Cardiorespiratory Physiotherapy
1/230
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
231 Terms
6 core cardiorespiratory problems
Respiratory failure (Type 1 and 2)
Sputum retention
Loss of volume
Increased work of breathing
Pain
Reduced exercise tolerance
What are the 5 Carinal Signs of Respiratory Disease?
Dyspnea
Cough
Sputum
Wheeze
Chest Pain
Cardinal Sign - Dyspnea
+ and the 4 classes
increase work of breathing/shortness of breath
can be related to: Orthopnea (lying down), Paroxysmal nocturnal dyspnoea (SOH when asleep)
Important to gain info on: Duration, severity, pattern and associated factors
Classified into 4 classes
Class 1: no physical activity limitation
Class 2: slight physical activity limitation
Class 3: marked physical activity limitation
Class 4: unable to perform physical activity
Cardinal Sign - Cough
Protective reflex
Caused by: inflammation, irritation, habit, excess secretions
Check: frequency (day/night), effectiveness (weak/strong/pain), Quality (wet/dry/raspy)
Complications: fractured ribs, hernias, incontinence, embarrassing
Cardinal Sign - Sputum
excess tracheobronchial secretions, combination of saliva and mucus result of infection/disease
cleared by huffing/coughing, improving gas exchange & expiratory flow
may contain: mucus, cellular debris, microorganisms, blood (hemoptysis), foreign particles
Checklist: quantity (small/5c coin/cup), quality (consistency/colour/odour)
The ABCDE Approach
Airway- Blocked? Upper airway collapse? Aspiration? Tracheostomy? Ventilated? Do they require O2?
Breathing - Work of breathing? Pattern? Distress? Auscultation? Fatigue/weakness? Accessory muscle use?
Circulation - Colouring? Temp? BP/HR? Blood results? Stability for intervention? Oedema?
Disability - Previous medical history? Limiting factors? Impact on my ability to treat? surgery? Pain?
Environment/Exposure - Wounds/scars? Temperature? Palpation? Medication? Antibiotics/steroids?
Observations of the Head and Neck
Facial expression
Colour/pallor
Use of accessory muscles
Sculpturing: how much of the muscles can you see
pursed lip breathing
How to Auscultate?
Breath sounds - Wheeze
vibration of the walls of a narrowed airway
pitch determined by diameter and elasticity of the airway
expiratory wheeze - bronchospasm
inspiration wheeze - airway obstructions, oedema, mucous
Breath sounds - Crackles
discontinuous, short, explosive sounds
fine or course sounds
What colours do Air, Fat, Soft tissues and Bone correlate to in an X-ray?
Air = Black
Fat = Dark grey
Soft tissue = grey
Bone = white
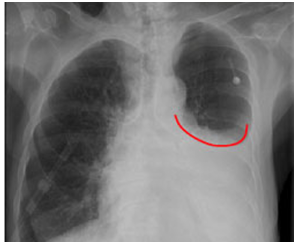
X-ray Exposure
Should be able to see T4 (not T5) vertebrae on PA
Over-exposed = appears black
Under-exposed = appears falsely white

X-ray Reading - Logical Progression - ABCDEFGHIM
Airways - Trachea should be central but deviates slightly to right
Bones - compare bone density
Cardiac silhouette - check heart is normal shape
Diaphragm - right is higher than left, should be smooth
Edges - should be well defined acute angles
Fields - should be equal, compare size
Gas - abdominal gas bubbles
Hilum - left higher than right, compare shape and density
Instrumentation - ETT, tracheostomy tube, catheter, nasogastric tubes, pacemaker
Mediastinum - border should be fuzzy and trachea visible
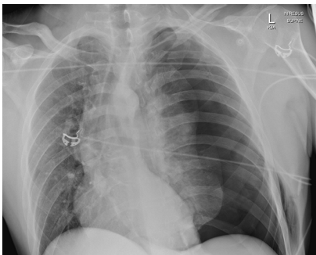
Pathology - Consolidation
Air filled paces replaced with fluid, blood or sputum
E.g. Pneumonia

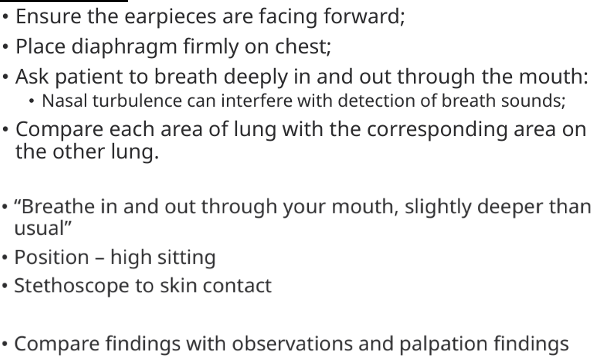
Pathology - Collapse
Elevation of hemidiaphragm
decrease in rib spacing
displacement of mediastinum, hilum, fissure - volume loss
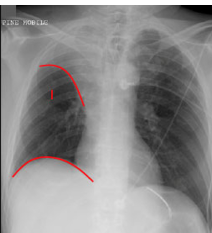
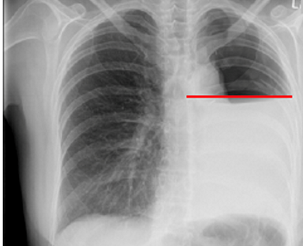
Pathology - Pleural Effusion
Accumulation of fluid in pleural cavity
collects in costophrenic angles
“Meniscus sign”
lateral lying x-ray
Pathology - Pneumothorax
lack of lung marking
deep sulcus sign
sharply outlined diaphragm
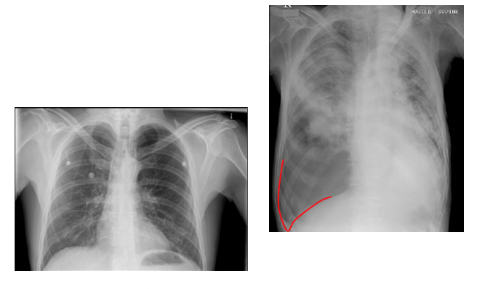
Pathology - Tension Pneumothorax
ipsilateral diaphragm depressed and flattened
mediastinum and heart pushed to other side
Pathology - Haemothorax
blood in lungs
air-fluid level
no meniscus sign → flax line
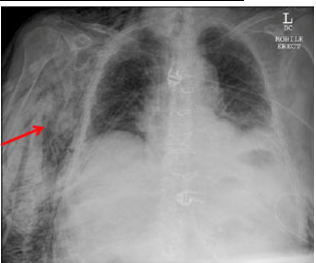
Pathology - Subcutaneous Emphysema
dark streaks in soft tissues
Air appears black (radiolucent) on X-ray
streaky, bubbly, or reticular (net-like) black areas in the soft tissue
Pathology - Bronchiectasis
Dilatation caused by congenital deficiency and weakening of the muscular and elastic layers in the bronchial walls
ring shadows
increased bronchiole diameter

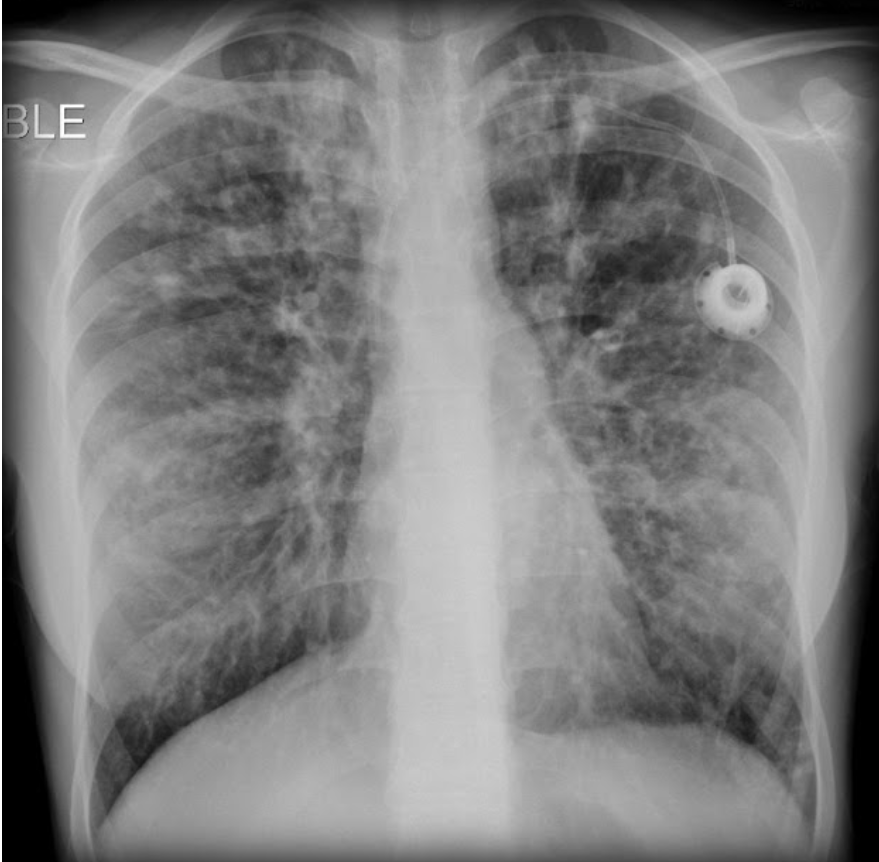
Pathology - Cystic Fibrosis
may show hyperinflation
dilated bronchi
over time, inflammation can cause scarring, leading to a mosaic pattern
Pathology - Pulmonary Oedema
“batwing” pattern
increased cardiac silhouette sign
pleural effusions present

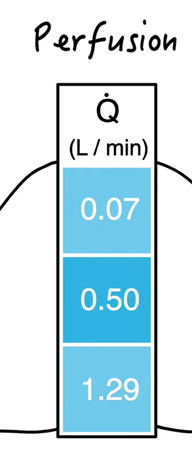
What is Perfusion?
Total volume of blood reaching the pulmonary capillaries
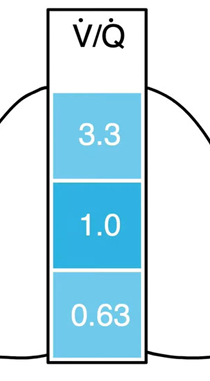
What is the ventilation-perfusion ratio when standing?
3.3 in the apex of the lung and 0.63 in the base
Ventilation exceeds perfusion in apex, and perfusion exceeds ventilation in base
The overall value in the average human lung is 0.8 V/Q
In regular upright ventilation, where does more ventilation go? And why?
into the lung base rather than the lung apex
more alveoli at the larger lung bases
basal alveoli are less stretched than the apical alveoli
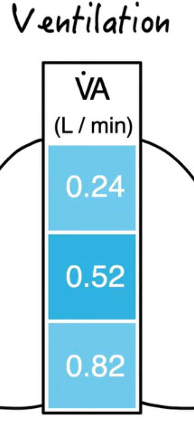
What is the “dependent region” in relation to distensibility?
dependent region: basal region of the lung in relation to gravity
basal alveoli are more compliant (distensibility), therefore is more ventilated at the basal alveoli
In regular upright ventilation, where does more perfusion go? And why?
into the lung base rather than the lung apex
more alveoli and pulmonary blood vessels at base
gravitational effects on pulmonary blood
Both ventilation and perfusion are greater at the lung bases in upright posture, but perfusion increases more steeply than ventilation
what happens if there is a mismatch between alveolar ventilation and blood flow?
it will be seen in the V/Q ratio
if the V/Q ratio reduces due to inadequate ventilation, gas exchange within the affected alveoli will be impaired.
^ capillary partial pressure (PO2) falls and PCO2 rises
What are some reduced ventilation problems?
affects oxygen levels as carbon dioxide is more soluble and continues to diffuse despite impairment
Type 1 Respiratory Impairment
(PaO2 less than 80mmHg) → Type 1 Respiratory Impairment
(PaO2 less than 60mmHg) → Type 2 Respiratory Failure
Pneumonia, Asthma, COPD, Hypoxia
What are some reduced perfusion problems?
pulmonary embolism → circulation is obstructed
other areas will receive increased blood supply
hypoxemia to the lung
What are some contraindications to a head down tilt position?
cardiac failure
Unstable HR
Hypertension
cerebral oedema (swelling of brain)
hemoptysis (coughing up blood)
obesity
pregnancy
surgery/head or neck trauma
What is SpO2?
peripheral oxygen saturations measured by pulse oximetry (finger/earlobe/forehead)
What is SaO2?
arterial oxygen saturations measured by ABG
How to document Oxygen Use? “7 steps”
Document starting device/flow;
Start O2 and ensure target is achieved quickly;
Titrate O2 to keep in SpO2 range
Monitor O2 minimum 4 hourly
Record SpO2 & delivery device
Wean off O2 if clinically stable
Codes to be written on obs. chart and initialled.
When are ABGs required with Oxygen therapy?
Critically ill patients with cardiorespiratory or metabolic dysfunction
In patients with a SpO2<92%
Deteriorating oxygen saturation requiring increased FiO2
Patients at risk of hypercapnia
Breathless patients in whom a reliable oximetry signal cannot be obtained
What is the normal peak inspiratory flow rate (PIFR)
ranges between 20-30 L.min-1
What is FiO2?
Minimum flow rate required to ensure a patient receives an exact concentration of oxygen
What are some Low Flow Oxygen Devices
Nasal cannula (long-term O2 therapy, hypoxic patients)
Hudson face mask (short-term use, following surgery)
Reservoir mark (emergencies, severe hypoxaemia)
What are some examples of High Flow Oxygen Devices?
High-flow nasal cannula therapy (HFNC) (100% O2 delivery, increased tidal volume, minimal air room entrainment)
Venturi Mask (increase flow of gas without increasing amount of O2)
Physiotherapy role in Oxygen delivery
Ensure correct mode of delivery
Assess the need for oxygen with exercise
Advise whether oxygen is sufficient
Can alter prescription in certain situations
Benefits of Humidification
Improves mucociliary function
Facilitates secretion removal
Reduce work of breathing
Improved patient comfort and compliance
Methods of Humidification
Systemic Hydration (drinking/IV water)
Bubble through (cold water)
Heated water bath (humidifier)
Pass over humidification
What is the ventilation-perfusion ratio?
ratio of alveolar ventilation (V̇A) to pulmonary blood flow (e.g. V/Q)
In the ventilation-perfusion relationship, where in the lung is there more perfusion and ventilation?
more perfusion at bases
more ventilation at the apical regions
Nasal cannula: What is the recommended dosage for oxygen?
No more than 4 L.min-1 O2
Hudson face mask: What is the recommended dosage for oxygen?
Minimum of 5 L.min-1 O2
Reservoir Mark: What is the recommended dosage for oxygen?
Minimum 12 L.min-1 O2
What are the 5 physiological mechanisms responsible for the efficacy of high-flow nasal cannula?
Increases function residual capacity (FRC)
Washout of waste gases including carbon dioxide (CO2)
Decreased respiratory rate
Provides Positive end-expiratory pressure (PEEP) ~2-4cmH2O
Increased tidal volume (VT)
Administration range for SpO2 in a patient with an acute condition:
Administration range for SpO2 in a patient with COPD:
acute condition: less than 92% and titrated to 92-96%
patient with COPD: less than 88% and titrated to 88-92%
What is a PF Ratio? (PaO₂ /FiO₂)
A measure of how well oxygen is being transferred from the lungs into the blood (assess severity of hypoxemia)
Determined by dividing Blood/Oxygen = (hopefully more than 400)
Normal: >400
What is a “A-A” gradient? + normal range
The difference in partial pressure of oxygen between arterial blood and alveolar gas
Normal: 5-10mmHg
Requirement for normal airway clearance - Mucociliary escalator
Whipping action of the cilium within the sol layer of the mucus produces a wave motion
Stroking action speed = 2cm per min
Requirement for normal airway clearance - effective cough and phases
A voluntary cough is generally characterised by an inspiration of approximately 80-90% total lung capacity
The contraction of abdominal muscles and expiratory muscles generates a sudden increase in intrathoracic pressure, before the glottis is rapidly opened, and a blast of turbulent air is expelled
3 phases → inspiration, compression, expulsion
Peak Cough Flow in Adults
Normal: 720 L.min-1
Minimum required for effective airway clearance: >160 L.min-1
Factors decreasing mucociliary clearance
medications
mucosa drying
High FiO2
Endotracheal tube
Pollutants
Decreased lung volumes
Dehydration
Reasons for an Ineffective Cough?
Decreased lung volume
pain, restriction, weakness
^ Solution: use breath-stacking to increase lung volume
Decreased expiratory force
poor elastic recoil, can’t close glottis
^ Solution: assist expiratory phase
7 Examples of Physiotherapy techniques to improve Airway Clearance Therapy (ACT)?
Gravity-assisted positioning (GAP)
Airway clearance devices
Manual techniques (chest wall vibrations, percussion)
Drainage
Nebulized inhalation therapy
Exercise
Assist cough
Indications and Considerations for Airway Clearance Therapy (ACT)
Indications
Diseases (COPD, CF etc), post-operation, collapsible airways, productive asthma
Considerations
consent, infection control, patient comfort
If a patient has bronchoconstriction (wheeze), consider Salbutamol or nebulized mucolytic
OSCE: Active Cycle of Breathing Technique (ACBT)
Components (varies with each patient)
Breathing Control (gentle breathing, lower chest) ~2mins
Thoracic expansion exercise (deep breathing, hands on ribs, with or without hold) (x3)
Forced expiratory technique HUFF (x2) (squeeze not wheeze, “Fogging up a mirror”)
What for?
secretion clearance, improving ventilation, no equipment required, moist environments (shower)
What is an Equal Pressure Point mechanism?
describes how, during forced expiration, the point where ‘airway pressure = pleural pressure’ determines where the airway is prone to collapse, limiting expiratory flow.
Ideal positioning for Airway Clearance Therapy (ACT)
Sitting position with arms supported that promotes an increase in FRC
(Sitting supported)
OSCE: Positive Expiratory Pressure Devices - PEP mask
prevents small airway collapse
The patient performs controlled expiration against the resistance, to maintain respiratory pressures between 10-20cmH20
Consider size and patients expiratory flow
10-12 cycles of 8-10 exhalations= until secretions are cleared

OSCE: 3 Types of Oscillating Devices with PEP
Acapella
creates oscillation effect on airways with PEP
Flutter
creates oscillation effect on airways, with a steel ball interrupting the flow of air
Position dependent
Aerobika
dial up resistance, independent of gravity
All treatments consist of 10-12 cycle of 10-12 exhalations
3 Stages of Autogenic Drainage
Stage 1: low volume breaths to mobilize secretions
Stage 2: medium (tidal) beaths to collect mucus
Stage 3: Large volume breaths to enable expectoration
OSCE: Manual Technique - Chest wall Vibrations (CWV)
increases peak expiratory flow
helps to shift secretions from lung peripheries
never perform on a breathless patient
creates airway oscillation
Manual Technique - Exercise
performed before ACTs to loosen secretions
increased BMI and posture, well-being, cardiovascular fitness etc
What is Atelectasis?
The collapse of a part/all of an alveolus, leading to reduced gas exchange and respiratory problems (Loss of volume).
Usually from surgery, smoking, obesity, age, impaired cognition etc
Type: Obstructive (bronchial obstruction)
Type: Non-Obstructive (surgery, wound etc)
6 Signs and Symptoms of a Post-Op chest Infection
SpO2 less than 90% on 2 consecutive days
Chest x-ray findings
Temp over 38deg 1-day post-op
Productive Sputum
Abnormal lung auscultation
Raised white cell count
4 Clinical Signs of Atelectasis?
Reduced PaO2
Reduced lung compliance
Reduced FRC
Non-productive cough
What is Collateral Ventilation?
Thoracic expansion exercises
Increase collateral ventilation
Increase lung volume
Mobilise secretions as air can get behind the sputum.
Importance of Mobilization
uptake of O2
reduction in FiO2
increase in cardiac output and oxygen extraction in tissues
exercise increases SV and HR therefore increases CO
What is Alveolar Interdependence?
When an alveolus begins to collapse, the surrounding alveoli pull open the collapsing one (using expanding forces and neighboring tension)
protective mechanism against atelectasis
Expanding forces exerted between adjacent alveoli & higher lung volume > expanding forces
OSCE: Positive Expiratory Pressure - Pari PEP
splinting open airways prone to dynamic compression during forced expiration
Can be used in conjunction with a Nebulizer
not position dependent
Maintain 10-20cmH2O
Backwards pressure to hold airways open
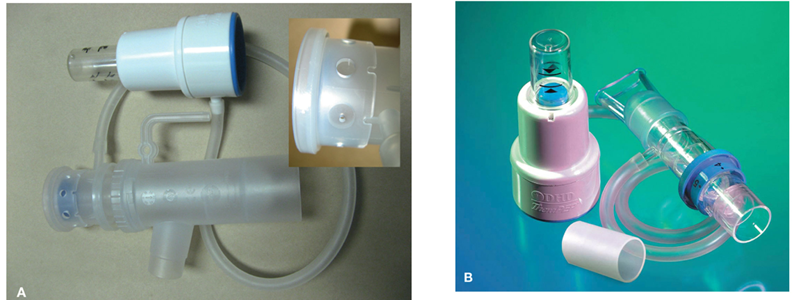
OSCE: Nebulized Inhaled Therapy
Inhalation of saline solution through Pari PEP to increase water to lungs to thin out sputum for it to be coughed up easier
Breathe in and out normally
OSCE: Incentive Spirometry
provide visual feedback via a ball/chip rising to the preset marker via inspiration
track lung volumes

Movement of the Ribs
Ribs 1-6: _______
Ribs 7-10: _______
Ribs 10-12: ________
Ribs 1-6: “Pump handle” - up and down movement
Ribs 7-10: “Bucket handle” - contraction of diaphragm
Ribs 10-12: “Caliper motion” - outwards and backwards swing
What are the 3 Basic elements of the Respiratory Control System? (C.E.S.)
Central Controller (brainstem)
Effectors (causes of ventilation)
Sensors (chemoreceptors to adjust output (Co2, H+ and O2)
What is the Normal PaCO2, and some problems that can arise?
Normal PaCO2 = 35-45mmHg
Type 2 Respiratory Failure (PaCO2 more than 50mmHg (hypoxemia) & PaO2 less than 60mmHg (hypercapnia))
What is Ventilation? + normal ranges
The movement of air between the environment and the lungs via inhalation and exhalation
Normal at rest: 5-8L/min
Light exercise: 12L/min
Moderate exercise: 40-60L/min
What is Work of Breathing (WOB)?
The amount of work that the respiratory muscles have to exert during a single respiratory cycle
Airflow resistance
Increased elastic load
Loss of elastic recoil
4 Causes of Respiratory muscle dysfunction?
Change is length-tension relationships (hyperinflation)
Myopathy (steroid-induced)
Neuromuscular disease
Connective tissue disorders
What is Dynamic Hyperinflation?
air gets trapped in the lungs during rapid or obstructed breathing, causing lung volumes to gradually increase above their normal resting level.
Objective Findings for Dyspnea (B.R.A.A.C)
Abnormal breathing pattern
Increased RR
Apical breathing (upper chest)
Accessory muscl use
Weak cough
How to assess Work of Breathing? (R.F.P.R)
Patient rates their symptoms
Impact on functional abilities
Clarify pattern of breathlessness
Look for reversible causes
H.I.F.L.O.W. Humidification Benefits
H - Heated & humidified
I - Inspiratory demands
F - Functional residual capacity
L- Lighter = more tolerable
O - Oxygen dilution
W - Washout of dead space (CO2 removal)
6 Physiologic mechanisms for efficacy of High Flow Nasal Cannula
Increases FRC
Physiological dead space washout of waste gases
Decreased respiratory rate
Provides positive end-expiratory pressure (PEEP)
Increased tidal volume
Increased lung recruitment
4 Outcome measures for Dyspnea
M
V
B
15
Medical Research Council Dyspnea Scale (MRC Scale)
Visual Analogue Scale (VAS)
Modified 0-10 Borg Breathlessness scale
15-count breathlessness score
5 Rights of Clinical Reasoning
Right Cue
Right Patient
Right Time
Right Action
Right Reason
pH level less than 7.35 / PaCO2 more than 50mmHg / HCO3 22-26 (normal) is what _________?
Uncompensated Respiratory Acidosis
pH level less than 7.35 / PaCO2 more than 50mmHg / HCO3 more than 26 is what _________?
Partially Compensated Respiratory Acidosis
pH level between 7.35-7.45 (normal) / PaCO2 more than 50mmHg / HCO3 more than 26 is what _________?
Compensated Respiratory Acidosis
pH level more than 7.45 / PaCO2 between 35-45mmHg (normal) / HCO3 more than 26 is what _________
Uncompensated Respiratory Alkalosis
pH level more than 7.45 / PaCO2 more than 50mmHg / HCO3 more than 26 is what _________
Partially Compensated Respiratory Alkalosis
pH level between 7.35-7.45 (normal) / PaCO2 less than 35mmHg / HCO3 less than 22 is what _________
Compensated Metabolic Alkalosis
OSCE: Positions of Comfort & Ease
High side lying
Supported side lying (optimal treatment position)
Unsupported 45-60deg
Supported in 45-60deg
Upright sitting supported
Slumped over railing, chair or table
Increase the curvature of diaphragmatic fibres (effectively contract)
Provide support for the arms/shoulder optimising accessory muscle function
OSCE: Breathlessness Techniques
Pacing
Breathing may be timed with stepping during walking or stair climbing
co-ordinate breathing control with activity.
Pursed lip breathing
Exhaling against pursed lips helps to splint open the airways and improve oxygenation…but it increases the work of expiration.
Blow as you go
breathe out on effort
Fan therapy
stimulates the trigeminal nerve reducing perception of breathlessness
Bronchiectasis
What is it: irreversible dilatation and destruction of the bronchial walls, leading to impaired clearance of mucus, recurrent infections, and airway inflammation.
Caused by: post-infection, immunodeficiency, tumors, enlarged lymph nodes
Clinical Features: Productive cough, foul sputum, hemoptysis, dyspnea
Management: ACT, antibiotics, bronchodilators, surgery, vaccines
Cystic Fibrosis
What is it: genetic, autosomal recessive disorder caused by mutations in the CFTR gene (Cystic Fibrosis Transmembrane Conductance Regulator).
Clinical Features: chronic cough, wheeze, finger clubbing, diabetes, malabsorption, steatorrhea (fat in feces)
Management: ACT, antibiotics, lung transplant, diet changes, CFTR modulators
Pneumonia
What is it: acute infection of the lung alveoli, interstitium, and distal airways, causing inflammation and consolidation
Caused by: CAP (community-acquired), HAP (hospital-acquired), immunocompromised
Clinical Features: fever, chills, cough, dyspnea, tachycardia, confusion, consolidation, bronchial breath sounds/crackles
Management: oxygen, IV fluids, antibiotics, steroids