PHYL 141 LECTURE EXAM
1/165
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
166 Terms
Common Properties of Cartilage:
All types of cartilage are made of chondrocytes in lacunae
lack blood vessels
have a firm flexible extracellular matrix
They are shock absorption
have a thick gel type ground substance
limited healing ability
Name the Types and Differences of Cartilage
Hyaline Cartilage, Elastic Cartilage, and Fibrocartilage
Hyaline Cartilage
Smooth matrix (collagen fibers), Stiff BUT flexible, reduces friction between bones
e.g. Synovial joints, trachea and rib tips (in connections to the sternum)
Elastic Cartilage
Has both collagen and elastic fibers (more flexible than hyaline cartilage)
Highly flexible and resilient
Provides structural support while allowing flexibility
e.g. Externa ear(pinna) and epiglottis
Fibrocartilage
Dense with bundles of collagen fibers
Tough and durable
Acts as a shock absorber and provides strong support against pressure
e.g. Intervertebral discs, menisci of knee, pubic symphysis
Give a summary of cartilage locations
Hyaline Cartilage: Joints, trachea, nose, rib-sternum
Elastic Cartilage: External ear, epiglottis
Fibrocartilage: Intervertebral discs, knee menisci,
What is the Extracellular Matrix of Bone Tissue made of
Collagen fibers (flexibility and strength for the bone to resist stretching and twisting)
Inorganic mineral Salts (Calcium, phosphate carbonate, magnesium,sodium, ad potassium)
Collagen + Ca2++ salts = Bone ECM
Name the Types of Bone Cells
Osteoblasts, Osteocytes, and Osteoclasts
Osteoblasts (BONE-FORMING—immature)
Bone-forming cells that secrete collagen and other proteins to build the bone matrix.
Key role in GROWTH AND REPAIR
Osteocytes (MATURE BONE CELLS)
Mature bone cells derived from osteoblasts, resides in lacunae within the bone matrix.
Help maintain the surrounding bone tissue.
Osteoclasts (BONE DESTROY OR RESORBS)
Resorbs or break down bone matrix
Active during BONE REMODELING, Removes damaged bone
Decreases bone desnsitybut ALLOWS FOR SHAPE ADJUSTMENTS AND CALCIUM RELEASE
Ossification
Ossification is the process by which bone tissue forms, involving either the conversion of mesenchymal tissue or cartilage into bone
What is the process of Intramembranous Ossification?
Begins in the mesenchymal tissue —> gets differentiated directly into osteoblasts that start forming a bone
What are the steps in Intramembranous Ossification
Mesenchymal cells cluster and differentiate into osteoblasts
Osteoblasts secrete bone matrix, which calcifies
Trabeculae (spongy bone) form, and surrounding mesenchyme condenses into periosteum
Compact bone eventually forms around spongy bone
Neural crest derived mesenchymal cells → osteoblasts
Process of Endochondral Ossification
Process: Cartilage is gradually replaced with bone tissue. Begins with a cartilage model, which serves as a template that is ultimately replaced by bone.
Process of Endochondral Ossification
Hyaline cartilage model forms in the shape of the future bone.
Cartilage cells die, and a bone collar forms around the model’s midsection.
Blood vessels invade, bringing osteoblasts that build bone matrix, creating the primary ossification center.
Cartilage continues to grow at the ends, but is progressively replaced by bone in the center.
Secondary ossification centers develop in the epiphyses, eventually leaving cartilage only at the articular surface and epiphyseal plate.
Examples of Bones Formed: Most long bones, such as the femur, tibia, and humerus.
Intramembranous Ossification vs. endochondral Ossification
Intramembranous Ossification:
Starts directly from mesenchymal tissue.
Forms flat bones and involves direct mineralization.
Endochondral Ossification:
Begins with a hyaline cartilage model that is replaced by bone.
Forms most bones in the body, particularly long bones.
Similarity: Both processes ultimately lead to the formation of mature bone structures capable of growth and remodeling.
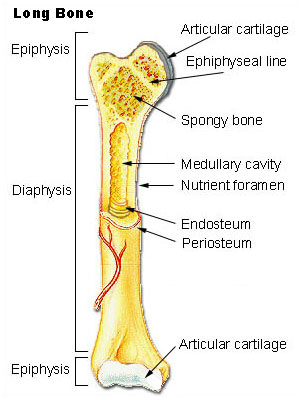
Diaphysis
The Long cylindrical shaft of the bone, primarily composed of compact bone, providing strength and support
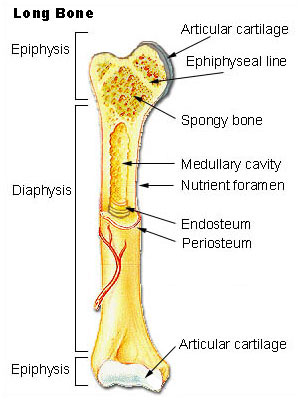
Epiphyses
The enlarged ends of the bone, containing spongy bone and red marrow, which contribute to joint formation and shock absorption
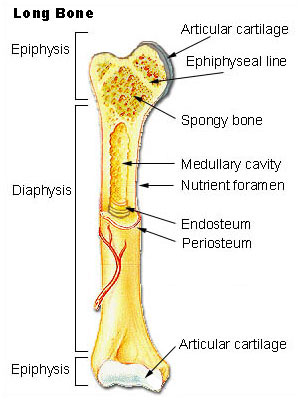
Metaphysis
The region between the diaphysis and epiphysis, containing the epiphyseal (growth) plate in growing bones
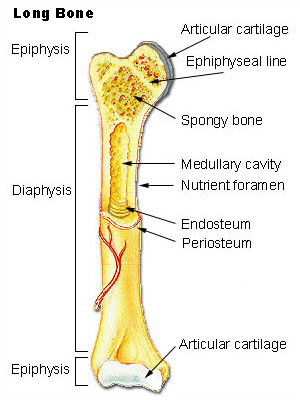
Medullary Cavity
The hollow space within the diaphysis, containing yellow marrow
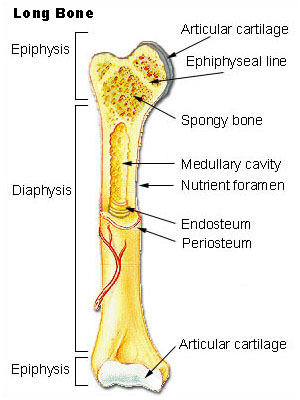
Periosteum
The outer fibrous layer covering the bone, containing blood vessels and nerves and providing attachment for tendons and ligaments
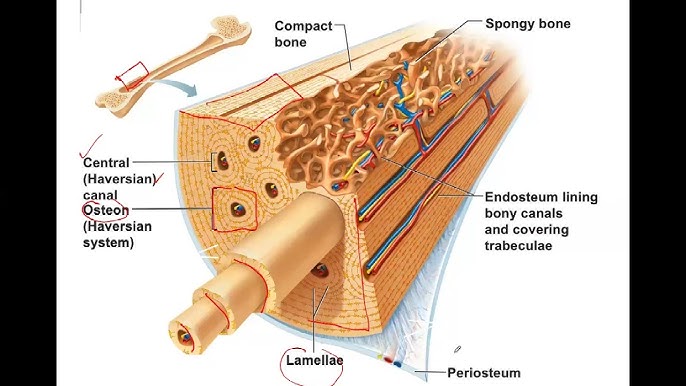
Compact Bone
Organized into osteons, or haversian system, with central canals surrounded by concentric lamellae
Contains dense, tightly packed bone matrix, providing high strength and protection.
Found primarily in the diaphysis of long bones.
Spongy bone
Composed of a lattice-like network of trabeculae, which are thin plates of bone.
Less dense and lighter than compact bone, allowing space for bone marrow.
Found mainly in the epiphyses of long bones and in the interior of other bones.
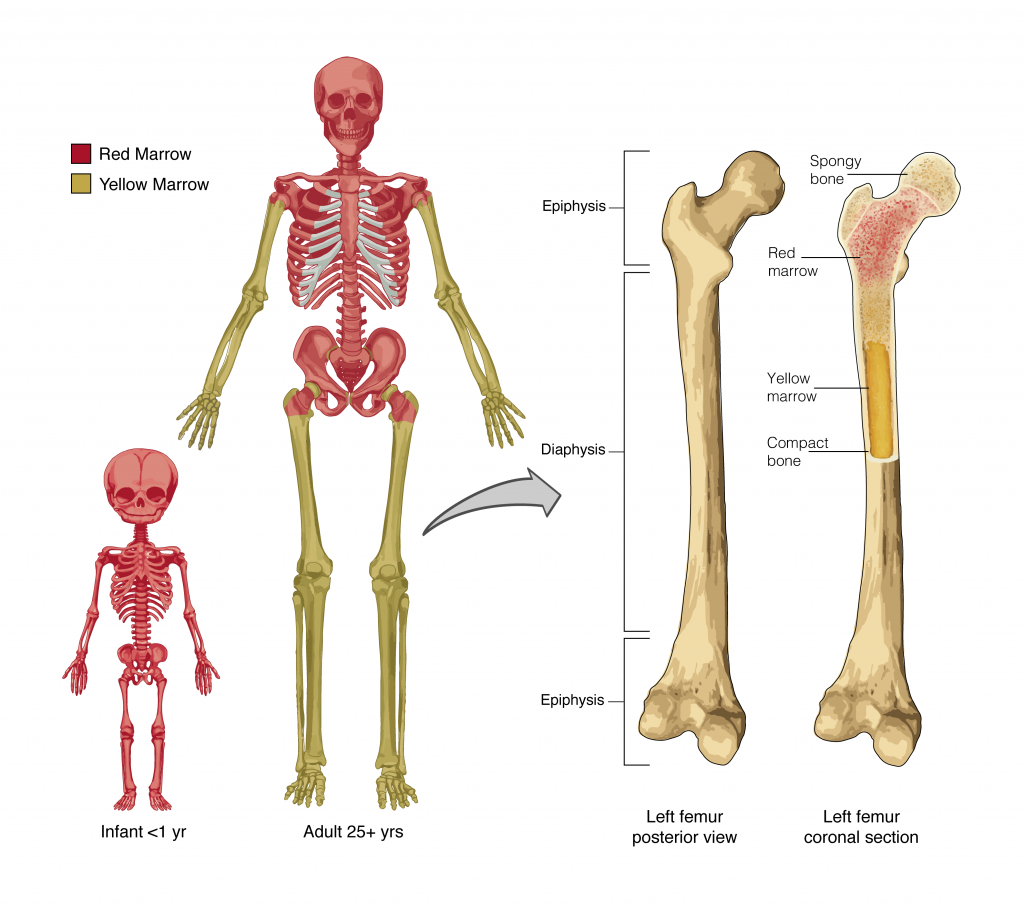
Red Bone Marrow
Found primarily in the flat bones (skull, ribs, pelvis) and in the epiphyses of long bones IN CHILDREN. Adults have it more tot he flat bones and ends of long bones
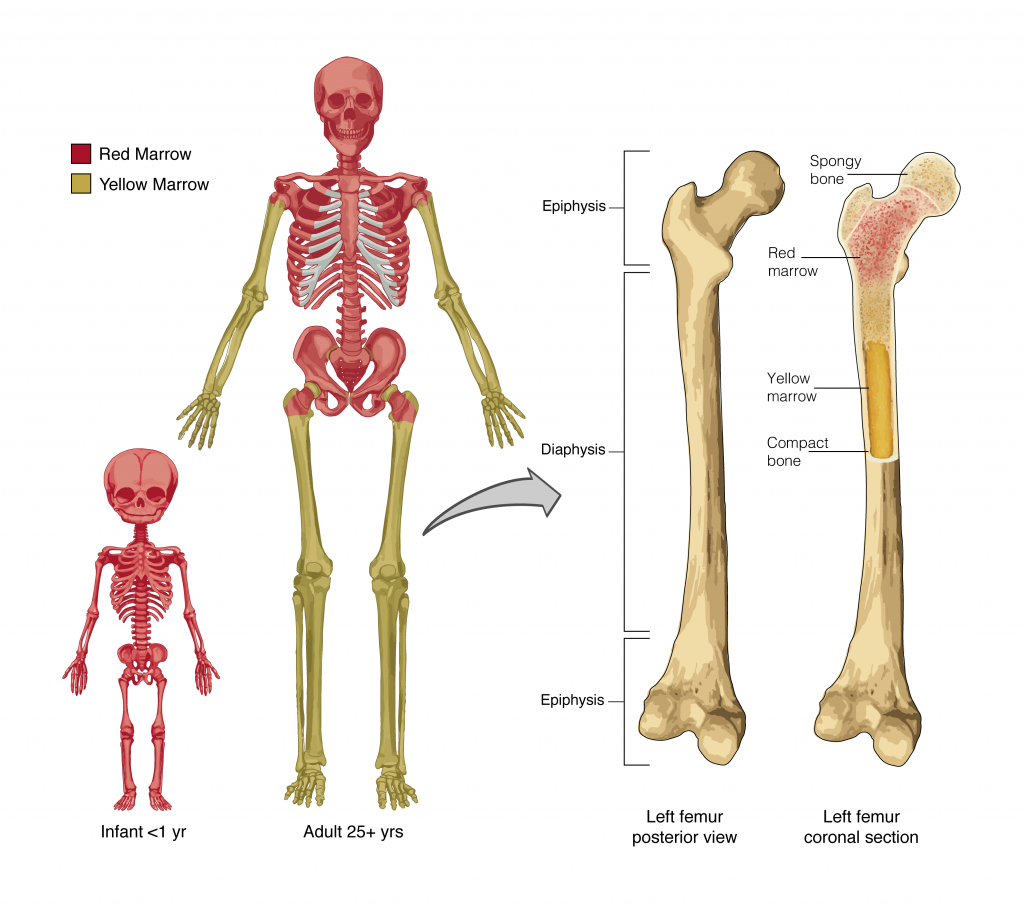
Yellow Bone Marrow
Occupies the medullary cavity in the diaphysis of long bones in adults and primarily stores fat. Red marrow gradually converts to yellow marrow with age.
What are the cells in Red Bone marrow and what do they do?
Hematopoietic Stem Cells— Give rise to red blood cells, white blood cells, and platelets, which are crucial for oxygen transport, immune function, and blood clotting.
What are cells in the Yellow Bone Marrow and their function?
Adipocytes (Fat cells)— Store fat as an energy reserve for the body. Yellow marrow can revert to red marrow if necessary (e.g., in severe blood loss).
Epiphyseal (Growth) Plates and their growths
Interstitial Growth and Appositional Growth
Interstitial Growth (Lengthwise)
Occurs at the epiphyseal plates, where cartilage expands and is replaced by bone, contributing to bone lengthening.
Appositional Growth (Width)
Bone tissue is added to the outer surface of the bone, increasing its diameter and thickness, which strengthens and widens the bone.
Epiphyseal Plates in Long Bones
Location: Found between the epiphysis and metaphysis of long bones.
Role in Growth: They contain layers of cartilage where new cells proliferate and expand, pushing the epiphysis outward and contributing to lengthwise growth until maturity.
The Process of the Epiphyseal closure
Description: During adolescence, hormones signal the slowing of cartilage production and increase in bone formation, causing the epiphyseal plates to gradually ossify.
Effect: Once the plates fully ossify (close), they become epiphyseal lines, and lengthwise bone growth ceases. This marks the end of height increase in adulthood.
List the vitamins needed for Bone Growth
Vitamin D, B12, C, K
How does Vitamin D Contribute to Bone Growth
Essential for calcium absorption in the intestines and maintaining calcium and phosphate levels for bone mineralization. It helps to prevent conditions like rickets in children and osteomalacia in adults.
Found in: Exposure to SUN
How does Vitamin C Contribute to Bone Growth
Vital for collagen synthesis, which is a major component of the bone matrix. Collagen provides the structural framework that gives bones flexibility and strength.
Found in: Oranges, lemons (citrus fruits)
How does Vitamin K Contribute to Bone Growth
Plays a role in bone mineralization by helping in the formation of osteocalcin, a protein involved in binding calcium to the bone matrix, enhancing bone density.
Found in: Leafy Greens
How does Vitamin B12 Contribute to Bone Growth
Contributes to bone-building processes by supporting osteoblast activity and helps reduce bone loss. It’s important for DNA synthesis, which aids in the production of bone cells.
Found in: Meat, fish, dairy..
Hormonal Regulation of Skeletal growth
During growth and development, several hormones work together to regulate bone growth and density
Growth Hormone, Thyroxine, Estrogen, Androgen
Growth Hormone (GH)
Stimulates overall bone growth by promoting the formation of new bone tissue. It acts on the liver to produce insulin-like growth factor-1 (IGF-1), which directly stimulates cartilage and bone growth at the epiphyseal plates.
Thyroid Hormones (T3 and T4(thyroxine)
Regulate the body’s metabolic rate, which includes influencing bone growth and maturation
Estrogen and Androgen
Estrogen: Promotes bone formation and helps in maintaining bone density, playing a key role in closing epiphyseal plates, which stops longitudinal bone growth. Estrogen also protects against excessive bone resorption, which is why low estrogen levels in postmenopausal women increase osteoporosis risk.
Androgen: Promotes the growth of bone mass and density, particularly during the adolescent growth spurt, contributing to the development of stronger and larger bones.
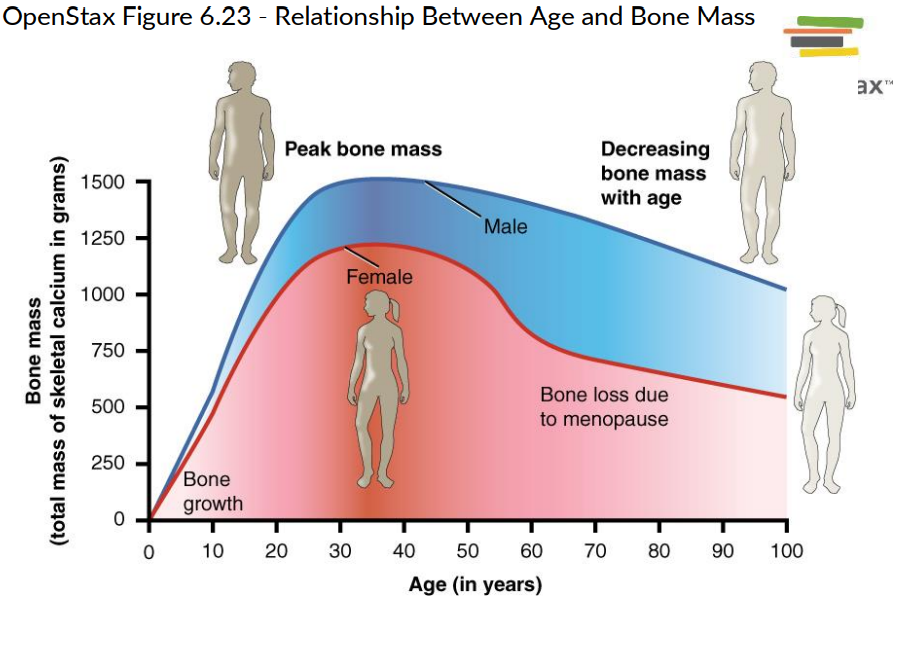
Effect of Hormones on Bone density and Structure as people age:
Adolescence: High levels of growth hormone, IGF-1, and sex hormones stimulate bone growth.
Adulthood: Hormone levels stabilize, and bone remodeling continues under the influence of parathyroid hormone (PTH), calcitriol, and other factors to maintain bone strength.
Aging: Decreases in sex hormones (especially estrogen in women after menopause) lead to increased bone resorption, reduced bone density, and a higher risk of osteoporosis. Aging also reduces growth hormone and IGF-1 levels, further slowing bone formation.
Parathyroid Hormone (PTH)
Released by the parathyroid glands when blood calcium levels are low.
Stimulates osteoclast activity to increase bone resorption, releasing calcium into the bloodstream.
Enhances calcium reabsorption in the kidneys and stimulates calcitriol production in the kidneys to boost intestinal calcium absorption
Calcitrol (Active Vitamin D)
Increases blood calcium levels by promoting calcium absorption from the intestines.
Works with PTH to mobilize calcium from bones when needed.
Calcitonin
Secreted by the thyroid gland when blood calcium levels are high.
Inhibits osteoclast activity, reducing bone resorption, which helps lower blood calcium levels.
Name all Bone classifications on shape
Long Bones, Short Bones, Flat Bone, Irregular bones, Sesamoid Bones
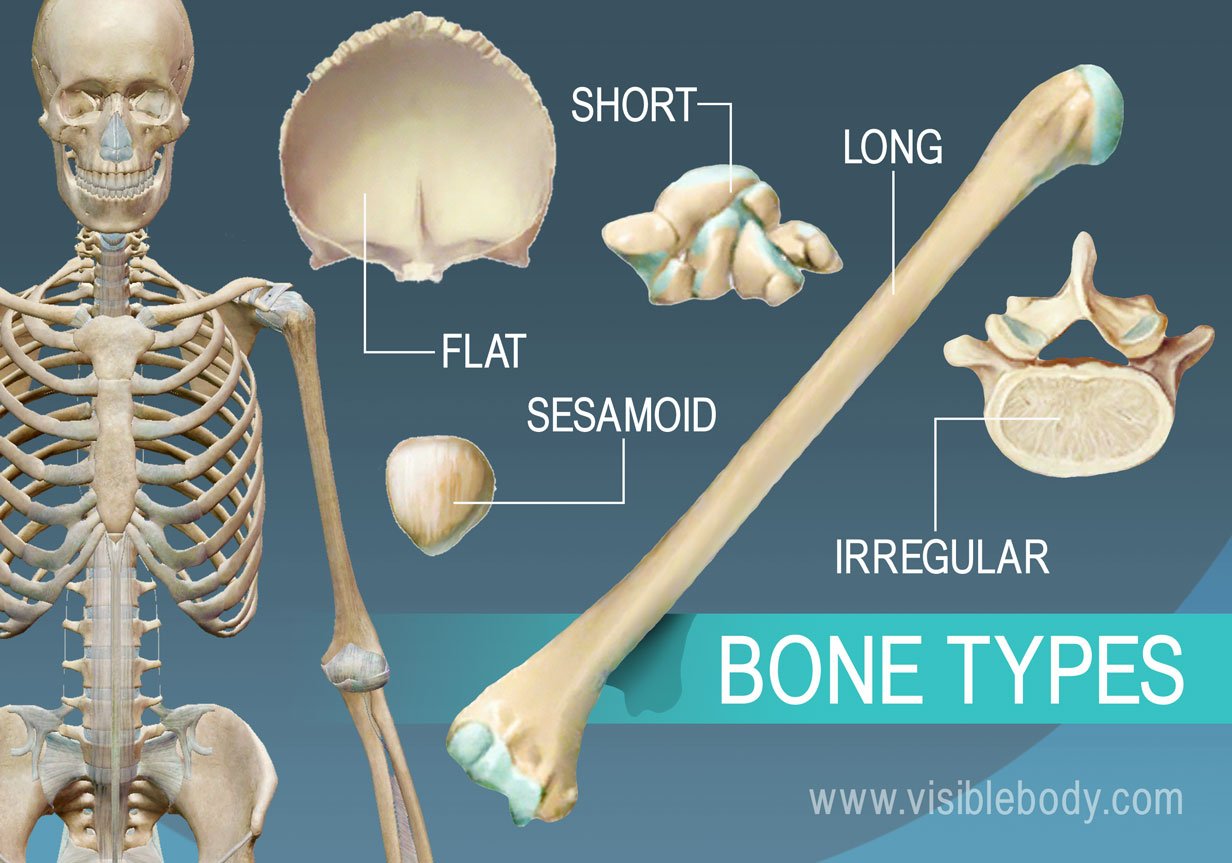
Long bones
femur, humerus
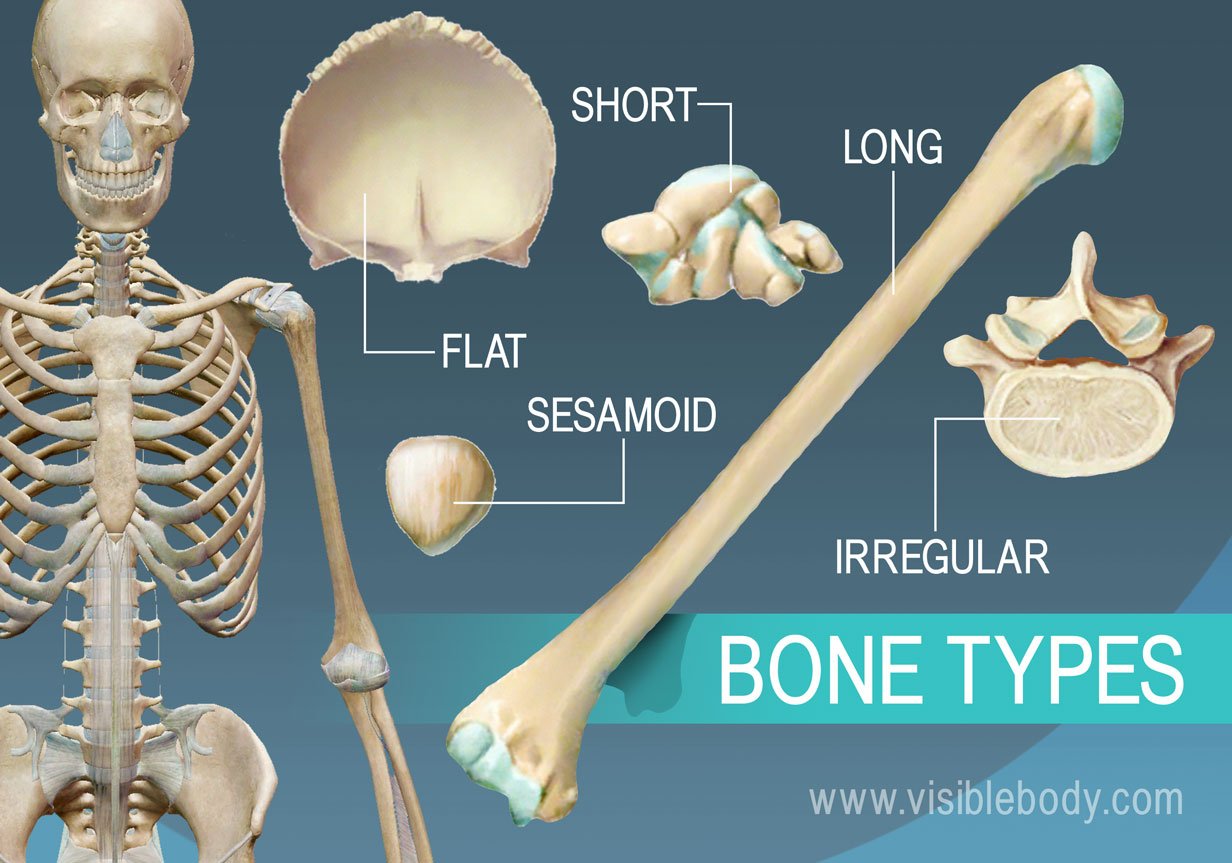
Short Bones
carpals, tarsals
Flat bones
Skull bones, sternum
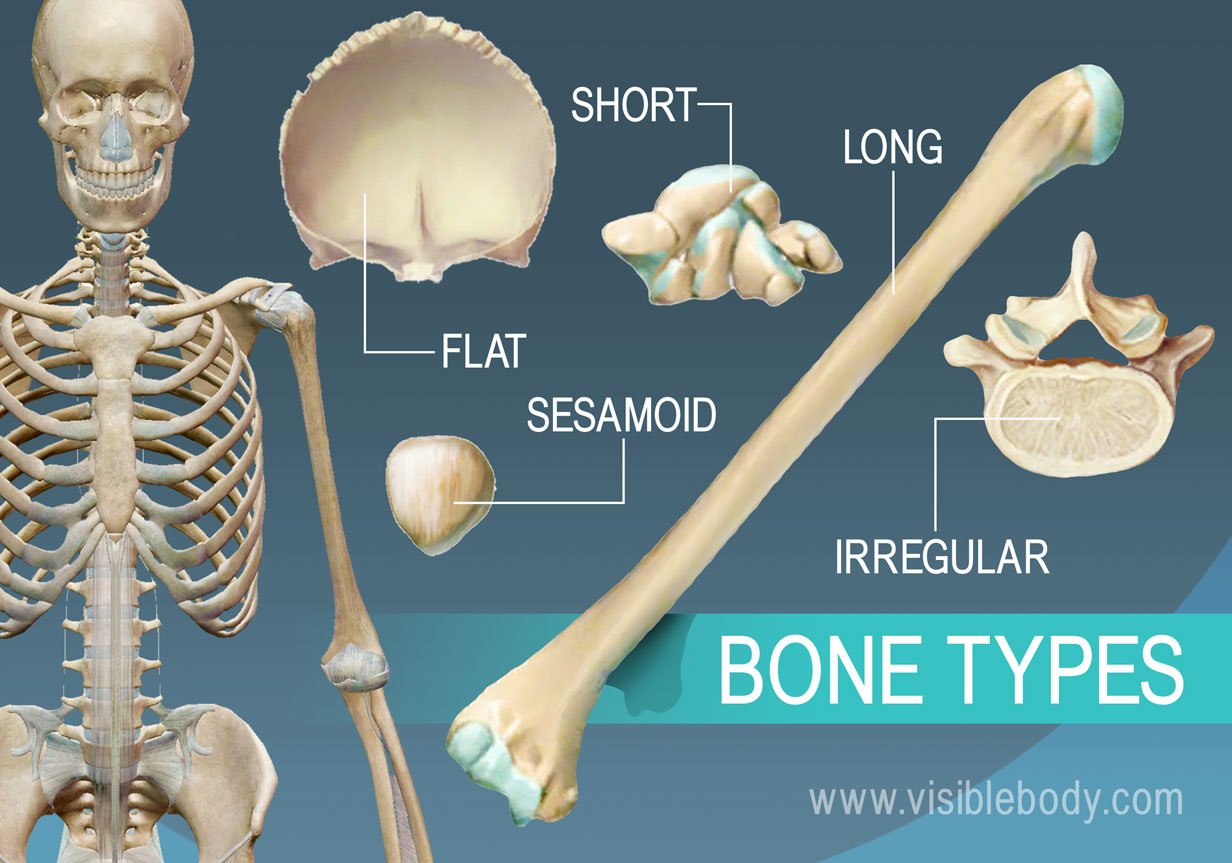
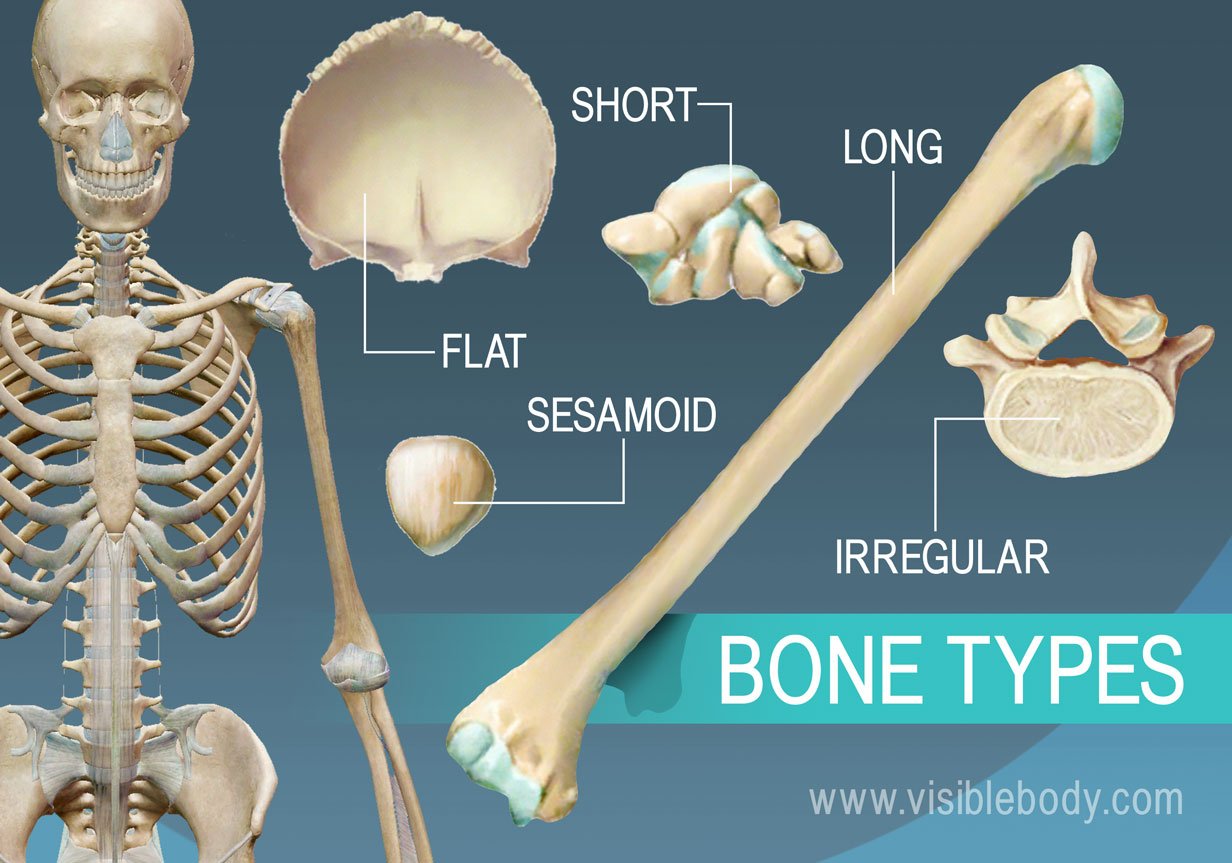
irregular bones
vertebrae, pelvis
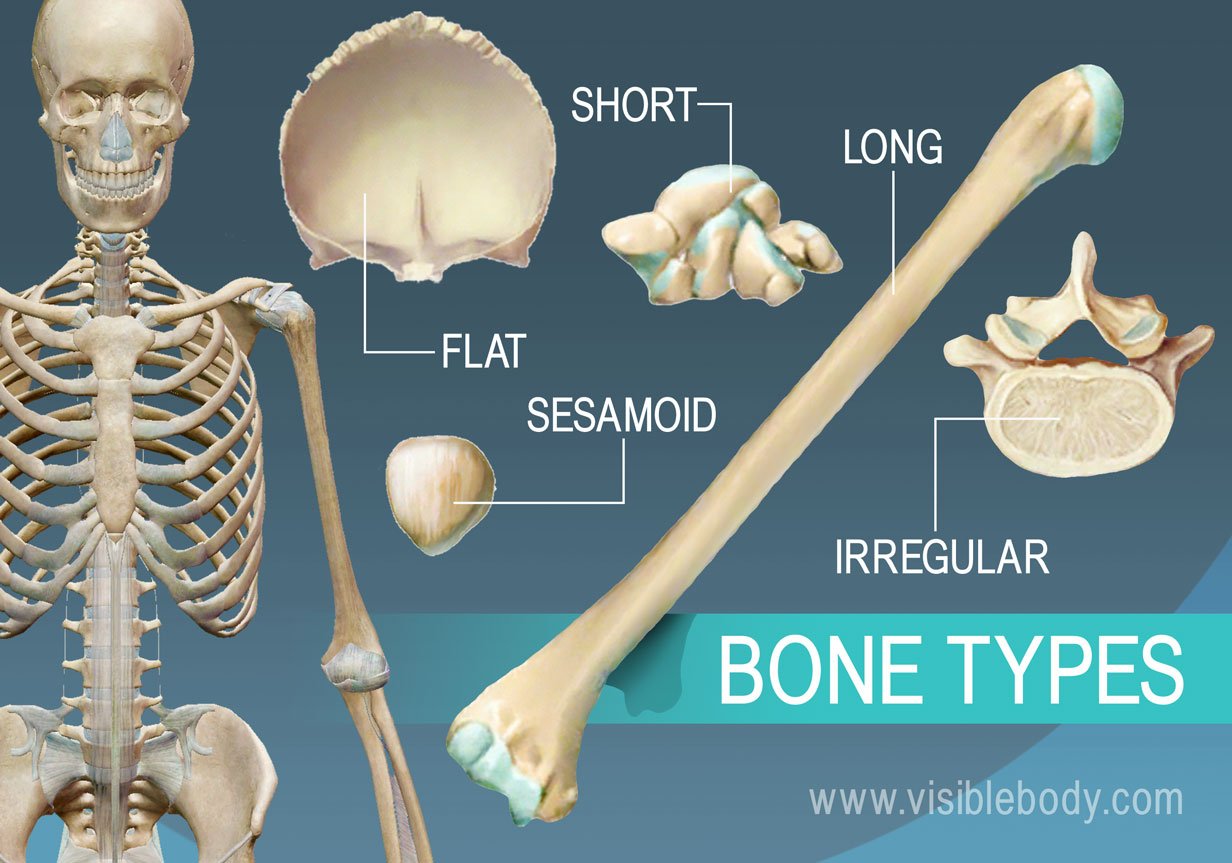
Sesamoid bones
patella
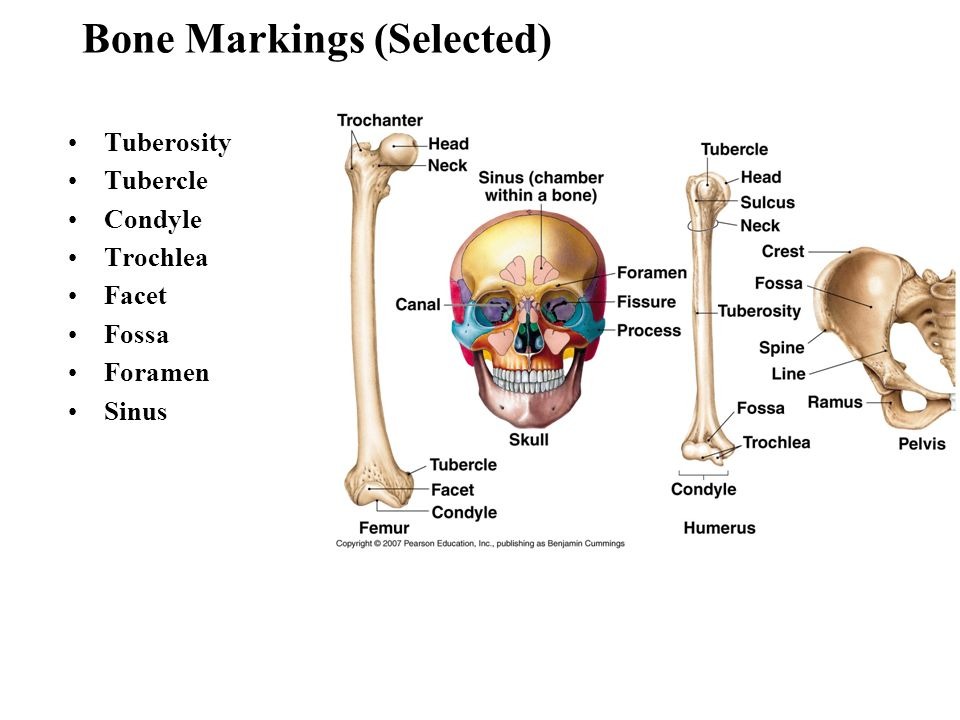
Condyle
A rounded, knuckle-like prominence often involved in forming joints (e.g., femoral condyle)
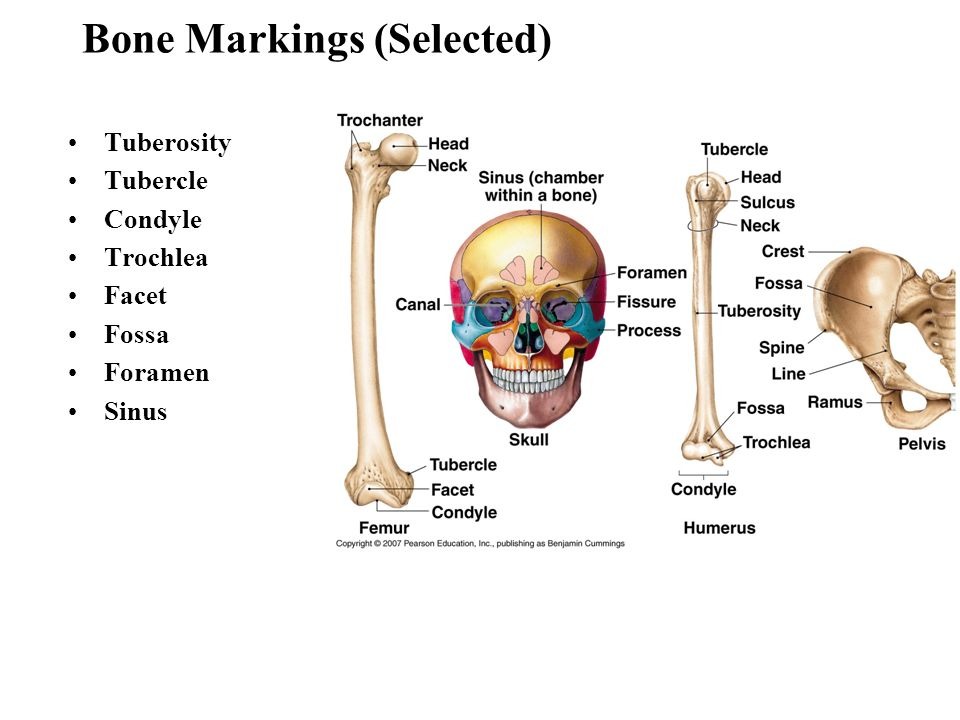
Tubercle
A small, rounded projection for muscle or ligament attachment (e.g., greater tubercle of the humerus).
Foramen
A hole or opening in a bone that allows passage of nerves and blood vessels (e.g., foramen magnum in the skull).
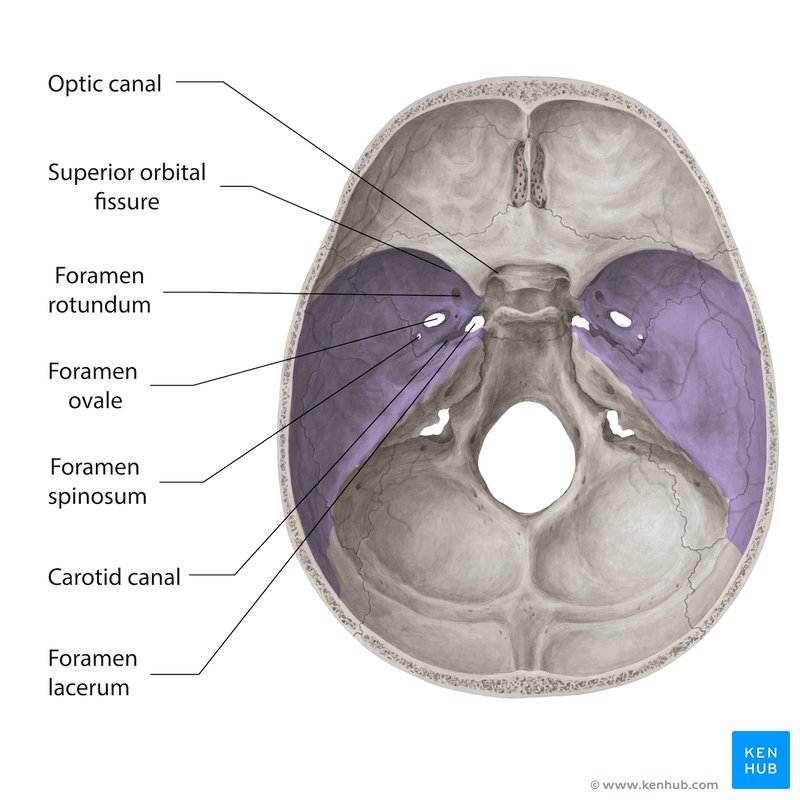
Canal
A tubular passage or tunnel in a bone (e.g., auditory canal in the skull).
name some of the Locations and Major Structures of the Axial Skeleton
The Skull, (protects the brain), Vertebral Column (supports the body’s weight and protects spinal cord), Thoracic Cage (rib cage)— protects the heart and lungs.
What are the articulation points for upper and lower limps with the axial skeleton?
The Upper limbs: Clavicles and Scapulae (shoulder girdle) allows for arm attachments
Lower Limbs: Pelvic girdle connects to axial skeleton at sacrum allowing for Leg attachment
name 8 Cranial bones
Frontal, Parietal x2, occipital, temporal x2, sphenoid, and ethmoid
Name the major sutural bones
Coronal Suture, Sagittal suture, Lambdoid Suture, Squamous Suture
Fontanelles
Soft, membranous gaps between cranial bones IN INFANTS— allows for skull flexibility during birth and brain growth. They ossify ad form the sutures we know that form the adult skull.
Name the facial bones
Nasal bones maxillae, zygomatic bones, mandible, lacrimal bones, palatine bones, inferior conchae, nasal conchae and vomer
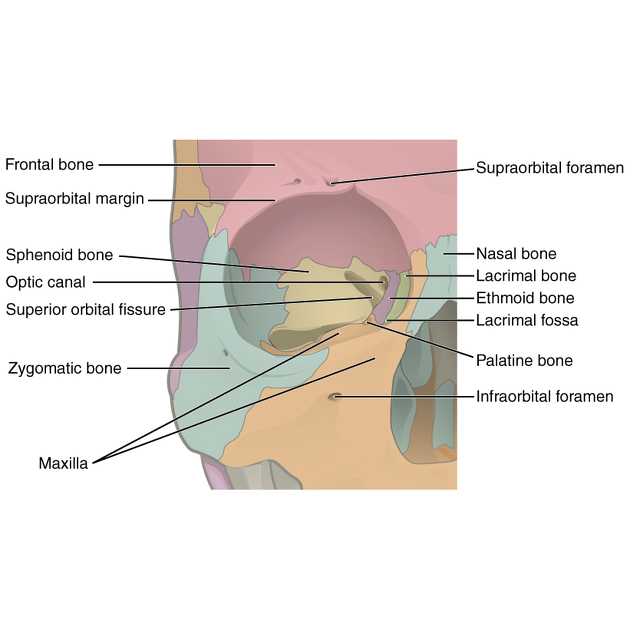
Name bones in the Orbital Complex Structure
Frontal, sphenoid, ethmoid, maxila, lacrimal, zygomatic, and paatine bones
Now name some of the bones in the Nasal Complex Structure
ethmoid, maxilla, nasal, palatine, and inferior nasal conchae bones, creating the nasal cavity structure
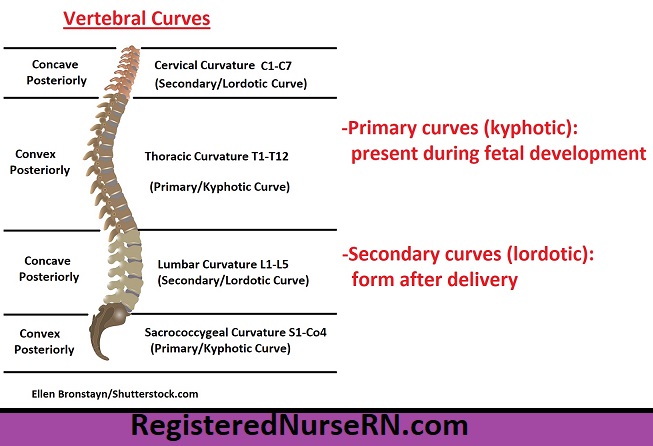
Primary Curvatures (Vertebral Column Curvatures)
Present from birth and include the thoracic and sacral curves (KYPHOTIC). They are concave anteriorly, which provides space for organs in the thoracic and pelvic cavities.
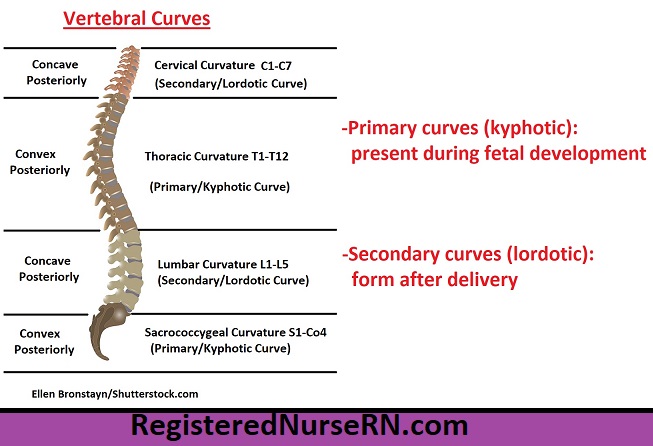
Secondary curvature (Lordotic)
Develop after birth and include the cervical and lumbar curves. The cervical curvature develops as the infant begins to hold up their head, and the lumbar curvature develops when the child begins to stand and walk. These curves are convex anteriorly, aiding in balance and posture
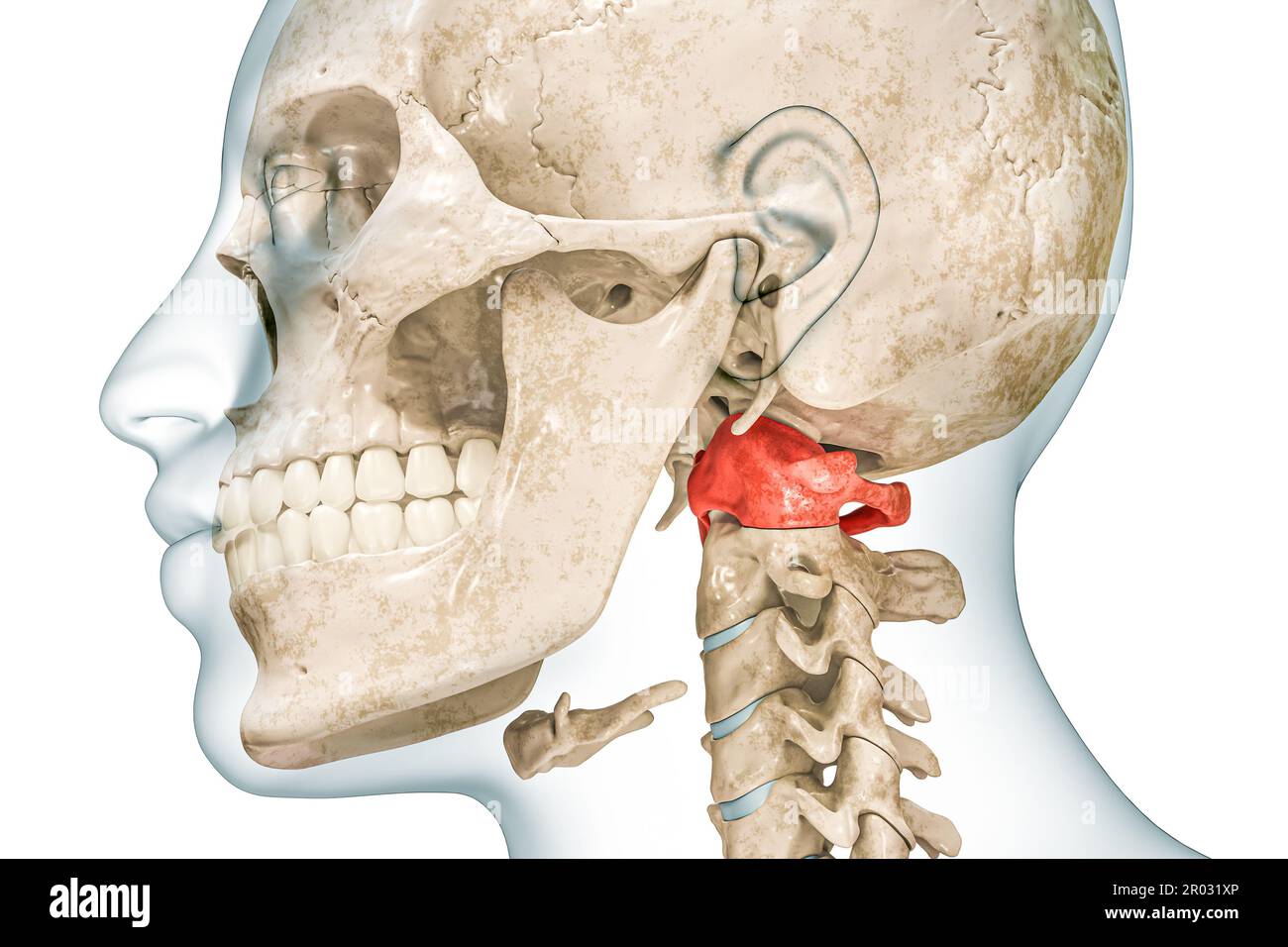
Atlas Bone
Allows for the head to nod “yes”
Permits flexion and extension of the head.

Synarthrosis
immovable joints, provides stability and protection
e.g. Skull sutures, tooth sockets (gomphoses)

Amphiarthrosis
Slight movement — offers balance between stability and mobility
e.g intervertebral discs in spine and pubic symphysis

Diarthrosis
Freely movable joints= wide range of motion
e.g. synovial joints-shoulder, hip joints
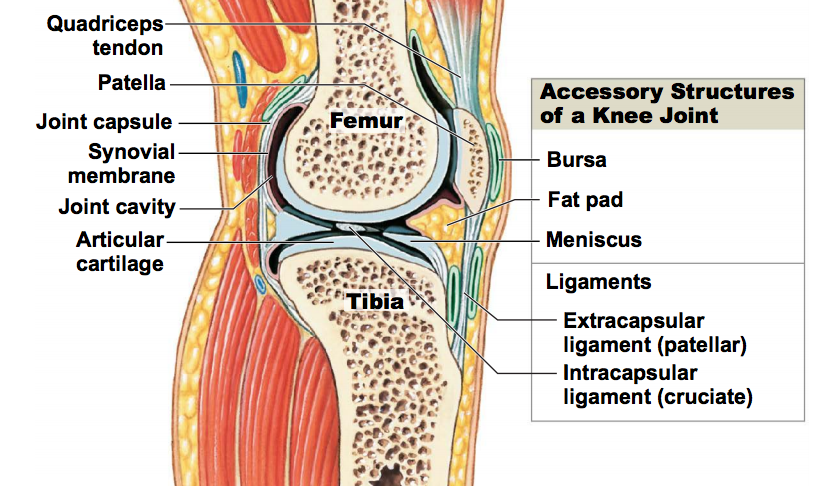
Name the structural components of a synovial joint
Articular cartilage—ends of the bones, reduce friction and absorbs shock
Joint (synovial) cavity—fluid filled space between articulating bones
Synovial membrane — lines the inner surface of the joint capsule and secrets fluid for lubrication
Synovial fluid—fills the joint cavity to reduce friction + provide nutrients to the articular cartilage
Joint capsule—Fibrous capsule, providing stability and protection
Ligaments— Bands ofconnective tissue, reinforces joint capsule and stabilizes the joint
Bursae— Fluid filed sacs that reduce friction between tendons and bones
Tendon— Connects muscle to bone
Fat pads- Cushion for the joint and is shock absorbing
Name structure types of synovial joints
Plane (gliding) joints
Hinge joints
Condylar (condyloid) joints
Saddle Joints
Pivot joints
Ball and Socket Joints
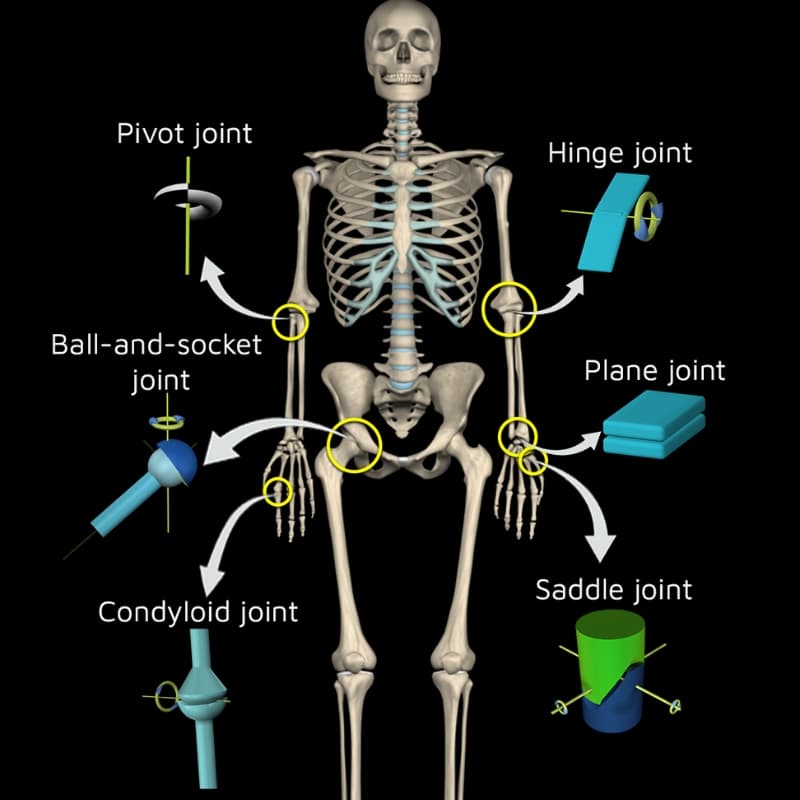
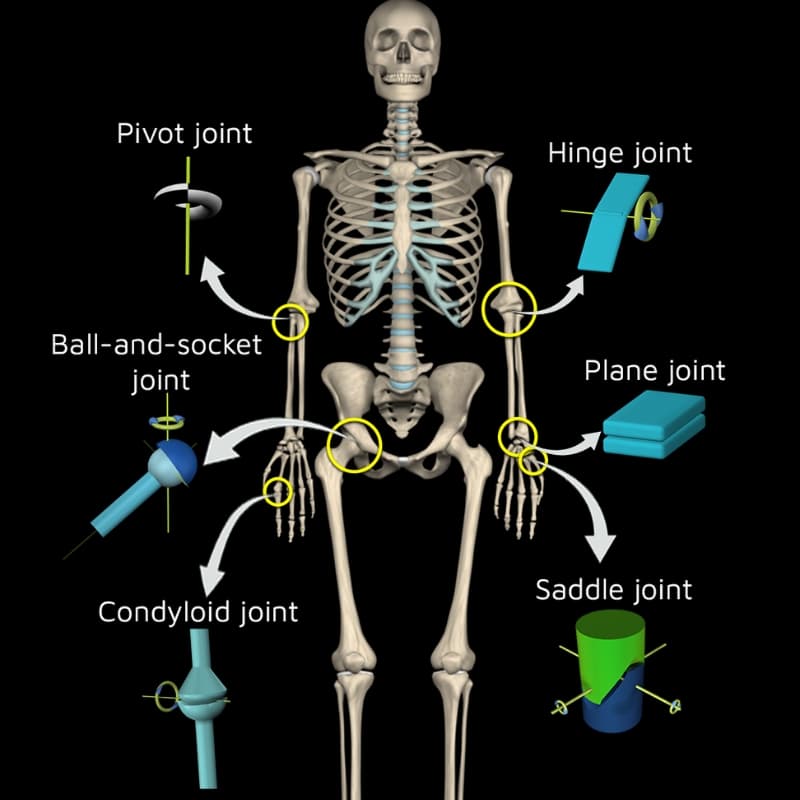
Plane (Gliding Joints:
Example: Intercarpal joints of the wrist.
Articulation: Flat surfaces slide over one another.
Movement: Allows gliding or sliding movements, usually nonaxial.
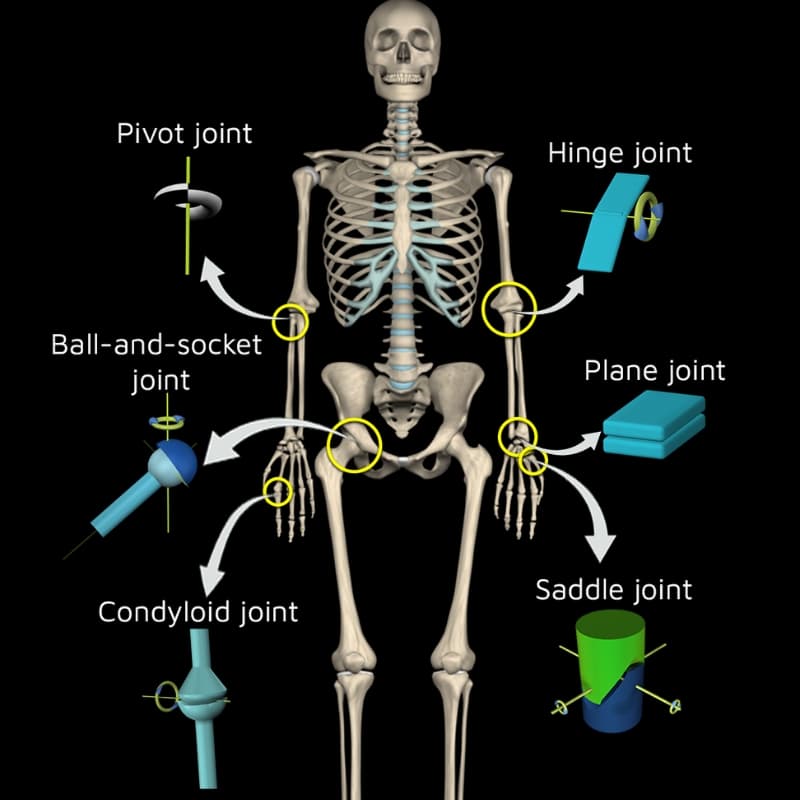
Hinge Joints
Example: Elbow joint.
Articulation: A convex bone end fits into a concave end.
Movement: Allows flexion and extension, monaxial movement.
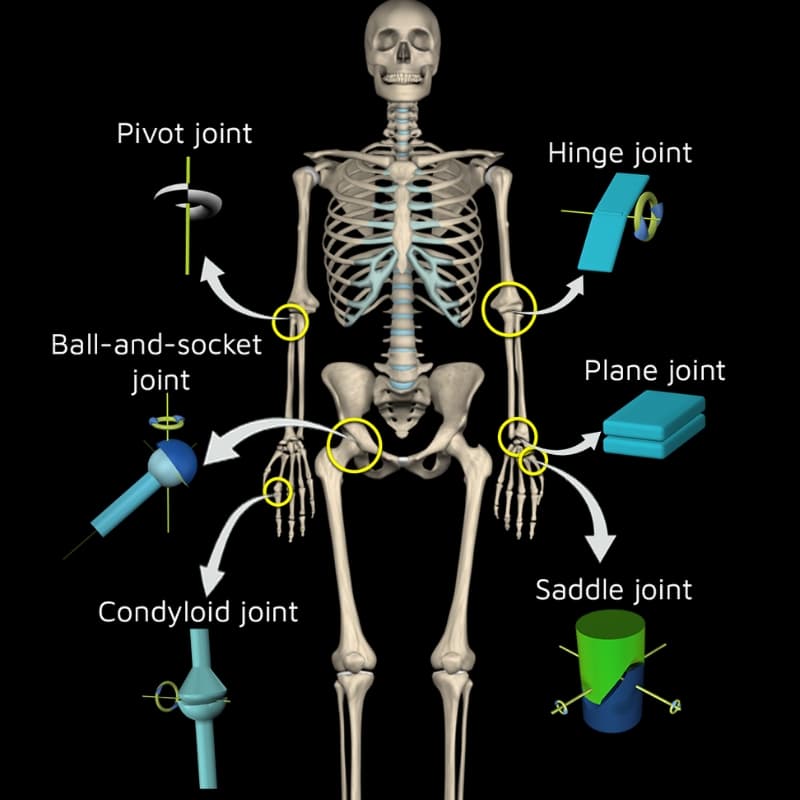
Condylar (Condyloid Joints)
Example: Knuckle (metacarpophalangeal) joints.
Articulation: An oval-shaped end of one bone fits into a concave end.
Movement: Biaxial, permitting flexion-extension and abduction-adduction.
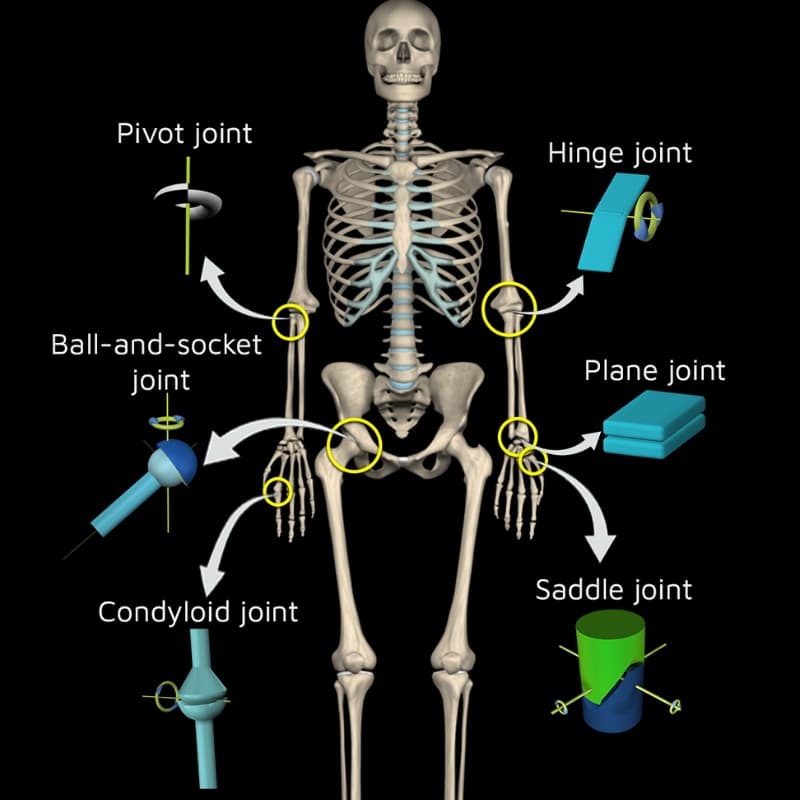
Saddle joints
Example: Thumb carpometacarpal joint.
Articulation: Both bone surfaces are concave and convex.
Movement: Biaxial, allowing flexion-extension and abduction-adduction.
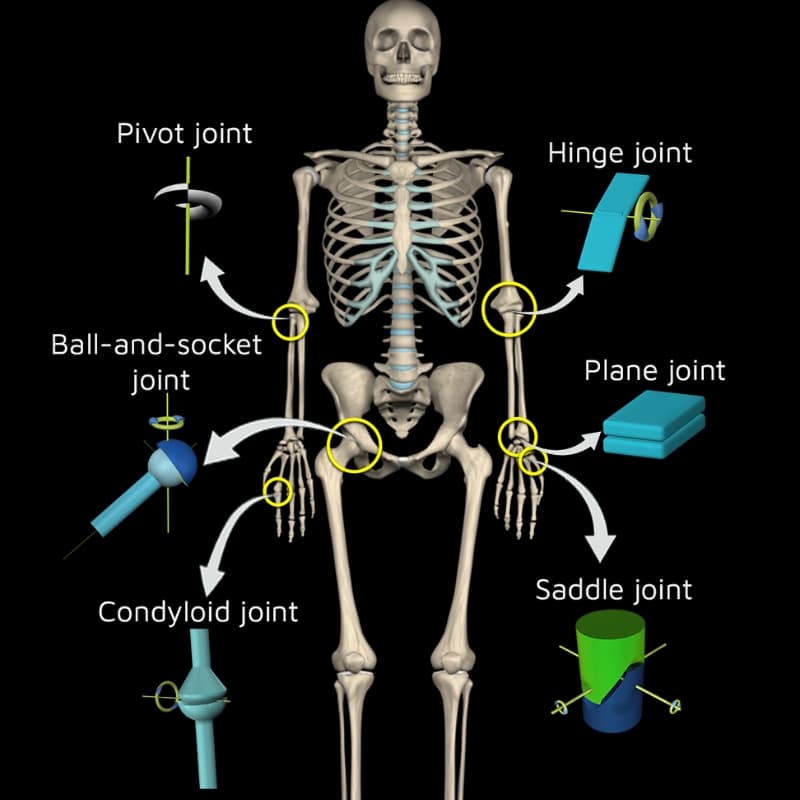
Pivot Joints
Example: Atlantoaxial joint (between C1 and C2 vertebrae).
Articulation: A rounded end fits into a ring-like structure.
Movement: Monaxial, allowing rotational movement.
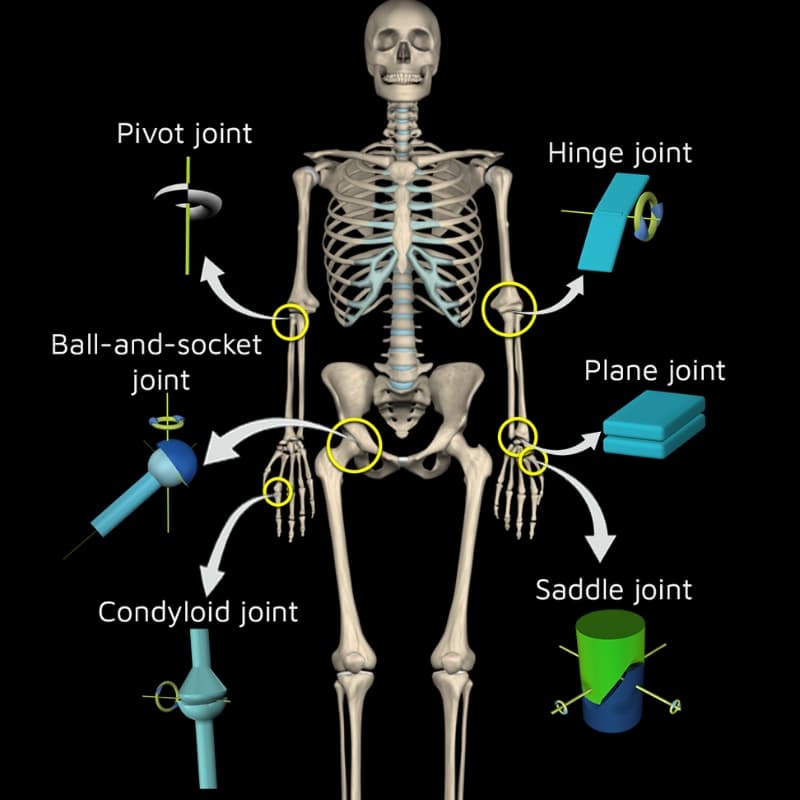
Ball and Socket Joints
Example: Shoulder and hip joints.
Articulation: A spherical end fits into a cup-like cavity.
Movement: Triaxial, allowing flexion-extension, abduction-adduction, and rotation
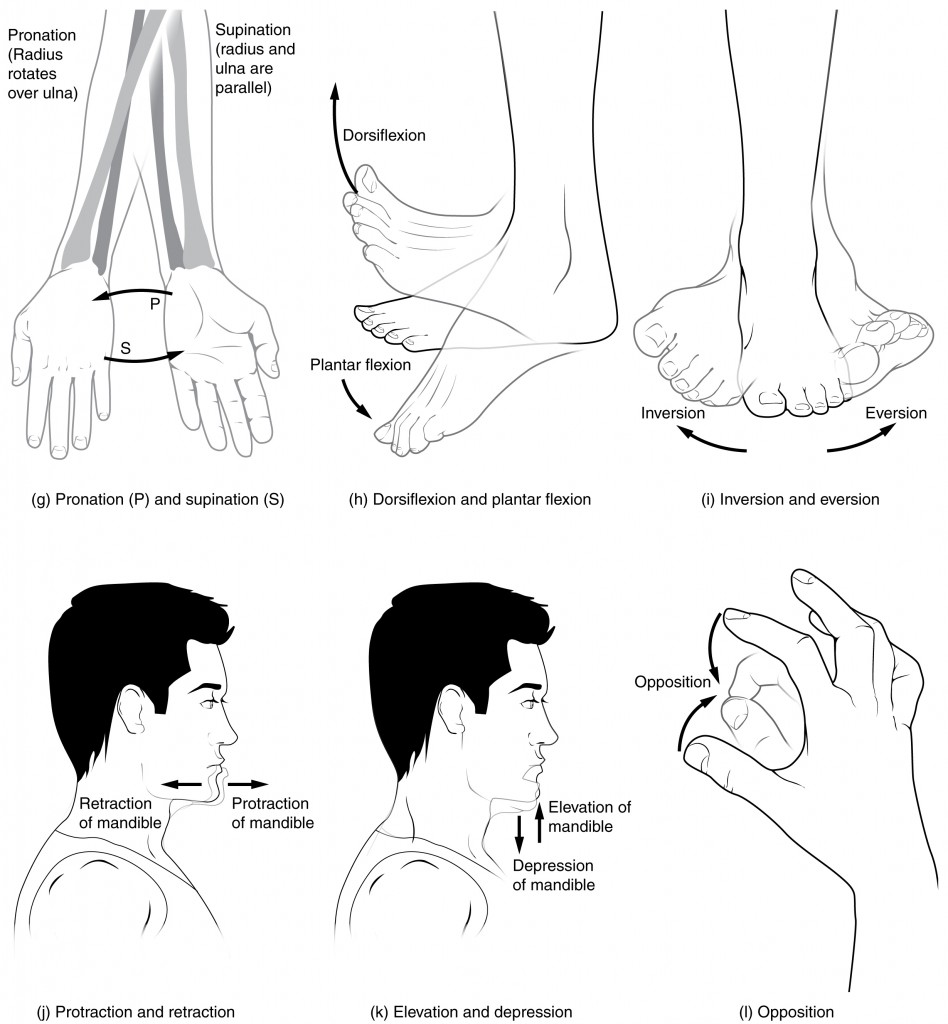
Types of Movement — Axial Classification
Monoaxial— angular movement in ONE PLACE (flexion, extension (elbow))hinge and pivot joints
Biaxial— Movements in TWO PLANES (condyloid and saddle) (fingers moving)
Triaxial- movements in 3 axes and MULTIPLE DIRECTIONS — think shoulder and hip joints
Atlanto-occipital joint (Skull and C1)
joint connects the occipital bone of the skull to the atlas (C1) vertebra. It allows for flexion and extension of the head (nodding "yes")
Atlantoaxial Joint C1 and C2
This joint connects the atlas (C1) and axis (C2) vertebrae, enabling head rotation (shaking "no").
Structure: The dens (odontoid process) of the axis fits into the atlas, forming a pivot joint that allows rotational movement.
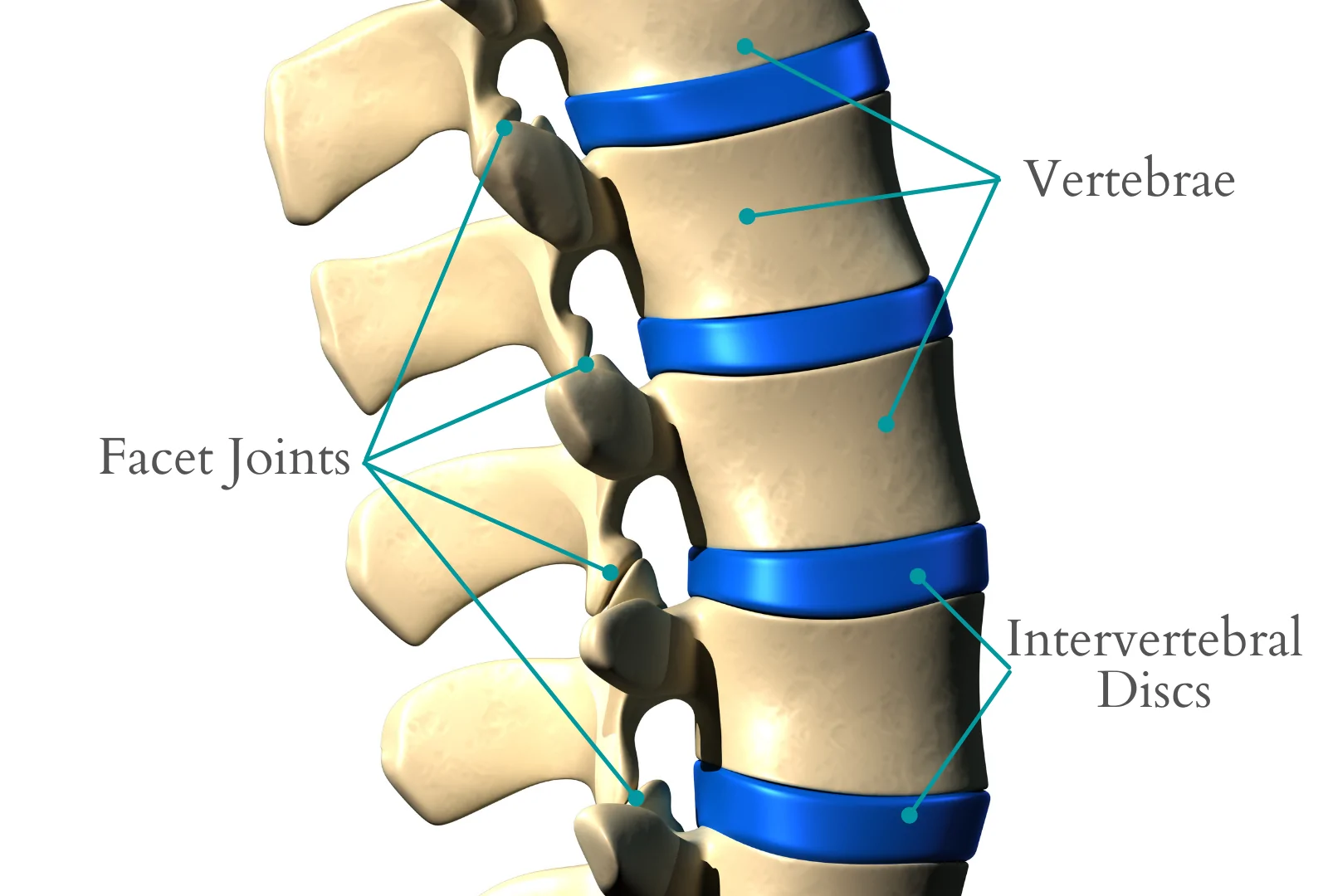
Typical Intervertebral Joints C3 to L5
Structure: Each vertebra from C3 to L5 articulates with adjacent vertebrae at intervertebral joints, which include two main components
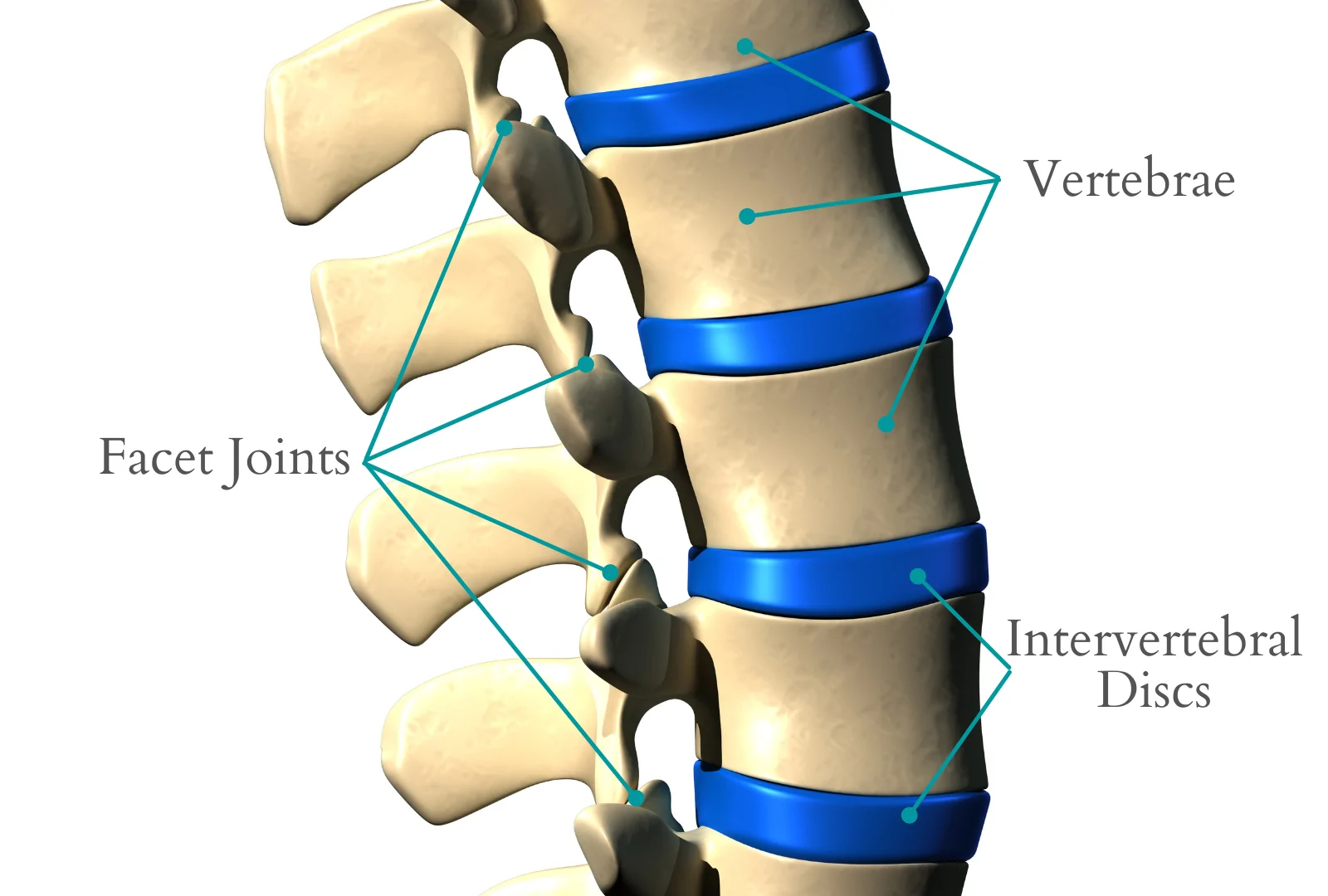
Intervertebral Discs
Located between vertebral bodies, these provide cushioning and flexibilit
Facet (zygapophyseal) Joints
Synovial joints between the articular processes of adjacent vertebrae, allowing controlled movement and flexibility.
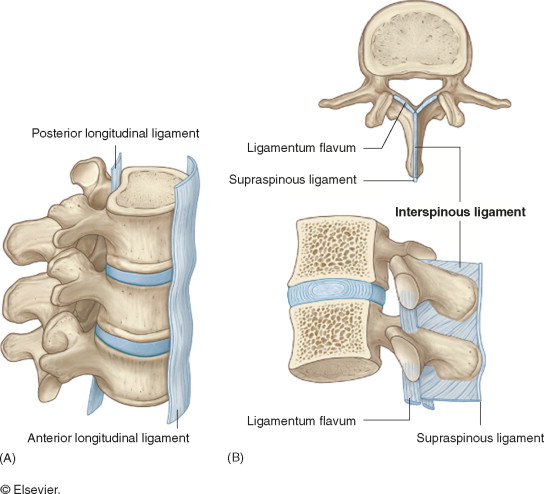
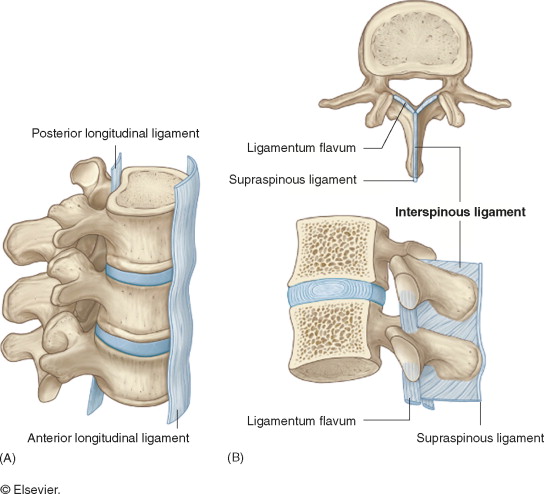
Name the Ligaments supporting the vertebral column
Anterior Longitudinal Ligament, Posterior Longitudinal Ligament, Ligamentum Flavum, Interspinous and Supraspinous Ligaments
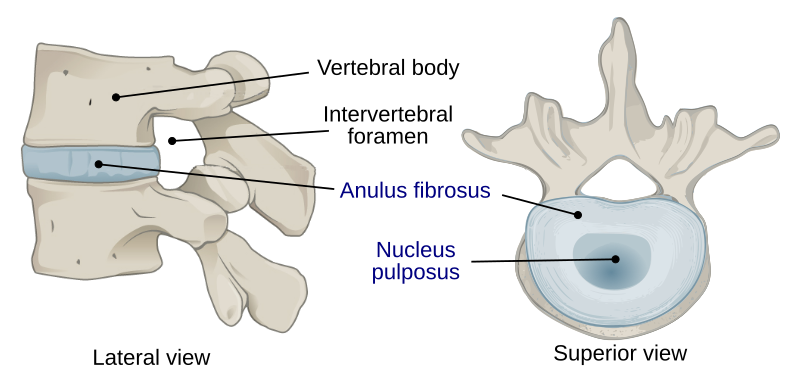
Anulus Fibrosus
The tough outer ring of fibrocartilage that surrounds the disc.
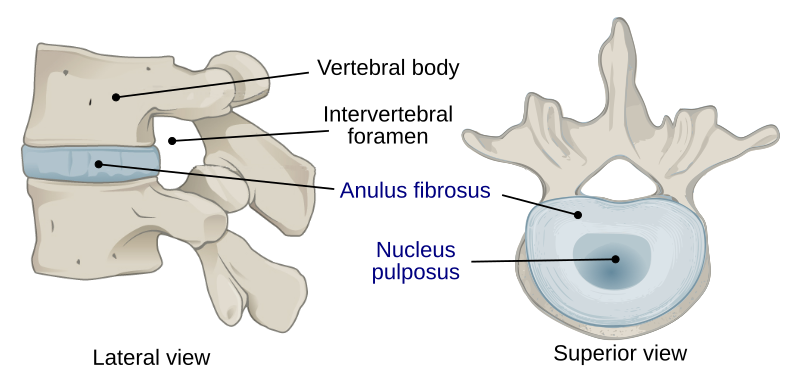
Nucleus Pulposus
The gel-like core that provides flexibility and acts as a shock absorber.
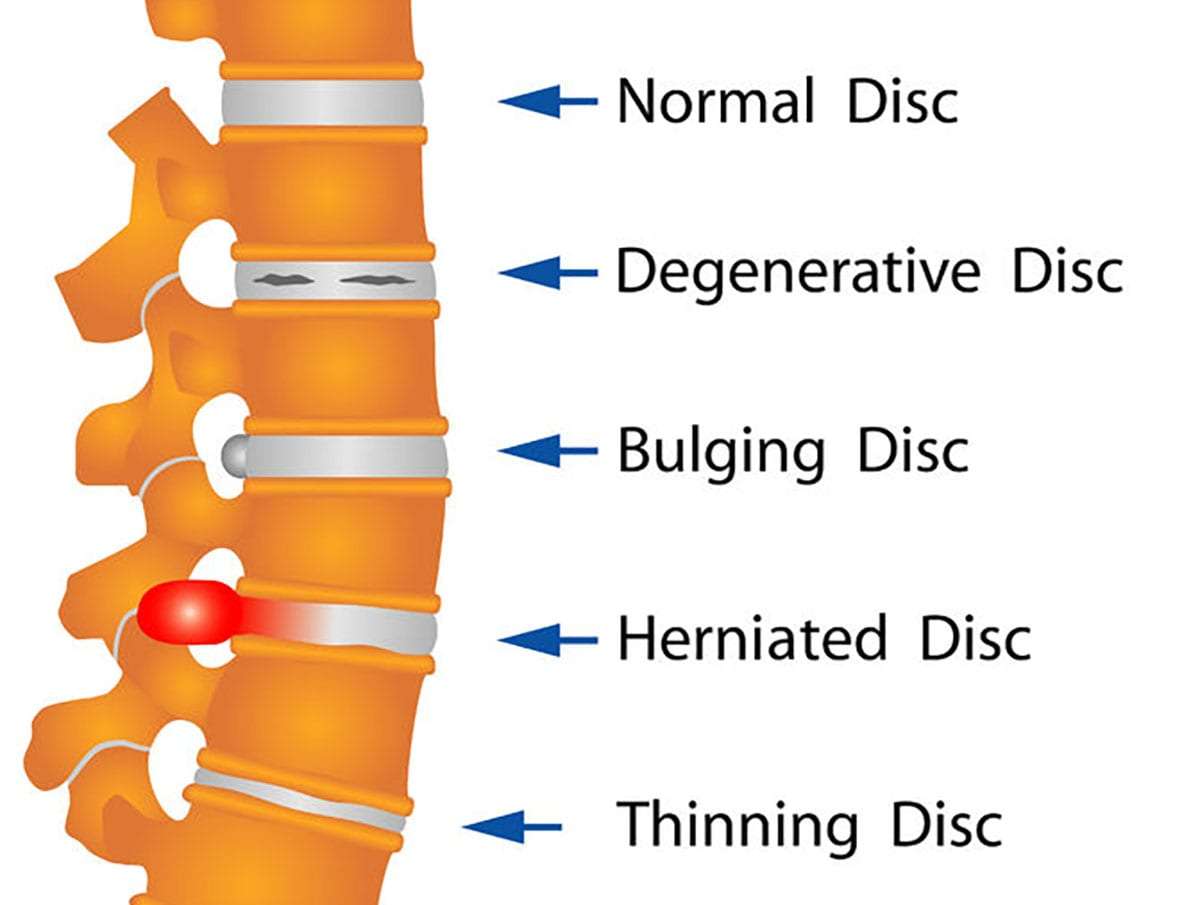
Bulging Disc
Occurs when the anulus fibrosus bulges outward, but the nucleus pulposus remains contained. This can cause mild pressure on spinal nerves
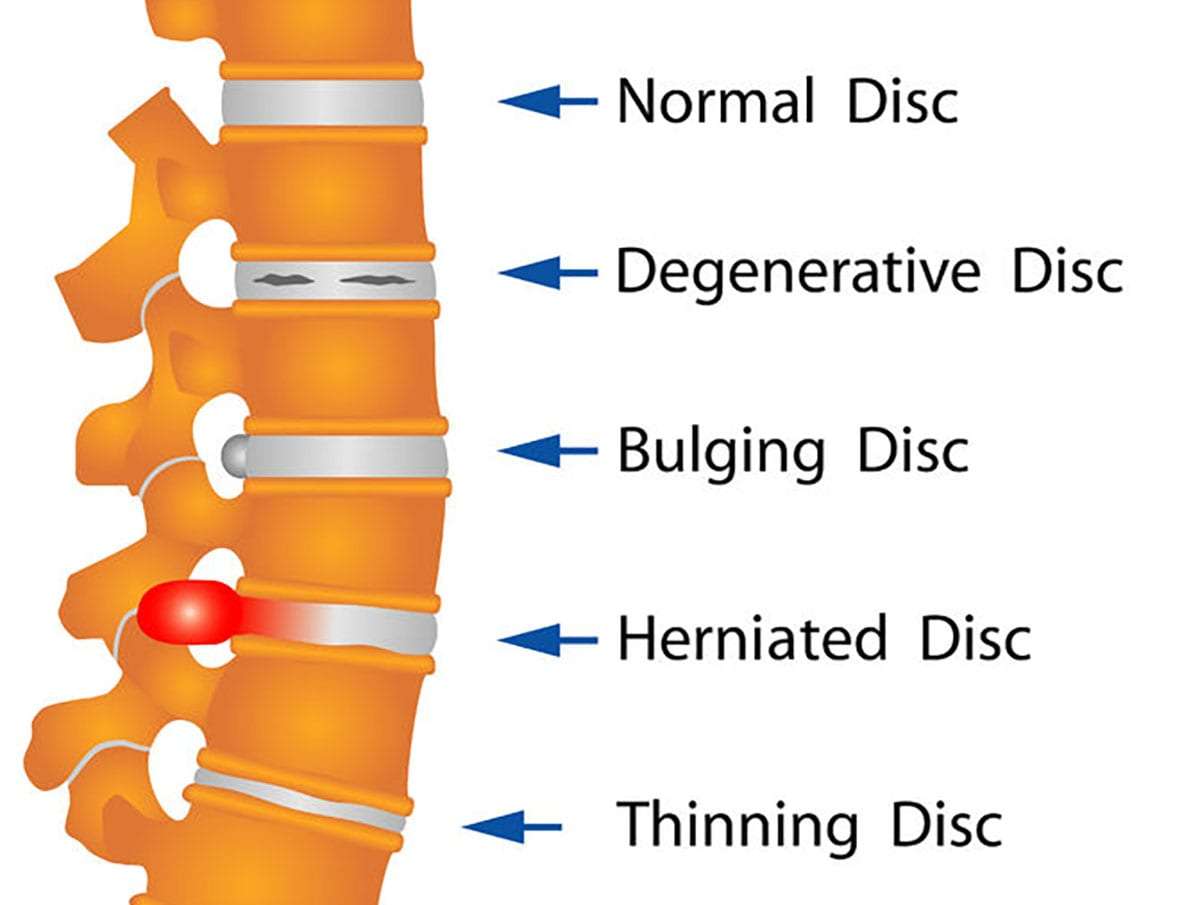
Herniated disc
The nucleus pulposus breaks through a tear in the anulus fibrosus, often pressing on nearby nerves, causing pain or numbness.
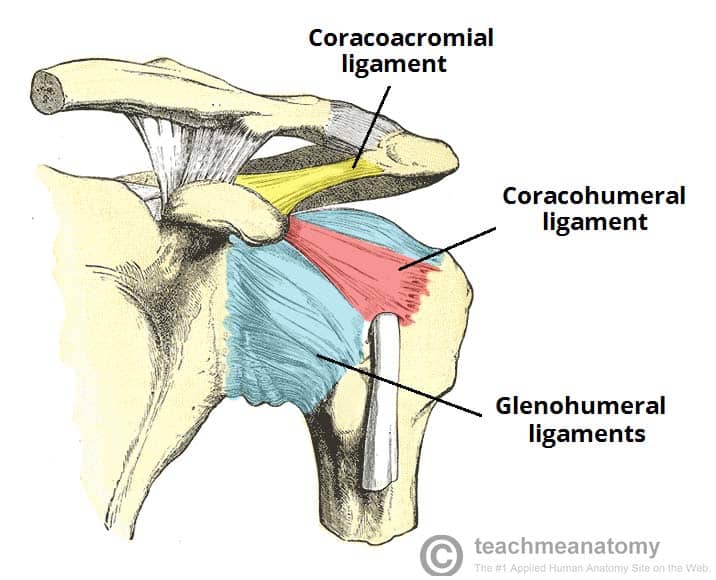
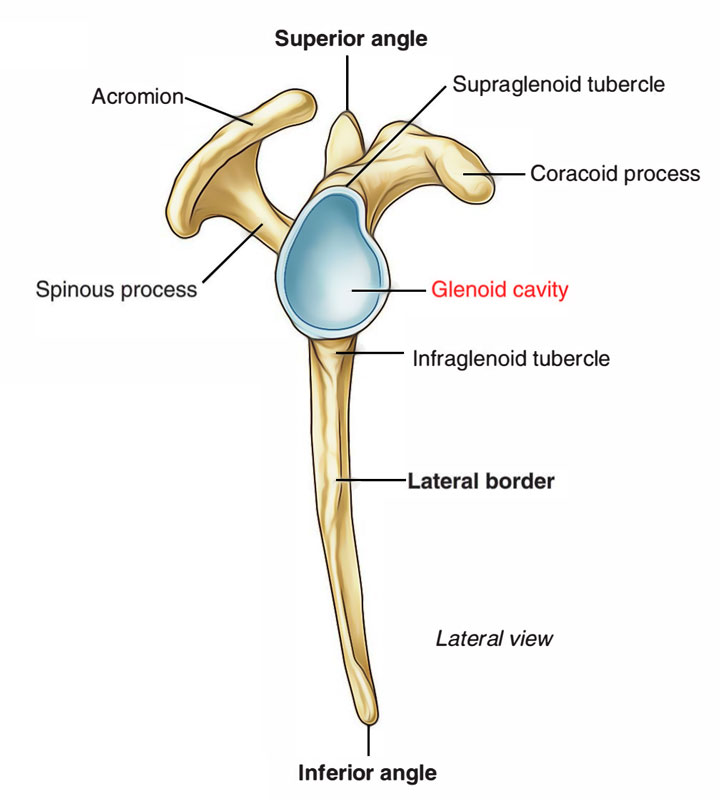
Structure of the Shoulder Joint
Bones: Involves the scapula (shoulder blade), clavicle (collarbone), and humerus (upper arm bone).
Articulation: The head of the humerus fits into the glenoid cavity (fossa) of the scapula, forming a ball-and-socket joint.
Ligaments:
Glenohumeral Ligaments: Reinforce the joint capsule.
Coracohumeral Ligament: Connects the coracoid process of the scapula to the humerus, providing stability.
Coracoacromial Ligament: Connects the coracoid process to the acromion, preventing upward dislocation of the humerus.
Glenoid Labrum
Location: Surrounds the rim of the glenoid cavity.
Structure and Role: A fibrocartilaginous ring that deepens the socket of the glenoid cavity, increasing joint stability.
Structures and Components of the Elbow Joint
The elbow joint involves the Humerus, Radius, and Ulna
What are the articulations for the Elbow Joint
Humeroulnar Joint: Formed by the trochlea of the humerus fitting into the trochlear notch of the ulna; this joint primarily allows flexion and extension.
Humeroradial Joint: Formed by the capitulum of the humerus articulating with the head of the radius; assists in movement alongside the humeroulnar joint.
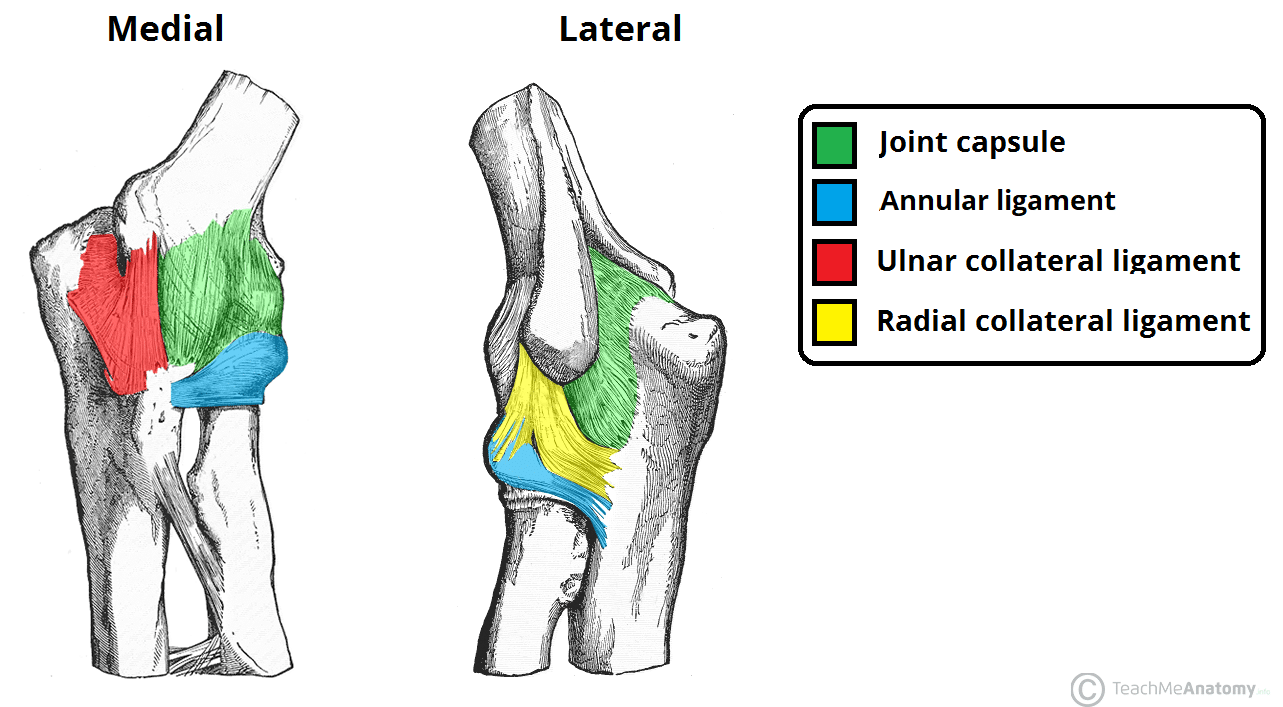
Name the ligaments of the Elbow Joint
Radial Collateral Ligament, Ulnar Collateral Ligament an the Annular Ligament
Name the bones that compose of the Hip Joint
Femur and the Pelvis
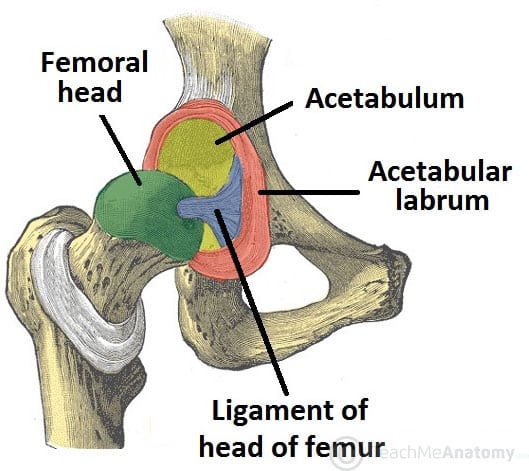
What are the articulations of the Hip Joint
The head of the femur fits into the acetabulum of the pelvis, forming a stable ball-and-socket joint that allows a wide range of motion.
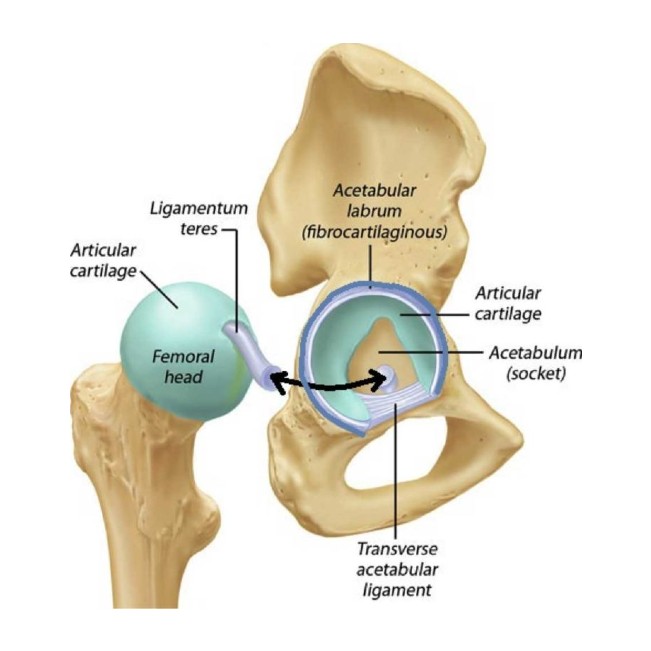
What are the ligaments and associated structures of the Hip Joint
Acetebulum, Acetabular Labrum, Femoral Head Ligament (Ligamentum teres), Transverse Acetabular Ligament, Greater an Lesser Trochanters
What bones make up the knee joint
Femur, Tibia, and Patella
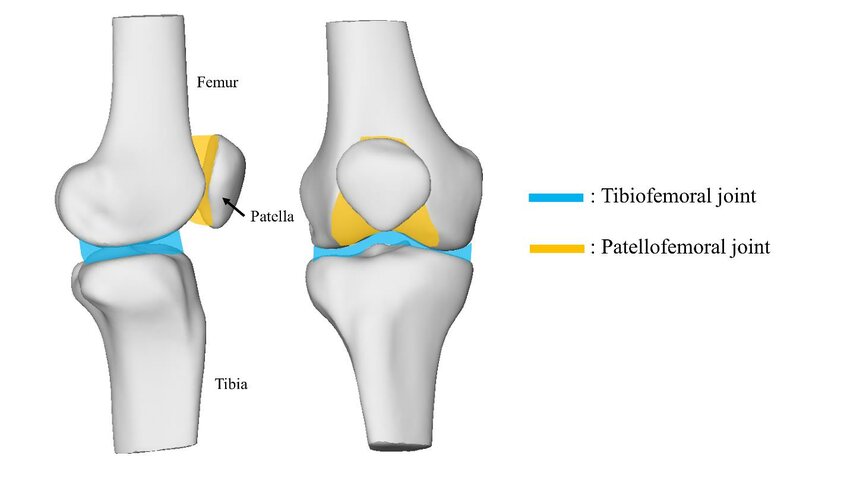
What is the articulation for the knee Joint
Tibiofemoral Joint: Between the femur and tibia, allowing for flexion, extension, and a slight degree of rotation.
Patellofemoral Joint: Between the patella and the femur, guiding the patella's movement over the femur.
What are the ligaments in the Knee joint
Anterior Cruciate Ligament ACL, Posterior Cruciate Ligament PCL, Medial Collateral Ligament MCL, and Lateral Collateral Ligament LCL, Even the Menisci (medial and Lateral)