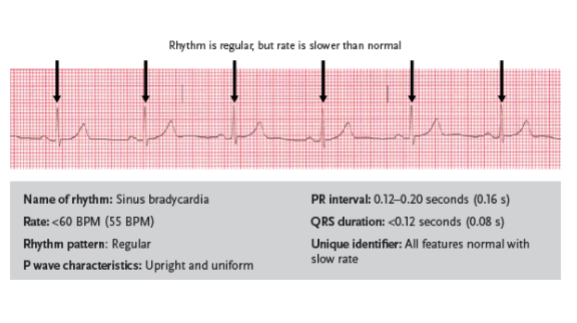
sinus bradycardia
a slow sinus rhythm with normal characteristics but with a rate below 60 BPM
Dizziness
Weakness
Syncope (fainting)
Changes in mental status/consciousness
Chest pain
Shortness of breath
Clammy skin
Low blood pressure
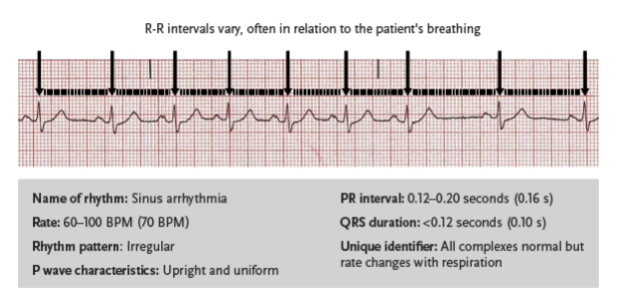
sinus arrhythmia
a sinus rhythm in which all characteristics are normal except for rhythm regularity; R-R intervals are irregular and usually vary with the patient’s breathing
Occurs naturally in some children and adults
Rarely requires treatment
If the heart rate slows so dramatically that it causes problems with circulation or cardiac output a medication may be prescribed
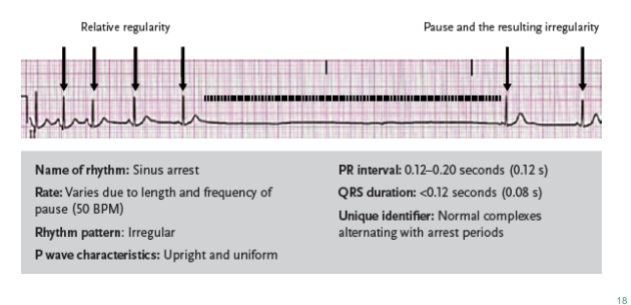
sinus arrest
a sinus rhythm resulting when the SA node does not initiate an impulse, causing pauses in the heart’s electrical activity; similar to sinoatrial block but with a greater time between complexes. Also called sinus pause
Can be caused by SA node damage, medications, or increased vagal tone
The vagus nerve, which is part of the parasympathetic nervous system, controls vagal tone.
When the vagus nerve is stimulated the heart rate may slow.
Patients who are asymptomatic may not require treatment.
Medication may be prescribed for symptomatic patients
symptomatic
experiencing symptoms
asymptomatic
not experiencing symptoms
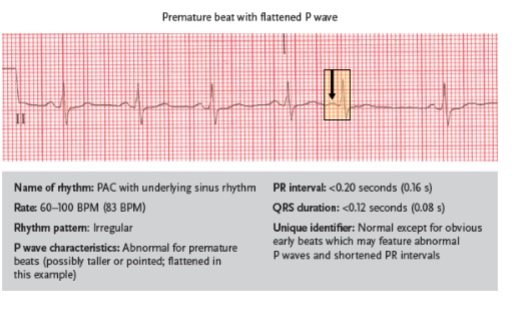
premature atrial complex
an atrial rhythm featuring obvious premature beats; other aspects of the rhythm are often normal
wandering atrial pacemaker
an atrial rhythm that occurs when impulses arise from multiple areas, including the atria, the AV node, and the SA node; also called multiformed atrial rhythm

atrial tachycardia
a fast atrial rhythm caused by irritability in the atria, with a rate of 160–250 BPM

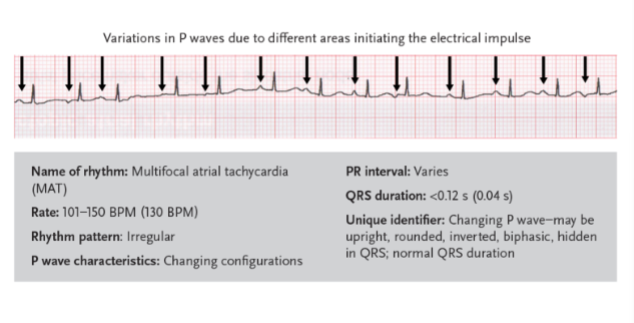
multifocal atrial tachycardia
a rhythm related to wandering atrial pacemaker, but with a ventricular rate greater than 100 BPM
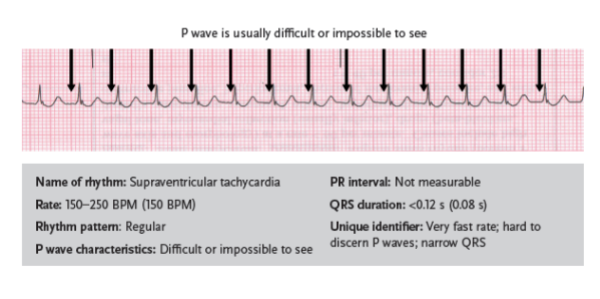
supraventricular tachycardia
can be a general term for all tachycardias (fast rhythms) that begin with impulses generated above the ventricles, or for a specific dysrhythmia marked by a very fast rate, P waves that are difficult or impossible to distinguish, and narrow QRS complexes; also called narrow complex tachycardia
atrial fibrillation
a common dysrhythmia that occurs when multiple irritable sites fire in the atria; considered controlled if the ventricular rate is under 100 BPM and uncontrolled if the ventricular rate is above 100 BPM
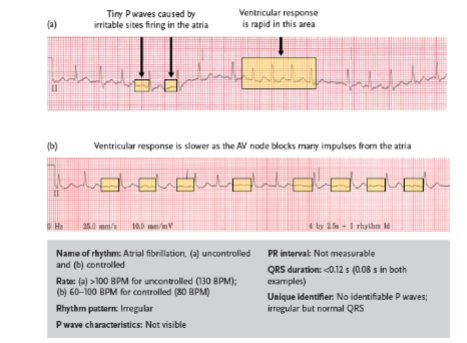
rapid ventricular response
contractions of the ventricles in an atrial fibrillation rhythm at a rate of 100 BPM or greater
atrial flutter
an atrial rhythm that occurs when an irritable site in the atria fires at a very rapid rate
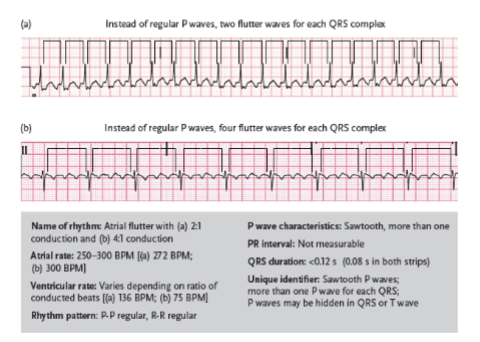
F-waves
short for flutter waves; waves displayed on the EKG tracing of a patient with atrial flutter representing the distortion of the P wave as the AV node blocks impulses that exceed 180 per minute; also called sawtooth or picket fence waves
atrial rate
the rate at which the atria contract (in normal rhythms, it is the same as the ventricular rate).
ventricular rate
the rate at which the ventricles are contracting; in normal rhythm it is the same as the atrial rate.
vagal maneuvers
actions taken to stimulate the vagal nerve and slow the heart rate; may be recommended by a doctor to stop certain dysrhythmias
transient rhythm
a rhythm that comes and goes
sustained rhythm
a rhythm that is always present
retrograde
moving backward; in cardiology, an impulse that travels backward compared to the usual cardiac conduction path
premature junctional complex
a cardiac rhythm in which an early impulse is generated by an irritable area of the AV junction; characterized by an abnormal P wave
junctional escape beats
a cardiac rhythm in which the AV junction area generates an impulse because the SA node is either slow to generate an impulse or does not generate one at all; as in premature junctional complexes, the P wave is abnormal, but these beats are late while PJCs are early.