(21.5.6) Humoral immune response & Cellular immune response
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
Define Humoral Immune Response
When B cell encounters target antigen → antibodies specific for that particular antigen are then produced
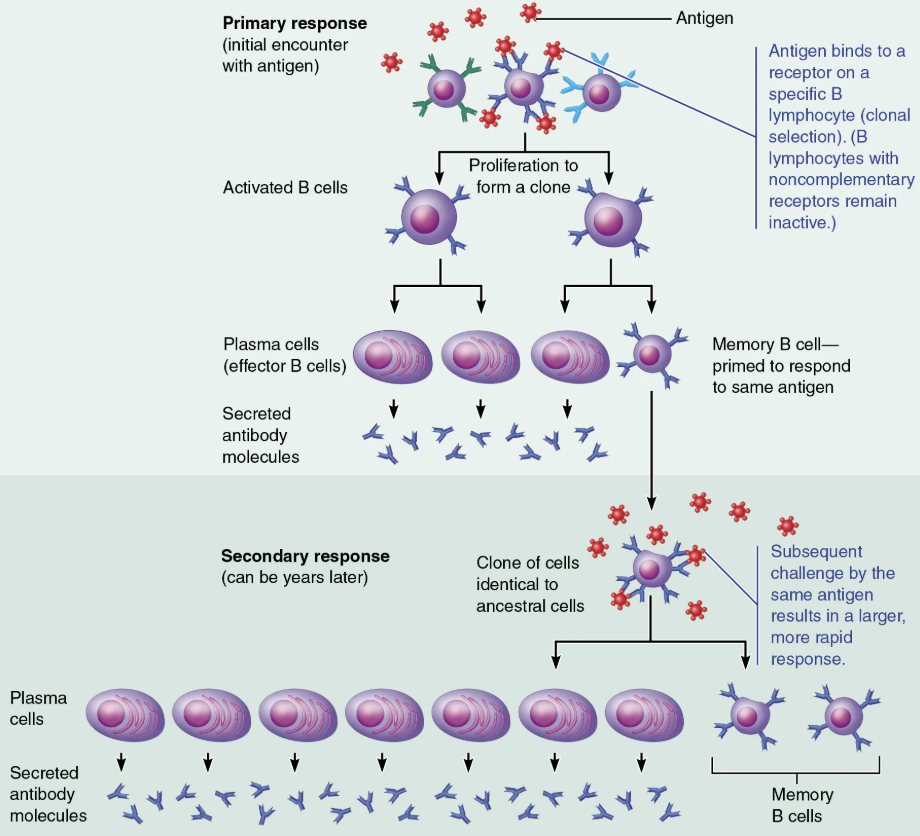
What is meant by the clonal expansion of a B cell?
An activated B cell divides into cells that give rise to memory B cells and plasma cells.
Describe the process of clonal selection of a B cell
Immunocompetent but NAIVE B lymphocyte is ACTIVATED when antigens bind to its surface receptors
The activated B lymphocyte begins clonal selection → the process of the B cell growing and multiplying to form an army of cells that are capable of recognizing the same antigen
Most cells of the clone develop into plasma cells → the antibody-secreting cells of the humoral response
The cells of the clone that do not become plasma cells develop into memory cells
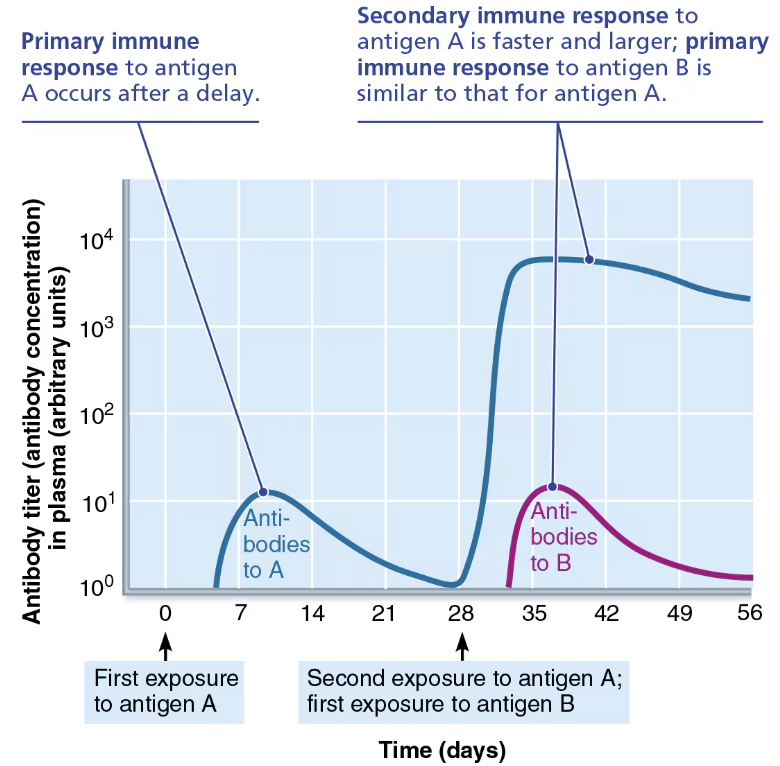
Compare and Contrast Primary Immune Response & Secondary Immune Response
Humoral Responses
PRIMARY
Cell proliferation and differentiation upon exposure to antigen for the first time
LAG period: 3-6 days
Peak levels of plasma antibody are reached in 10 days
Antibody levels then decline
SECONDARY
Re-exposure to same antigen gives faster, more prolonged, more effective response
Sensitized memory cells provide immunological memory
Respond within HOURS, not days
Antibody levels peak in 2 to 3 days at much higher levels
Antibodies bind with GREATER affinity
Antibodies level can remain HIGH for weeks to months
Discuss the roles of plasma cells and memory cells in humoral immunity
Plasma cells → Members of a B cell clone
Effector B cells specialized to produce and release antibodies
Memory cells → Members of T cell and B cell clones
Provide for immunological memory.
What roles do memory B cells play when a patient is re-exposed to an antigen?
Memory B cells trigger a secondary immune response, which is faster, more prolonged, and more effective than the first immune response
Memory cells to that specific virus are stored in the lymph nodes for many years
When the patient comes into contact with this specific virus, these memory cells quickly divide and differentiate into antibody-producing plasma cells
The antibodies will prevent the virus from reaching an infectious titer
KNOWN Primary and Secondary Humoral Responses Graph
The primary response to antigen A generates memory cells that give rise to the enhanced secondary response to antigen A
The response to antigen B is independent of the response to antigen A.
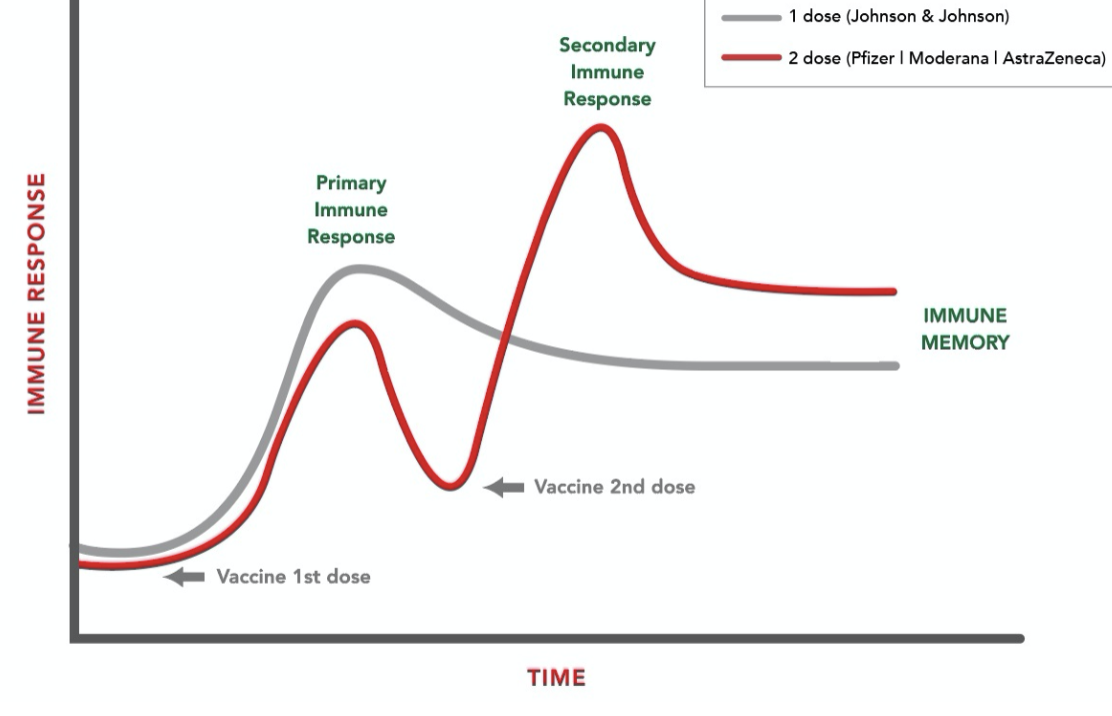
KNOWN Primary and Secondary Humoral Responses with Vaccies Graph
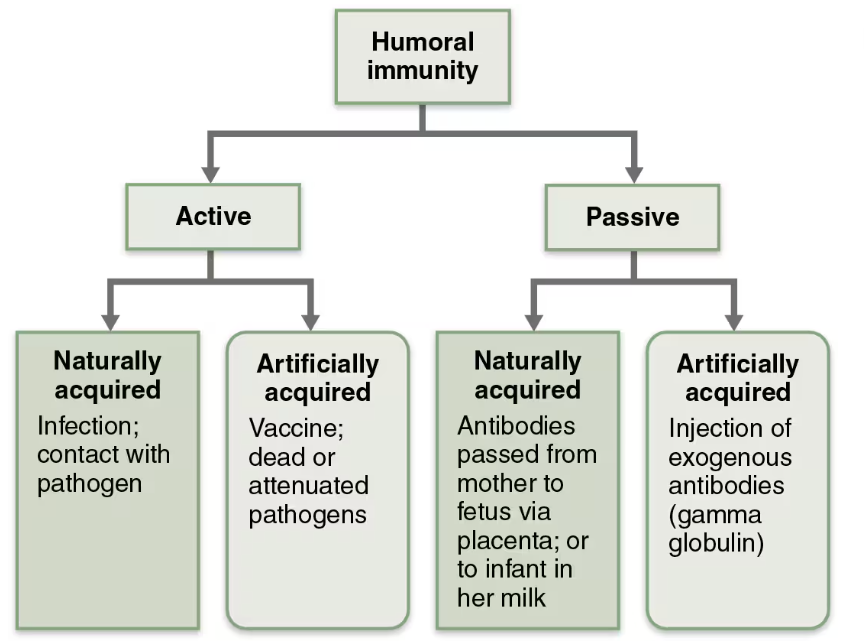
Define Active Humoral Immunity
Occurs when B cells encounter antigens and produce specific antibodies against them
Two types:
Naturally acquired
Artificially acquired
Compare and Contrast Naturally acquired & Artificially acquired Active Humoral Immunity
Naturally acquired
Formed in response to actual bacterial or viral infection
Artificially acquired
Formed in response to vaccine of dead or attenuated pathogens
Benefits from Vaccines
Provide antigenic determinants that are immunogenic and reactive
Spare us symptoms of primary response
Define Passive Humoral Immunity
Occurs when ready-made antibodies are introduced into body
B cells are not challenged by antigens
Immunological memory does not occur
Protection end when antibodies degrade
Two Types:
Naturally acquired
Artificially acquired
Compare and Contrast Naturally acquired & Artificially acquired Passive Humoral Immunity
Naturally acquired
Occurs when a mother’s antiboides enter fetal circulation
Artificially acquired
Occurs when a person is given preformed antibodies that have been harvested from another person
Compare and Contrast Active and Passive humoral immunity
ACTIVE
Occurs when B cells encounter antigens and produce specific antibodies against them
PASSIVE
Occurs when ready-made antibodies are introduced into body
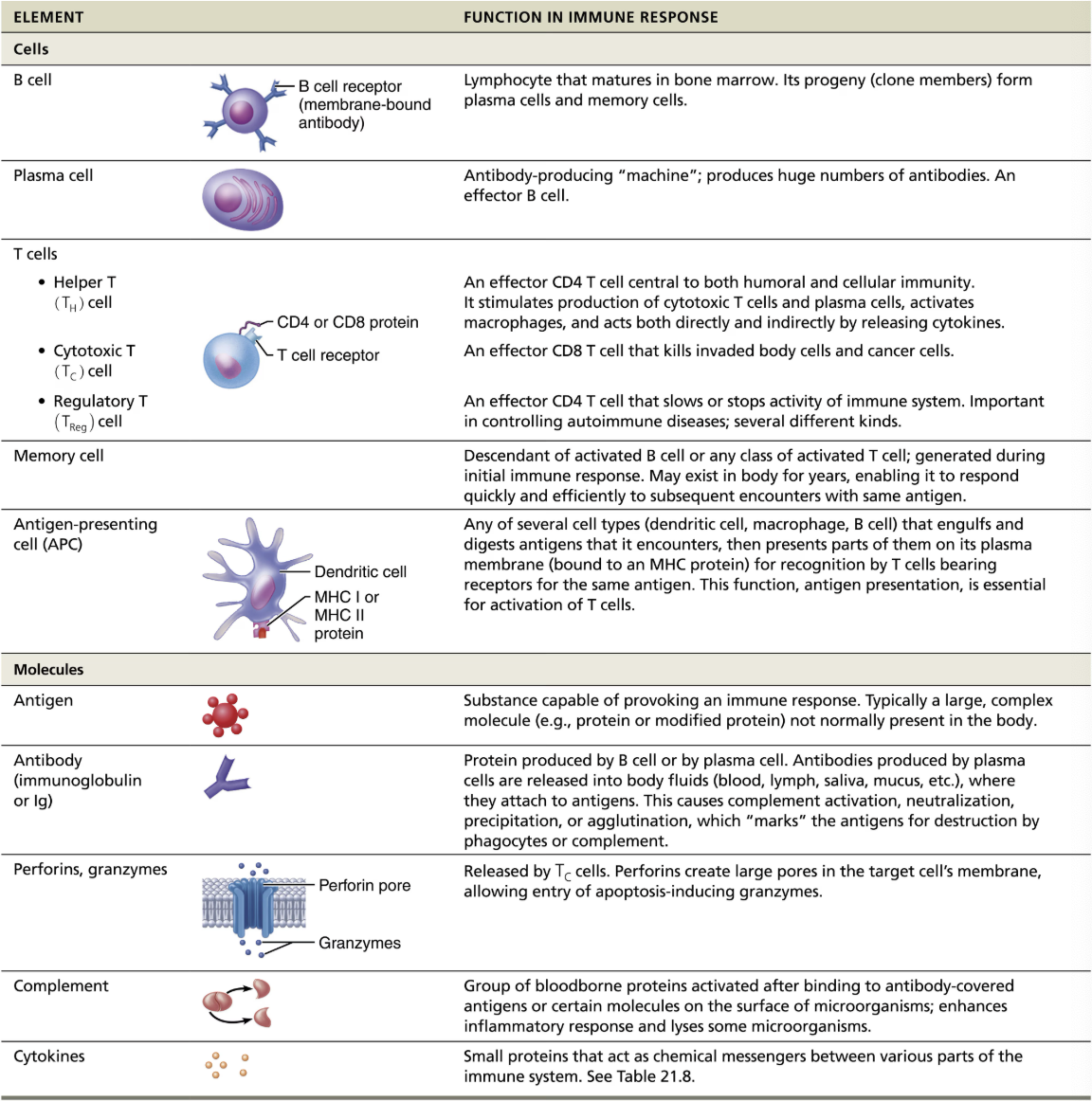
Define Antibodies
Immunoglobulins (Igs)
Proteins secreted by plasma cells
Make up gamma globulin protein of blood
Capable of binding specifically with antigens detected by B cells
Group into one of 5 Ig classes
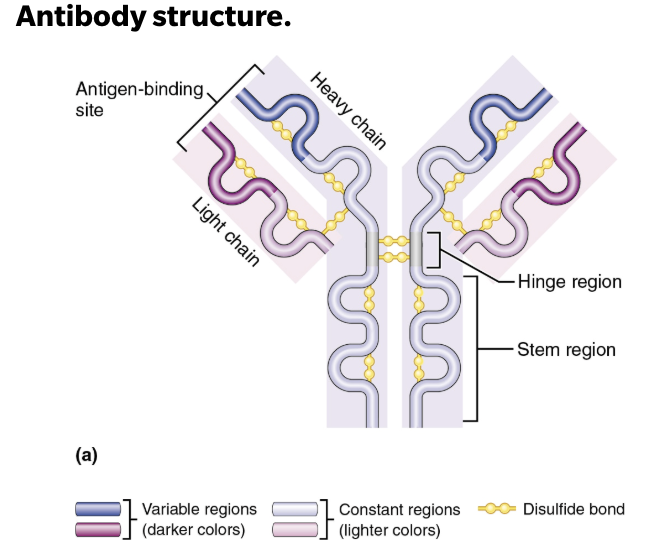
Describe the Structure of Antibodies
T- or Y-shaped antibody monomer consists of 4 looping polypeptides chains linked by disulfide bonds
2 identical heavy (H) chains
2 identical shorter, light (L) chains
Each chain has a variable region at one end, which varies depending on the antigen it binds, and a constant region at the other end, which is nearly identical among all members of a given class of antibodies
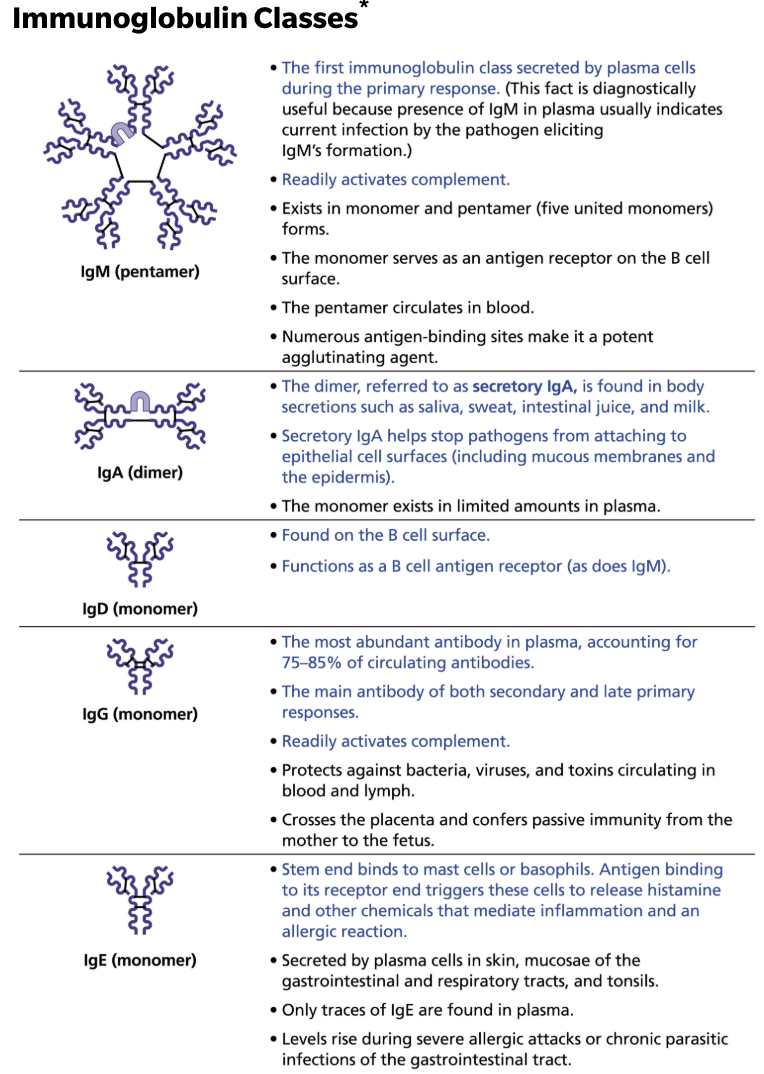
Describe the structure and functions of antibodies and name the five antibody classes.
Antibodies are divided into 5 classes based on their structure
IgM
1st immunoglobulin class secreted by plasma cells during primary response
Readily fixes and activates complement
IgA
The dimer, referred to as secretory IgA, is found in body secretions such as saliva, sweat, intestinal juice, and milk
Secretory IgA helps stops pathogens from attaching to epithelial cell surfaces (inculding mucous membranes and the epidermis)
IgD
Found on the B cell surface
Functions as B cell antigen receptor (as does IgM)
IgG
The most abundant antibody in plasma, accounting 75-85% of circulating antibodies
The main antibody of both secondary and late primary responses
Readily fixes and activates complement
IgE
Stem end binds to mast cells or basophils
Antigen binding to its receptor end triggers these cells to release histamine and other chemicals that mediate inflammation and an allergic reaction
Cause and Treatment of Ascaris and Schistosoma
CAUSE
Parasitic infections by worms, require different immune attack strategies
TREATMENT
IgE antibodies still play a critical role in worm’s destruction by binding to surface of worm, marking it for destruction by eosinophils
Eosinophils bind to exposed stems of IgE → which triggers eosionphils to release their toxic contents onto prey, lysing it from the outside
Describe Antibody Targets and Function(s)
Antibody do not destroy antigens → they inactivate and tag them
Form antigen-antibody (immune) complexes
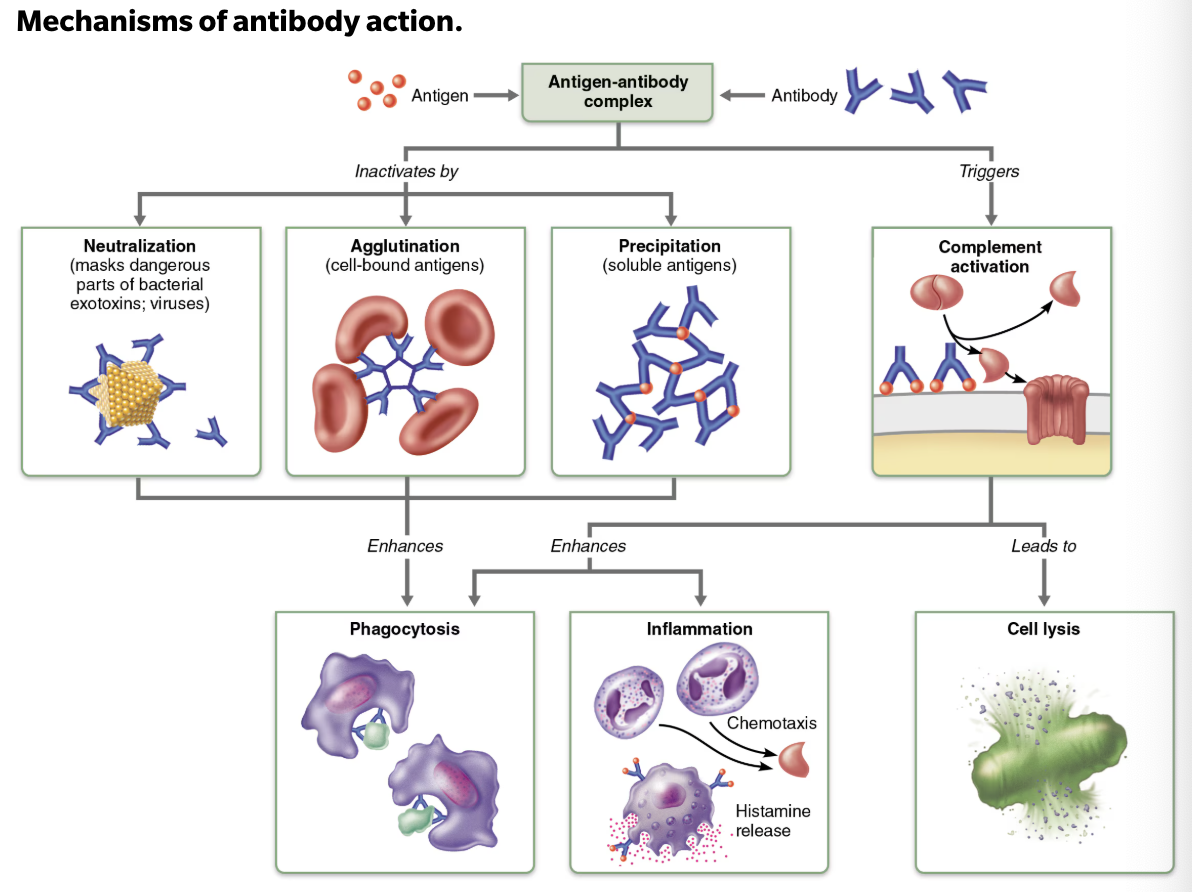
List and Describe Defensive Mechanism Used by Antibodies
Neutralization
Occurs when antibodies block specific sites on viruses or bacterial exotoxins → causing them to lose their toxic effects
Agglutination
Occurs when antibodies cross-link to cells-bound antigens→ causing clumping
Precipitation
Occurs when soluble molecules are cross-linked into large complexes that settle out of solution
Complement activation
Occurs when complement binds to antibodies attached to antigens →leads to lysis of the cell
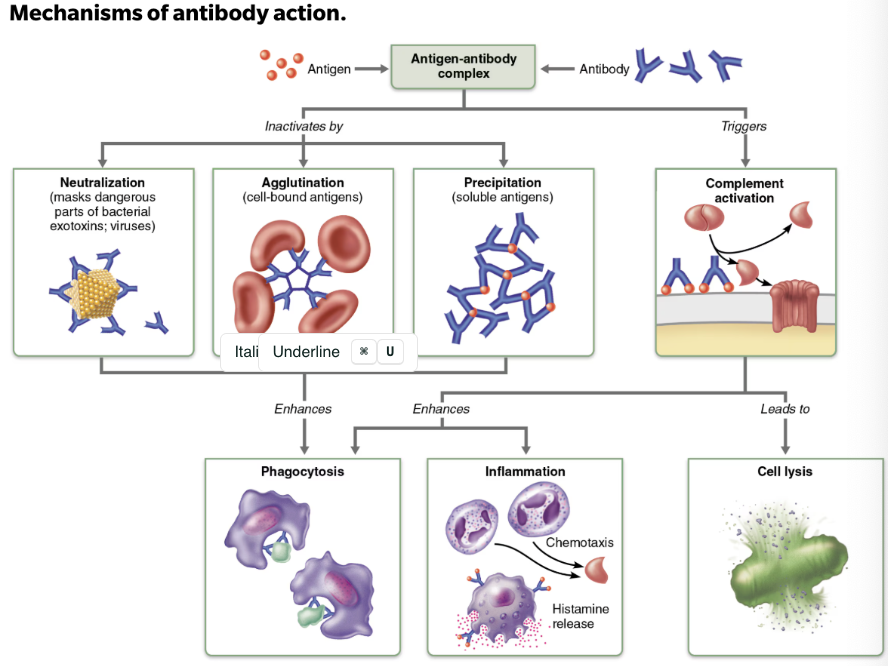
Summary of Antibody Actions
Antigen-antibody complexes do not destroy antigens → they prepare them for destruction by innate defenses
Antibodies go after extracellular pathogens → they do not invade solid tissue unless lesion is present
EXCEPTION → antibodies can act intracellularly if attached to virus before it enters cell
Define Monoclonal Antibodies
Clinical and research tools
Commercially prepared pure antibodies that are specific for a single antigenic determinant
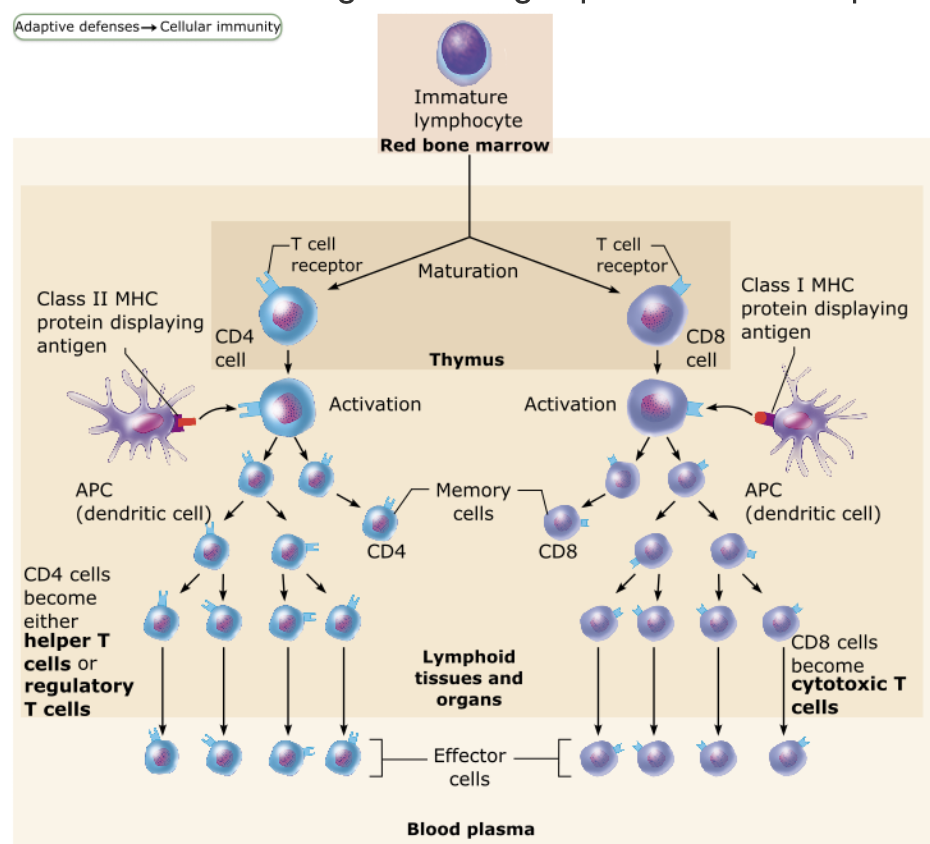
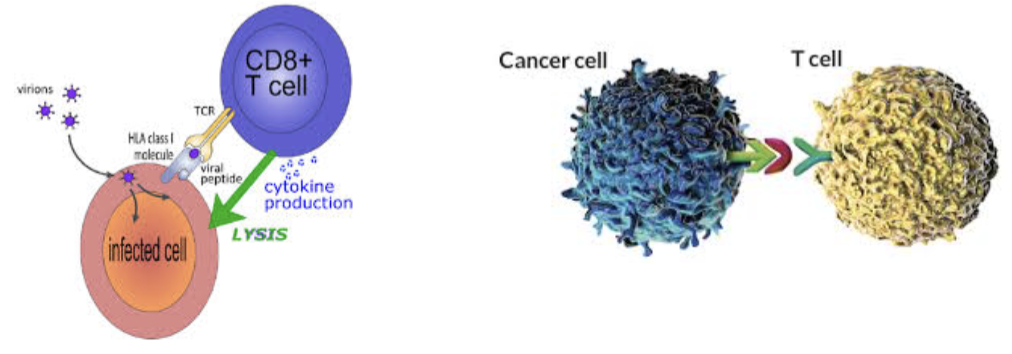
Define Cellular Immunity
T cells provide defense against intracellular antigens
EX: cells infected with viruses or bacteria, cancerous or abnormal cells, foreign (transplanted) cells
Function of T cells
Directly kill cells
Others release chemicals that regulate immune response
T/F: T cells are more complex than B cells both in classification and function
→ True
Name the Major Populations of T cells
Based on which cell differentiation glycoprotein receptors are displayed on their surface
CD4+ T cells
CD8+ T cells
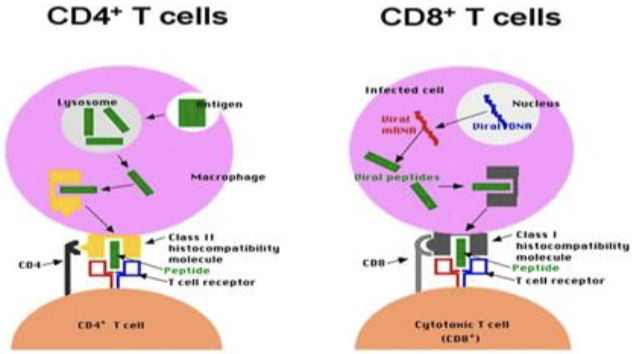
Function of CD4 cells
CD4 cells become helper T cells (TH) → that can activate B cells, other T cells, and macrophages
Direct adaptive immune response
Can also become memory T cells
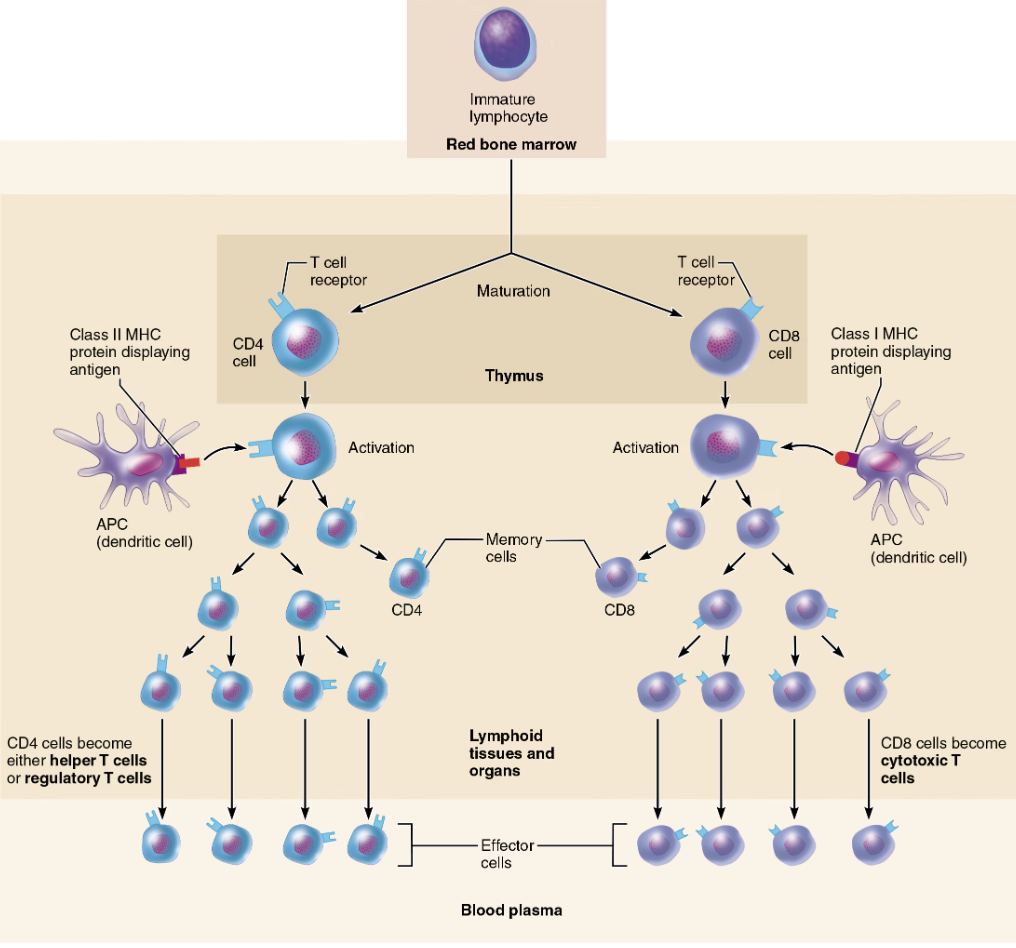
Function of CD8 cells
CD8 cells become cytotoxic T cells (TC) → that are capable of destroying cells haboring foreign antigens
Can also become memory T cells
Role of Helper, Cytotoxic, & Regulatory T cells
Activated T cells
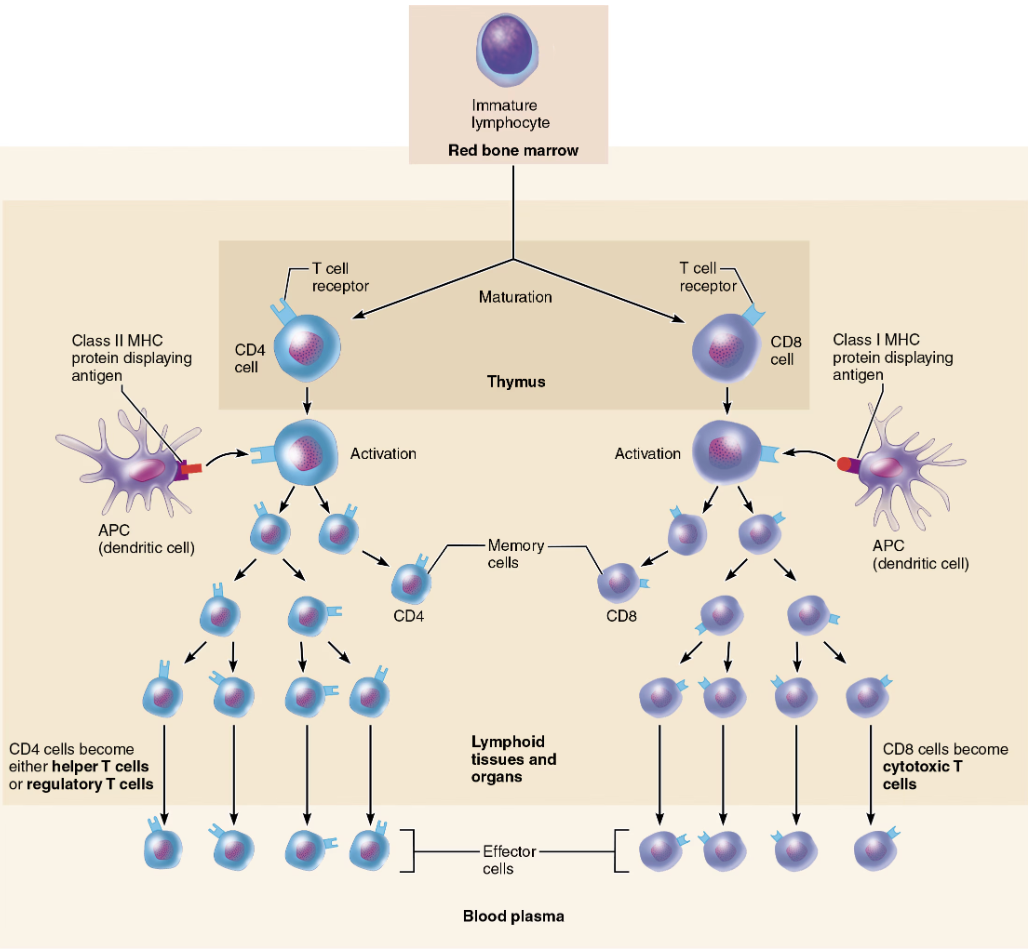
Define Naive T cells
Simply termed CD4 or CD8 cells

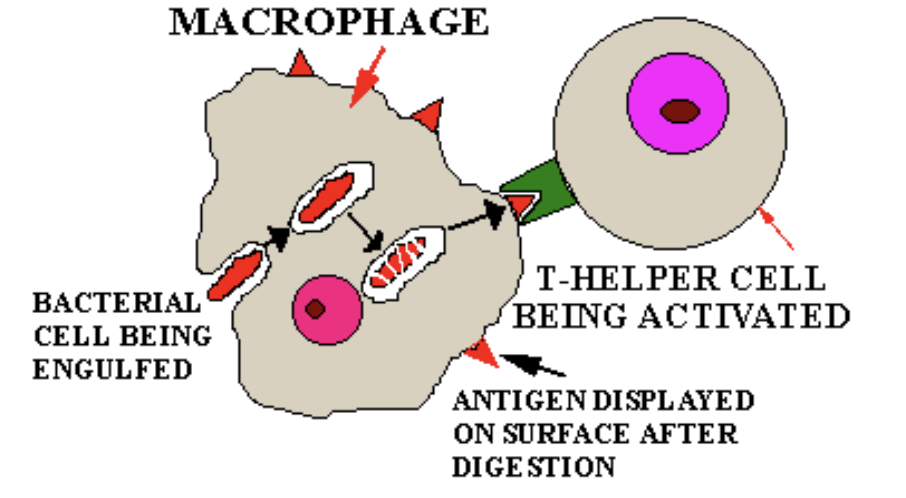
Role of MHC proteins
Antigen presentation through the use of MHC (Major Histocompatibility Complex) proteins is necessary for BOTH activation and functioning of T cells
Where does most exogenous antigen presentation take place?
Most exogenous antigen presentation to T cells occurs in lymphoid tissues and organs located throughout the body
Dendritic cells are primarily responsible for presenting antigens to T cells in these sites.
T/F: T cells can ONLY be activated by APCs
→ True
Explain the Activation of T cells
T cells respond only to processed fragments of antigens displayed on surfaces of cells by Major Histocompatibility Complex (MHC) proteins
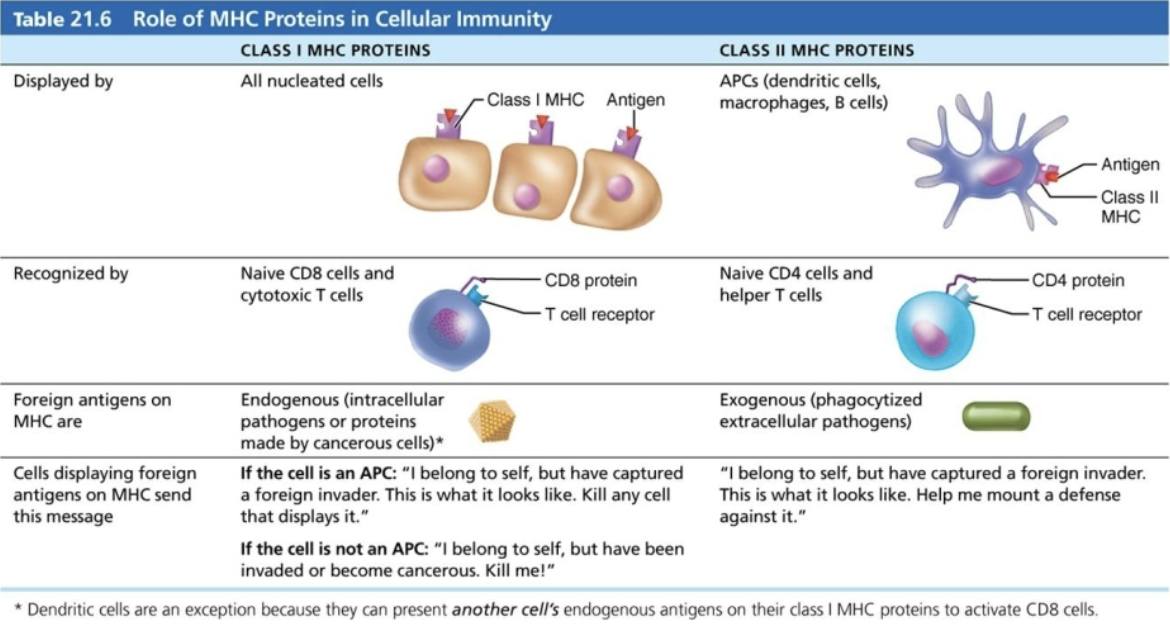
Name and Describe Two Classes of MHC Proteins
Class I MHC proteins
Displayed by ALL cells except RBCs
Antigens synthesized from within the cell
If infected → fragments of foreign antigens
FUNCTION → crucial for CD8 cell activation
Act as antigen holders → form “self” part that T cells recognize
Class II MHC proteins
Displayed by APCs (dendritic cells, macrophages, and B cells)
Antigens arising from outside the cell that are engulfed by the displaying cell
FUNCTION → recognized by helper T cells
Signal CD4 cells that help is required
BOTH types are synthesized in ER and bind to peptide fragments
Which of the following types of cells display protein fragments produced by the cancer within them?
ALL nucleated body cells bring pieces of endogenous proteins to the surface to display on the MHC protein
Class II MHC proteins are found on which of the following cell types?
Only on antigen-presenting cells
Which class of MHC proteins presents exogenous antigens?
II MHC proteins present antigens that originated from outside the cell (phagocytized extracellular pathogens)
Class I MHC proteins are recognized by which of the following cell types (that are destined to become Tcells)?
I MHC proteins are recognized by CD8 cells
T/F: BCR and TCR interact
→ FALSE
CD4 and MHC-II
BCR and epitope
CD8 and MHC-I
SUMMARY of Role of MCH Proteins in Cellular Immunity
Explain MCH Restriction
CD4 and CD8 cells have different requirements for MHC protein that presents antigens to them
CD4 cells that become TH are restricted to binding to ONLY II MHC (typically on APC surfaces) → Once activated, cytotoxic T cells seek out same antigen on class I MHC proteins on ANY cell
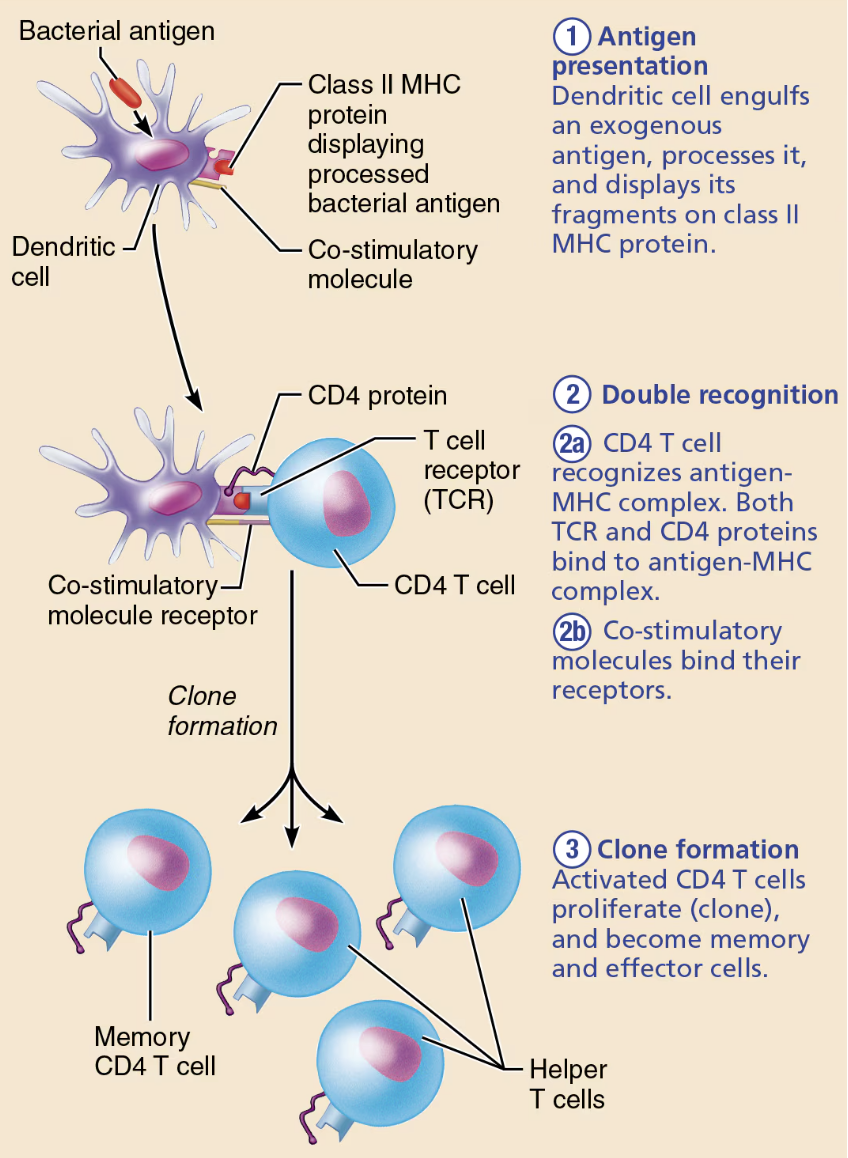
Describe the process of Activation and Clonal Selection of T cells.
Simultaneous recognition of self and non-self
Antigen presentation
Dendritic cell engulfs an exogenous antigen, processes it, and displays it fragments on class II MHC protein
Double recognition
CD4 T cell recognizes antigen-MHC complex → Both TCR and CD4 proteins bind to antigen-MHC complex
T cell must bind one or more co-stimulatory signals present on the antigen-presenting cell
Clone formation
Activated CD4 T cells proliferate (clone), and become memory and effector cells
Name the Major Groups of Effector T cells
Helper T cells
Cytotoxic T cells
Regulatory cells
Function of Helper T (TH) cells
Activate both
HumoralandCellulararmsOnce primed by APC presentation of antigen, helper T cells
Help activate B cells and other T cells
Induce T and B cell proliferation
Secrete cytokines that recruit other immune cells
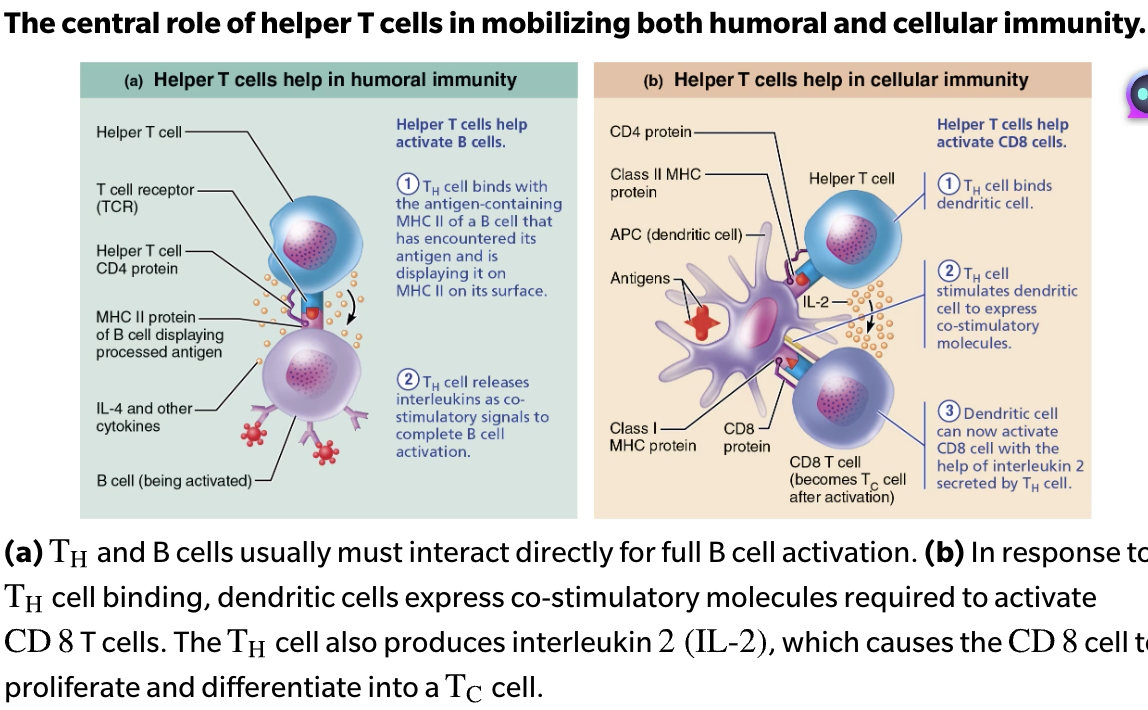
Which lymphocytes act as the bridge between the cellular and humoral responses?
Helper T cells are lymphocytes that organize the cellular and humoral immune response branches of the immune system.
Central Role of Helper T cells in Mobilizing Both Humoral and Cellular Immunity
Humoral Immunity
TH cell binds with the self-nonself complexes of a B cell that has encountered its antigen and is displaying it on MHC II on its surface
TH cell releases interleukins as co-stimulatory signals to complete B activation
Cellular Immunity
TH cell binds dendritic cell
TH cells stimulates dendritic cell to express co-stimulatory molecules
Dendritic cell can now activate CD8 cell with the help of interleukin 2 secreted by TH cell
Function of Cytotoxic T (TC) cells
Activated TC cells circulate in blood and lymph and lymphoid organs in search of body cells displaying antigen they recognize
Directly attack and kill other cells
List Activated TC cells Targets
Virus-infected cells
Cells with intraceullar bacteria or parasites
Cancer cells
Foreign cells (transfusion or transplants)
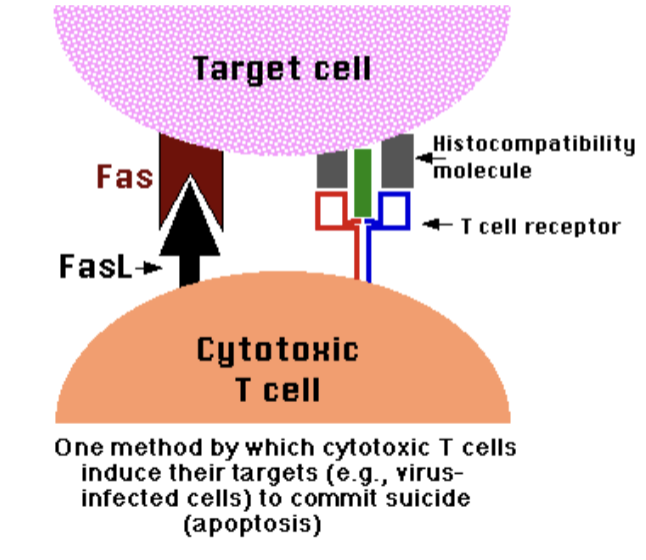
Describe Steps Cytotoxic T cells Attack Mechanism
TC identifies foreign antigens on MHC I proteins and binds tightly to target cell
TC releases perforin and granzyme molecules from its granules by exocytosis
Perforin molecules insert into the target cell membrane, polymerize, and form transmembrane pores (cylindrical holes) similar to those produced by complement activation
Granzymes enter the target cell via the pores → Once inside, granzymes activate enzymes that trigger apoptosis
The TC detaches and searches for another prey
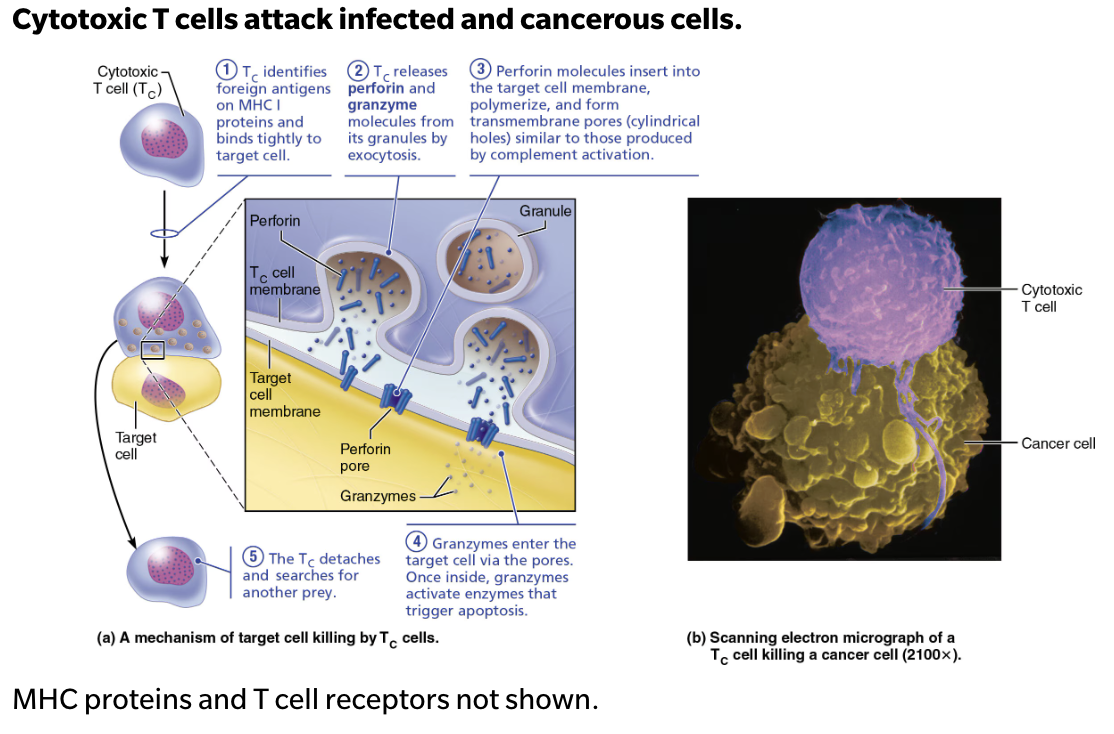
T/F: A step used by cytotoxic T cells to kill infected host is recognition of infected host cell using its CD4 glycoprotein
→ FALSE
The cytotoxic T cell uses its CD8 glycoprotein to bind to the MHC-I of an infected host cell.
Recognition of infected host cell using its TCR
Secretion of granzyme
Secretion of perforin
T/F: T cells can become effector cells and memory cells
→ FALSE
T cells can become effector cells OR memory cells
Similar like B cells
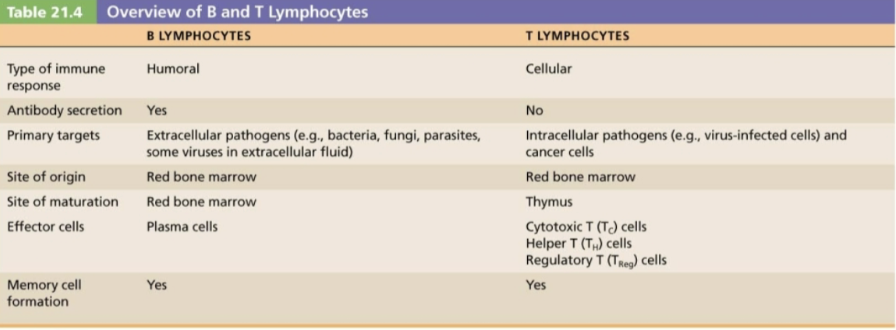
Describe the roles of different types of T cells
Helper T cells
Effector CD4 T cell
Central to both humoral and cellular immunity → Stimulate proliferation of other T cells and B cells that have already become bound to antigen
Cytotoxic T cells
Effector CD8 T cell
ONLY T cells that can directly attack and kill other cells displaying antigen to which they have been sensitized, through the use of perforin and granzymes, or by triggering apoptosis of the target cell
Regulatory cells
Effector CD4 T cell
Either by direct inhibition or by causing the release of cytokines, suppress the activity of both B cells and other types of T cells
Sequence of Cellular Immunity
Dendritic cells activate CD4 cells
Activated CD4 cells form a clone of Helper T (TH) cells and memory cells
Helper T cells and dendritic cells activate CD8 cells
Activated CD8 cells form a clone of Cytotoxic T (TC) cells and memory cells
A person who has AIDS contracts rare and often life-threatening infections because their helper T cell count is so low. Which of the following components of the immune response still respond to antigen despite the low helper T cell count?
Clonal selection of B cells → However, without a helper T cell, clonal expansion and antibody production will not occur
Define Allograft
Most common type of organ transplant (from same species)
What determines Transplant Success Depends?
Success depends on similarity of tissues
ABO, Other blood antigens, MHC antigens are matched as closely as possible
WHY → Cytotoxic T cells, NK cells, and antibodies work to destroy foreign tissues
Explain Immunosuppressive Therapy
After surgery
Patient treated with immunosuppressive therapy → to suppress rejection
Many of these therapies have severe side effects → weakened immune system
What happens when Patient’s immune system is suppressed?
Cannot protect body from foreign agents such as bacterial and viral infections → Leading cause of death among transplant recipients
Best circumstances → rejection after 10 years in
SUMMARY of Cells and Molecules of the Adaptive Immune Response
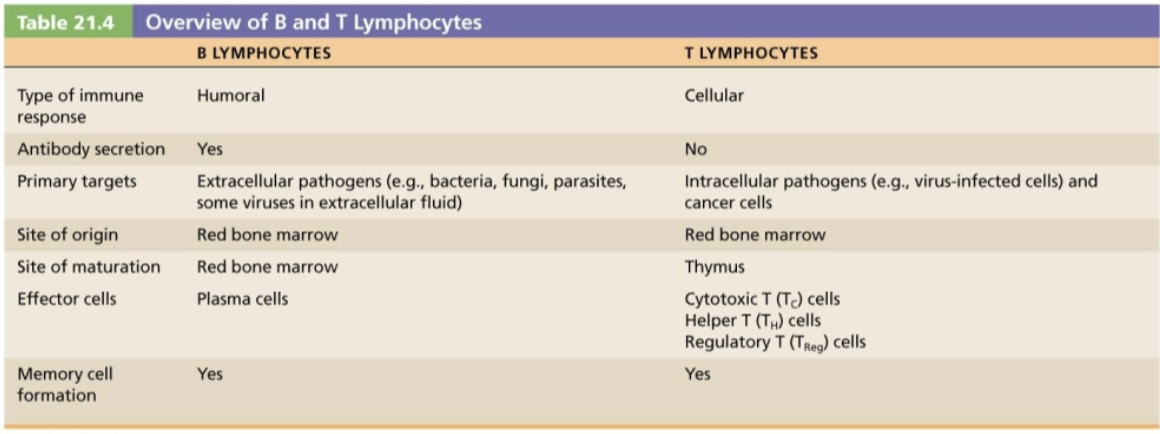
SUMMARY B & T Lymphocytes
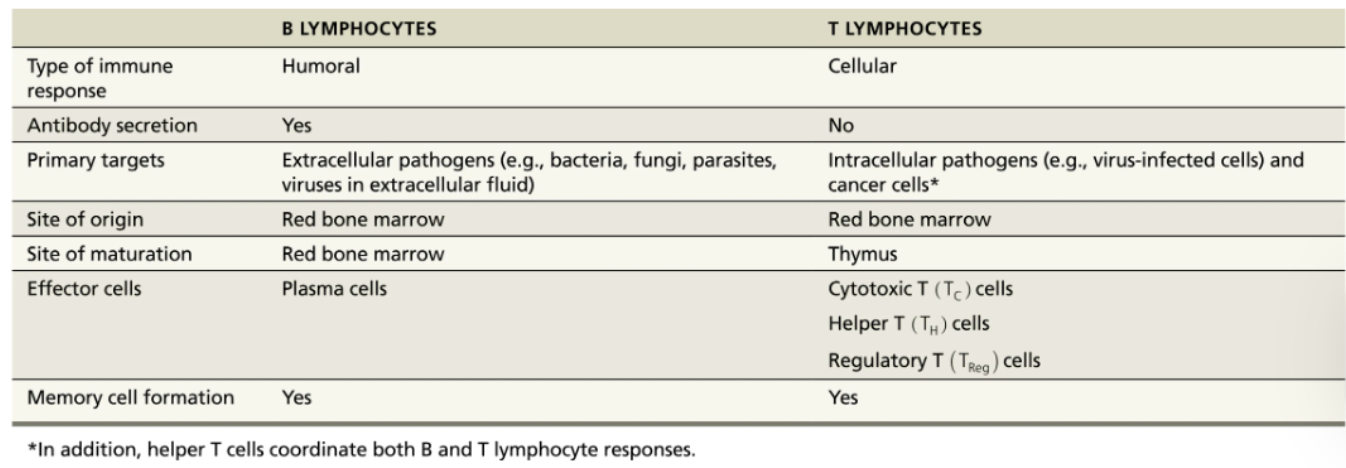
Which specific type of cell produces antibodies?
Activated plasma cells
When activated by the presence of antigens, B lymphocytes proliferate into plasma cells
Plasma cells generate antigen-specific antibodies.
How do cytotoxic cells directly attack target cells?
Cytotoxic cells bind to the target cell and secrete chemicals that induce apoptosis
Cytotoxic cells are able to dock with antigens on the target cell membrane
Once docked, the cytotoxic cell releases perforins and granzymes, which weaken the cell membrane and induce apoptosis
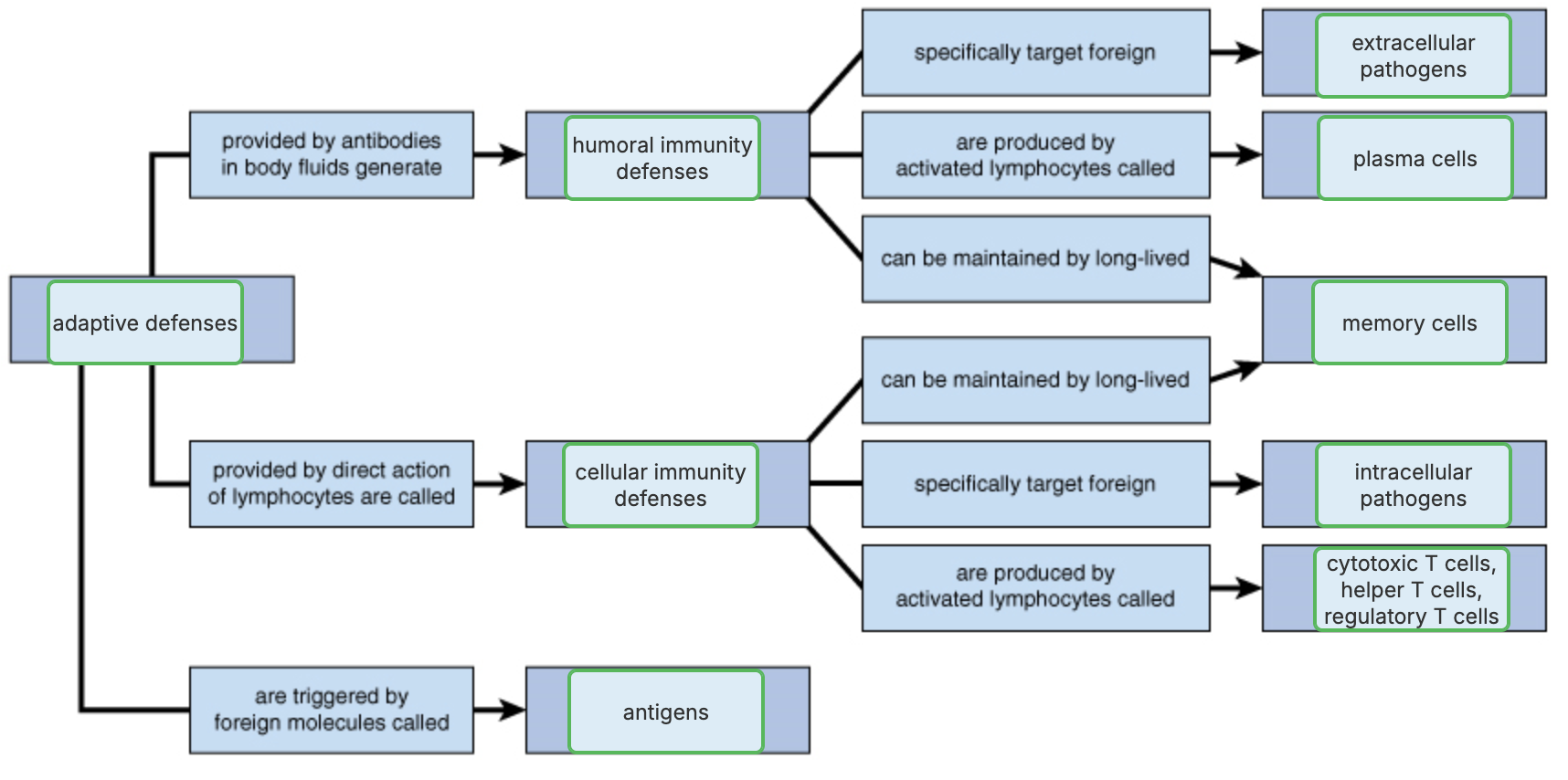
SUMMARY of ADAPTIVE DEFENSES
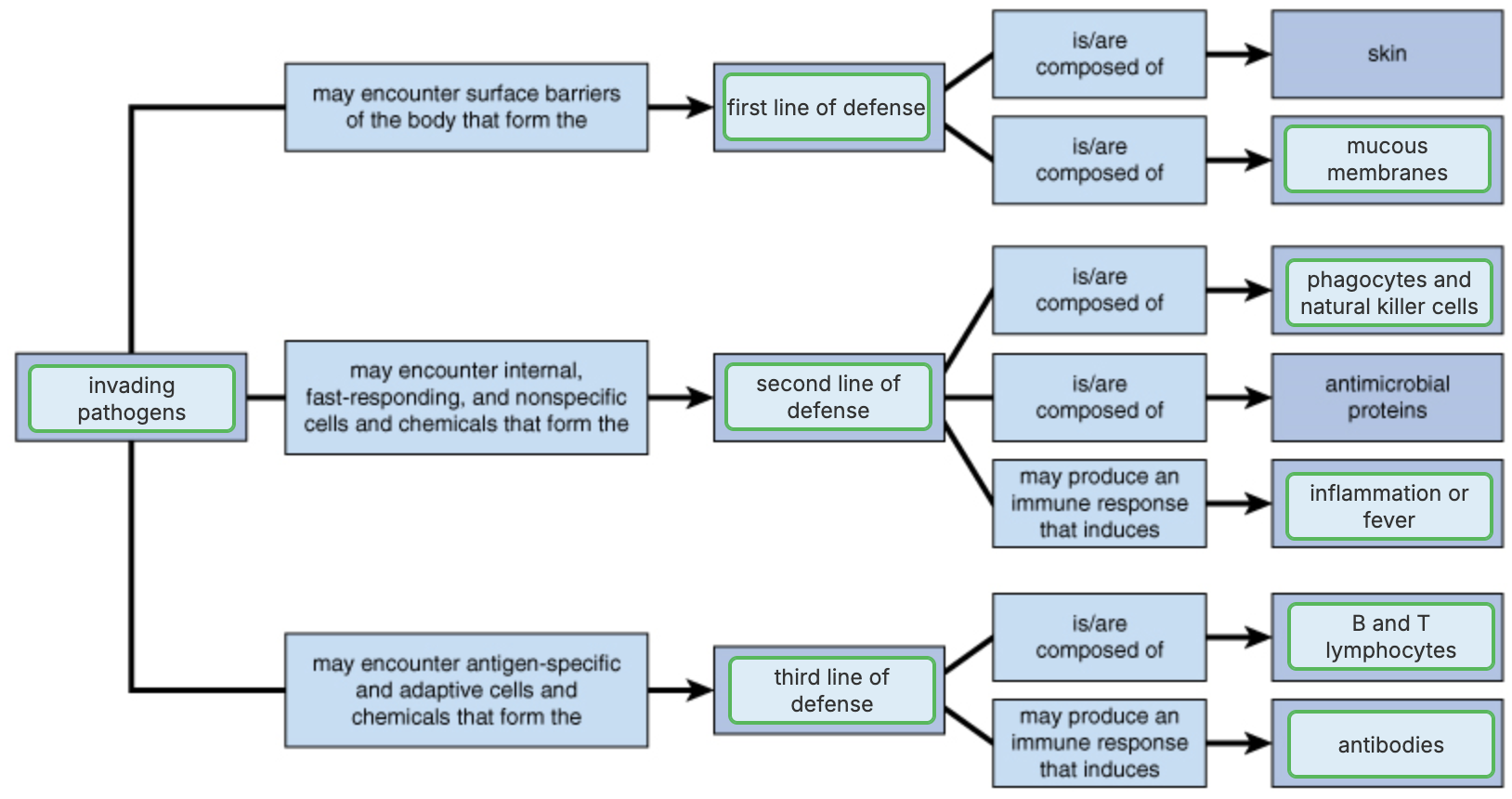
SUMMARY of 1st, 2nd, 3rd Line of Defense
SUMMARY of Key Differences between Adaptive & Innate Defenses
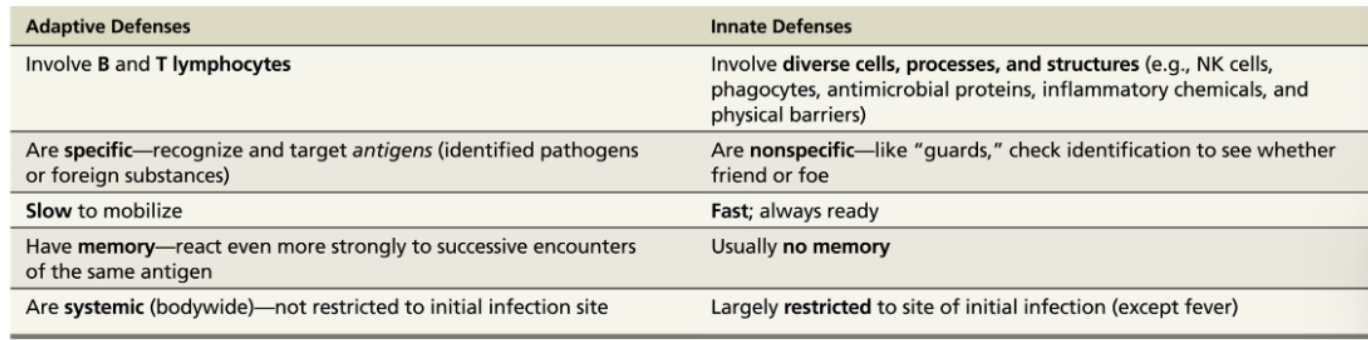
Tears and mucous membranes would be a part of which defense system?
Innate external defenses → (surface barriers) are the first line of defense and include tears, mucous membranes, and the skin
Phagocytotic cells such as macrophages identify a variety of enemies by recognizing markers unique to pathogens. They would be classified as which type of defense system?
Innate internal defenses
What type of immunity can be transferred by bodily fluids from one person to another, thus conferring immunity to the recipient?
Humoral immunity → involves antibodies that can be transferred from one person to another.
If a virus attacks a cell, which type of immunity would be activated?
Cell-mediated immunity → involves an intracellular pathogen such as a virus