LCCW Neuromuscular Physiopathology II - PNS Review and Neuromusc Intro
1/656
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
657 Terms
What are the components of the CNS? (2)
Brain and Spinal cord
What are the components of the PNS? (6)
-Cranial nerves
-Spinal nerves
-Plexuses
-Peripheral nerves
-ANS neurons and ganglia
-Enteric nervous system
What are the two efferent motor divisions of the PNS?
-Somatic motor
-Visceral motor
Somatic motor system aka?
Voluntary motor system
Visceral motor system aka?
Involuntary motor system
What is the function of the somatic division of the Efferent motor system?
Motor innervation of all skeletal muscles.
What is the function of the visceral division of the Efferent motor system?
Motor innervation of smooth muscle, cardiac muscle, and glands.
What are the two divisions that constitute the ANS?
-Parasympathetic division
-Sympathetic division
What are the characteristics of the sympathetic division of the ANS? (3)
-Fight-or-flight
-Thoraco-lumbar outflow (T1-L2)
-para-vertebral chain ganglia and pre-vertebral ganglia
What are the characteristics of the parasympathetic division of the PNS? (3)
-Rest-and-digest
-Cranio-sacral outflow (CNs III, VII, X, and S2-4)
-Ganglia located adjacent to, or in the walls of the target organs
What are the divisions of the sensory afferent portion of the PNS? (2)
-Somatic sensory
-Visceral sensory
What are the general somatic sensory functions of the somatic sensory division of the afferent nervous system?
Sense touch, pain, pressure, vibration, and proprioception in the skin, body wall, and limbs.
What are the special sensory functions of the somatic sensory division of the afferent nervous system?
Hearing, equilibrium, vision, smell.
Three letter designation for the somatomotor system.
GSE: General somatic efferent
Three letter designation for the autonomic nervous system.
GVE: General visceral efferent
Three letter designation for the somatosensory system.
GSA: General somatic afferent
Three letter designation for the visceral sensory system.
GVA General visceral afferent
Three letter designation for the special sensory division (excluding taste).
SSA: Special somatic afferent
Three letter designation for the special sensory division (taste).
SVA: Special visceral afferent
What makes up a peripheral nerve? (3)
-numerous axons
-associated connective tissues
-blood vessels (vaso nervosum)
How many total pairs of spinal nerves are there?
31
Where do cervical nerves exit the spinal canal?
Through the IVFs of the vertebrae above, because there are 8 cervical nerves, but only 7 vertebrae.
i.e.// C6 spinal nerve passes through the IVF between C5-C6 vertebrae.
Where do the lumbosacral nerves exit the spinal canal?
The exit below the vertebrae with the same numeric designation.
What is the cervical spinal nerve most likely to be compressed by disc herniation at the C4-5 level?
C5
What is the cervical spinal nerve most likely to be compressed by disc herniation at the C5-6 level?
C6
What is the cervical spinal nerve most likely to be compressed by disc herniation at the C6-7 level?
C7
What is the cervical spinal nerve most likely to be compressed by disc herniation at the C7-T1 level?
C8
What could cause a C6 radiculopathy?
C5-6 disc herniation
C5-6 IVF stenosis
What could cause a C7 radiculopathy?
C6-7 disc herniation
C6-7 IVF stenosis
Which spinal nerve is most likely to be compressed by disc herniation at the L4-5 level?
L5
Which spinal nerve is most likely to be compressed by disc herniation at the L5-S1 level?
S1
Which spinal nerve would most likely be compromised by stenosis of the L4-5 IVF?
L4
Which spinal nerve would most likely be compromised by stenosis of the L5-S1 IVF?
L5
What is radiculopathy?
It is a set of conditions in which one or more nerves are affected and do not work properly.
What are the common causes of radiculopathies?
Compression, inflammation, injury, herniation, IVF stenosis
Where do radiculopathies most commonly develop?
Lumbosacral spine
What are the two most common lumbosacral radiculopathies?
L5 and S1
What are the two most common cervical radiculopathies?
C6 and C7
At what level of the spinal canal does the spinal cord end in an adult?
L1 vertebral body.
What is the terminal end of the spinal cord called?
Conus medullaris
What is the cauda equina?
The group of lower lumbar and sacral nerves that travel the rest of the way down the spinal column.
What is cauda equina syndrome?
Disruption of the cauda equina resulting in numbness in the S3-4 dermatomes (saddle anesthesia).
What additional symptoms are associated with cauda equina syndrome?
-Urinary retention
-Fecal elimination dysfunction
-Sexual dysfunction
What can cause cauda equina syndrome?
Central disc herniation
What is the sensory distribution of the S3-5 spinal nerves?
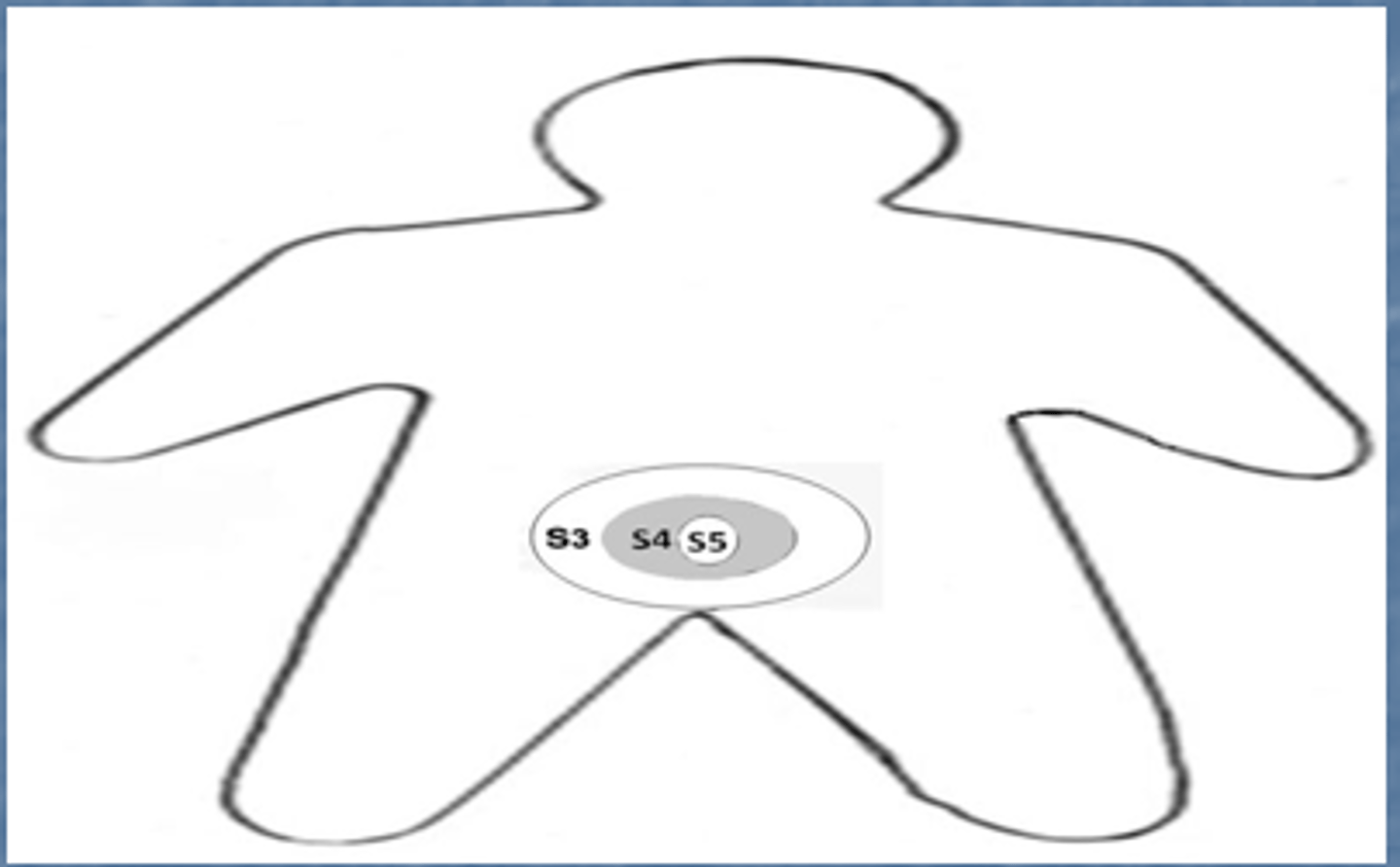
What is the descriptive name for numbness in the pelvic floor/perianal region?
Saddle anesthesia
Why is saddle anesthesia a "red flag"?
It is indicative of cauda equina syndrome, which can have much more serious problems.
Why might cauda equina syndrome compromise parasympathetic neurons but not sumpathetic neurons?
Because parasympathetic neurons have craniosacral outflow whereas sympathetic neurons have thoracolumbar outflow, ending at L2.
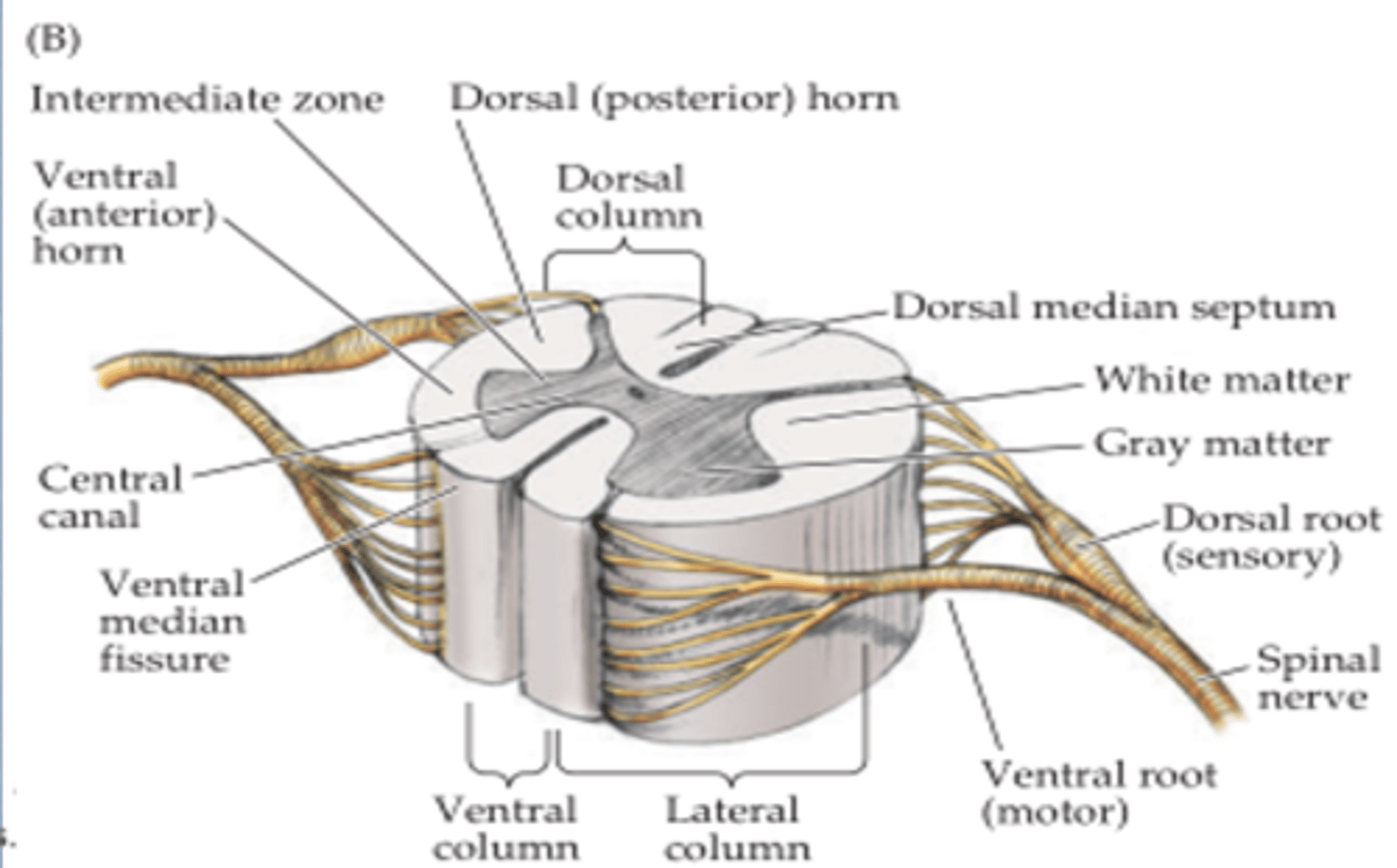
Which portion of the spinal nerve root is sensory?
The dorsal root.
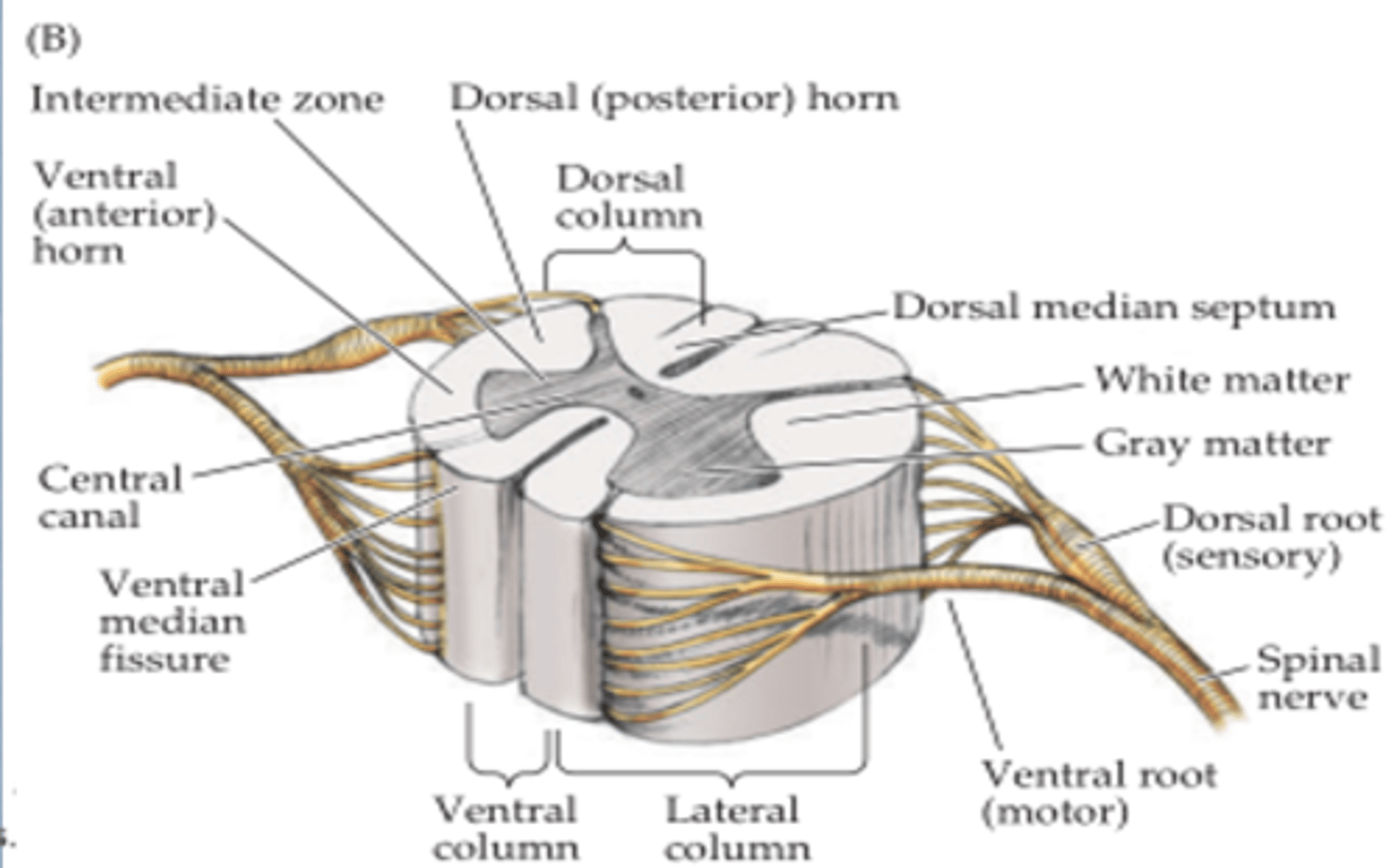
Which portion of the spinal nerve root is motor?
The ventral root
What is a dermatome?
It is an area of skin innervated by the sensory fibers of a single spinal nerve.
What is the name for the cutaneous area innervated by a spinal nerve?
Dermatome
What is the C5 dermatome?
In anatomical position, the upper-middle portion of the anterior arm.
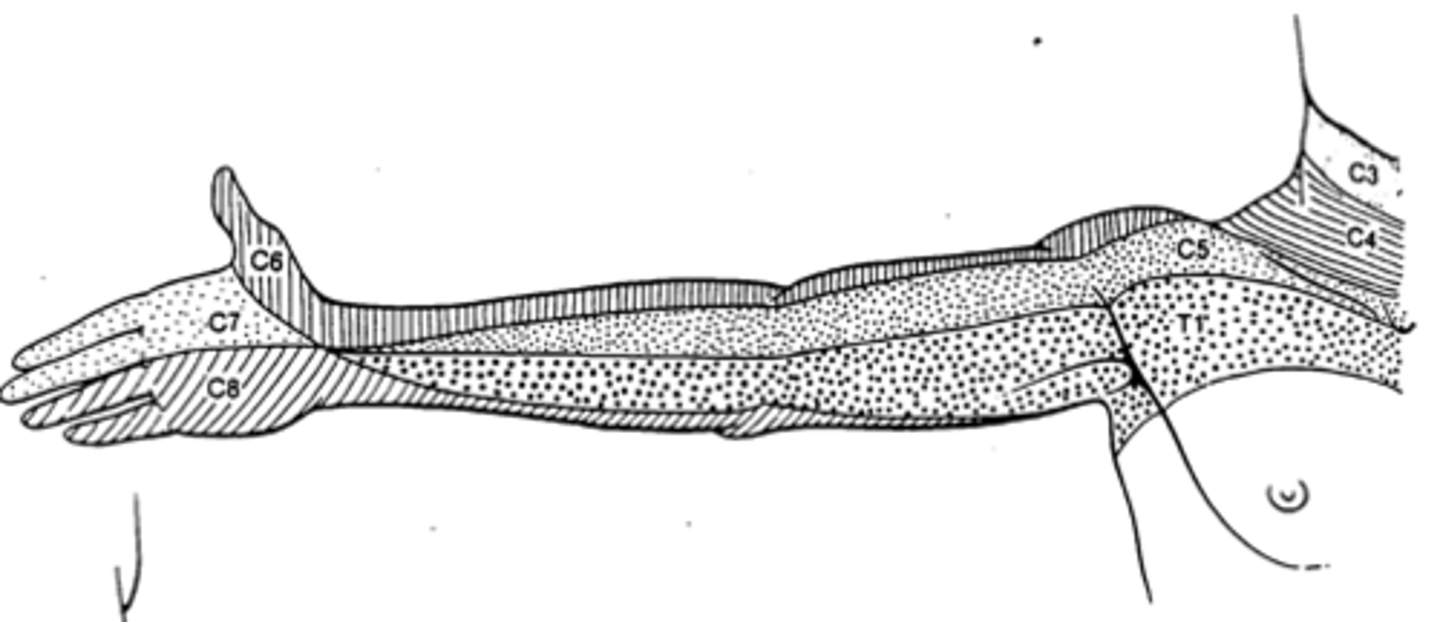
What is the C6 dermatome?
In anatomical position, the superior portion of the arm (both anterior and posterior) down to and including the thumb.
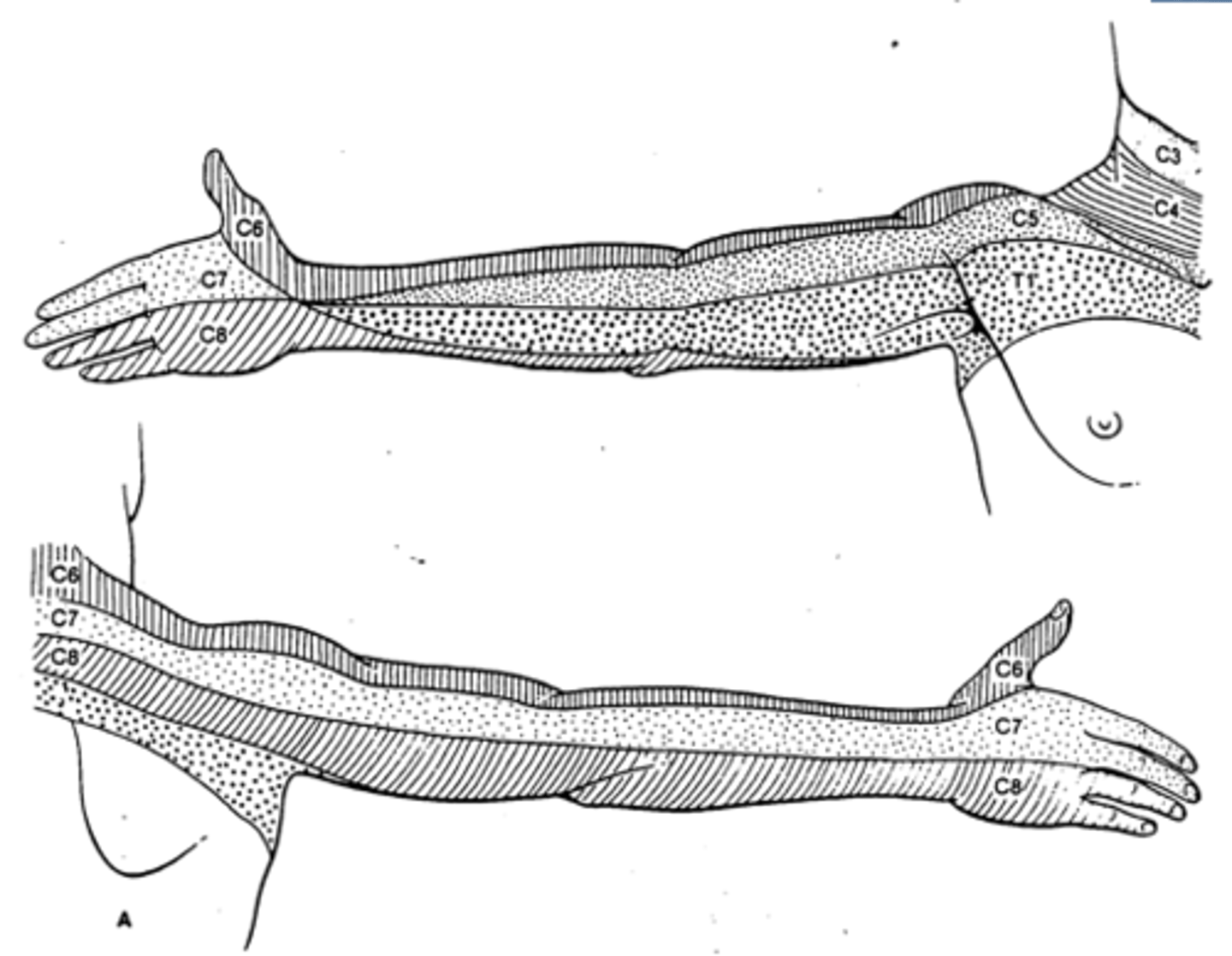
What is the C7 dermatome?
In anatomical position, the upper-middle portion of the posterior arm and the first two fingers anteriorly and posteriorly.
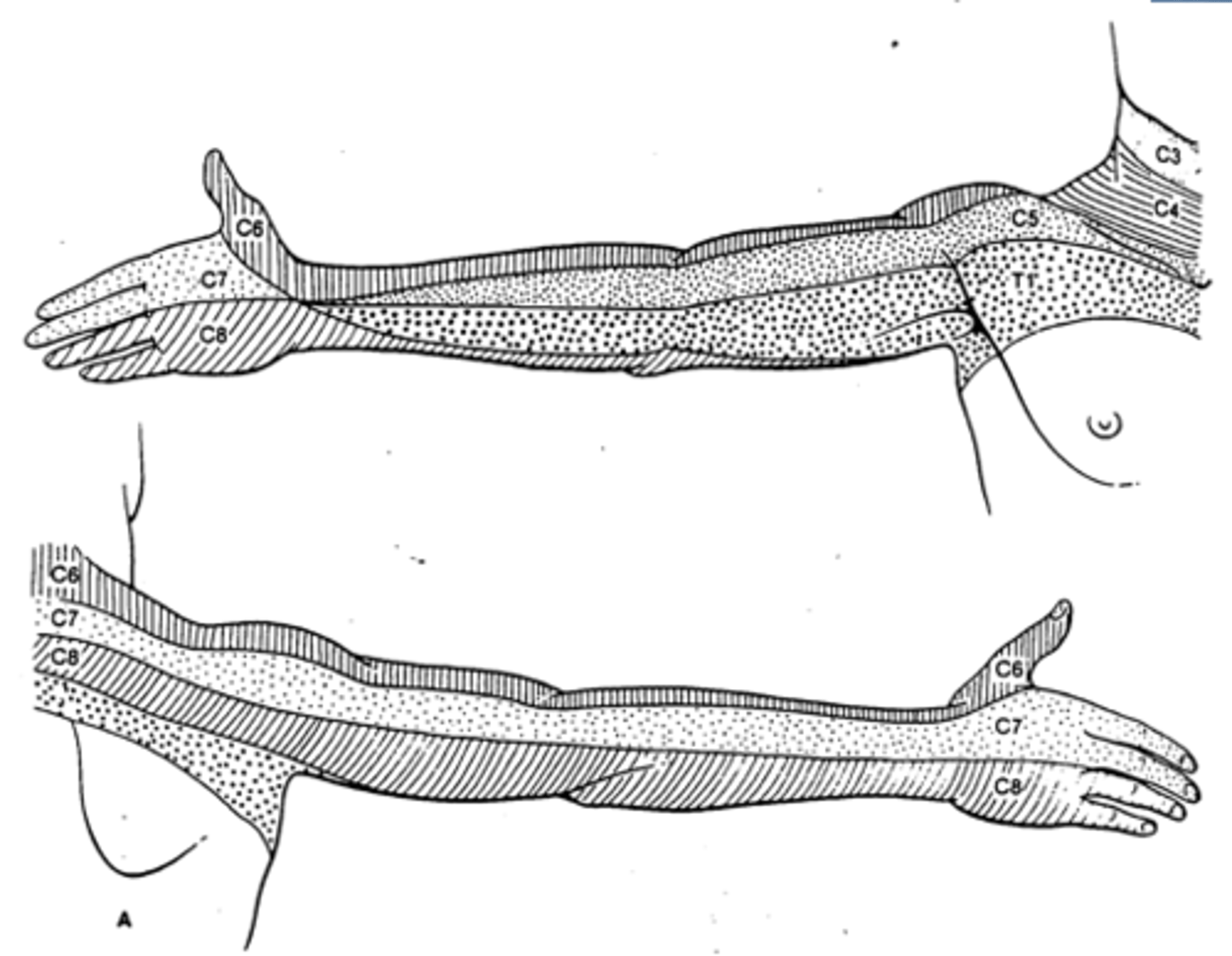
What is the C8 dermatome?
In anatomical position, the inferior portion of the posterior arm and the inferior portion of the distal anterior arm down to and including the last 2 fingers.
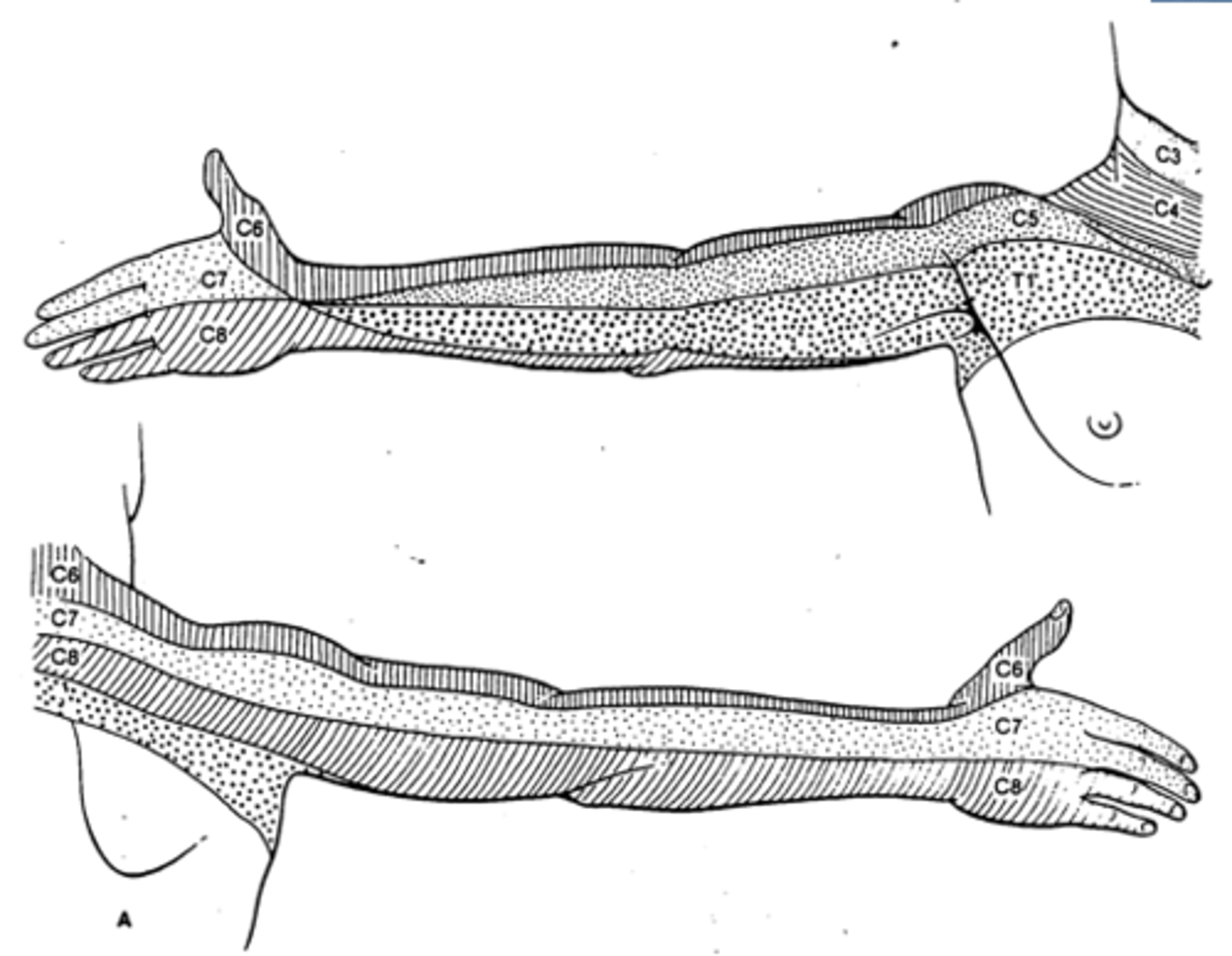
What is the T1 dermatome?
In anatomical position, the lower middle portion of the anterior arm near the elbow, possible extending medially into the pectoral region.
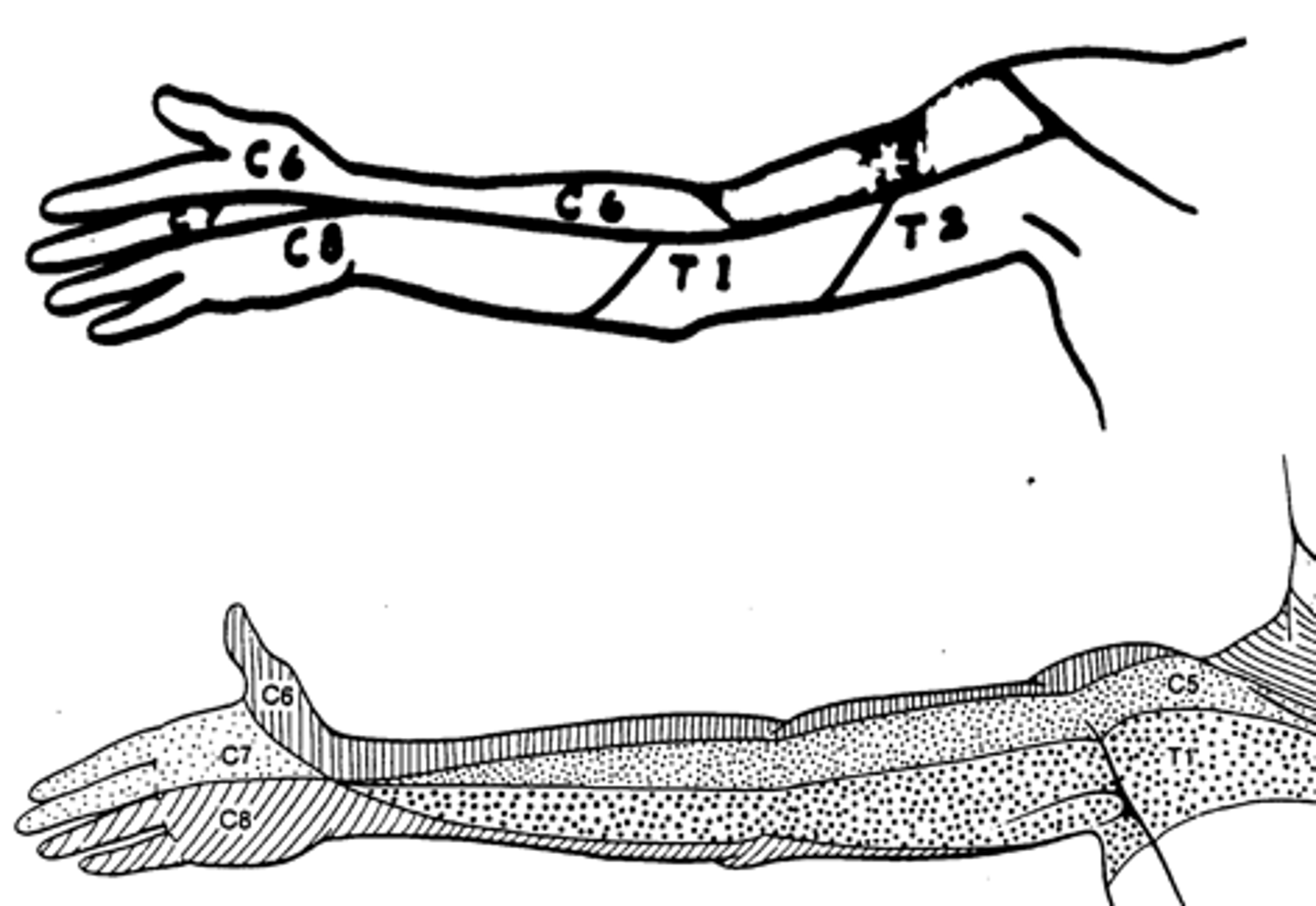
What are the variations of the dermatome innervation of the index finger?
It can be C6 or C7
What are the sensory complaints that could most likely develop in a patient with a C6 radiculopathy?
Tingling, pain and numbness, along with possible motor deficits of the lateral forearm and thumb.
Which spinal nerve is likely compromised when a patient has radicular pain, tingling, and numbness in the index and middle fingers?
C7
What is the T4 dermatome?
Nipple level across the torso.
What is the T7 dermatome?
Xiphoid process level across the torso.
What is the T10 dermatome?
Umbilicus level across the torso.
What is the T12 dermatome?
Distal pelvic level of the torso just above the inguinal ligament.
Describe the dermatome innervation of the trunk.
It is innervated by T1-T12 in order from top to bottom.
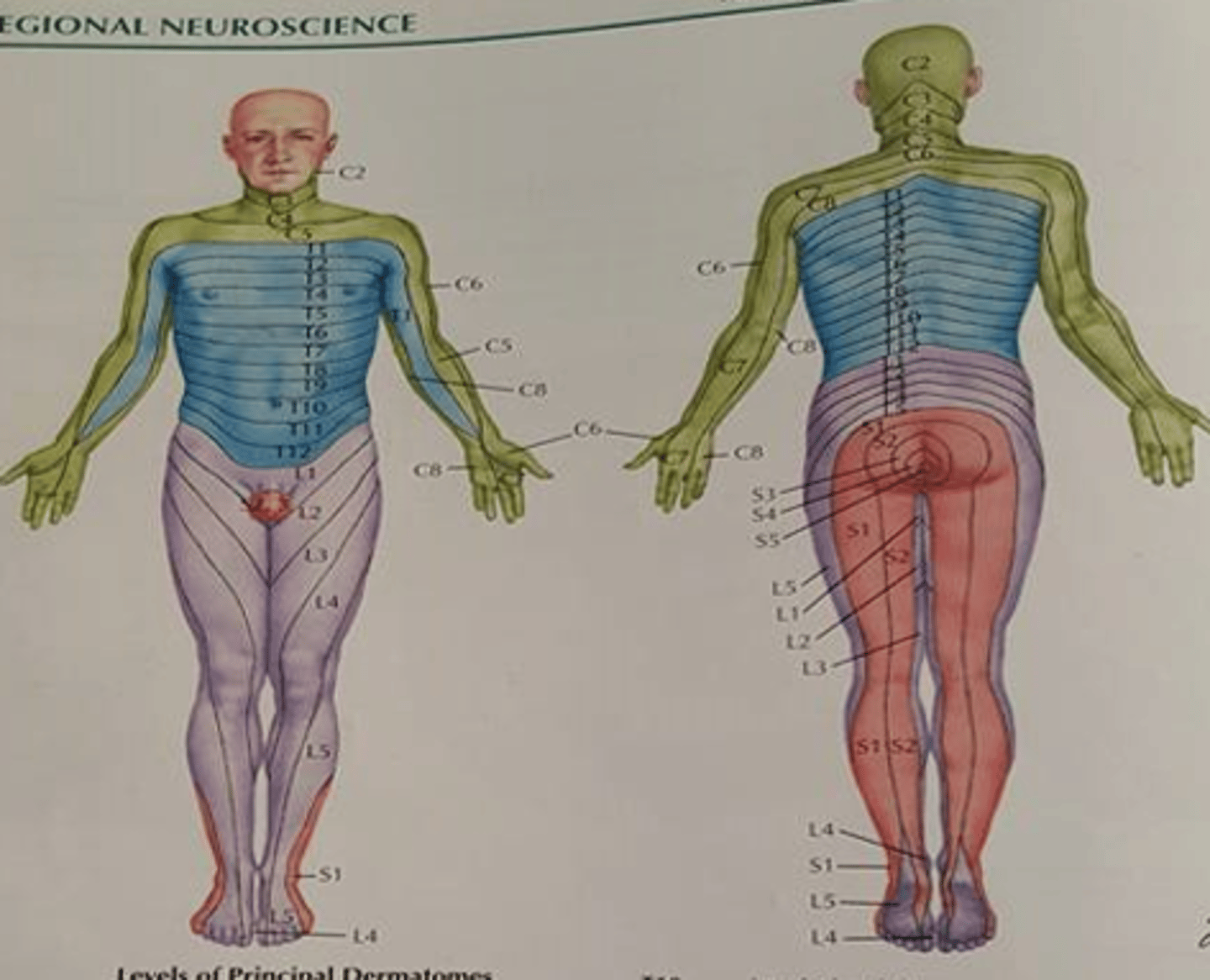
What is the L1 dermatome?
Proximal thigh just below the inguinal ligament.
What is the L2 dermatome?
Mid-thigh.
What is the L3 dermatome?
Distal thigh just above the patella.
What is the L4 dermatome?
Medial shin, ankle, and foot.
What is the L5 dermatome?
Lateral shin, dorsum of foot, toes (except little toe).
What is the S1 dermatome?
Posterolateral thigh, lateral calf, lateral ankle and foot, and little toe.
What is the S2 dermatome?
Posteromedial thigh and medial calf.

What is the sensory innervation of the big toe?
L5 dermatome
What are the primary/1st order afferent nerve fiber types?
Type I: A alpha (Ia, Ib)
Type II: A beta
Type III: A delta
Type IV: C
What primary afferent fibers originate from muscle spindles?
Type I, A alpha, Ia
What primary afferent fibers originate from golgi tendon organs.
Type I, A alpha, Ib
What primary afferent fibers originate from tactile receptors (pacinian corpuscles, meissner's corpuscles, merkel's discs, etc.)
Type II, A beta
What primary afferent fibers originate from nociceptors.
Type III, A delta
Type IV, C
What primary afferent fibers are more susceptible to the effects of compression?
Large-diameter afferents. i.e.// A alpha and A beta
What is the muscle-tendon receptor that is the stretch-length receptor?
Muscle spindle
What is the muscle-tendon receptor that is the tension-load receptor?
Golgi tendon organ (GTO)
How does a deep tendon reflex (DTR) occur?
The muscle spindle receptor sends action potential up the Type Ia fiber, which synapses with an Alpha lower motor neuron in the spinal cord, which effects the muscle.
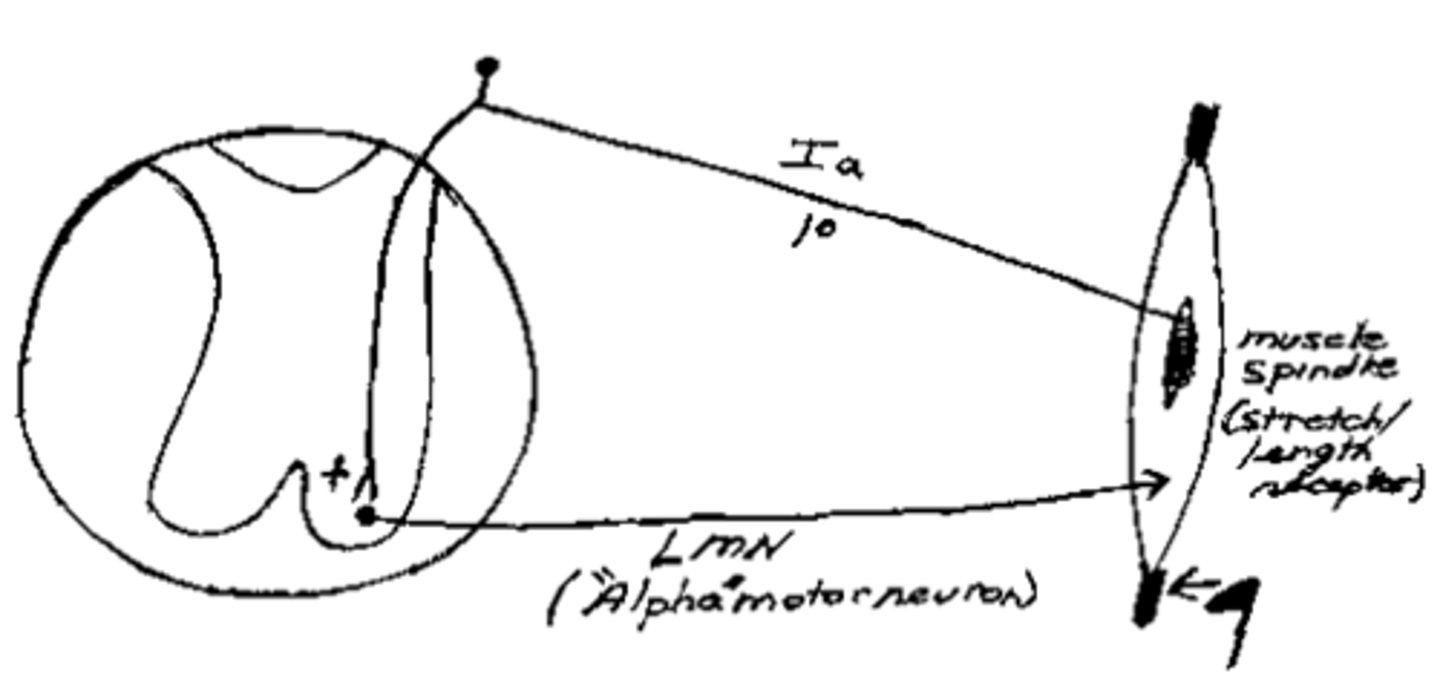
What can MSR stand for? (3)
-monosynaptic reflex
-muscle stretch reflex
-muscle spindle reflex
How does the golgi tendon organ (GTO) reflex occur?
The GTO sends an action potential up the Type Ib fiber, which synapses with an inhibitory Ib interneuron, which inhibits the Alpha lower motor neuron. This prevents overloading of the muscle and tendon.
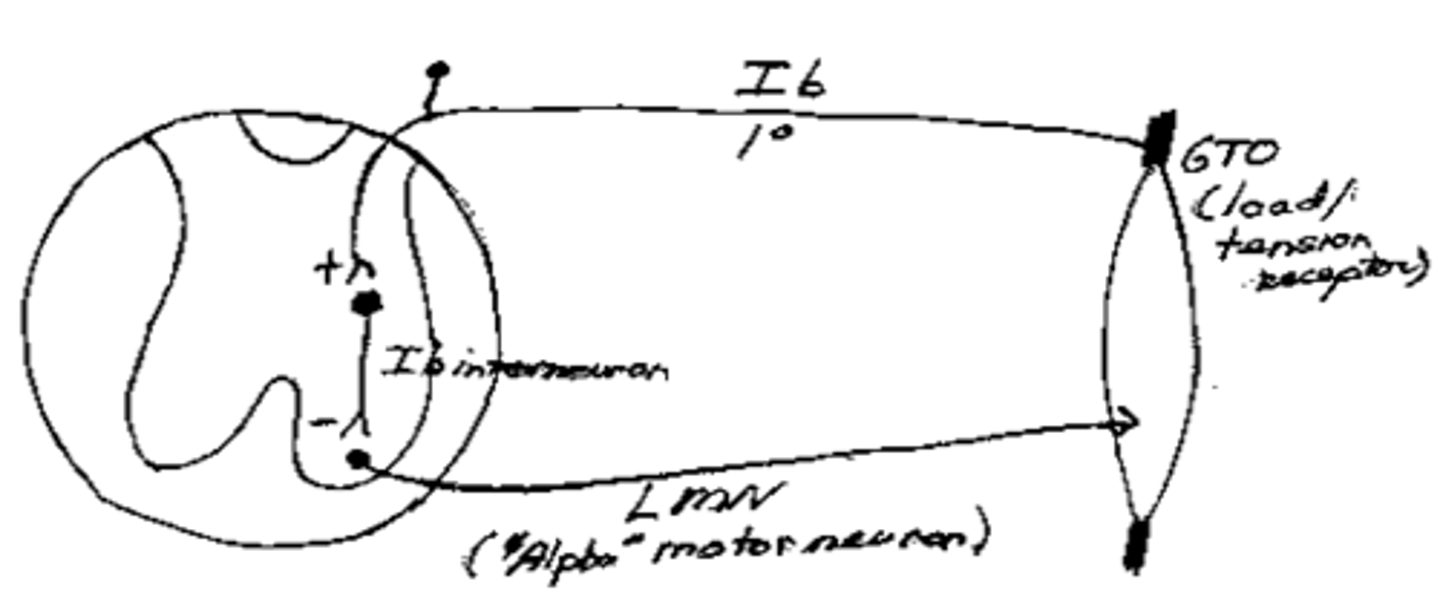
Which reflex would most likely be responsible for a reduction of local muscle spasm following an adjustment?
GTO reflex.
What is the technical name for pain receptors?
Nociceptors
Are nociceptors encapsulated or free nerve endings?
Free nerve endings
What other type of receptor (aside from pain) uses free nerve endings?
Temperature
Are tactile receptors encapsulated or free nerve endings?
Encapsulated
What are meissner's corpuscles? Are they fast or slow adapting?
Fast-adapting mechanoreceptors for detecting moving touch.
What are Merkel's discs? Are they fast or slow adapting?
They are slow-adapting mechanoreceptors for detecting sustained touch or maintained deformation.
What are Pacinian corpuscles? Are they fast or slow adapting?
They are fast-adapting mechanoreceptors for detecting vibration and deep pressure.
What are Ruggini endings? Are they fast or slow adapting?
They are slow-adapting mechanoreceptors for detecting steady pressure applied to hairy skin.
What are krause end bulbs?
Thermoreceptors
Which spinal tract conveys pain and temperature sensations?
Spinothalamic tract (anterolateral system)
Which spinal tract conveys tactile sensations?
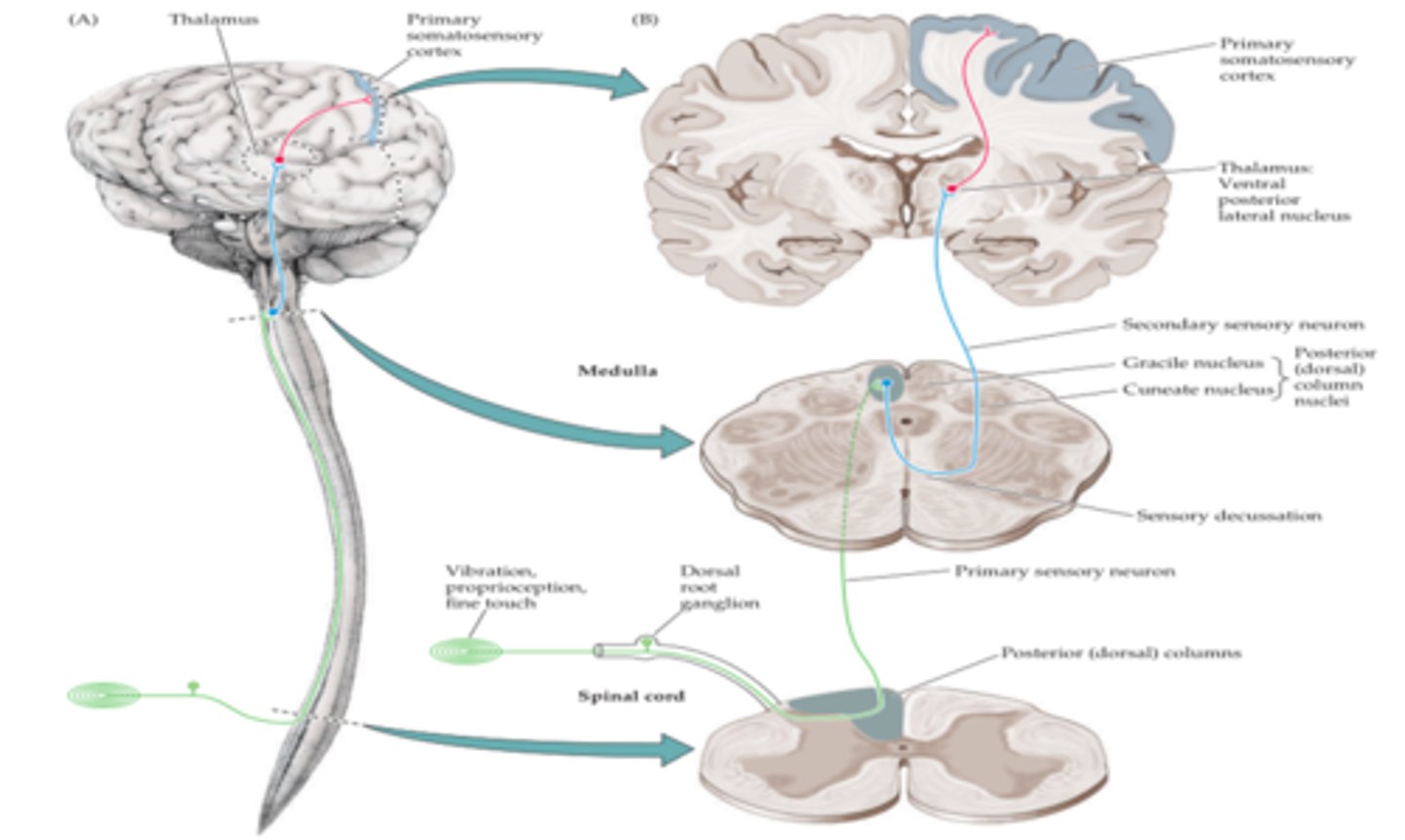
Dorsal Column Medial Lemniscus (DCML)
Does the somatic sensory system decussate?
Yes.
How is tactile sensation transmitted through the spinal cord?
It ascends ipsilaterally via the DC, and then decussates in the medulla and continues in the ML.
How is pain/temp sensation transmitted through the spinal cord?
It immediately decussates, and then ascends contralaterally to the medulla.
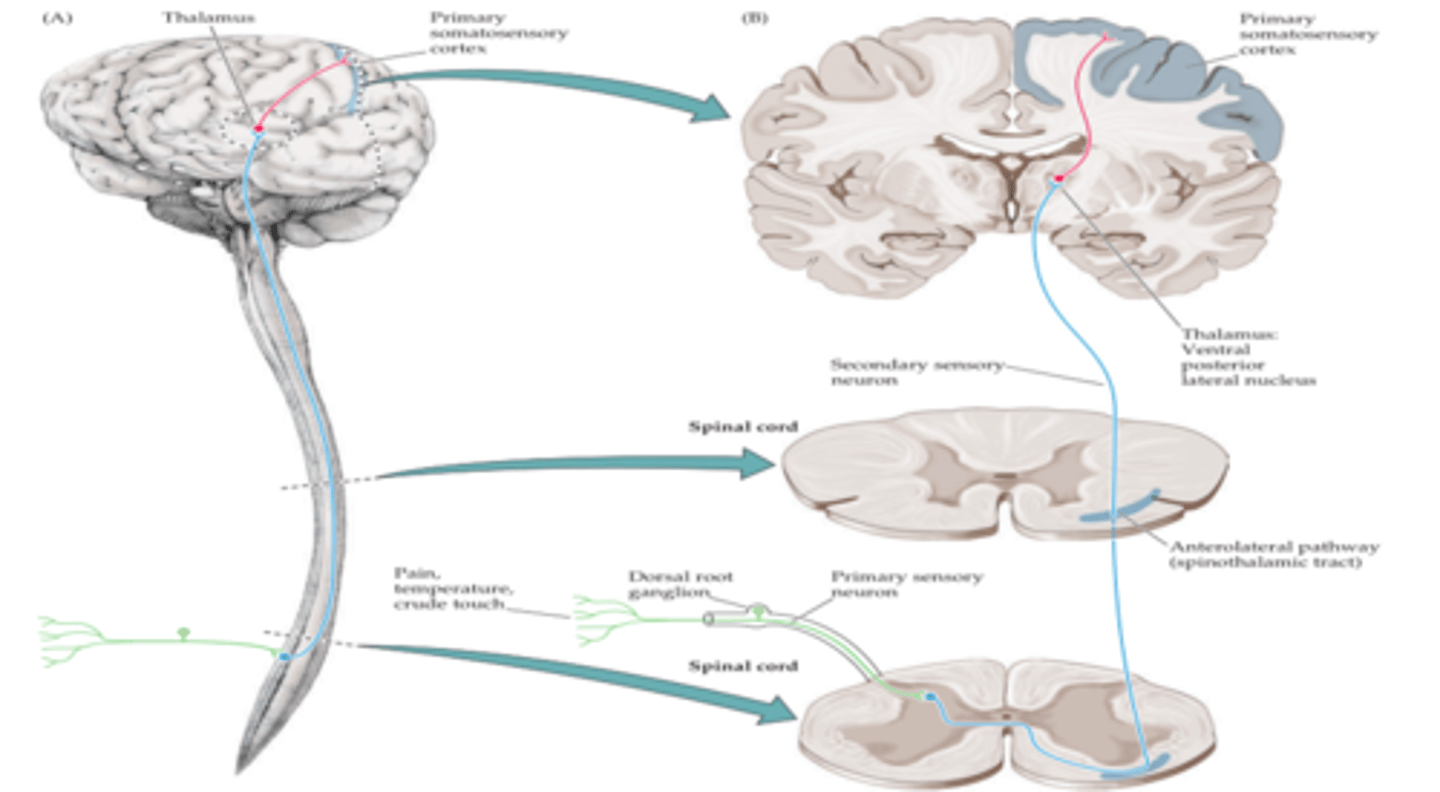
How would a lesion in the spinothalamic tract present?
Contralaterally