Physiology of exercise exam 3
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
Nervous system
governor of the internal enviroment. Allows for volunatry control of muscles. Works with the endocine system to regulate processes. Intakes experiences to create memories and learn. Responsible for reflex arcs.
Central Nervous system
Brain + spinal cord
Peripheral Nervous system. efferent? afferent?
Neurons outside of the CNS that sense stimulation and carry out responses.
efferent = sensory neurons that send information to CNS
Afferent = motor neurons that carry out response from CNS.
Efferent divisions; Somatic sensory versus Visceral Sensory
Somatic sensory is stimuli that is consciously perceived (ex; hearing, seeing, smell)
Visceral sensory is stimuli that is uncounciously percieved (blood pressure, internal organ biomarkers, gas concentrations)
Afferent divisions; somatic motor versus Autonomic motor
Somatic motor; carrys out CNA response voluntairly ( skeletal muscle)
Autonomic motor; carrys out CNA response automatically (smooth muscle, cardiac muscle, hormone secretion)
Neuron Structure
Cell body: contains nucleus and cell genetics. integration of information.
Dendrite; receive messages from other cells
Axon: long myelinated cords that send information to other cells
Synapse; point of contact between a messanger and reciever cell. So a synapse for two nerve cells would be between a axon and a dendrite. Neurotranmitters are released inbetween this gap to deliver messages.
Presynaptic neuron? Postsynaptic?
Presynaptic neuron sends the message
Postsynaptic neuron recieves the message
Multiple sclerosis destroys the myelin sheath of axons. What does this result in?
Myelin sheaths are used to speed up and enhance the signaling of the AP. in MS, signals are slowed. senses are slowed and in severe cases transmissions are blocked.
Nerve irritabillity and conductivity
irritabillity; threshold for excitment. A neurons abillity to respond to a stimulus by sending an AP. (think of this as how easily somebody wakes up if you pour water on them as they sleep. waking up ==AP and the water is the stimulus. a light sleeper has high irritabillity)
Conductivity: ease of transmission of AP across the axon (ex myelination improves conductivity)
Resting membrane potential. charge? determination of charge? how body regulates the charge? Repolarization?
at rest the inside of a cell is NEGATIVELY charged.
Charge is influenced by how easily ions cross the plasma barrier of the cell and the relative concentration of K+ and NA (and i suppose cl- to but nobody really cares about cl-)
Charge is EDITED by the sodium potassium pump. potassium tends to leak out of cell to balance the charge on either side. The cell maintains this difference by pumping sodium out of the cell and actively transporting potassium into the cell.
Repolarization is when a cell reconvenes to it’s resting state. cell is now polarized and the intracelluar charge is now negative again
Action Potential. What happens to the cell’s membrane when an AP reaches said cell?
An action potential is a chain of cellular depolarization that creates an electrical signal to deliver messages towards and away from the CNS. A change from polarization to depolarization of a cell requires sodium to flood the inside of the cell while potassium ejaculates from the inside of the cell.
All or nothing princible.
The stimulus must be of sufficent strength in proportion to the cells irritabillity in order to generate an action potential. however, once the AP has been activated, it will definetly transmit across the length of the cell.
Synaptic transmissionx
Neurons do not physically touch each other. Instead they communicate across a synapse in which the presynaptic neuron sends neurotransmitters across the gap into the postsynaptic neurons receptors for said neurotransmitter
Excitatory post synaptic potentials (action potentials recieved by a post synaptic neuron) promote depolarization via two methods…
Temporal summoning: generating several EPSPs from one neuron. involves repeated firing of single presynaptic neuron
Spatial summoning: several neurons generating one or more EPSPS. Involves simultaneous activation of multiple pre-synaptic neurons
Inhibitory postsynaptic neurons;
Promote an even greater negative intracellular charge. Resists depolarization
Proprioception
Proprioceptor neurons provide the CNS with information about where joints and muscles are in space and time. They are located in joints and muscles
Kinesthesia
Conscious awareness of shank movement, such as location in space and speed of shank.
Free nerve endings
Receptors for touch and pressure of said touch. Most common joint proprioceptor.
Golgi-type receptors; what kind of proprioceptor and function?
Similar function of touch and pressure receptor akin to free nerve endings, yet these are found specifically in joints and ligaments.
Pacinian corpuscles; what kind of proprioceptor and function?
Located in surrounding tissues of joints; detect the rate of change of the joint rotation.
Muscle spindle; what kind of proprioceptor and function?
Proprioceptor for muscles that provide information ion the length of the muscle and the rate of contraction. Consists of intrafusal fibers (specialized cell that acts as sensory organ) and gamma motor neurons (stretch reflex regulator)
The muscle spindle is responsible for the stretch reflex and the “knee jerk reaction” via the gamma motor neuron.
Golgi Tendon Organ; what kind of proprioceptor and function?
Monitors the force generation of the muscle. It acts as an inhibitory neuron that activates a relaxant reflex as well as employs inhibitory post synaptic potentials (remember these RESIST depolarization). GTO can be dulled with exercise adaptation overtime.
Skeletal Muscle Chemoreceptors
Detect cellular or intercellular levels of co2, H+, o2, k+. Insight into skeletal muscle metabolism. Essential for cardiopulmonary response.
Motor neurons
Relay information TO skeletal muscles
Motor unit
One motor neuron, its axons, and the muscles it innervates
low ratio motor unit (less muscle fibers per motor neuron) function
Precise movement and control.
High ratio motor unit ( many muscle fibers per motor neuron) function
Simple yet powerful movements
How are muscle fiber types graded?
By the size of the motor unit. Remember, when we mean size we mean the number of fibers being innervated.
Type 1 ( Slow twitch): Smallest motor unit
Type 2a (intermediate): Medium Motor Unit
Type 2x (Fast twitch): Large motor unit
And remember, unit size is inversely proportional to its efficiency as well. Partly why type 1 excels at long duration activities.
Neural Control of Motor Function
Subcortical brain areas create a rough draft of an initial movement pattern. This movement is then edited by feedback from spinal mechanisms and proprioceptors
Aging effect on movement
Degrades nervous system and results in a loss of motor neurons. lost fibers get picked up by other neurons that have A high ratio of fibers per unit, resulting in a loss of coordinated movements. Remaining units have moderate to low threshold for recruitment.
Neuromuscular aging results in declines in
• Reflex time
• Peak force
• Peak power
Exercise effect on brain health
Increases capacity for learning and memory. Stimulates genesis of new neurons. Improves overall vasculature and thus blood flow to brain. Combats depressive symptoms. Combats contributors to neurological degradation (hypertension, inflammation, insulin resistance, etc.)
Neuromuscular junction
The point of synapse between a muscle fiber and a neuron. There are indeed multiple junctions along one fiber in order to spread out the signal. The neuron is the presynaptic component while the muscle is the postsynaptic component. Neurotransmitter release from the presynaptic neuron incites an excitatory response from the muscle fiber.
Neurotransmitter at the neuromuscular junction?
Acytelcholine
Adaptations at the neuromuscular junction in response to exercise:
Increase size of NMJ (larger motor end plate?)
More synaptic vesicles (which release ACH into the motor end plate where receptors are located)
Increase number of ACH receptors
All if this results in a stronger signal (purpose?)
(couple questions on this one ill ask her bout)
Qualities of Cardiac muscle
Autonomic with PNS and SNS innervation
Qualities of Smooth Muscle
Autonomic with SNS innervation only. Controlled via chemoreceptors and baroreceptors.
Qualities of Skeletal muscle
Somatic. Moves skeleton :)
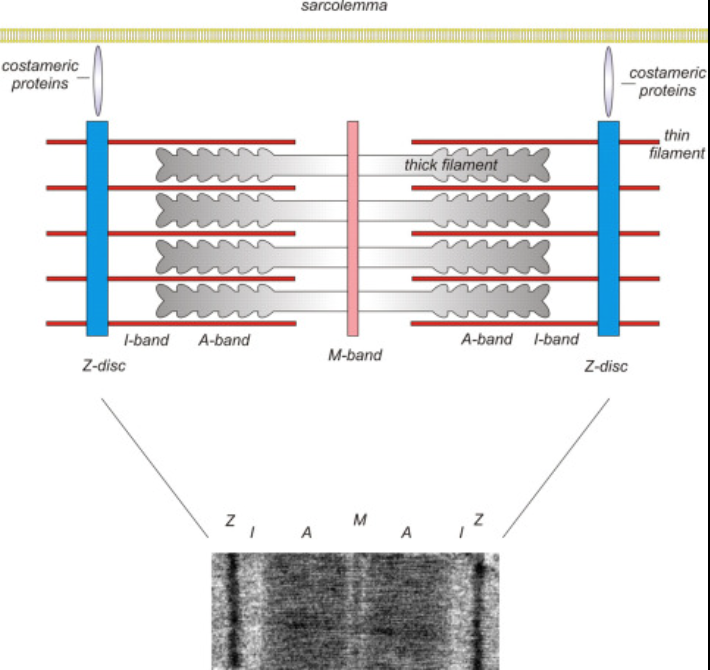
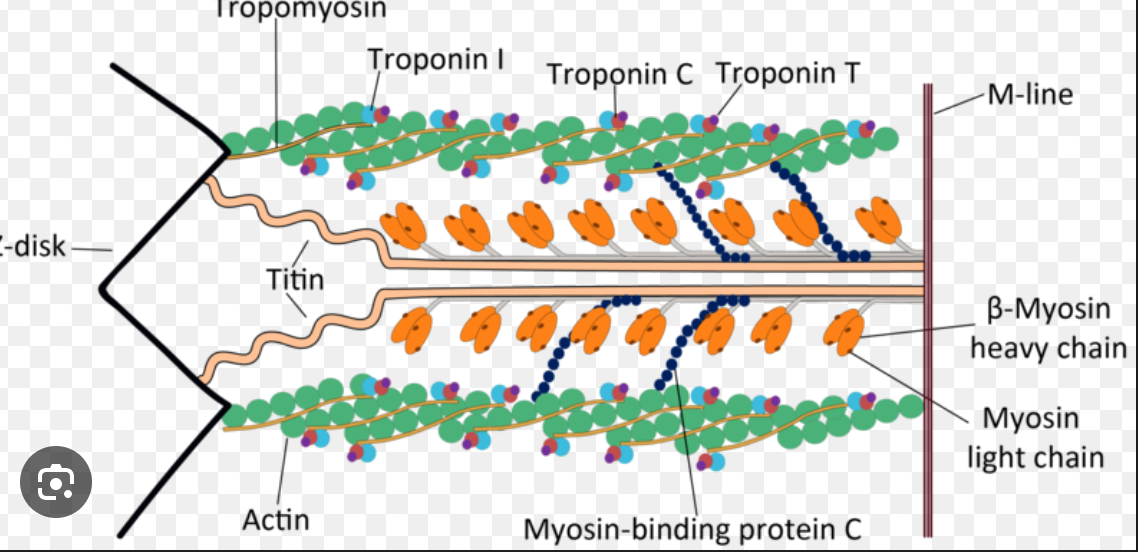
Sarcomere
Contractile unit of a muscle fiber. Measures from one z disk to the next z disk.
A band
Myosin strand with regions of myosin actin overlap
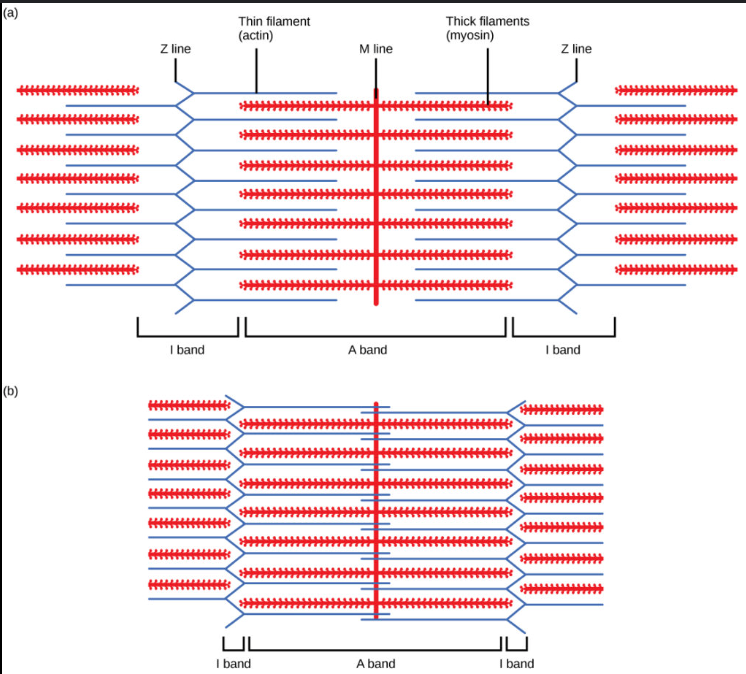
I band
Region of only actin
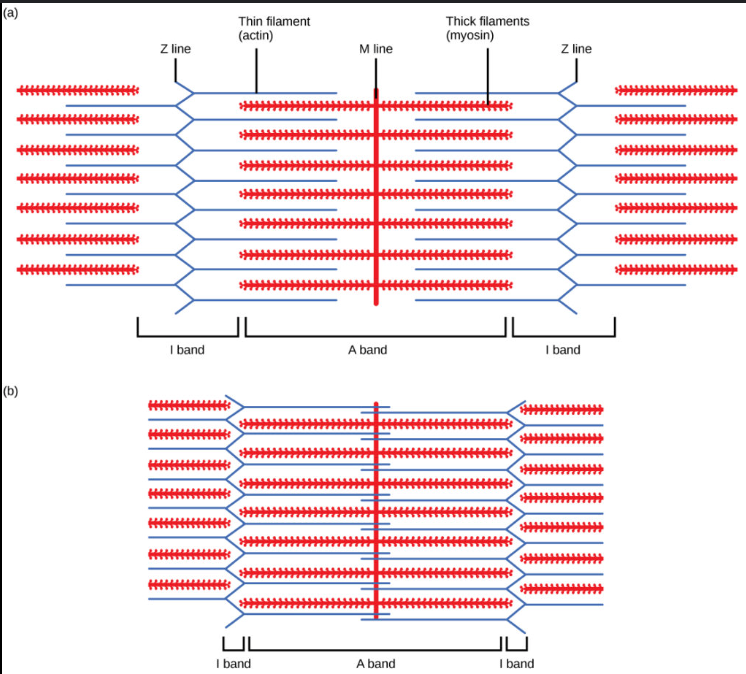
H zone
Central region of only myosin heads. Disappears during contraction
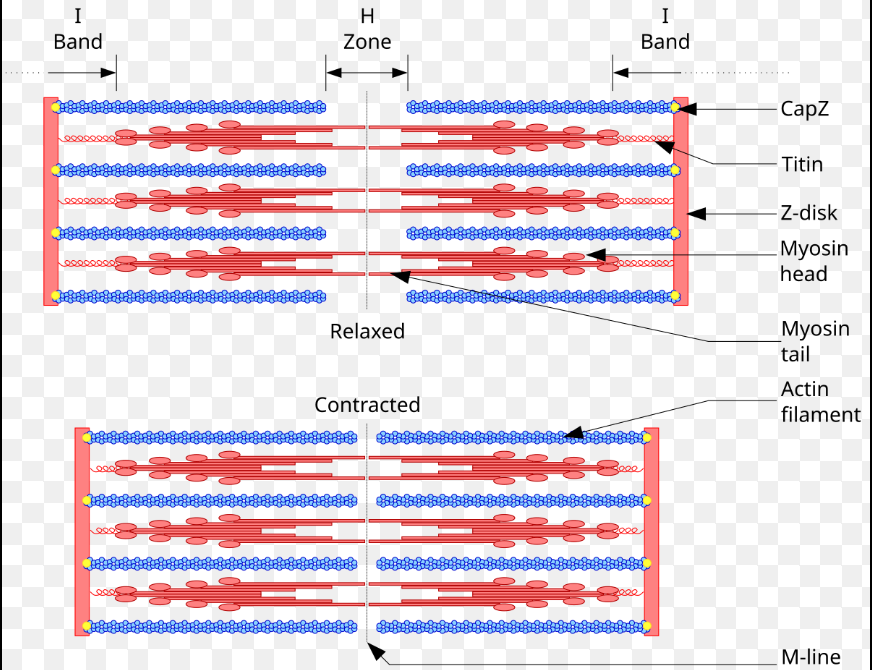
M line
Vertical line in the middle of the sarcromere
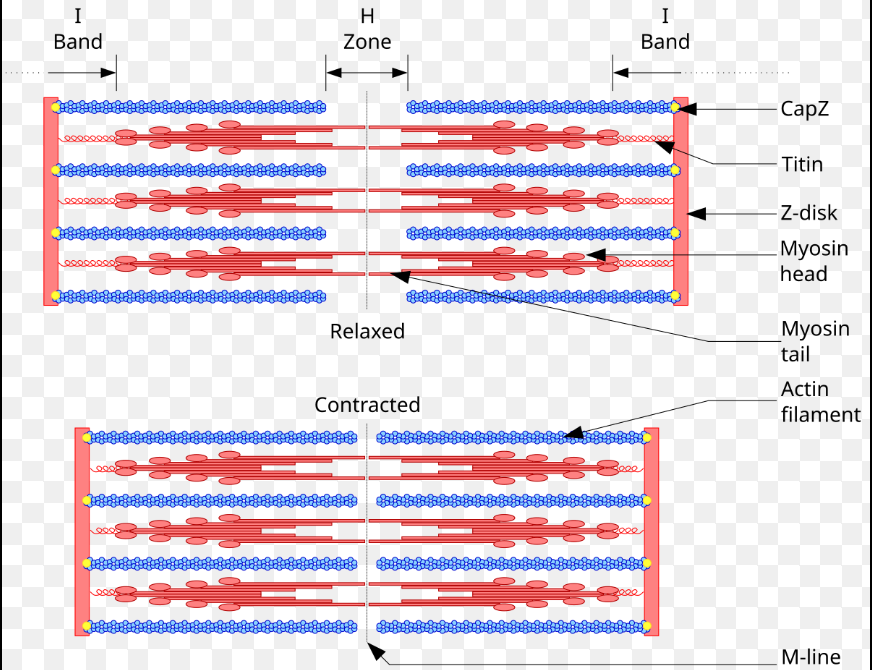
What structure is actin anchored to?
The z disk
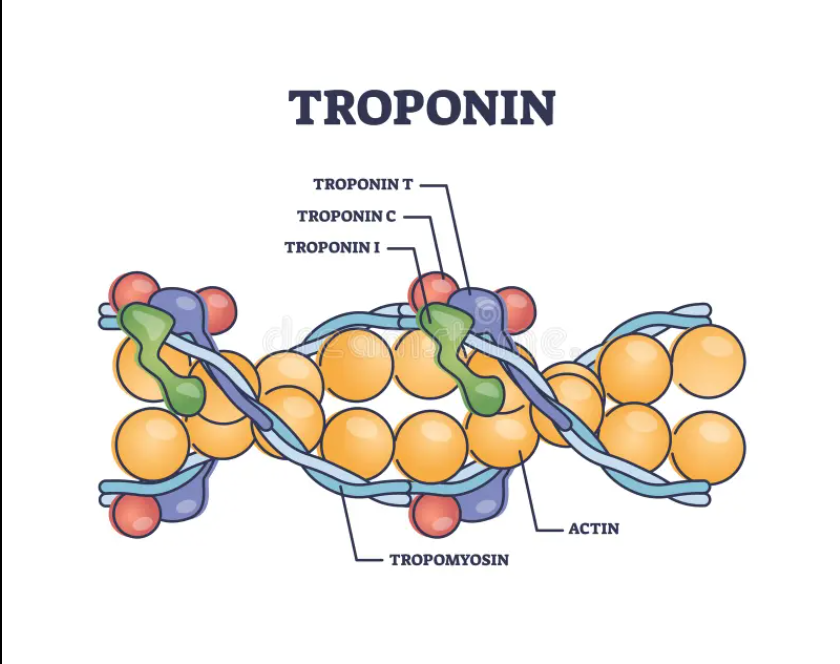
the three protiens of actin?
Actin: generates tension when interacting with myosin
Tropomyosin: Covers binding sites on myosin in order to prevent contraction (remember its function is related to its name; its the protien actively preventing myosin from binding. tropoMYOSIN)
Troponin: locomotor of tropomyosin. When bound to calcium it shifts tropomyosin off the binding sites
Components of troponin
Tnt: Binds to tropomyosin; essentially the bridge between the troponin tropomyosin complex (its in the last letter, tnT for Tropomyosin!)
Tni: Inhibitor of myosin actin interactions.
TnC: binds to calcium to introduce structural change to Tni (its in the last letter, tnC for calcium!)
Qualities of Myosin
2/3rds of our muscle is made of myosin. It is two intertwined filaments (thats why she be so thick, its two in one) with a gloublar head projection (globular head sounds amazing). Myosin is stabalized inside the sarcromere via titin. it connects to the Z disk.
Functions of skeletal muscle
Movement: DUH MUSCLE MOVE SHIT
Posture: Static and dynamic balance
Stabalizes Joints: self explanatory
Heat: Metabolism from contraction is heat ^^^
Sliding filament theory
Muscle contraction occurs when the actin and myosin filaments slide over each other. Z disks get closer to each other. (ask if we have ti know about atp binding to myosin head)
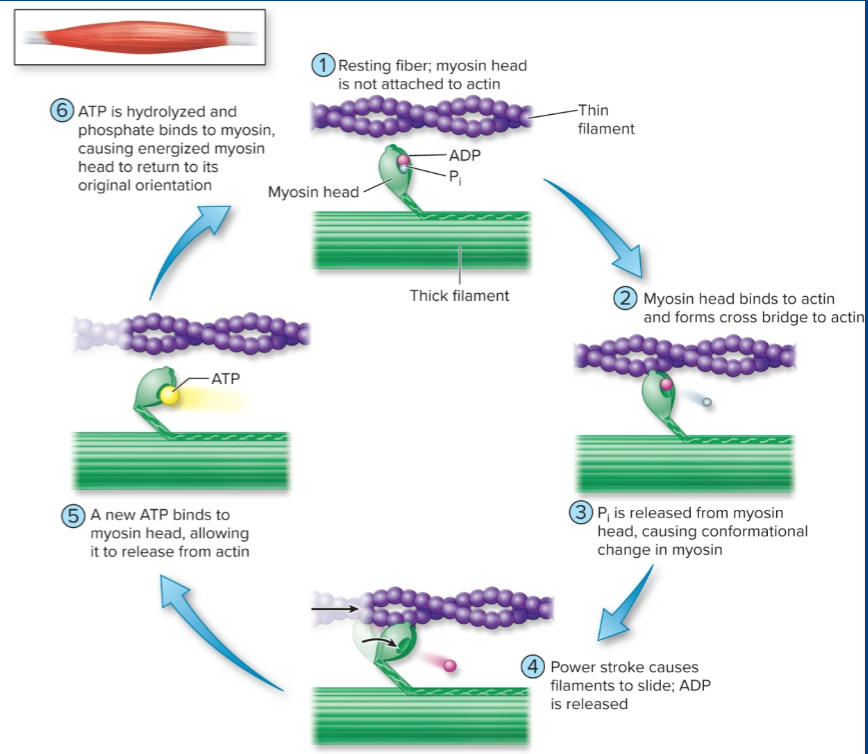
Muscle contraction steps:
AP travels down a neuron.
AP stimulates synaptic vessicles to release its ACH into the synapse
ACH binds to ACH receptors at the motor end plate.
Binding of ACH generates an action potential, which spreads the length of the muscle fiber.
AP travels down T tubule and eventually stimulates sarcroplasmic reticulum to release calcium
Calcium binds to troponin, which then moves tropomyosin out of the way and exposes binding sites on actin.
Globular head binds to actin and performs power strokes.
once contraction cycle has ended, calcium returns to sarcoplasmic retictlum. troponin moves tropomyosin back over the binding site.
Skeletal muscular fatigue
Occurs due to a decrease in force production at the level of the sacromere and a decrease in muscluar shortening velocity
Mechanisms of fatigue during high intensity exercise
Metaboloites, H+, Pi, and free radicals in our scope, are our culprit here. Metabolites interfere with a variety of processes.
*Hydrogen prevents contracting by binding with TnC
*Pi and radicals disrupt the structure of globular heads and thus reduce the number of crossbridges bound to actin
Mechanisms of fatigue during moderate intensity exercise
Free radical’s disrupt the myosin crossbridge structure. Muscle glycogen depletion decreases rate of glycolysis via oxidative phosphorilation and also reduces TCA cycle, reducing TCA intermediates.
(Ask about Pi and why Oxidative phosphorilation decreases)
Muscle cramps
Involuntary muscular contractions associated with high intensity exercise.
What are some ways muscle fiber types categorized?
Force generated per cross sectional area
Speed of contraction (Related to ATPase density)
Maximal power: that can be produced; Force * Shortening velocity
Ability to resist fatigue
Efficency of contraction (how much ATP does this need for x amount of force?)
Methods of determining muscle fiber type
Muscle biopsy: (small piece of muscle removed)
Immunohistochemichal staining: dyes bind to specific kinds of myosin head forms.
Gel electrophoresis: Myosin is seperated by size.
ATPase activity for different muscle fibers?
Type 1 = lower atpase activity
Type 2 = higher atpase activity
Type two goes through more ATP because it is quicker and less efficent. Theorefore it needs more atpase.
Which type has a more well developed SR?
Type II for a more rapid calcium release
Cell body size for muscle fiber types
Type 1 == teeny tiny
type 2 == obese
Recruitment pattern during exercise (from lowest intensity to highest)
type 1 —> type 2a —> type 2x
What motor unites recruit the most force?
Type 2 motor units (remember recruitment is based on the size of the fiber. one motor neuron innevrates fibers that have the same properties.)
Concentric
Contraction is greater than the force placed on it (muscle shortening)
Eccentric
Contraction is lesser than the force placed on it (muscle lengthening)
Isometric
equal to force placed on it
Muscle twitch
contract relax cycle from a single stimulus
What happens if an AP is sent before the muscle can fully relax
the contraction becomes stronger because of temporal summation. one “twitch” gets added to the next.
Remember the time scale on this; your body can achieve complete tetanus in milliseconds
Complete tetanus
multiple stimuli occuring that results in a smooth sustained contraction. there is no time for relaxation at all
incomplete tetanus
forceful contractions that appear more fluttered on a graph of APs. There is vert little relaxation here.
How does neural drive regulate skeletal muscular force production
increase of stimulus == increase force production
What does post activation potential mean and what does it accomplish for our physiology?
PAP essentialy states that a warmup contraction or stimulus will result in a more forceful contraction afterwards. an increase of temperature achieved by a warmup contraction increases cellular and enzyme function .(Ask her for clarification!)
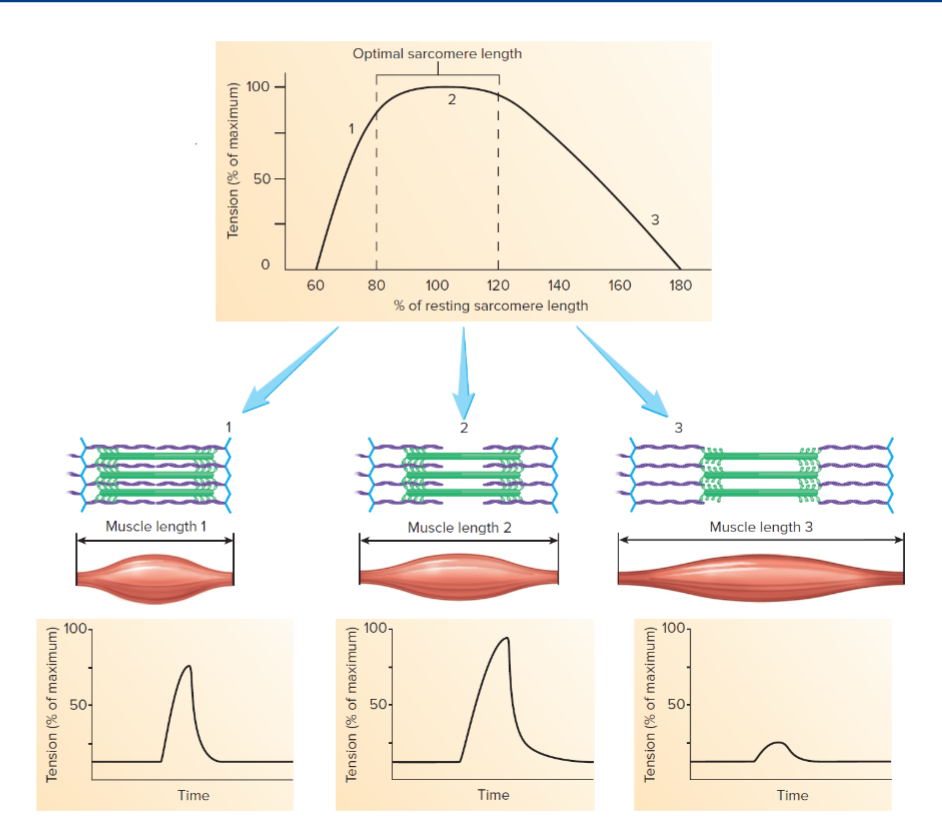
Muscle length/tension relationship; how is muscle length related to force of contraction
in general, a shorter muscle has a greater actin myosin overlap and will thus result in a stronger contraction. the caveat is if the muscle is close to full contraction, there will not be enough “room” for the contraction to actually result in any movement.
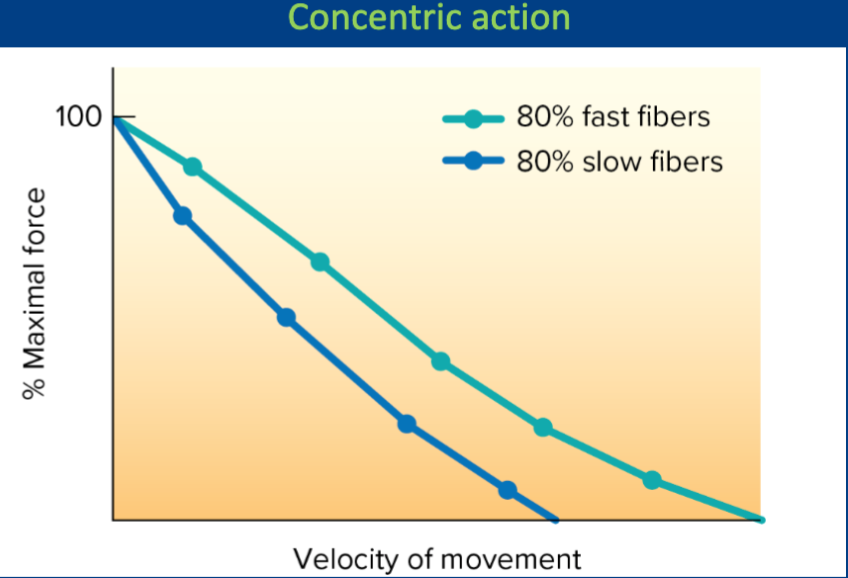
What is the relationship between amount of force generated and the speed of movement? Also, at the same given force, what muscle fiber will have a greater speed of movement? (THIS IS A CONCENTRIC CONTRACTION)
There is a positive relationship between force generated and speed of movement. At the same given force, fast twitch will have a greater velocity
At the same given power output of muscles, what happens to velocity as the force we place on the muscle increases?
the velocity increases
Body composition
Tissue makeup of the body
Identify the various models of body composition (chemichal, anatomical, two compartment
Chemical compartmentalizes the body on a molecular level (adipose, protien, mineral, water, etc.)
Anatomical compartmentalizes the body on a tissue level (muscle, bone, organ(not really tissue but whatever), adipose)
Two compartment model compartmentalizes the body between fat and fat free mass (everything that is NOT fat)
Function and qualities of essential fat? non essential fat?
Essential fat is required for physiological function. It is located in bone marrow (YELLOW BONE MARROW @JSCHEER), the heart, the lungs, muscles, and CNS.
Non essential fat is for insulation and protection of vital organs. Thus, it is usually around vital organs as well as underneath the skin. (subcutaneous)
Functions of fat
Warmth and protection
Stored energy (highest energy macro!)
Cellular structure (Remember bio 101? cell membranes are made of phosphoLIPID bilayer)
Essential for nervre conduction (fat makes up the myelin sheaths!)
A component of steroid based hormones
Neccessary to absorb vits the are fat soluble
Fat Free Mass Functions
Muscles = movement
Vits/Mins = Immune function, growth and development, bone health (CALCIUM HYDROXYAPATITE)
Water = thermoregulation, blood plasma (transportation), lubrication of joints, cushions brain and spine, digestion.
Relationship with adipose tissue and disease risk
Curvilinear relationsip. If one is too lean, they have poor prognosis. As they gain fat to a healthy level, they have optimal health in terms of the amount of fat they have. As fat levels increase beyond healthy levels, they return to poor health.
Outcomes coorelated with high adipose levels:
Cardiovascular disease
stroke
Arthrities
Hypertension
Metabolic disease
Type 2 diabetes
Outcomes coorelated with low adipose tissue
Compromised immune system (remember myelin sheaths?)
Hormone disregulation (remember its role in steroid hormones?)
Anemia (again, somehow hormone related)
Pregnancy complications (again hormones)
Bone loss (yep. Hormone related)
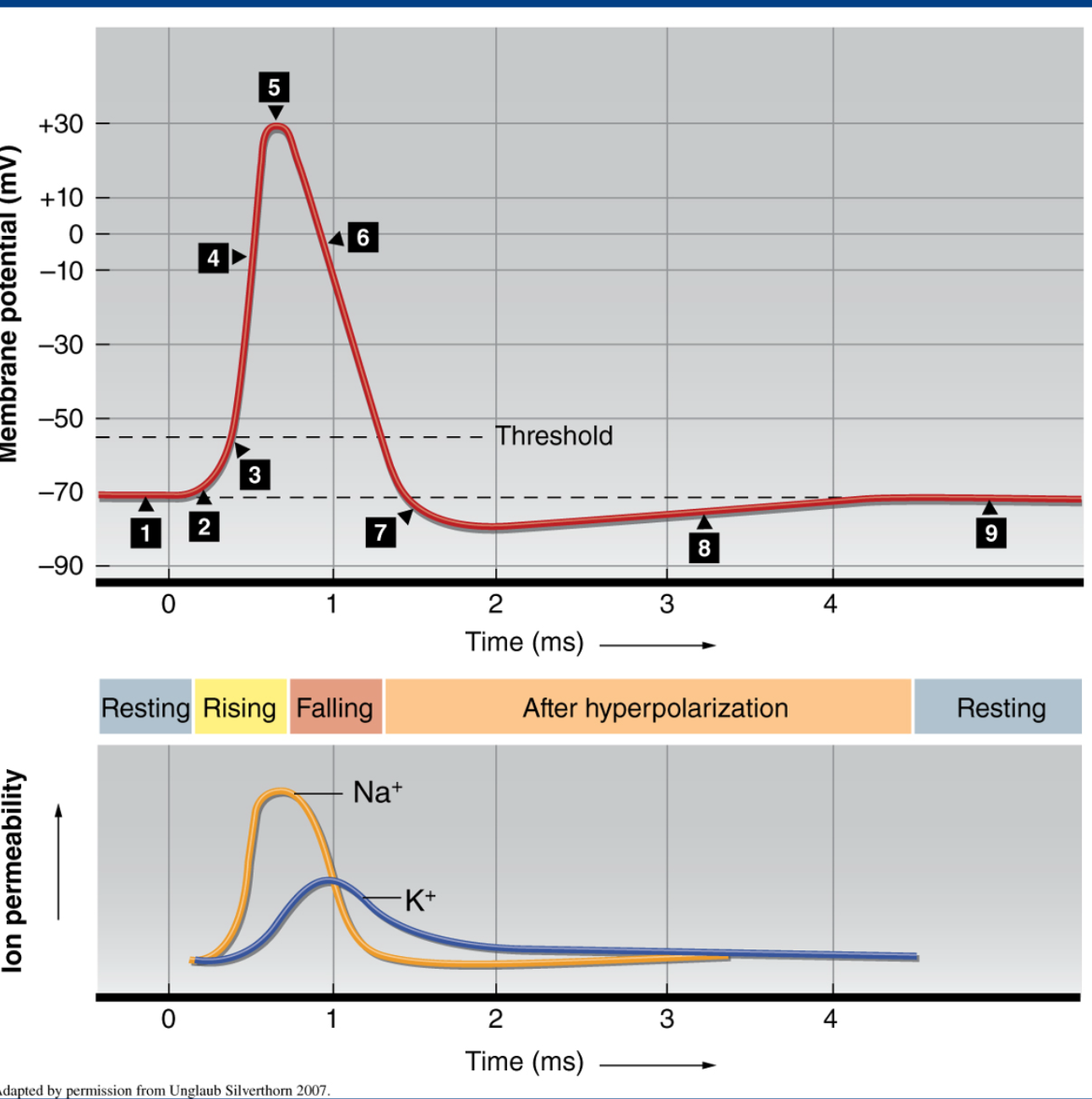
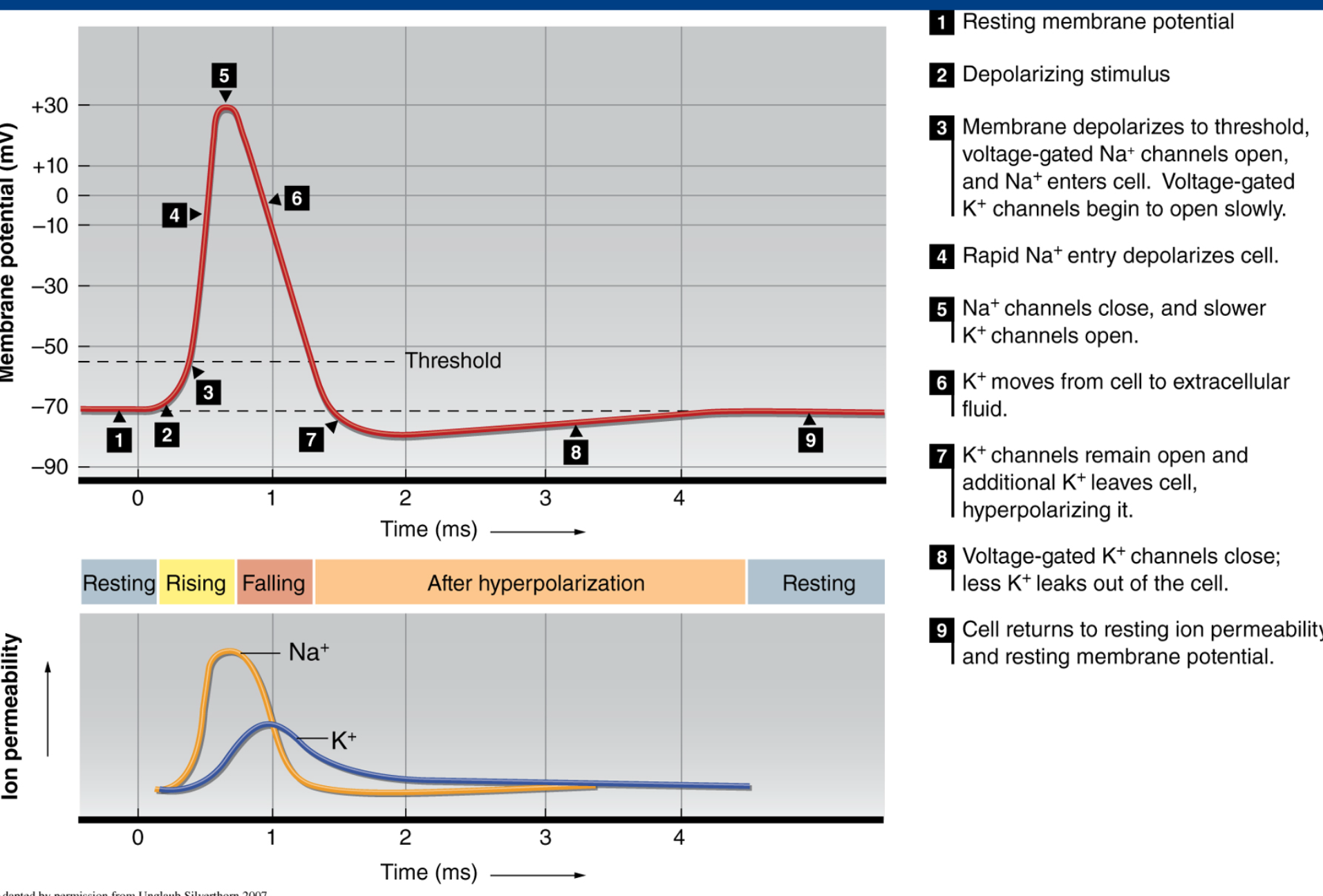
Action Potential graph: explain 1-7 and why it is in concert with the below graph. (i will ask her about some of the intricacies of this graph as well.)
Resting membrane potential. Sodium is high on the ECF and Potassium is high on the ICF
A stimulus is introduced to the receptor (like a neurotransmitter; take ACH binding to its receptor or example) small amount of depolarization occurs. ion permeabillity of sodium begins to spike as seen below
Depolarization levels are significant enough to reach the threshold.
Sodium floods the cell in concert with the opening of the NA+ gates. degree of polarization rises as seen by the mv reading.
Sodium channels close. Delayed potassium channels start to open
potassium is starting to leave the cell. degree of polarization decreases. As we can see on the ion permiabillity graph, potassium permiabillity is at its highest! Also, with the closing of sodium channels, sodium’s ion permiabillity has started to decrease
potassium and sodium have now offically flipped the flop, so much so that membrane potential has gone below baseline! K+ channels remain open, this is what we call hyperpolarization
k+ channels begin to close now. ion permiabillity of k+ has decreased.
cell returns to resting potential
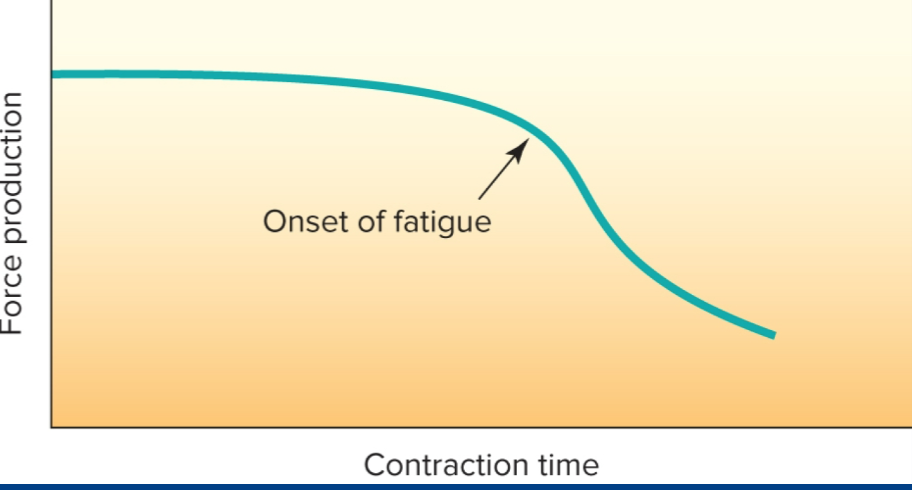
Explain dis graph. be able to draw it
as contraction time increases, the force production of said muscled decreases. Why? metabolic intermediates such as Pi, free radicals, and hydrogen fuck with cross bridges. For long duration activites, muscle glycogen begins to deplete, decreasing TCA intermediates and substrates for bioenergetic pathways.
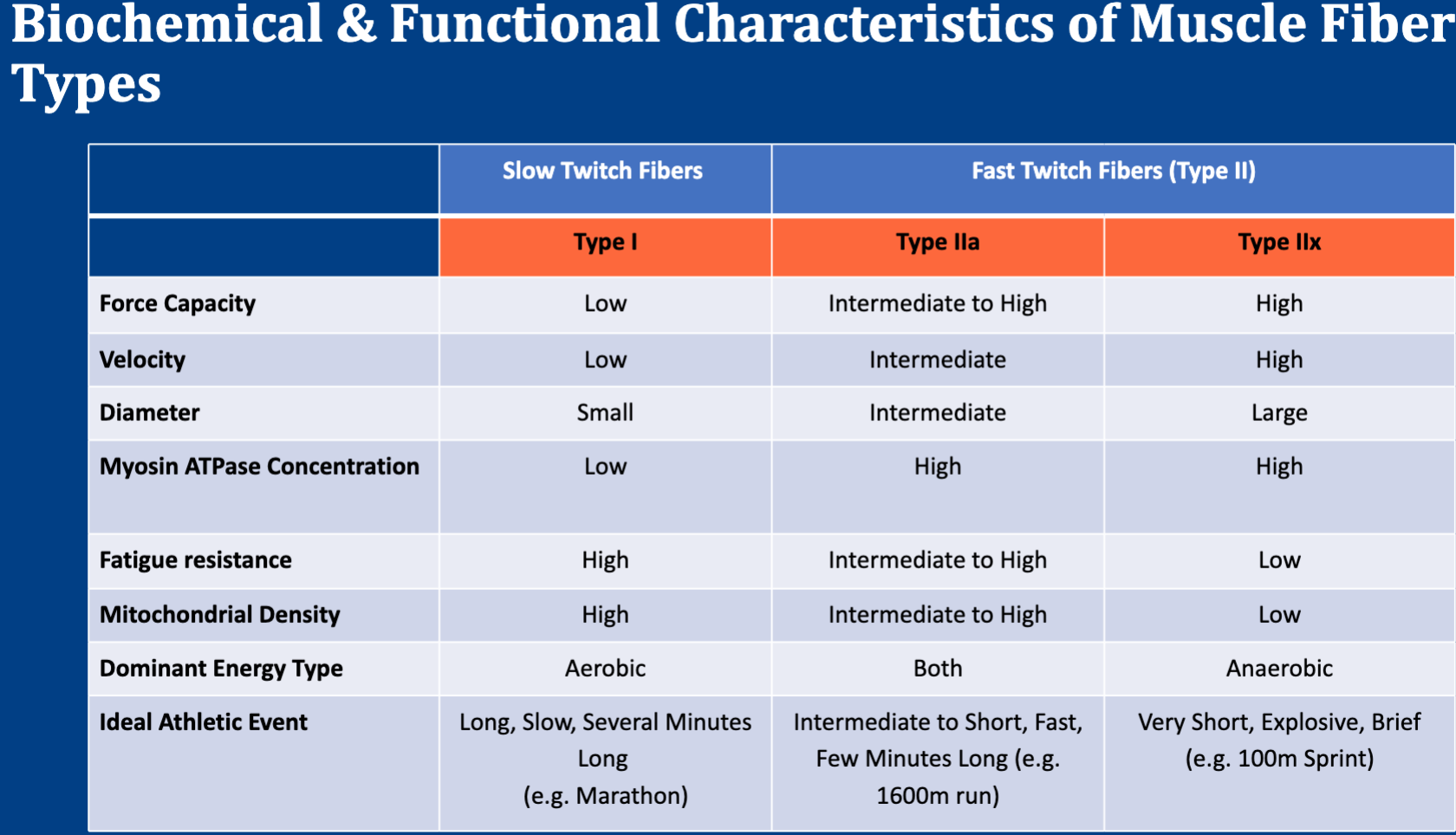
THIS BITCH WILL DEF BE ON THERE I SAW THE WAY SHE TALKED ABOUT IT
Its easy thou. the only thing to watch out for is that atpase concentration is also gonna be high in 2a. other than that it is extremely intuitive.
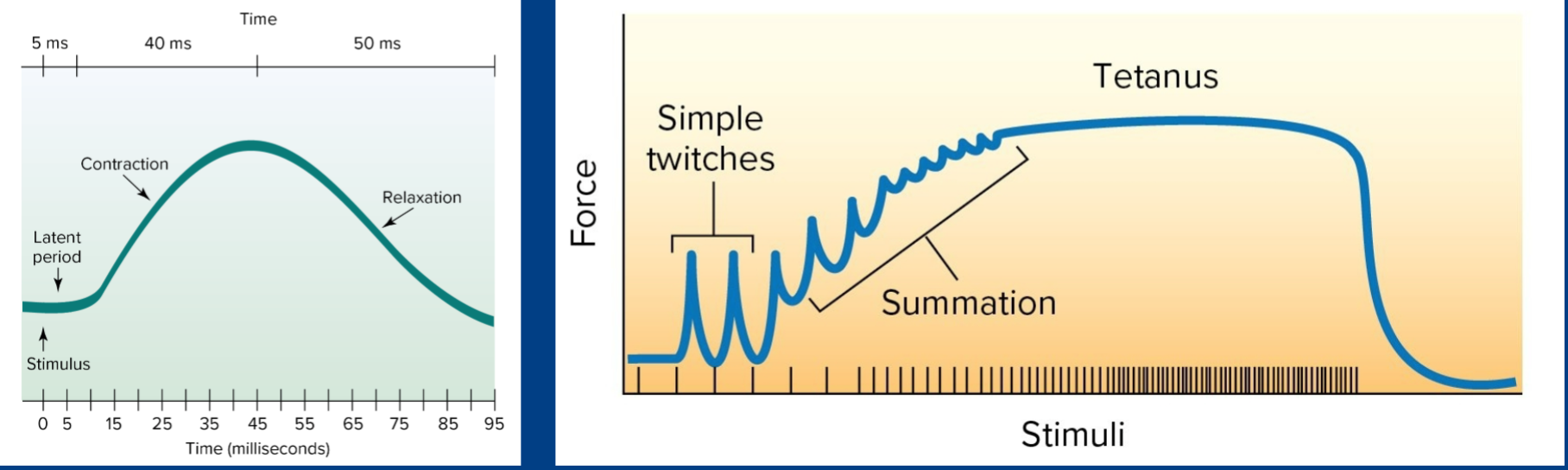
ok. dafuq going on here?
If you start sending out APs faster than the muscle can fully relax, the stimulus gets added on to the same AP, increasing the force of contraction. This is incomplete tetanus, leading to complete tetanus
ok. dafuq going on here?
fast twitch muscle fibers are gonna have a higher force generation at a given force than slow twtich.