OB Anesthesia
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
116 Terms
what forms placenta
HCG
alterations in every maternal organ system during pregnancy from what hormones 3
RT increases in hormones
HCG
Estrogen
Progesterone
§Also due to enlarged uterus & compression of surrounding structures
when do estrogen and progesterone peak
3rd trimester
purpose of estrogen & progesterone 4
support fetal development,
enlarge the uterus,
prepare breasts for lactation, and maintain the pregnancy, with estrogen stimulating tissue growth and progesterone preventing uterine contractions and supporting the lining,
sharp drop after birth triggers labor and postpartum changes.
what initially produces estrogen/progesterone hormones
corpus luteum but placenta takes over until delivery
enlarged uterus
crowds abdominal organs, causing frequent urination, constipation, heartburn, swelling (edema), and shortness of breath, while also compressing veins, leading to leg swelling and pressure
CV Changes in pregnancy
§Increased metabolic demands
§Hormonal changes (driven by estrogen, progesterone, and realxin and others) which causing vasodilation (widening blood vessels) to increase blood flow, boosting cardiac output (heart pumps more blood), increasing blood volume, and raising heart rate, all to support the fetus but also leading to lower blood pressure initially and a pro-clotting state
§Anatomic changes
§Increasing oxygen consumption increases during pregnancy, the maternal cardiovascular system adapts to meet the increasing metabolic demands of the fetus
EXAM when do CV changes begin
4 weeks, continue into postpartum
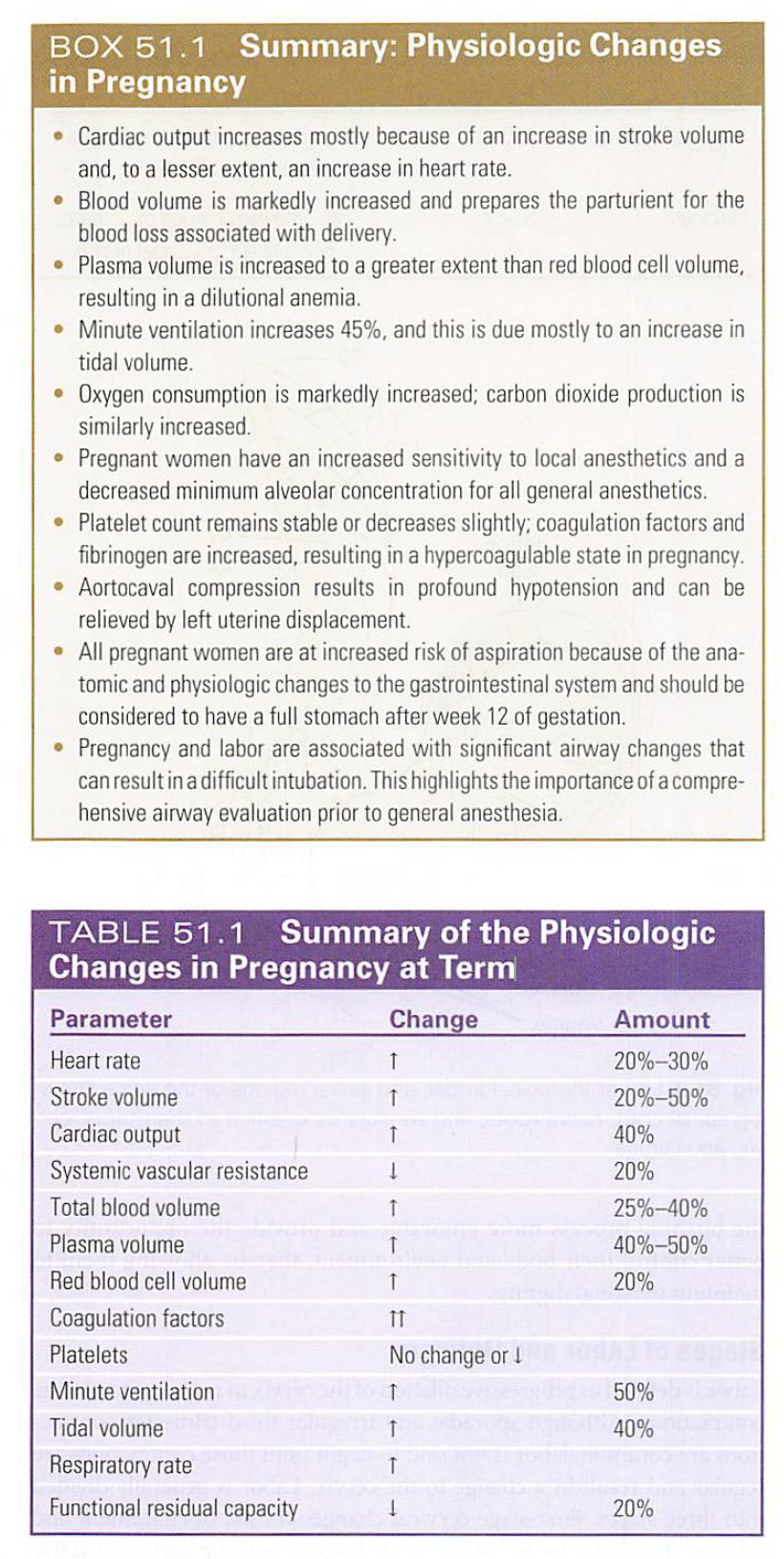
EXAM By what percentage does maternal heart rate increase by term?
20-30%
EXAM When does HR in pregnancy peak?
32 weeks , tachyarrhythmias in late pregnancy are common
EXAM How much does CO increase in pregnancy and what is this related to?
40% starting in week 5, r/t mostly increase in SV (lesser extent HR)
CO contiues to increase throughout pregnancy
EXAM At term, what percent of CO goes to the uterus?
10%
What happens to cardiac output during contractions?
increases as blood is autotransfused back into general circulation, about 500ml with each contraction
Post delivery how much does cardiac output increase above baseline?
80%,
related to autotransfusion and relief of aortocaval compression
When is the cardiac patient at greatest risk during pregnancy?
starting at 24 hours after delivery and continuing for about 2 weeks when HR and SV return to normal
Murmurs in pregnancy
can see a split S1 and S3 or a benign grade 1 or 2 murmur occur RT inc EDV
BUT if end diastolic murmur > 3 or with CP or syncope needs to be managed
how much does total bloood volume increase by
25-40%
how much does plasma volume increase
40-50%
dilutional anemia occrus from
plasma volume increases (40-50%) while RBC mass only increases (20%)
wht causes increase RBC vollume
eleveated erythropotien seen in 8th week geustationI
normal H&H
normal hemoglobin 11.6 and hematocrit 35%
What causes an increase in plasma volume in preganancy?
enhanced RAAS acitivtiy
EXAM Average blood loss in vaginal versus c/s delivery
vaginal 500ml, c/s 800-1000ml
baroreflex mediated changes in HR
Pregnant women have greater baroreflex-mediatedchanges in HR at term than at 6 to 8 weeks postpartum.'^ In the presence of adequate neuraxial analgesia, there is often a corresponding decrease in maternal HR during uterine contractions due to the transiently increased preload.
SVR changes in pregnancy
decreased by 20% due to decreased resistance in the uteroplacental, pulmonary, and renal vascular beds
at term, 10% of CO perfuses low resistant intervillous spaces of uterus
dec SVR—> dec DBP up to 15 mmhg—> dec. MAP
renin in pregnancy
•Pregnancy more dependent on the renin-angiotensin-aldosterone system for BP maintenance
•Plasma renin and angiotensin II increases during pregnancy, even though blood volume increases
•Renin is 12x greater in 3rd trimester, than non pregnant woman
•Angiotensin II is increased in the 3rd trimester to help maintain MAP
whh RAAS important in pregnancy
support the increased demands for fluid and salt essentially.
It is crucial for expanding maternal blood volume and maintaining blood pressure, placental health, and fetal development, but this system must be finely balanced, as dysregulation is a key factor in serious conditions like preeclampsia.
raas
Estrogen's Role: Placental estrogen increases liver production of angiotensinogen, a precursor for Ang II, stimulating the whole cascade.
Increased Renin: Renin levels rise significantly, driving the production of Ang II.
Aldosterone Release: Ang II stimulates the adrenal glands to release aldosterone, enhancing sodium reabsorption and water retention
What happens to NE sensitivity in preganancy?
unchanged
Phys changes in pregnancy
How does supine hypotensin syndrome (SHS) occur
when the gravid uterus compresses the vena cava in later pregnancy which redues preload to heart and therefore decreases SV and BP
can be instant or develop over time
what could compression be RT
§increased with a large uterus (polyhydramnios or multiple fetuses)
§gravid uterus may also compress the aorta, results in upper body BP to be normal but distal to the compression, (L3-L4) BP is decreased
normal physiologic response to SHS
tachycardia and vasoconstriction in the lower extremities to attempt to compensate
what happens when uterus compresses abdominal aorta
uterine blood flow decreased and the fetal perfusion & oxygenation decreases= BAD
EXAM How does one treat aortocaval compression?
left uterine displacement 15-30 degrees to get compression off the abdominal vasculature
** the autonomic sympathectomy from the spinal or epidural and the normal compensatory of lower body vasoconstriction is diminished
EXAM Leading causes of maternal death
Thromboembolic events
Coagulopathy in pregnancy
-hypercoagulable state, risk for DVT
-increase in factors 7,8,9,10 & 12
unchanged 2 & 5
-fibrinogen (factor I) double in late pregnancy (400-600)
-platelets stable 150-400K
factor 11 (XI) & 13 (XIII)= decrease
Pt/PTT shortened 20%
VIRCHOW TRIAD
venous stasis, hypercoagulability, endothelial injury
Why high risk for venous thromboembolism (VTE),
the growing uterus causes venous stasis (slowing blood flow),
pregnancy hormones create a hypercoagulable state (increased clotting factors),
delivery (especially C-section) causes endothelial damage (vascular injury).
prehgnant women are alway minimum ASA
2
WBC
increases
in 3rd trimester ranges from 10.5 – 30k/mm³
capillary enrogement in upper airway lead to
Capillary engorgement in the upper airway results in a narrowed glottic opening and edema in the nasal and oral pharynx, larynx, and trachea.
Mallampati score changing as labor progresses.^^
O2 consumption at term
inc from 33% at rest to 1o0% in 2nd stage of labor
Minute ventilation in pregnancy
MV, TV, and RR increased
MV increases 50% at term, TV ↑40% & RR ↑ 10%
why is MV increased
progesterone causes higher oxygen intake and lower CO2 levels (respiratory alkalosis); compensatory decrease in bicarb
reason Breathing pattern is more diaphragmatic
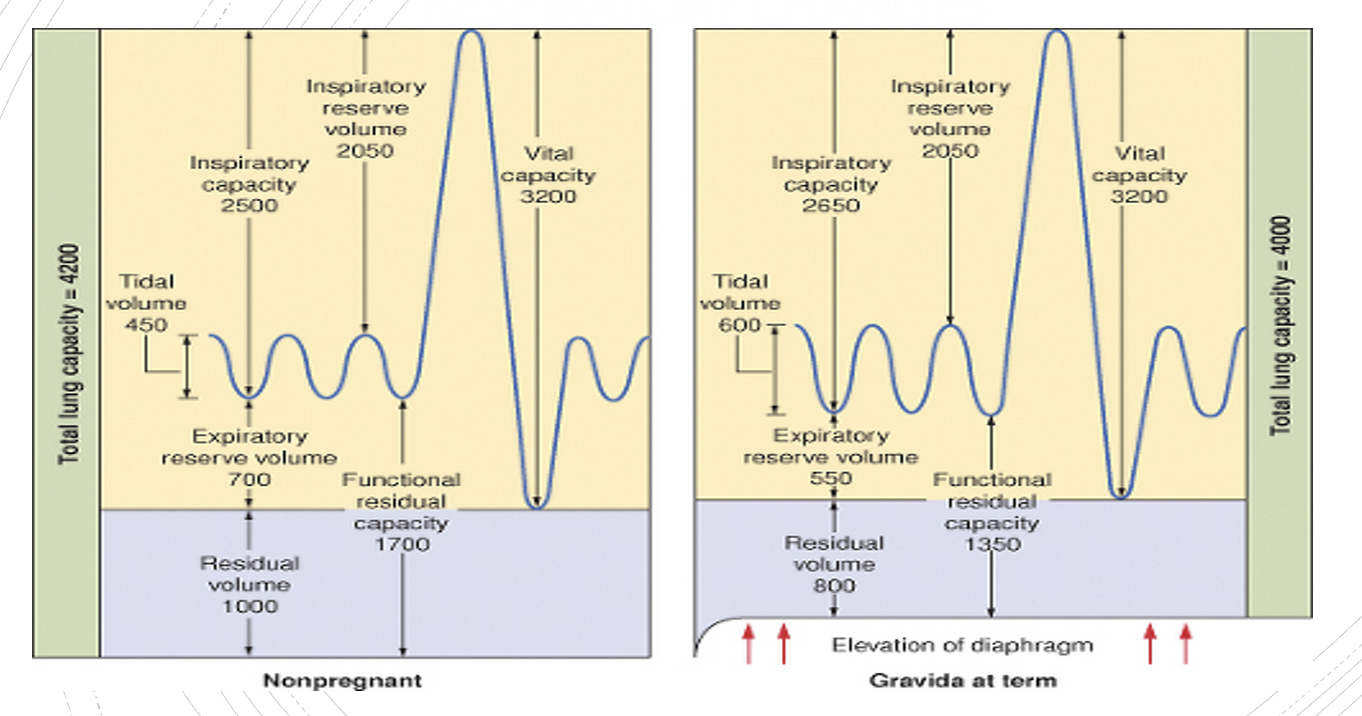
diagraphm is dispalced cephalad about 4 cm by expanding uterus
but the chest expands to maintain lung capacity, causing SOB as a normal feeling, alongside nasal congestion and increased risk of sleep apnea, all normal adaptations to support the mother and fetus
Will PaO2 & PACO2 be higher in nonpregnant or pregnant
PaO2= pregnant
PaCO2= nonpregnant
what is closing capacity
volume in lungs when airway closure begins at the respiratory bronchioles
§The alveoli lack supporting cartilage and depend on other factors to keep them open
Closing capacity in pregnancy volume in lungs when airway closure begins at the respiratory bronchioles
CC= CV & RV.
unchanged
FRC ERV and RV
decreases FRC (20%),
ERV and RV due to upward/outward pressure on the diaphragm (like a restrictive lung disease)
MV increase during labor
300% which can cause maternal Paco2 to drop <15
alkalemia causines hypoventilation resulting in hypoxemia
Effects of hyperventilation during labor
no effect if PaCO2 >20
can be determiental
decreased uterine blood flow r/t a reduction in fetal oxygen tension (PO2)
Normal fetal and maternal PO2
fetus 32-35
maternal 90-100
Airway changes in pregnancy: anesthetic significance
-glottic narrowing
-increased edema RT capillary engorgement
-increased friability→ bleeding→ difficult intubation
-mallamapati scpres change
avoid nasal intuabtions
use smalller ETT
use short-handed laryngoscope
Long handle may need require to push down chest RT excess tissue to fit handle
response to anesthetics
MAC decreased (15-40%)
decreased FRC l/t faster induction with insolluble agents
rapid OD with loss of airway reflexes
Greater risk of hypoxemai
Dec. FRC mean less O2 resere
increaed O2 consumptipon
rapid airway obstruction
nervous system changes in first trimeseter
increases sensitivity to LA and GA→ use less drug
Increased sensitivity is due to several physiological and hormonal changes, which also means that pregnant women are more susceptible to side effects like hypotension and potential toxicity.
Changes in the size of the epidural and subarachnoid space
epidural veins become engorged RT increase intrabd pressure which causes a decrease in both epidural and SA space (pushes dura anteriorly)
Physiologic & anatomic changes GI
§place the parturient at ↑ for aspiration and regurgitation
affect of increase in gastrin levels
increased gastric volumes and lower pH
EXAM gastric ph & gastric volumes
ph <2.5 & volume >25mls
consider full stomach
Increase in the upward & outward displacement of the stomach by the gravid uterus
may result in a mechanical obstruction to outward flow through the pylorus, which leads to delayed gastric emptying and increased intragastric pressure
Progesterone effect on GI tract
relaxes smooth muscle therefore the esophageal sphincter, may cause heartburn
PHYSICAL GI Changes
growing uterus compressing organs, leading to increased N/V, GERD, constipation, and hemorrhoids,
also appetite changes and cravings, while the liver works harder and gallstones risk increases due to cholesterol changes
When do gi changes normalize
§GI changes take several weeks post-partum to normalize
C/S NPO status
clears up to 2 hours before procedure sinc eonset of labor further reduces rate of gastric empyting
how to increase ph
Use H2 blocker that alters release of H+ by gastric parietal cells to increase gastric ph
Ex. cimetidine (Tagamet)ranitidine (Zantac)famotidine (Pepcid)
Metoclopramide (Reglan)
increase gastric emptying, reduce N/V, and icnrease lower esophageal sphincter tone to prevent reflux.
why cosndier zofran before admin of psinal anesthesia for C/S
hypotensive ppx
if GA is used in pregnant women, what anesthesia technique should you use
RSI
Cric pressure with cuffed ETT from 20 week to PP
Bicitra
neutralize gastric acid in the stomach- used as aspiration prophylaxis before regional anesthesia for elective C-Section
factors decrease uterine BF
decreases uterine arterial pressure
Supine position
hemorrhage/hypovolemia
hypotension
Increase uterine venous pressure
venal caval contraction
uterine contractions
drug induced uterine hypertonus (oxytocin, LA)
skeletal muscle hypertonus (seizures, valsalva)
factors increase uterine vascular resistance
endogenous vasoconstrictor
catecholamines (stress)
vasopressin (in response to hypovolemia)
exogenous vasoconstrictors
epi
vasopressors (neo> ephedrine)
LA in high concentrations
hepatic changes- what levels increrase
aspartate aminotransferase,
alanine aminotransferase,
lactate dehydrogenase, and
alkaline phosphatase
increase to the upper limits of nonpregnant normal levels.
Serum cholinesterase levels in pregnancy
decreases 30% during pregnancy and even more after delivery,
if low, certain meds will take longer to work (Ex. Sux)
§Will remain low at term & decreases again within a few days after delivery
§Returns to normal over the next few weeks
still safe to give succ and remifentanil in normal levels
Serum albumin in preganancy
decreased,
—> increased free fraction of highly protein-bound drugs
drugs will last longer if reliant on cholinesterase for elimination (ester LA, succs, and remifentanil)
hepatic changes
Blood Flow & Size: Liver mass increases (hepatomegaly), portal blood flow rises, but arterial flow stays stable, supporting metabolic demands.
Hormonal Influence: High estrogen and progesterone impact metabolism, synthesis, and excretion.
Metabolic Shifts: Increased lipid production (cholesterol, triglycerides) provides energy, while liver enzyme activity (like Cytochrome P450) changes, altering drug metabolism.
Biliary System: Reduced gallbladder contractility and increased cholesterol secretion make gallstones more common
Renal changes in pregnancy
-increase CO— increased RBF (80%)
-increased GFR (50%) & ncreases renal absorption —> can cause increase glucose excretion
urinary protein excretion elevated
-increased creatinine clearance (to 140-160)
BUN and creatinine levels in pregnancy
-decreased BUN r/t increased volume, 8 mg/dl
-decreased creatinine to 0.5 mg/dl
Kidney enlargement leads to decrease crt and BUN and common mild proteinuria/glucosuria.
C/W uterus in renal system
may cause compression/ obstruction of utereter
hromonal changes (progesterone & relaxin) renal system
increased blood volume cause systemic vasodilation, reduced blood pressure, and altered electrolyte handling (lowered sodium), while the enlarging uterus physically dilates the ureters, potentially causing hydronephrosis, all to support maternal and fetal needs
Musculoskeletal changes in pregnancy 4
-lumbar lordosis increased (RT change in center of gravity dt fetus weight)
-narrowing interspinous spaces (diff central regional block)
-shoulders slump and rotate back
-increased relaxin leading to increased joint mobility
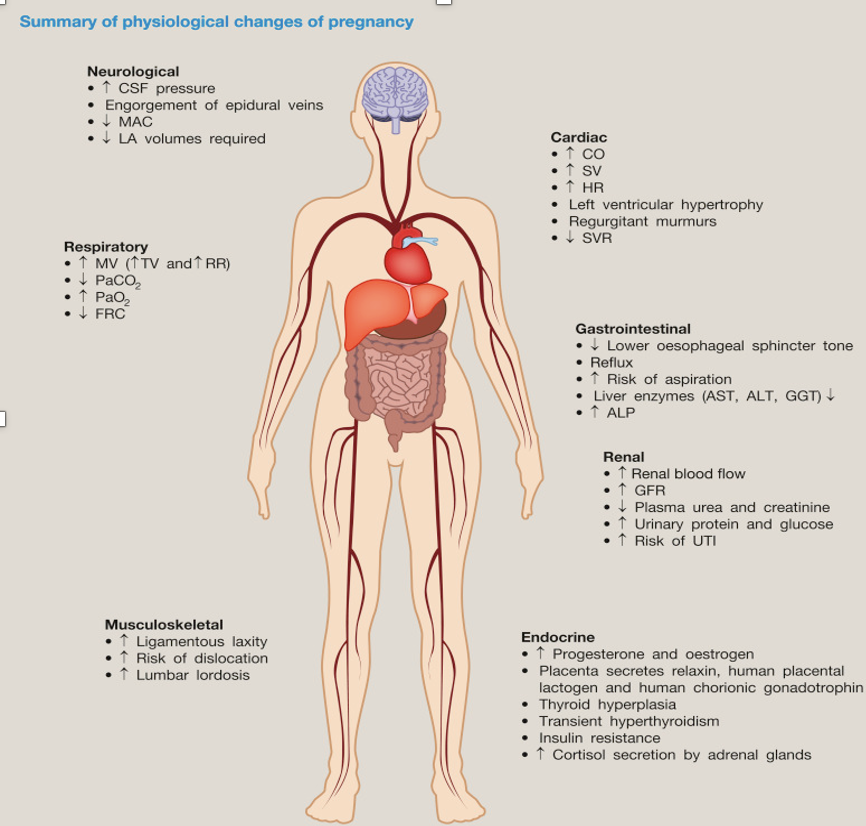
Know Box 51.1 & Table 51.1-page 1179 N7*
WBC in pregnancy
increased
uterine changes & blood flow
§The uterus enlarges, blood flow increases
Uterine blood flow at term increases to max of 800ml/min (10% of maternal CO)
Of this, 150 ml/min supplies nutrients to the myometrium & 100 ml/min to the decidua (lining of the uterus) and the rest in the intervillous space.
§ It is supplied by 2 dilated maternal uterine arteries (1 vein): these arteries are maximally dilated so no effects of autoregulation.
Placental arteries
-2 umbilical arteries carrying deoxygenated blood from fetus to uterus
Arteries involved in placental blood flow
arcuate, radial, and spiral
Spiral arteries expel blood into the intervillous space
Venous drainage of placenta
maternal venous sinuses collect blood from the intervillous space and return it to general circulation
How many umbilical veins is there?
1, carries oxygenated blood
deoxy blood flows from fetus to uterus
via 2 umbilical arteries which perfuse capillary networks within placental villi that protrude into the pool of maternal blood
what are placental vili
§small finger-like projections which maximizes the surface area of the placenta that contacts maternal blood.
§Each villus contains a capillary network that exchanges respiratory gases, nutrients and wastes with maternal blood.
what cross placental tissuse
O2 & CO2- but are perfusion limited based on the perfusion of the placenta, not the rate of diffusion of the gases themselves
Uterine BF
§Autoregulation of intervillous blood flow does not seem to occur
§The uteroplacental blood flow is solely dependent on maternal BP
§The spiral arteries do constrict in response to α-agonists (phenylephrine)
Fetuses do not tolerate:
maternal arrhythmias
maternal hypoxia
sustained decreases in placental blood flow
certain drugs
asphyxia
key changes in preg
Volume Increase:
Uterine blood flow (UBF) increases significantly, reaching up to 10% of the maternal cardiac output.
Vessel Dilation:
Uterine arteries dilate substantially, increasing in diameter and reducing vascular resistance to accommodate the higher flow.
Autoregulation:
Uterine vessels remain largely dilated and are not well-regulated by autoregulation, making them responsive to maternal blood pressure and volume.
Blood Flow Distribution:
Placenta: The intervillous spaces of the placenta receive the majority ~80%) of the blood flow.
Myometrium: The uterine muscle (myometrium) receives the remaining 20%.
Factors Affecting Uterine Blood Flow:
Maternal Cardiac Output:
UBF is heavily dependent on maternal heart function and blood volume, which nearly doubles during pregnancy.
Maternal Hypotension:
Any cause of maternal low blood pressure (like shock or anesthesia) can significantly decrease UBF.
Aortocaval Compression:
Lying on the back (supine position) can compress the vena cava, reducing venous return and UBF
Uterine Contractions:
Contractions temporarily decrease flow, and hyperstimulation (e.g., from oxytocin) can severely restrict it.
Clinical Significance:
Because of this high flow and reduced vascular resistance, the pregnant uterus is vulnerable to conditions that compromise blood supply, highlighting the importance of maintaining maternal circulation.
EXAM Determinants of placental transfer of free (non-protein-bound) drugs
concentration gradient,
molecular weight,
lipid solubility, and
degree of ionization
EXAM Size and permeability
->1000 daltons does not cross easily
-<500 daltons crosses easily
EXAM transfer of drugs from maternal circulation to fetus is determined
primarily by diffusion
EXAM Factors that favor diffusion across placenta
low molecular weight,
high lipid solubility,
low degree of ionization,
low protein binding
what helps drugs pass membranae
Cell membranes consist primarily of lipids, so the drug’s degree of lipid solubility helps it to pass through the cell membrane
highly lipid-soluble drugs such as fentanyl cross easily
ionized drugs are
§polar & water soluble, which limits the drug's ability to diffuse through lipophilic cell membranes
LA are variably ionized basic compounds à the degree of ionization depends on pHà the more alkaline the pH, the greater degree of non-ionization
what protion cross placenta
non ionized
NDMR
§large, ionized drugs that are not affected by pH
§NDMR have a quaternary group in their structure and are not able to cross the placenta