Module 1: Pregnancy/Preterm Labor/Labor, Delivery, & Postpartum
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
89 Terms
1. steroid hormones
2. GI motility
3. pH
4. GFR
5. drug dilution
6. concentrations
Changes in Drug Action During Pregnancy
-Effect of circulating (1) (progestin, estrogen) on liver’s metabolism of drugs
-Reduced (2) and increased gastric (3)
GERD is common
-Increased (4) and increased renal perfusion
-Expanded maternal circulating blood volume causing (5)
-Alteration in drug clearance in later pregnancy causing decrease in drug (6)
pregnancy, labor, certain disease states
What are three factors that alter drug half lives?
teratogens
substances that cause developmental abnormalities
prevent maternal iron deficiency anemia - not to supply the fetus
What is the goal of iron supplementation during pregnancy?
Adverse Reactions of Iron
N/V, constipation, black tarry stools, diarrhea, epigastric pain, urine discoloration
-inform patient of adverse rxns (not tolerated well by most individuals)
-should be separated 2 hr before or after meals
-green tea can affect absorption rates
What are three nursing implications for iron?
before pregnancy
When should you start folic acid supplements?
reduce birth defects, notably neural tube defects
What's the goal for folic acid supplements r/t pregnancy?
Adverse Reactions of Folic Acid
bronchospasm, flushing, rash, pruritus, erythema, malaise, dark yellow urine
Cues Associated w/Preterm Labor
-Headache
-Sinus congestion
-Eye strain
-Backaches
-Joint pain
-Round ligament pain
N/V, heartburn (pyrosis), constipation, pain
Name four discomforts associated w/pregnancy.
hyperemesis gravidarum
excessive vomiting during pregnancy
Elevation
Crackers
Adequate hydration
Avoid greasy, gas-forming foods, citrus juices, reclining immediately after eating
Name four non-pharmacologic measures for treating discomfort during pregnancy.
pyridoxine hydrochloride (B6), doxylamine succine (antihistamine + B6)
What are two medications that help treat N/V r/t pregnancy?
antacids, chewable calcium carbonate, histamine2 receptor antagonists, proton pump inhibitors
What are four medications that help treat heartburn r/t pregnancy?
acetaminophen; ASA and NSAIDs aren't recommended
300 mg
What's the recommended analgesic during pregnancy and its max dosage/day?
SSRIs, tricyclic antidepressants
What are two antidepressants that are commonly used during pregnancy?
1. birthweight
2. preterm
3. attentiveness
4. irritability
Antidepressant Drugs During Pregnancy
Associated w/adverse birth outcomes
-Low (1), born small for gestational age
-(2) delivery
-decreased (3)
-increased neonatal (4)
1. substance abuse
2. aspirin
3. iron
Clinical Judgment: Antepartum Drugs
Concept: Reproduction
Recognize Cues:
-Identify pts at risk for (1)
-Review history of (2) use
Analyze cues and prioritize hypothesis:
-Anxiety, need for pt teaching
Generate Outcomes
-Pt will discuss drugs and herbal supplements w/HCP before use
Take action
-Advise pt ot use decaffeinated products or dilute caffeinated products
-Instruct patient about nonpharmacologic and pharmacologic measures to relieve discomforts
-Instruct patient about nausea, constipation, and bowel habit changes if they’re taking (3)
-Encourage patient to speak w/their HCP before taking any drugs
smooth
What type of muscle is the uterus?
39-40 weeks
What is full-term pregnancy?
preterm labor (PTL)
cervical changes and uterine contractions occurring at 20 to 37 weeks of pregnancy
12% of pregnancies
How prevalent is PTL?
Goals of PTL Care
-Interrupt or inhibit uterine contractions to create additional time for fetal maturation in utero
-Delayed delivery so antenatal corticosteroids can be delivered to facilitate fetal lung maturity
-Allow safe transport of the patient to an appropriate facility if required
1. 20 weeks
2. rupture
3. fetal death
4. hemorrhage
Contraindications of Tocolytic Therapy
-Pregnancy of less than (1) gestation
-Bulging or premature (2) of the membranes
-Confirmed (3) or anomalies incompatible w/life
-Maternal (4) and evidence of severe fetal compromise
-Chorioamnionitis
chorioamnionitis
infection of the amniotic fluid and tissue that surrounds a fetus during pregnancy
tocolytic therapy
-Drug therapy used to decrease uterine contractions
-Not FDA approved and are used “off label”
beta-2-sympathomimetic (terbutaline) and magnesium sulfate (calcium antagonist)
What are two drugs used in tocolytic therapy?
delay delivery by 48 hr to maximize effect of the glucocorticoids
What's the goal of corticosteroid therapy in PTL?
stimulates beta 2-receptors on uterine smooth muscle (relaxes them), which decreases the frequency and intensity of uterine contractions
What's the action of terbutaline?
only for short term prolongation of pregnancy
What's the black box warning of terbutaline?
tachycardia, ketoacidosis, pulmonary edema, anaphylactic shock
What are four adverse reactions of terbutaline?
SUBQ injection
How is terbutaline administered?
relaxes smooth muscle of the uterus through calcium displacement
What's the action of magnesium sulfate?
calcium gluconate
What's the antidote of magnesium sulfate?
1. maturation 2. surfactant 3. respiratory distress syndrome 4. intraventricular
Action of Corticosteroid Therapy
-Accelerates lung (1) and lung (2) development in the fetus in utero
Infants don’t produce much surfactant, which is what keeps alveoli open
-Decreases incidence and severity of (3)
-Increases survival of preterm infants
-Decreases incidence of (4) bleeds
betamethasone, dexamethosone
What are two drugs used during corticosteroid therapy?
1. 24 hr 2. shake 3. heat/light 4. large muscle
Clinical Judgment: Betamethasone
Concept: Reproduction
Recognize Cues:
-assess for history of hypersensitivity
-assess VS and FHR
Analyze Cues
-Anxiety, need for pt teaching
Generate Solutions
-The pt will not deliver within (1) of receiving betamethasone
Take Action
-(2) the suspension well
-avoid exposing drug to excess (3)
-inject drug into (4), not the deltoid
-maintain accurate I&)
gestational hypertension
-Most common serious complication of pregnancy
-SBP > 140 or DBP > 90
-AKA pregnancy-induced HTN
preeclampsia
hypertension, edema, and proteinuria during pregnancy
HELLP syndrome
What's a severe sequel of preeclampsia?
defined by hemolysis, elevated liver enzymes, and low platelet count [thrombocytopenia]
What does the acronym of HELLP stand for?
eclampsia
(preeclampsia + seizures)
New-onset grand mal seizures in a patient w/preeclampsia
reduction of vasospasm and prevention of seizures?
In addition to delivery of an uncompromised fetus and psychological support for the patient and family, two primary treatment goals in preeclampsia are what?
methyldopa
What's the first line therapy for mild preeclampsia?
stimulates alpha-adrenergic receptors (resulting in decreased sympathetic outflow to heart, kidneys, and peripheral vasculature)
What's the action of methyldopa
Adverse Reactions of Methyldopa
-Peripheral edema, anxiety, nightmares, fever
-Drowsiness, headache, dry mouth, mental depression
hydralazine
What drug is used to treat acute onset, severe HTN r/t gestational HTN?
arterial vasodilator
What's the action of hydralazine?
Adverse reactions of Hydralazine
-Headache, dizziness, nasal congestion, angina
-Nausea, vomiting, tachycardia, hypotension, palpitations
magnesium sulfate
What drug is used to treat severe preeclampsia?
calcium antagonist
What type of drug is magnesium sulfate?
Adverse Reactions of Magnesium Sulfate
-Lethargy, flushing, warmth, perspiration, thirst, sedation
-Heavy eyelids, slurred speech, hypotension, decreased DTR, decreased muscle tone
1. BP
2. preeclampsia
3. emergency drugs
4. left lateral recumbent
5. toxicity
Clinical Judgment: Gestational HTN
Concept: perfusion
Recognize cues:
-VS from early pregnancy, (1) readings during prenatal visits
-Pt history predisposing pt to (2)
Analyze cues and prioritize hypothesis:
-Decreased tissue perfusion
Generate Solutions
BP within acceptable ranges
Take action
-Airway, suction, resuscitation equipment, and (3) available
-Maintain pt in a (4) position in low-stimulation environment
-S/S of magnesium (5)
Nonpharmacologic Pain Management r/t pregnancy
Ambulation
Effleurage and counterpressure
Touch and massage
Changing positions and rocking
Engaging support persons
Breathing and relaxation techniques
Transcutaneous electrical nerve stimulation
Application of heat and cold
Aromatherapy
Hydrotherapy (warm water baths)
Alternative and complementary drugs
visceral pain during labor
First 2 stages of labor from uterine contractions and pressure of stretching cervix
somatic pain during labor
-Pressure of presenting part and stretching of the perineum and vagina
-Pain of transition phase and 2nd stage of labor
sedative hypnotics
-Drugs that can act in the body either as sedatives or as hypnotics
-Adverse effects: opioid based risks, crosses placenta to baby
-e.g. Pentobarbital, hydroxyzine.
opioid agonists
-Adverse effects: opioid based risks, crosses placenta to baby
-E.g. fentanyl, morphine
mixed opioid agonist-antagonists
Adverse effects - opioid based risk
E.g. butorphanol
Drugs cross placenta; may temporarily affect HR of fetus
What's the black box warning of systemic pain management drugs used during pregnancy?
(sedative-hypnotics, opioid agonists, and mixed opioid agonst/antagonists)
Goals of Regional Anasthesia
-Achieves pain relief during labor and delivery w/o loss of consciousness
-Temporarily blocks painful impulse conduction while maintaining consciousness
Lidocaine for episiotomy, which can cause burning at site of injection
What's an example of local anesthesia?
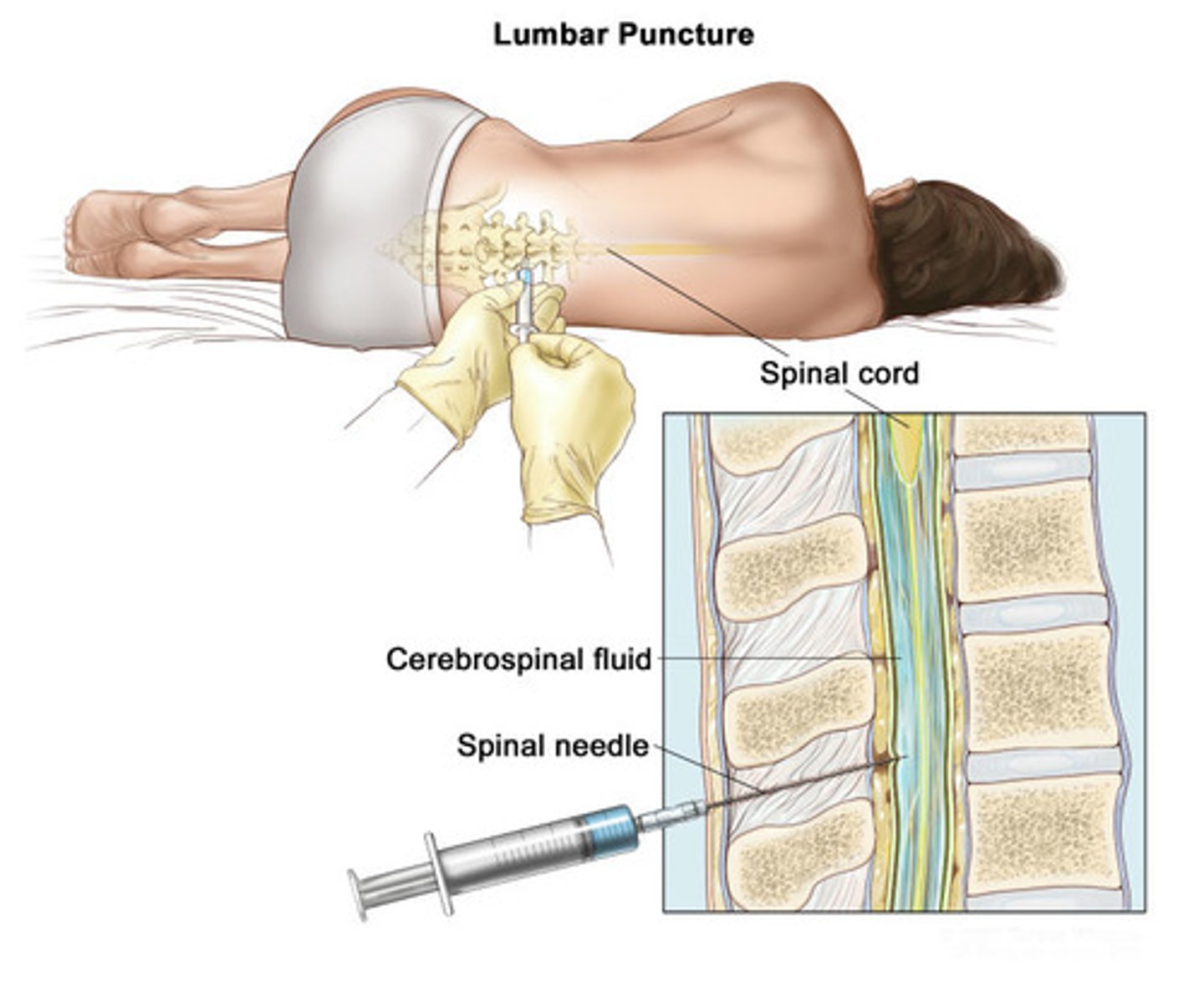
subarachnoid, T10-S5; lumbar
Regional anesthesia includes spinal, in the ____ space ____, or epidural, in the _____.
general anesthesia
May be necessary for emergency deliveries and/or when spinal and epidural is C/I
uterotropics
Used in term/near term pregnancy w/an indication for labor induction of labor augmentation
dinoprostone, oxytocin, and ergot alkaloids
What are three uterotropic drugs?
dinoprostone (Cervidil)
-Cervical ripening agent
-Creates cervical effacement and softening for cervical dilation
oxytocin
-Labor induction
-Stimulate uterine contraction by increasing intracellular calcium
-Synthesized in hypothalamus and secreted from posterior pituitary gland
Direct smooth-muscle-cell receptor stimulation
What's the action of ergot alkaloids?
Can cause tetanic contractions resulting in fetal hypoxia and possible ruptured uterus
Why aren't ergot alkaloids used during labor?
1. hemorrhage
2. involution
Uses of Ergot Alkaloids
USED AFTER DELIVERY
-Control postpartum (1) (bleeding)
-Promote uterine (2)
preexisting/gestational HTN, peripheral vascular diseases
What are two contraindications for ergot alkaloids?
Side effects of ergot alkaloids
-Uterine cramping, nausea, vomiting, sweating
-Dizziness, tinnitus, sudden severe headache
-Itching, HTN, chest pain, dyspnea
-Ergot toxicity
hypertensive patients
In which population should you proceed with caution for ergot alkaloids?
1. dilation
2. hydration status
3. positioning
4. FHR
5. distension
Clinical Judgment: Regional Anesthetics
Concept: pain
Recognize cues:
-Check sensitivity to local anesthetic agents
-Assess cervical (1)
Generate solutions
Verbalization of pain relief
Take action
-Assess (2) before anesthesia is given
(IV bolus of 500-1000 mL)
-Proper (3) (left side)
-Monitor maternal VS and (4)
-Assess uterine contractions
-Assess for bladder (5)
1. peri-bottle
2. benzocaine spray
3. 6-12
4. prolonged use
Clinical Judgment for Pain Relief for Perineal Wounds
Concept: pain
Recognize cues
-Pain rating
-Presence of infection at perineal site
Generate solutions
-Free of S/S of infection
Take Action
-Teach pt use of (1)
-Don’t use (2) when perineal infection is present
-Shake spray can and administer benzocaine (3) inches from perineum w/pt lying on her side, top leg up and forward
-Advise pt that drug is not for (4)
maternal rubella
-German Measles (virus)
-Devastating to a fetus
-Depends on gestational age
-First trimester risks are worst
-Goals in care: immunize and prevent rubella in pt of child bearing age
congenital rubella syndrom
-transmission of rubella virus to fetus via the placenta
-cataracts, glaucoma, deafness, heart defects, mental retardation
1. Rh sensitization
2. second
3. after delivery
Rh₀ (D) Immune Globulin
-Rh-negative mother + Rh-positive fetus → mother is at risk for (1) (development of protective antibodies against incompatible Rh-positive blood)
-in (2) pregnancy, there's a more rapid IgG immune response and an increased potential for fetal hemolysis in an Rh-positive fetus
-Rh₀ (D) immune globulin is routinely administered (3) to women w/maternal/fetal blood mixing
1. hypersensitivity reactions
2. 72 hr
3. epinephrine
Clinical Judgment: Clients Receiving Rh₀ (D) Immune Globulin
Concept: Perfusion
Recognize Cues
-Determine blood type and Rh status of prenatal patient
-Follow agency policy for Rh blood testing for patients and infants at delivery
Analyze cues
(1)
Generate solutions
Pt will receive Rh0(d) immune globulin as indicated within (2) after delivery or abortion
Take action
-Document Rh workup and eligibility of pt to receive drug
-Check lot numbers on vials and lab administration
-Administer Rh0(d) immune globulin according to gestational weeks, exposure and route, provider orders, and agency protocol
-Have (3) available to treat anaphylaxis
Use of NSAIDs for Pain Relief During Uterine Contractions
-Mild to moderate pain
-Cause GI irritation - take w/full glass of water
-Ongoing assessment for GI bleeding
Dark, tarry stools
Blood in urine
Coffee-ground emesis
What are three S/S of GI bleeding?
Avoidance of drugs while pregnant if symptoms of GI bleeding occur; Avoidance of concurrent use of alcohol, aspirin, an corticosteroids
What are two patient teachings for NSAIDs used during pregnancy?
Use of Opioids for Pain Relief During Uterine Contractions
-Decreased alertness
-Observe the pt as she cares for her newborn to ensure safety
-Assess bowel function and respirations
Topical and local agents used for perineal wounds and hemorrhoids
Witch hazel
Benzocaine
Dibucaine ointment
Hydrocortisone, pramoxine, and pramoxine hydrochloride
ducosate sodium
stool softener; promotes bowel function to relieve postpartum constipation
1. bisacodyl
2. color
3. simethicone
Clinical Judgment: Postpartum Discomfort (specifically Laxatives)
Recognize cues
Assess perineal area for wounds, hemorrhoids, and episiotomy
Generate solutions
-Pt will have bowel movement by 2-4 days postpartum
-Pt will resume bowel pattern within 4-6 weeks
Take action
-Full glass of water
-Don’t crush tablets of (1)
-No straining required
-Senna may change (2) of output
-Administer (3) after meals and at bedtime
Purpose of Drugs Used During Postpartum
-Prevent uterine atony (flabby uterus) and postpartum hemorrhage
-Relieve pain from uterine contractions, perineal wounds, and hemorrhoids
-Enhance or suppress lactation
-Manage engorgement, sore, or cracked nipples
-Promote bowel function
-Enhance immunity