vitals and measurements (part one)
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
vital signs
temperature, pulse, respirations, blood pressure, pain assessment
taken at each visit
understand the standard range of values
also completed as a baseline
body measurements
height
weight
head circumference
what are vital signs and body measurements used for?
used to evaluate health problems
temperature
determined the relationship of heat production and heat loss
most common reason for fever is infection
measurements are taken in:
degrees fahrenheit (ºF)
degrees celsius/centigrade (ºC)
normal adult oral temperature
98.6 ºF
37.0 ºC
febrile
fever (greater than 100.5)
sign of inflammation or infection
afebrile
normal temperature (98.6 - 99.1 ºF)
pyrexia
fever
hyperpyrexia
extremely high temperature
oral temperature
electronic or digital
normal is 98.6
place under tongue in one pocket just of-center in lower jaw
insure patient does not talk
wait at least 15 minutes after eating, drinking, or smoking

aural (ear) temperature
tympanic
normal is 99.6
proper technique is essential
fit in ear must be snug
adult → pull ear up and back
child → pull eat down and back

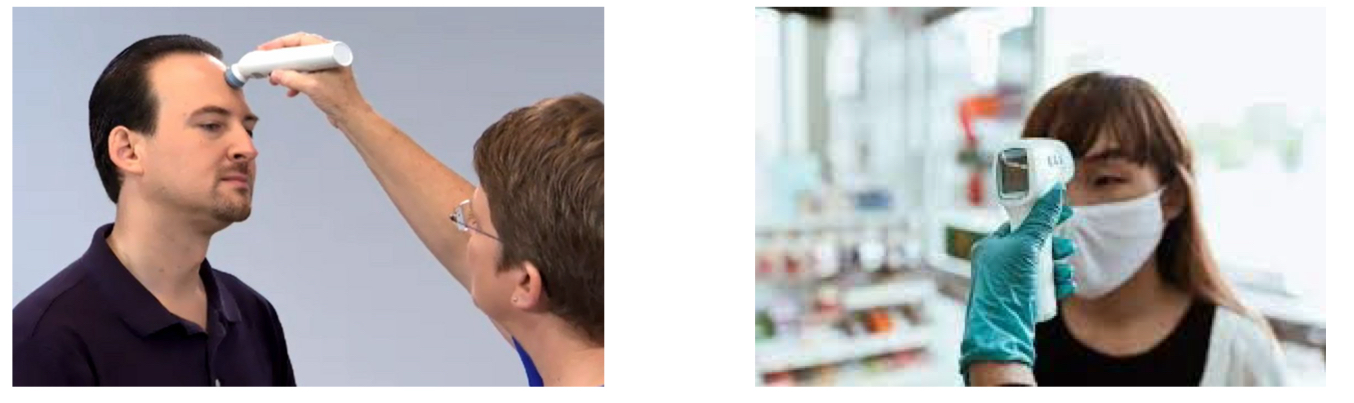
temporal temperature
temporal scanner
normal is 99.6
stroke scanner across forehead, crossing over the temporal artery
infrared thermometers (thermal) - direct laser in middle of forehead
axially (under the arm) temperature
least accurate
electronic or digital
normal is 97.6 (1 degre lower)
place tip in middle of axilla
probe must touch skin on all sides

rectal temperature
most accurate
electronic or digital
normal is 99.6 (1 degree higher)
use standard precautions
slowly and gently insert tip
use lubrication
hold thermometer in place

why and how are pulse and respirations related?
circulatory is pulse, respiratory is respirations
they are related because the heart and lungs work together
normally an increase or decrease in one causes the same effect on the other
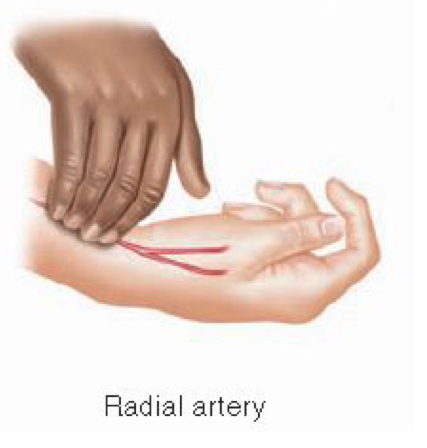
pulse
palpate artery against a bone
measure at the radial artery (most common)
count for 1 minute
may be counted for 30 seconds and multiplied by 2
if the pulse is irregular, count for 1 full minute
normal pulse
60-100 bpm
tachycardia
pulse greater than 100 bpm
fast
bradycardia
pulse less than 60 bpm
slow
what rhythms can a pulse be?
regular or irregular
what volumes can a pulse be?
weak, strong, bounding
what are the reasons for an elevated pulse rate?
fever
pain
dehydration
anxiety
infection
poor physical conditioning
what are other locations to obtain pulse besides the radial artery?
carotid
temporal
brachial
femoral
popliteal
posterior tibial
dorsalis pedis
apex of the heart (use stethescope to listen)
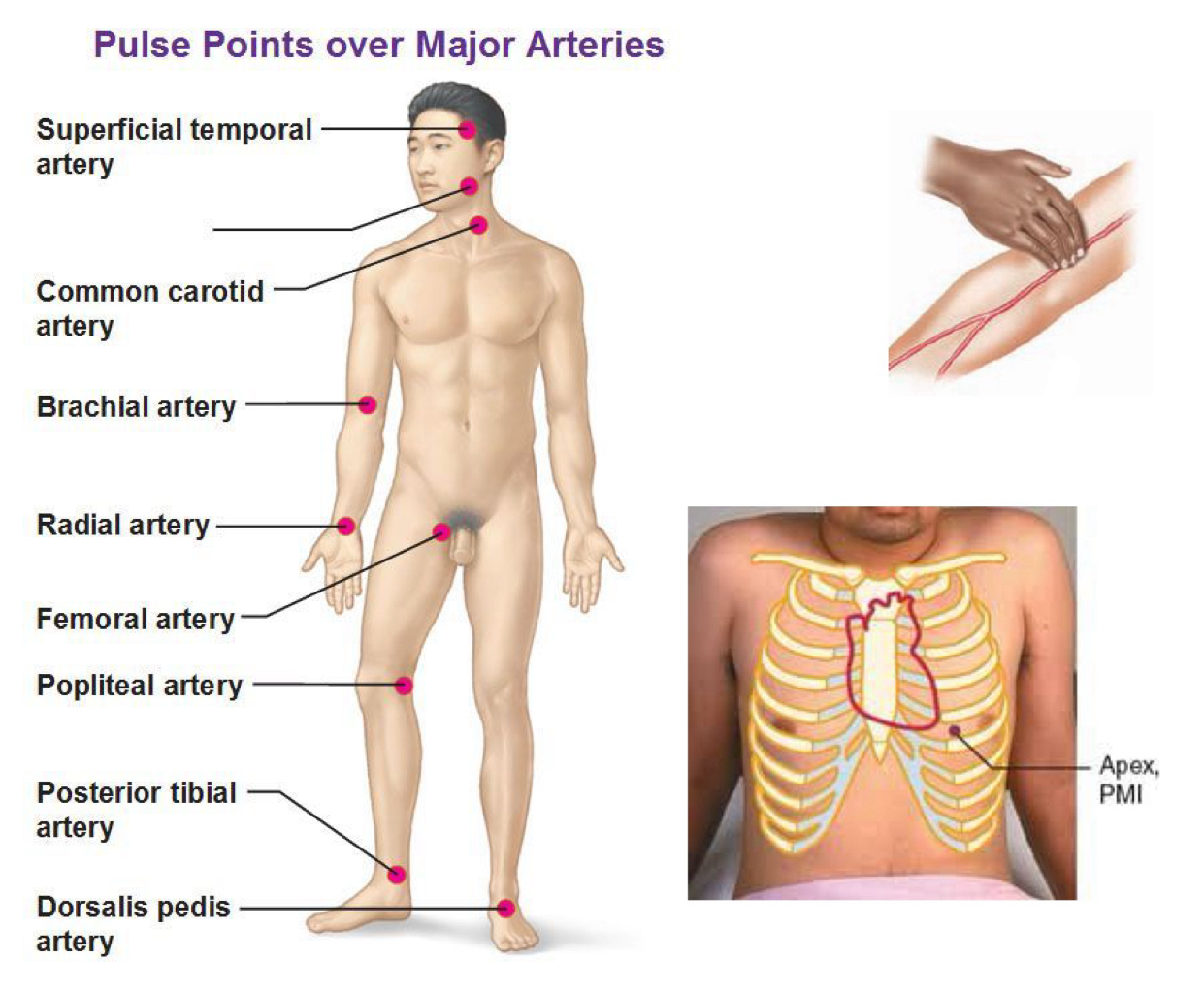
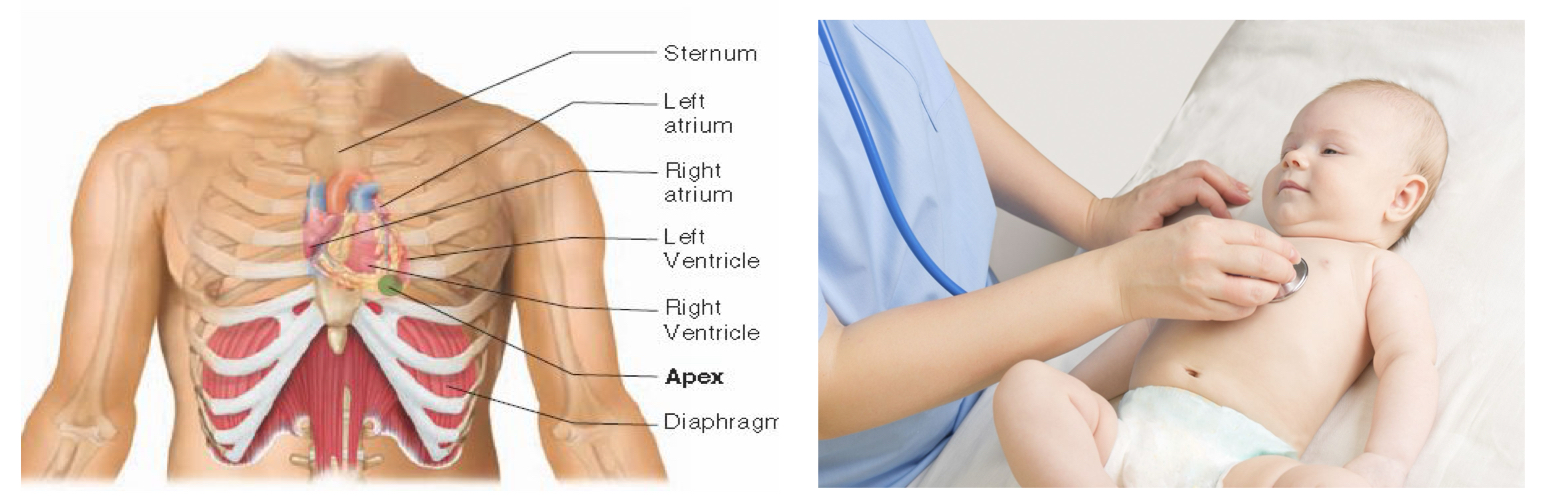
apical pulse
using a stethescope
method for obtaining pulse in an infant
the apex is located in the fifth intercostal space between the ribs on the left side of the sternum of the chest
respiratory rate
indication of how well the body provides oxygen to the tissues
check by watching chest rise and fall, listening, or feeling movement
may use stethoscope
count for one full minute and note rate and rhythm
one respiration
one inhalation and one exhalation
normal respiration rate
12-20 / minute in adults
why and how do you count respirations subtly?
once the patient is aware that respiration is being measured, they may unintentionally alter breathing
count the respirations while you have your hand on the pulse site
if using a stethoscope, tell the patient that you want to listen to their lungs
what can the quality of effort be for respiratory rate?
normal, shallow, or deep
what are the abnormal sounds found when using a stethoscope to measure respiratory rate?
wheezing
rales
rhonchi
what are the irregularities that can be found when measuring respiratory rate?
hyperventilation
dyspnea - difficult of painful breathing
tachypnea - rapid breathing
bradypnea - slow breathing
hyperpnea - abnormally rapid or labored breathing
rales
clicking or crackling sounds
fluid in the lungs
pneumonia, collapse of part or all of a lung, pulmonary edema (excess fluid in the lungs)
rhonchi
deep rattling sounds
partial obstruction of airway
asthma, acute bronchitis
apnea
period of breathing cessation
sleep apnea
periods of increasing and decreasing depth of respiration between periods of apnea
strokes, head injuries, brain tumors, congestive heart failure
blood pressure
the force at which blood is pumped against the walls of the arteries
standard unit of measurement is millimeters of mercury (mmHg)
systolic pressure
measure of pressure when left ventricle contracts
top number
first sound heard during a blood pressure reading
diastolic pressure
measure of pressure when heart relaxes
minimum pressure exerted against the artery walls at all times
bottom number
last sound heard during a blood pressure reading
normal blood pressure
less than 120/80
prehypertension
120-139 mmHg systolic
80-89 mmHg diastolic
hypertension
140/90 mmHg or more
if blood pressure reading is elevated after 2 or more visits to the physican
essential hypertension
no identifiable cause
95% of all hypertension
secondary hypertension
as a result of some other condition like kidney or heart disease
hypotension
low blood pressure
not generally a chronic health problem
slightly low blood pressure may be normal and does not usually require treatment
sphygmomanometer
blood pressure cuff and dial
inflatable cuff
pressure bulb or automatic device for inflating cuff
manometer to read the pressure
aneroid and electronic
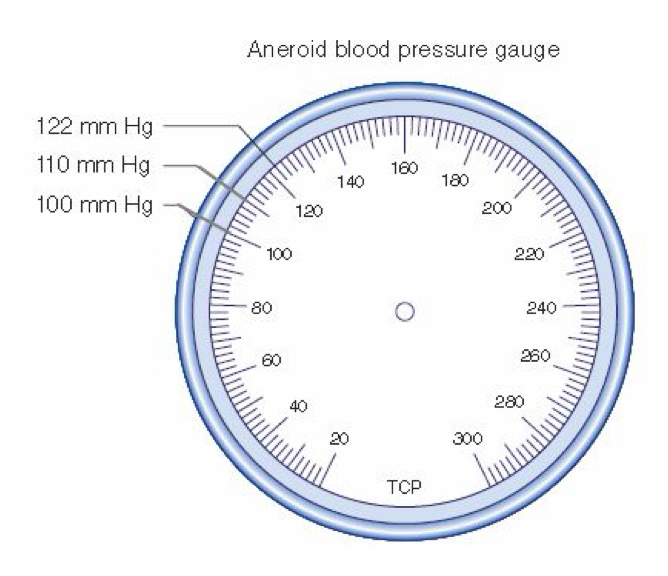
aneroid sphygmomanometers
circular gauge for registering pressure
each line 2 mmHg
requires use of a stethescope
must be calibrated to maintain accuracy
electronic sphygmomanometers
digital readout
easy to use
costly
less accurate

stethoscope
amplifies body sounds
earpieces
chest piece
diaphragm - high-pitched sounds
bell - low-pitched sounds
measuring blood pressure
place cuff on the upper arm
measured in the brachial artery
palpatory method - to determine the palpatory pressure that represents the target peak inflation
palpate the radial pulse
inflate the cuff until you can no longer feel the radial pulse
note the pressure at that point
allow the arm to rest for 1 minute or remove the cuff and replace
inflate the cuff to 30 mmHg above the palpatory result (approximately 180-200 mmHg)
place the stethoscope over the brachial pulse point
release the air in cuff and listen for sounds (the first sound is the systolic BP and the last sound is the diastolic BP)
korotkoff sounds
the five phases of sound that are heard during a blood pressure reading
phase 1: tapping sounds (systolic pressure)
phase 2: change to softer swishing sound
phase 3: resumption of a crisp tapping sound
phase 4: sound becomes muffled
phase 5: sound disappears (diastolic pressure)
what are special considerations for measuring blood pressure in adults?
allow patients to relax if the initial reading is elevated
especially for patients who are:
post exercise
ambulatory disabilities
obese
known blood pressure problems
anxiety or stress
when do you avoid measuring blood pressure in an arm?
on the same side as a mastectomy (causes lymphoedema)
with an injury or blocked artery
with an implanted device under the skin
what happens to the blood pressure if the cuff is too small?
artificially elevated
what happens to the blood pressure if the cuff is too large?
artificially low
orthostatic or postural hypotension
blood pressure drops and pulse increases as patient stands up
assess for by checking BP and pulse in three positions: lying down, sitting up, and standing
palpation
the act of touching
auscultation
listening with a stethoscope
which method gives the most accurate temperature?
temporal
oral
rectal
tympanic
rectal
how should the MA manipulate the ear to obtain a tympanic temperature on a child?
pull ear down and back
pull ear up and back
pull ear outward
pull ear up and out
pull ear down and back
when measuring an abnormal pulse or rhythm, how long should the MA count the beats?
30 seconds
1 minute
3 minutes
15 seconds
1 minute
which is the most common pulse point?
dorsalis pedis
femoral
radial
brachial
radial
why should the MA avoid telling the patient that they are counting respirations?
to prevent the patient from refusing the procedure
to avoid scaring the patient
to keep the patient from unconsciously changing their breathing rate
to help the MA count the pulse rate more accurately
to keep the patient from unconsciously changing their breathing rate
which of the following statements is true regarding a patient’s respiratory rate?
high pulse means that respiration rate is likely to be low
one breath equals one inhalation and one exhalation
the respiration rate is the number of complete breaths counted in 30 seconds
the respiration rate in females is generally faster than in males
one breath equals one inhalation and one exhalation
what do you actually measure when you take blood pressure?
the minimum amount of pressure the veins can withstand
the force with which the heart beats
the force with which blood is pumped against the arterial walls
the amount of pressure the chest exerts on the heart
the force with which blood is pumped against the arterial walls
what is the maximum expected systolic blood pressure in a healthy adult?
less than 80 mmHg
less than 120 mmHg
less than 140 mmHg
less than 100 mmHg
less than 120 mmHg
where should the cuff of the stethoscope be wrapped?
above the brachial pulse point
below the brachial pulse point
above the radial pulse point
below the radial pulse point
above the brachial pulse point
you asked your patient to roll up her sleeve so that you can check her blood pressure. however the sleeves of her blouse are too tight to roll up without the risk of cutting off circulation to the arm. what should you do?
ask the patient to change into a gown and check her blood pressure
leave the sleeve in place and check her blood pressure
roll up the sleeve anyway and check her blood pressure
explain that you cannot check her blood pressure today
ask the patient to change into a gown and check her blood pressure