Ella Kulman Neurology
1/162
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
163 Terms
Give 3 examples of a primary headache
1. migraine
2. tension headache
3. cluster headache
Give 4 examples of a secondary headache
1. meningitis
2. subarachnoid haemorrhage
3. giant cell arteritis
4. medication overuse headache
give potential red flags for suspected brain tumour in a pt presenting with headache
1. new onset and hx of cancer
2. cluster headache
3. seizure
4. significantly altered consciousness, memory, confusion
5. papilloedema - swollen optic disc
6. other abnormal neuro exam
How long do migraine attacks tend to last?
4-72 hours
describe the pain of a migraine
1. unilateral
2. throbbing
3. moderate/severe pain
4. aggravated by physical activity
Would a pt with migraine experience any other symptoms?
photophobia and/or phonophobia are common complaints. may have nausea but not vomiting
what % of migraines are with/out aura?
20% with, 80% without
what would a pt experiencing migraine with aura complain of?
-visual disturbances e.g. flashing lights, zig-zag lines
-sensory disturbances e.g. tingling in hands/feet
-language aura and motor aura
describe treatment for migraine (non/pharmacological)
-lifestyle modification and trigger management
-PO triptan and NSAIDs
-anti emetics
-preventative treatments: propranolol, acupuncture, amitriptyline
how long do tension headaches usually last for?
30 mins - 7 days
describe the pain of a tension headache
1. bilateral
2. pressing/tight
3. mild/moderate pain
4. not aggravated by physical activity
would a pt with a tension headache experience any other symptoms?1
no!
what is the diagnostic criteria for medication overuse headache?
-headache present for >15 days/months
-regular use for 3mths+ of 1+ symptomatic treatment drugs
-headache has developed or markedly worsened during drug use
describe the pain of a cluster headache
-severe/very severe pain
-pain around the eye/temporal area
-unilateral
-headache accompanied by cranial autonomic features
how long do cluster headaches usually last?
15mins - 3hours
what features present in a history may indicate meningitis?
-pyrexia
-photophobia
-neck stiffness
-non-blanching purpura rash
investigations for suspected meningitis:
-bloods: FBC, U+E, CRP, serum glucose, lactate
-blood cultures
-throat swab
-lumbar puncture
-CT head
how would you describe the headache associated with sub-arachnoid haemorrhage?
thunderclap headache - maximum severity within seconds
describe the management for subarachnoid haemorrhage
1. resuscitation
2. nimodipine - CCB
3. early intervention and close monitoring will improve prognosis
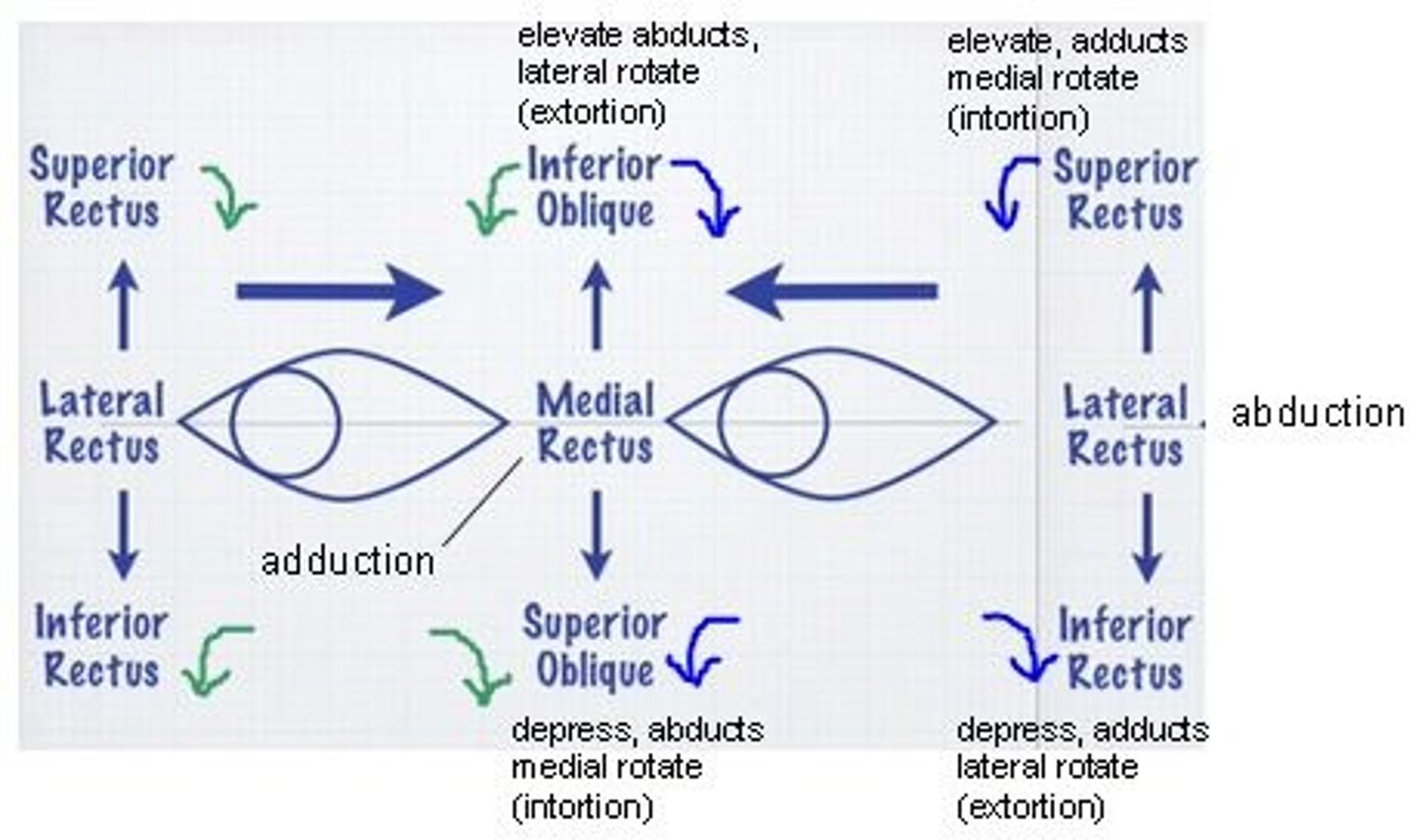
what muscle needs to be working in order to test the action of superior and inferior rectus?
lateral rectus
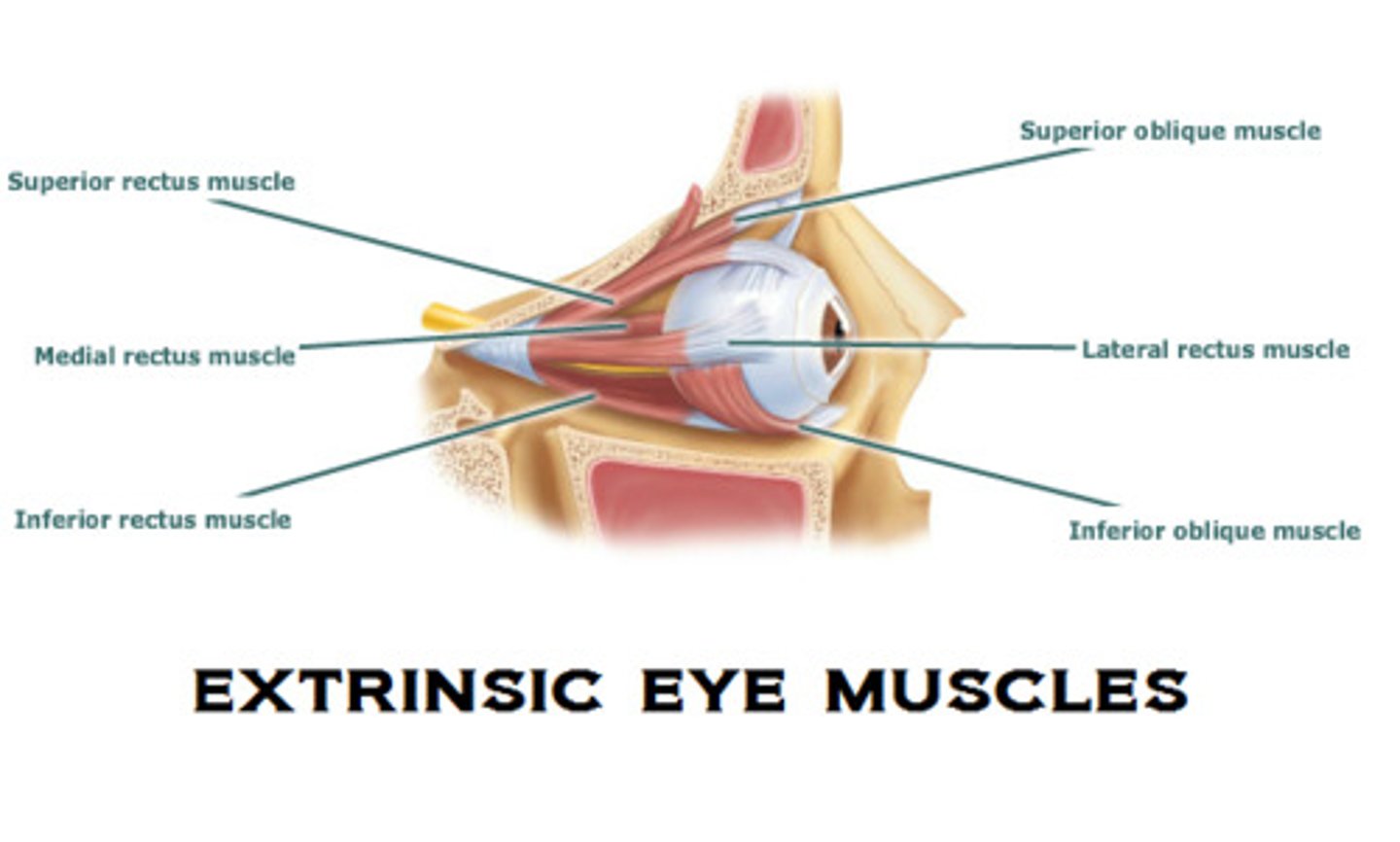
superior and inferior oblique can never be isolated in action. how can they be tested?
position the eye so that superior and inferior recti are giving maximal rotation, and look for complete correction
name 3 organisms that can cause meningitis in adults
1. N.meningitidis (g-ve diplococci)
2. S.pneumoniae (g+ve cocci chain)
3. Listeria monocytogenes (g+ve bacilli)
name 3 organisms that can cause meningitis in children
1. E. coli (g-ve bacilli)
2. group B streptococci (e.g. s.agalactiae)
3. Listeria monocytogenes
give symptoms of meningitis
1. non-blanching petechial rash
2. neck stiffness
3. headache
4. photophobia
5. papilloedema
6. fever
what antibiotic is commonly given to treat meningitis?
cefotaxime
for which bacteria is meningitis prophylaxis effective against?
N.meningitidis
What can be given as prophylaxis against N.meningitidis infection?
Ciprofloxacin
at what vertebral level would you do a lumbar puncture?
L4/5
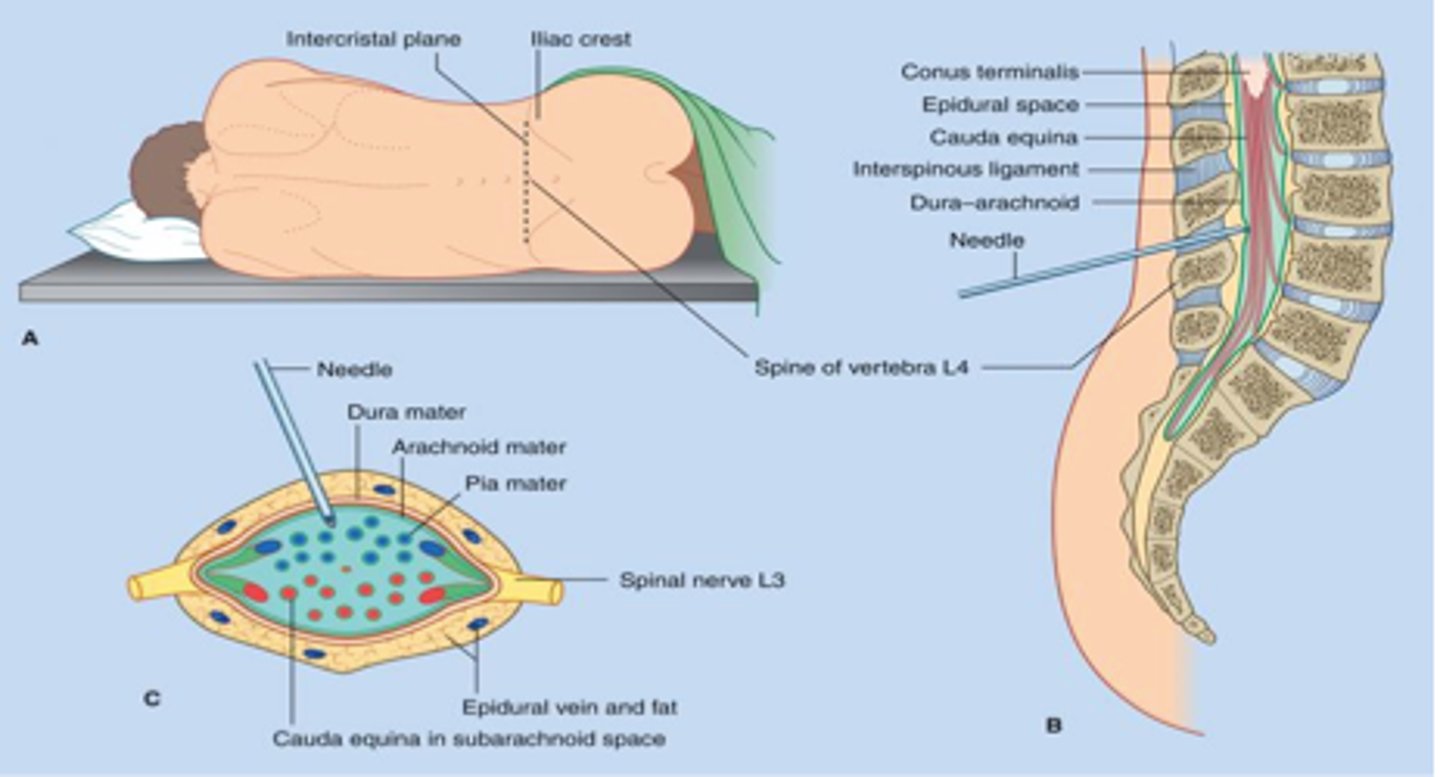
give 4 potential adverse effects of doing a lumbar puncture
1. headache
2. damage to spinal cord
3. paraesthesia
4. CSF leak
what investigations would you do on a CSF sample?
-protein and glucose levels
-MCS
-bacterial and viral PCR
what is the most common cause of viral meningitis?
enterovirus
what is the colour of CSF in someone with bacterial infection?
cloudy (it is normally clear)

give symptoms of encephalitis
-fever
-headache
-lethargy
-behavioural change
treatment for encephalitis
acyclovir
Give 5 symptoms of rabies
1. Fever
2. Anxiety
3. Confusion
4. Hydrophobia
5. Hyperactivity
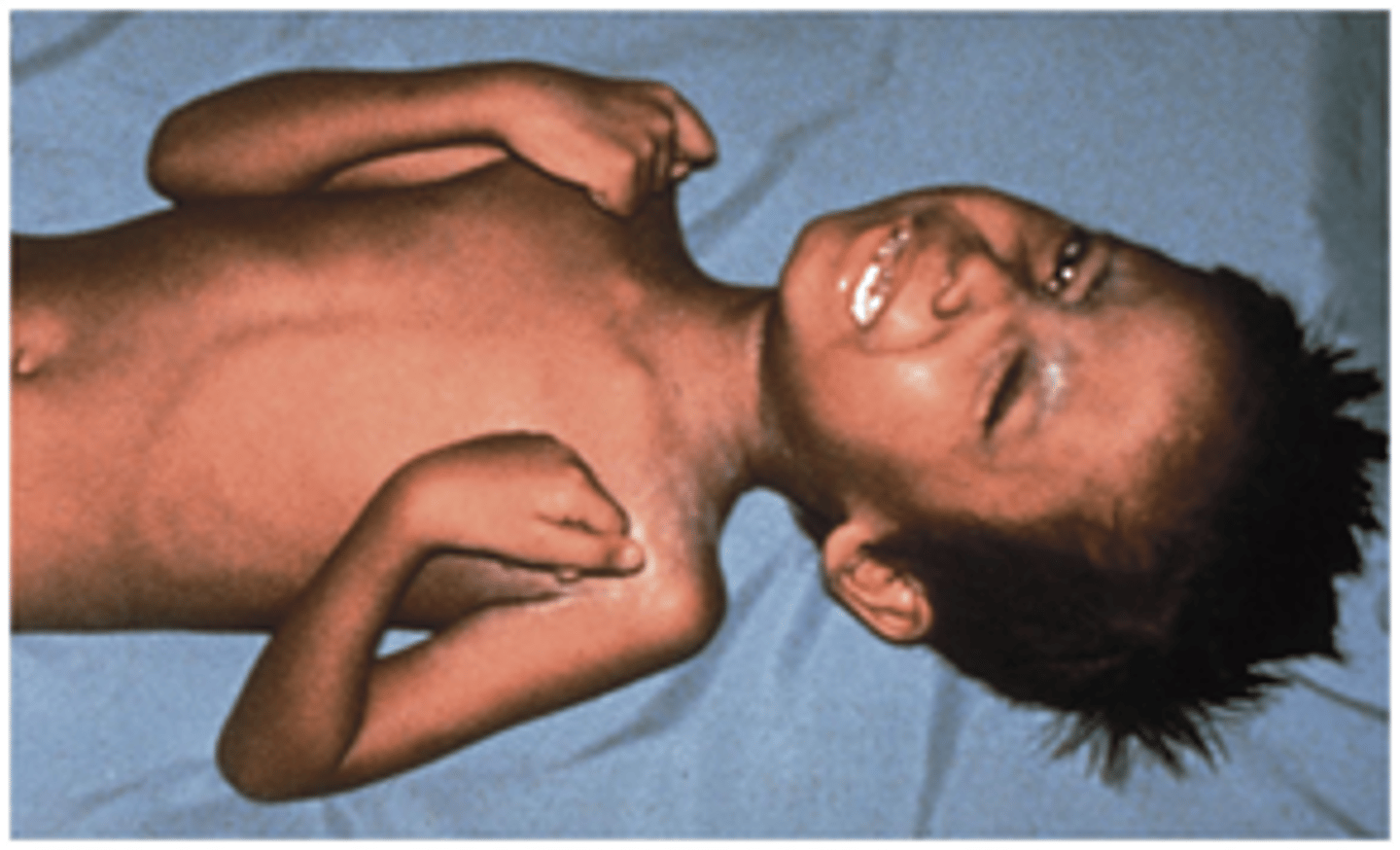
Name the organism responsible for causing tetanus
Clostridium tetani (gram +ve anabrose) → infects via dirty wounds
3 symptoms of tetanus
1. Trismus (lockjaw)
2. Sustained muscle contraction
3. Facial muscle involvement
It a pt has aphasia, what region of the brain has been affected?
Broca's area
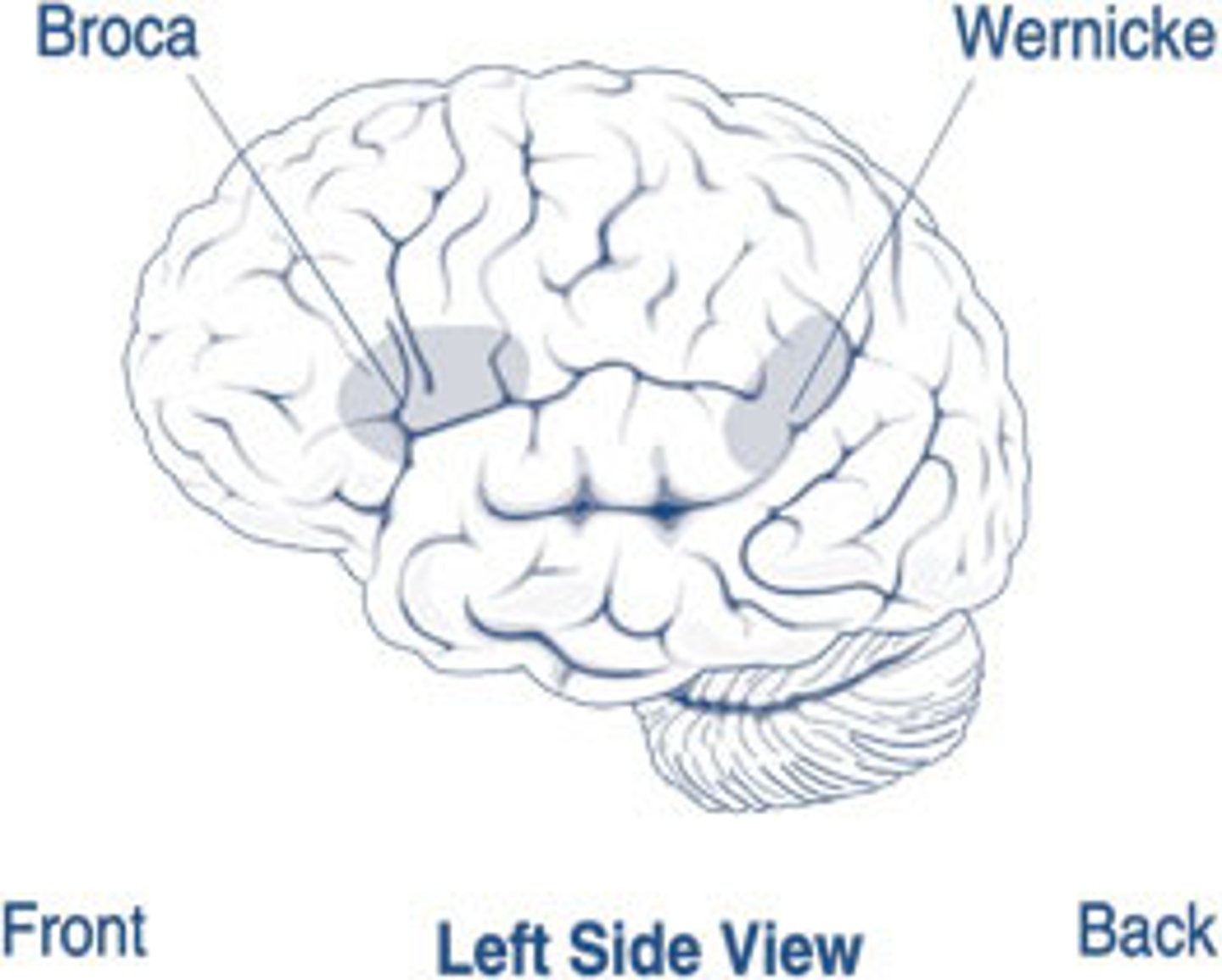
If a pt has receptive dysphagia what region of the brain has been affected?
Wernicke's area
Name 3 intracranial haemorrhages
1. Extra-dural
2. Sub-dural
3. Sub-arachnoid
What can cause sub-arachnoid haemorrhages?
rupture of a berry aneurysm around the circle of Willis
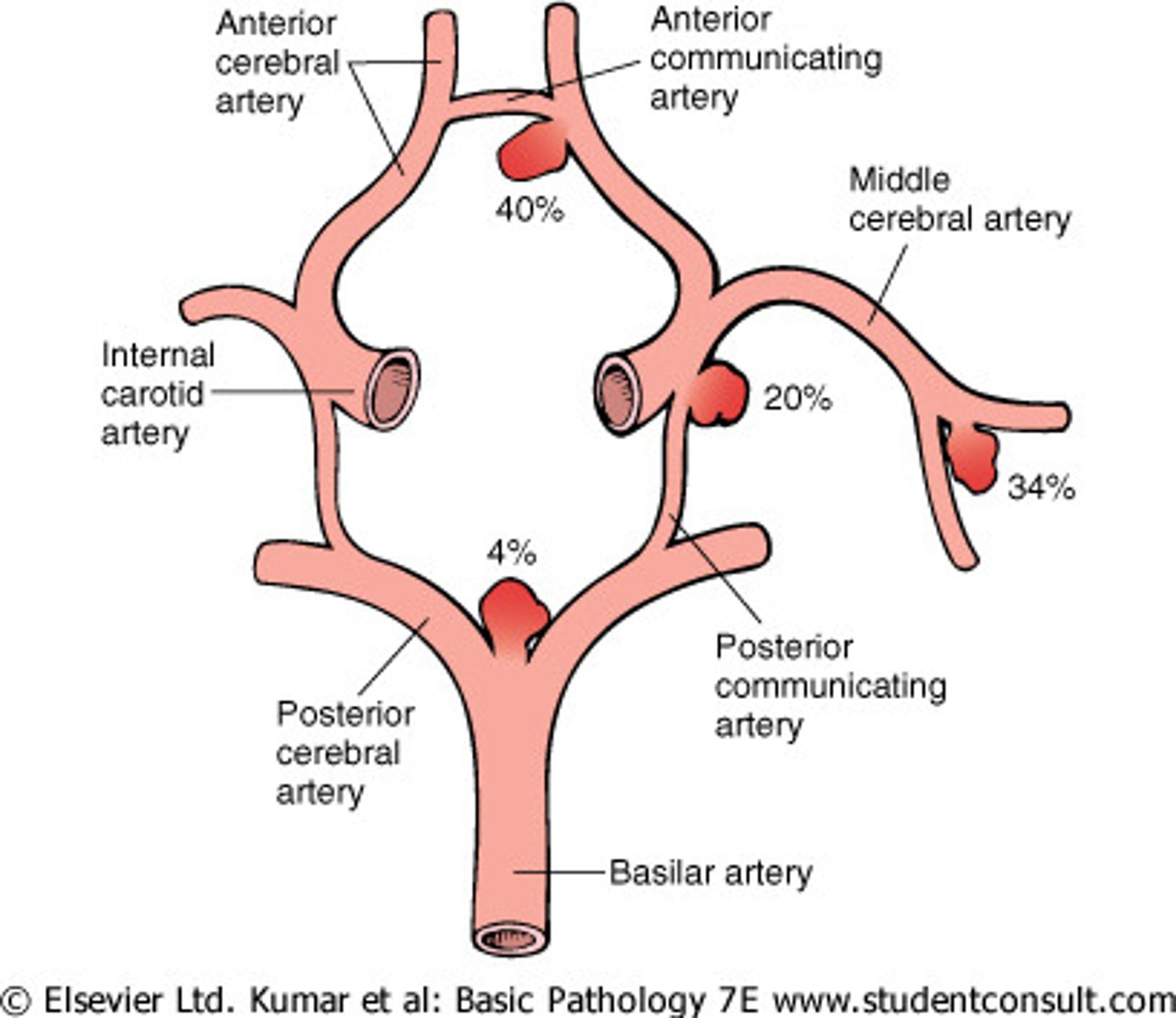
Give 5 symptoms of a sub-arachnoid haemorrhage
1. Sudden onset 'thunderclap' headache
2. Photophobia
3. Reduced consciousness
4. Neck stiffness
5. Nausea and vomiting
What is the treatment for a sub-arachnoid haemorrhage?
- Bed rest and BP control
- CCB to prevent cerebral artery spasm
- IV saline
what can cause a sub-dural haematoma?
head injury → vein rupture
Describe the natural history of a sub-dural haematoma
Latent period after the head injury. 8-10 weeks later the clot starts to breakdown, and there is a massive increase in oncotic pressure, water is sucked up into the haematoma → signs and symptoms develop. There is a gradual rise in ICP
3 symptoms of sub-dural haematoma
1. Headache
2. Drowsiness
3. Confusion
Treatment for a sub-dural haematoma?
surgical removal
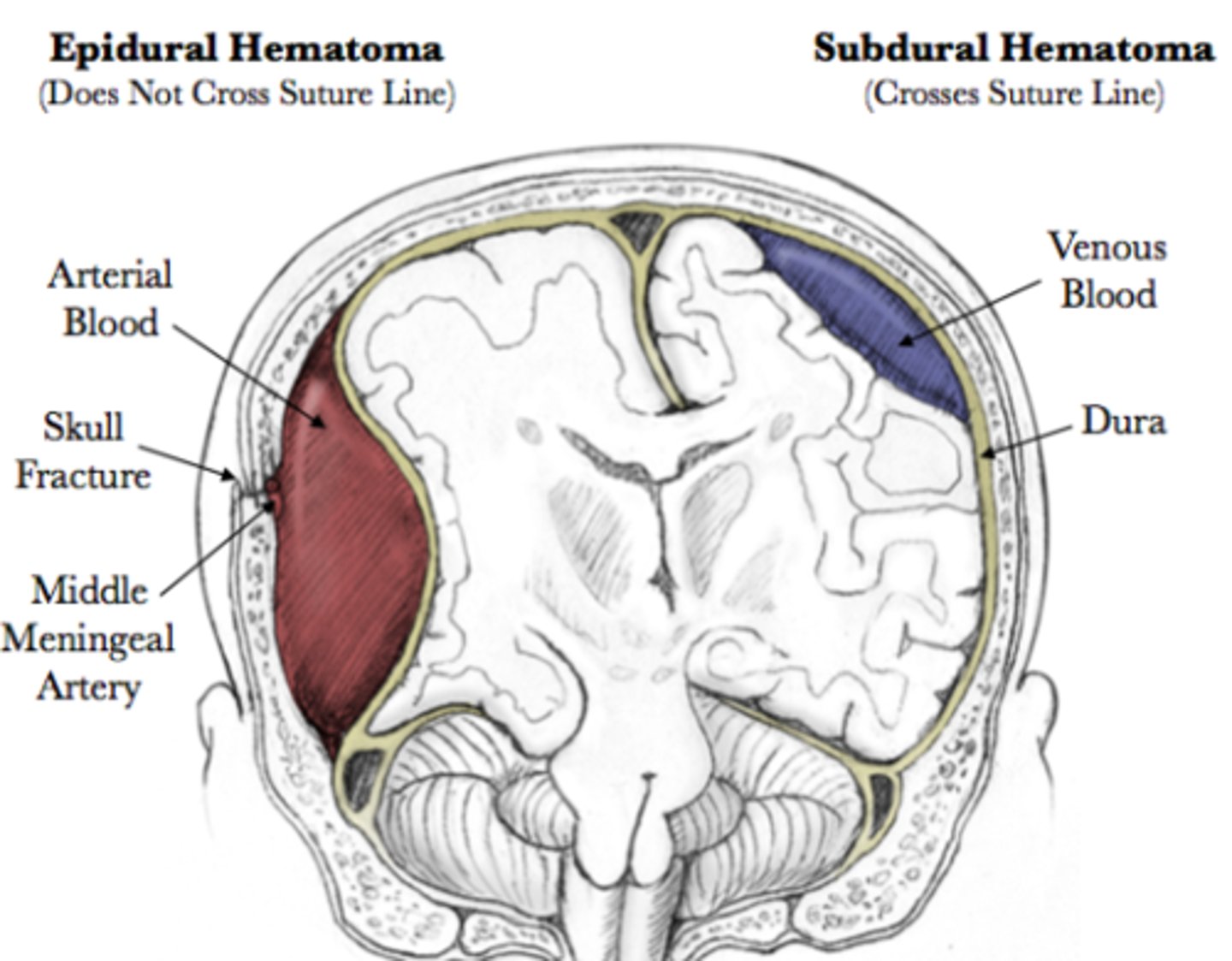
What can cause an extra-dural haematoma?
Trauma to the temporal bone → bleeding from the middle meningeal artery
What do ventricles do to prolong survival in someone with an extra-dural haemorrhage?
The ventricles get rid of their CSF to prevent the rise in inter-cranial pressure
What is the treatment for an extra-dural haematoma?
Immediate surgical drainage
give 2 primary causes of intra-cerebral haemorrhage
1. hypertension → berry or Charcot-Bouchard aneurysms rupture
2. lobar (amyloid angiopathy)
give 5 secondary causes of an intra-cerebral haemorrhage
1. tumour
2. arterio-venous malformations (AVM)
3. cerebral aneurysm
4. anticoagulants e.g. warfarin
5. haemorrhagic transformation infarct
what is the most likely cause of bleeds in the basal ganglia, pons and/or cerebellum?
hypertension
describe the treatment for anti-coagulant related intra-cerebral haemorrhage
check warfarin INR (test for how long it takes for your blood to clot) and consider reversal with vitamin K
*if platelets low → platelet transfusion
define stroke
rapid onset of neurological deficit which is the result of a vascular lesion and is associated with infarction of CNS tissue
what can cause a stroke?
1. cerebral infarction due to embolus or thrombosis (85%)
2. intracerebral/sub-arachnoid haemorrhage (15%)
give risk factors for stroke
-hypertension
-diabetes mellitus
-cigarettes
-hyperlipidaemia
-obesity
-alcohol
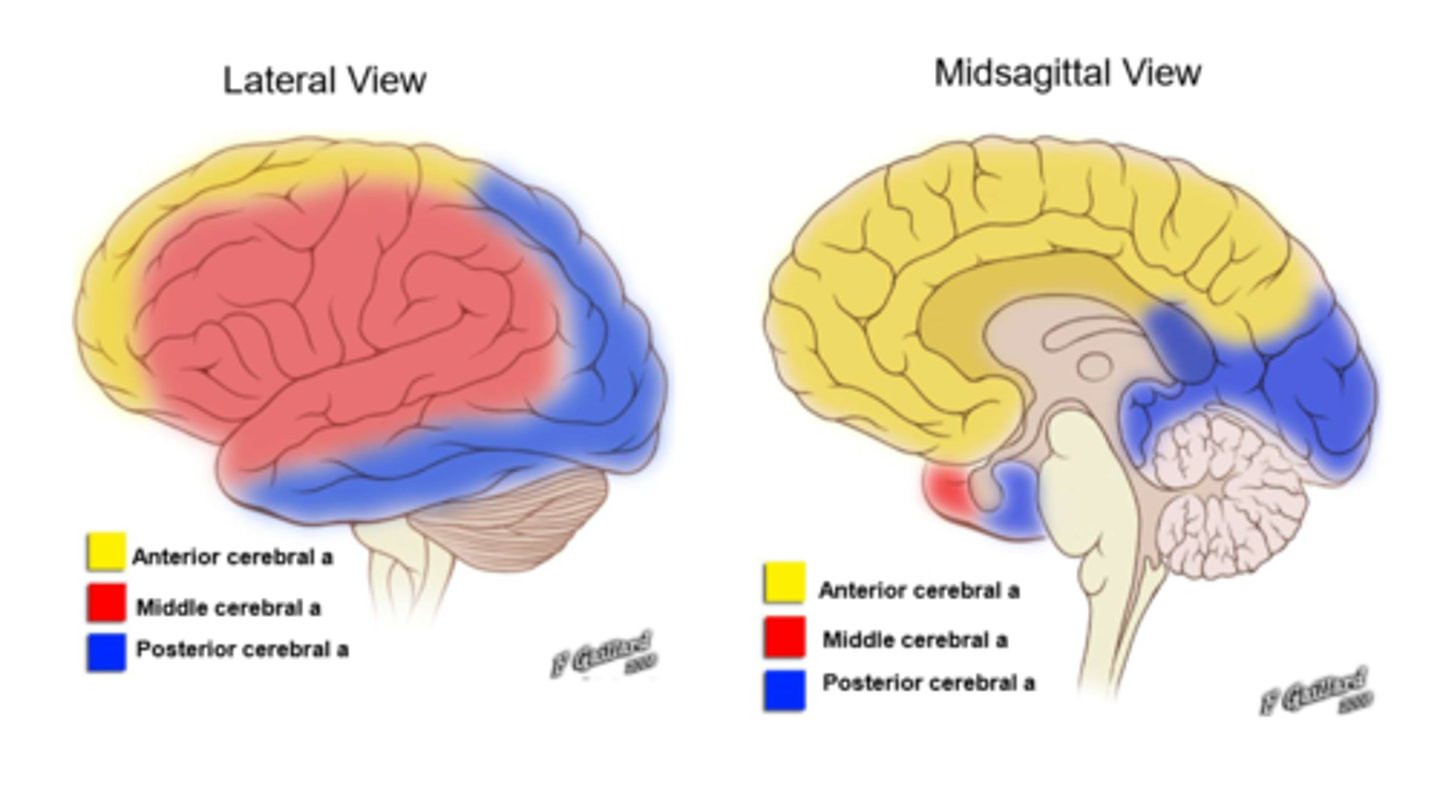
signs of an ACA stroke
-lower limb weakness/loss of sensation
-gait apraxia (unable to initiate walking)
-incontinence
-drowsiness
-decrease in spontaneous speech
what does the ACA supply?
medial surface of frontal and parietal lobes
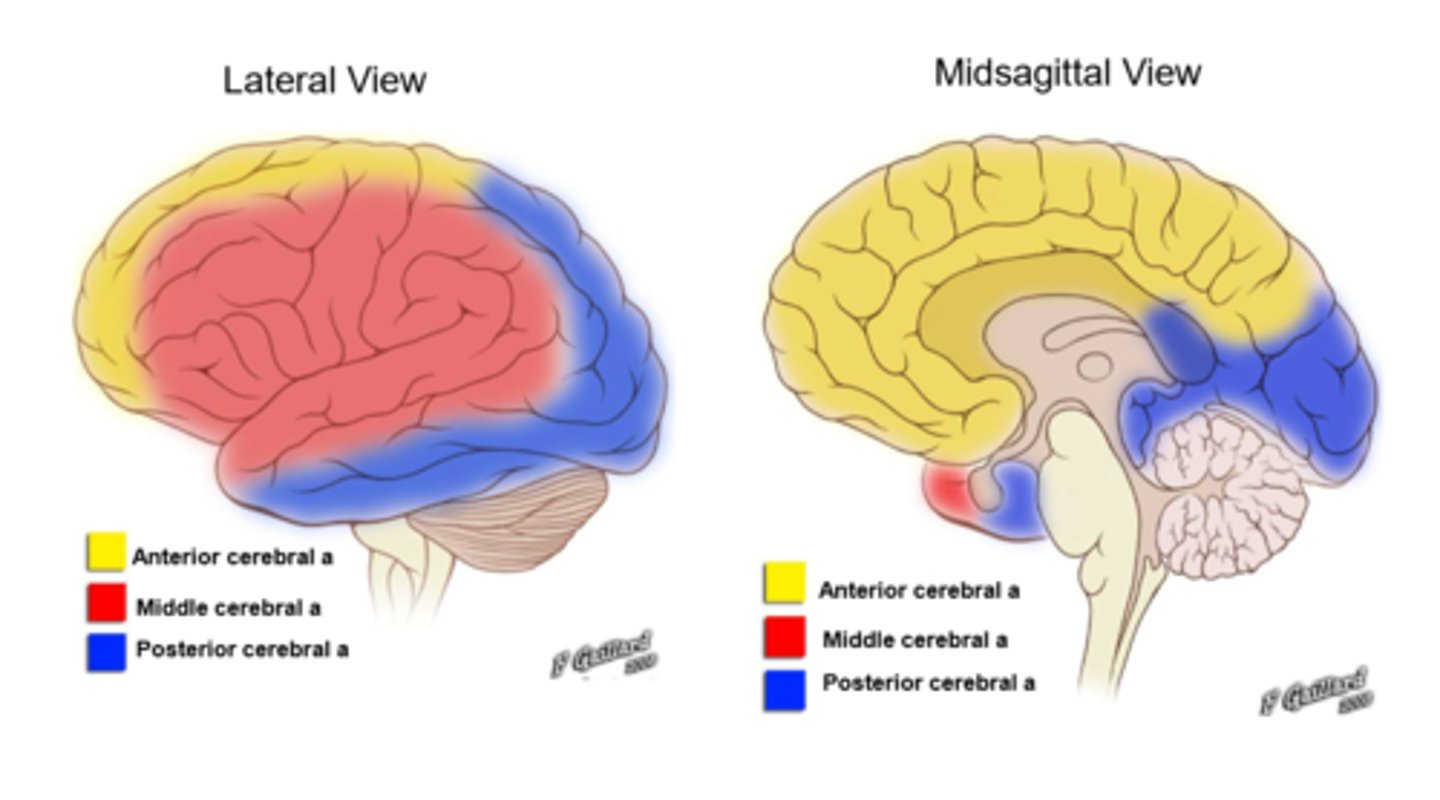
signs of a MCA stroke
-upper limb weakness/loss of sensation
-hemianopia
-aphasia (difficulty with speech/language)
-dysphasia (impairment in speech production)
-facial drop
What does the MCA supply?
Most of the lateral cortex,
speech/language/swallowing
& Broca/Wernicke
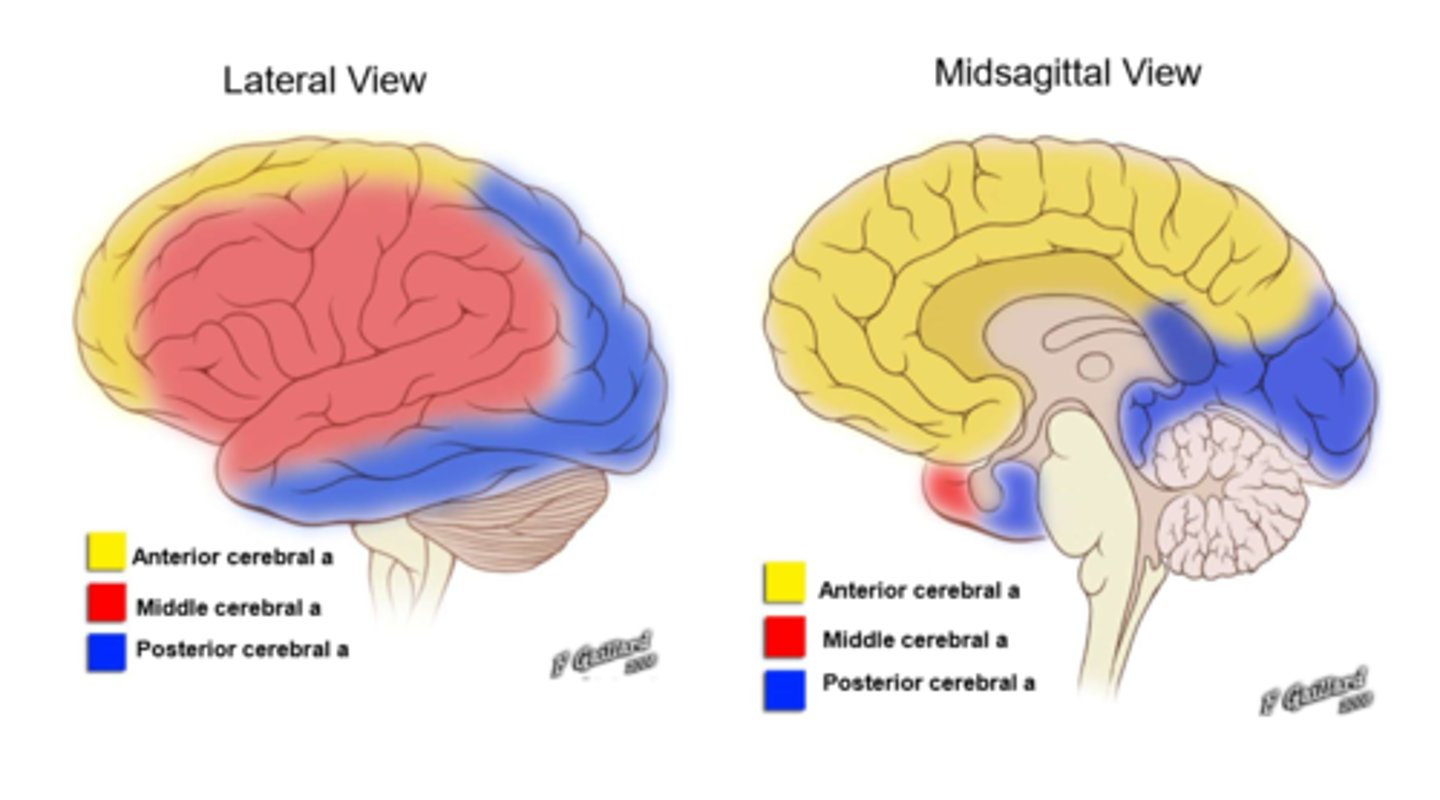
signs of a PCA stroke
-visual field defects
-cortical blindness (total/partial blindness in a normal-appearing eye)
-visual agnosia (impairment in recognition of visually presented objects)
-prosopagnosia (impairment in processing information about faces)
-dyslexia
-unilateral headache
What does the PCA supply?
occipital lobe
what is visual agnosia?
an inability to recognise/interpret visual info
what is prosopagnosia?
inability to recognise a familiar face
pt presents with weakness and loss of sensory sensation to the upper limb, aphasia and facial drop. which artery is likely to have been occluded?
middle cerebral artery
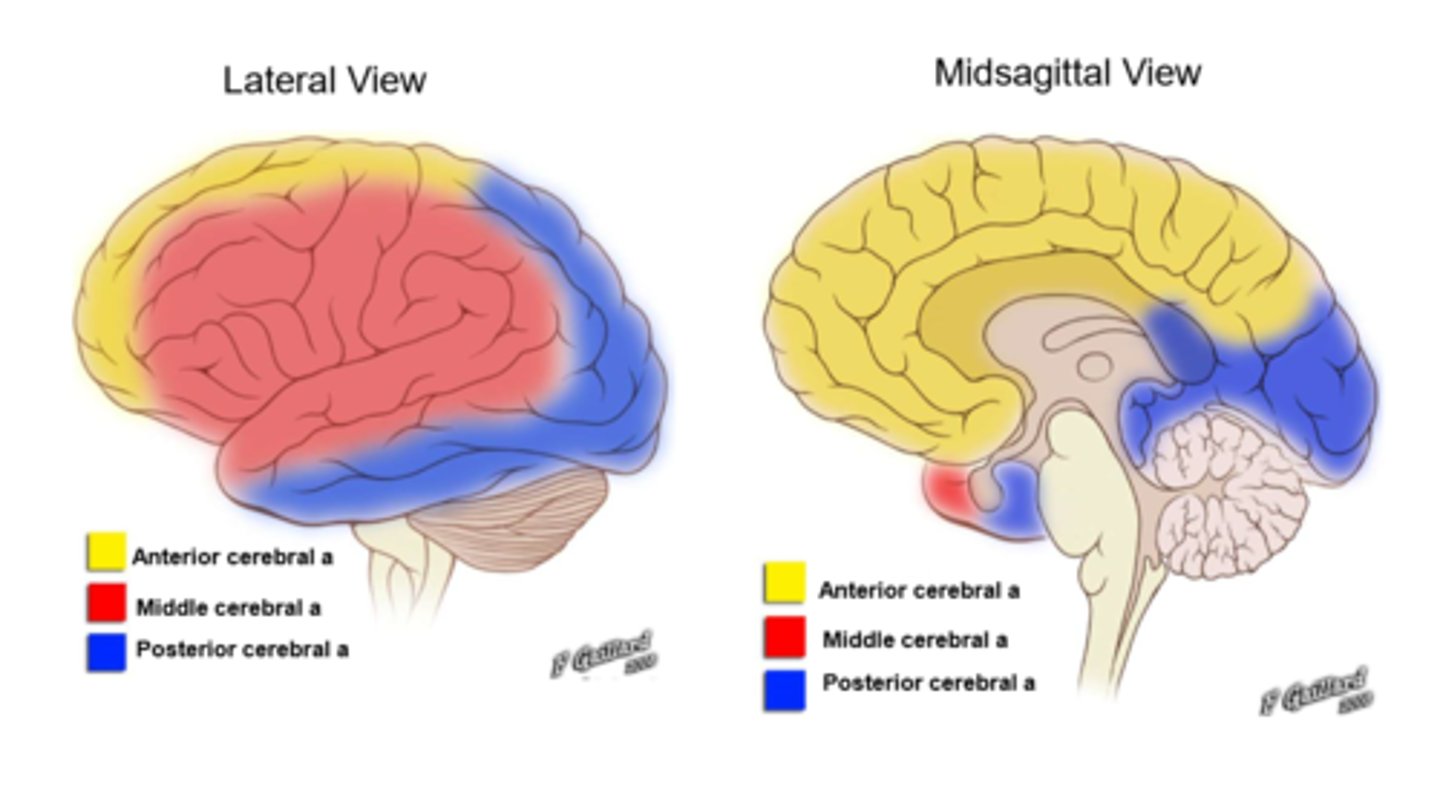
pt presents with weakness and loss of sensory sensation to the lower limb, incontinence, drowsiness and gait apraxia. which artery is likely to have been occluded?
anterior cerebral artery
pt presents with contralateral homonymous hemianopia, they are unable to recognise familiar faces and complain of a headache on one side of their head. which artery is likely to have been occluded?
posterior cerebral artery
what is the treatment for ischaemic stroke?
thrombolysis e.g. alteplase → IV infusion to break up the clot
what is MS?
a chronic auto-immune disorder of the CNS. it's an inflammatory and demyelinating disease characterised by progressive disability
where would MS plaques be seen histologically?
around blood vessels: perivenular
does myelin regenerate in someone with MS?
yes, but it is much thinner which causes inefficient nerve conductions
give 3 major features of an MS plaque?
1. inflammation
2. demyelination
3. axon loss
describe the relapsing/remitting course of MS
pt has a number of random attacks over a number of years, between attacks there is no disease progression
describe the chronic progressive course of MS
slow decline in neurological functions from the onset
what can exacerbate the symptoms of MS?
heat → typically a warm shower (relieved by cooler temps)
potential signs of MS
-spasticity
-nystagmus (involuntary eye movement)/double vision
-optic neuritis → impaired vision and pain
-paraesthesia
-bladder/sexual dysfunction
give 3 atypical MS symptoms (i.e. if they have these it is unlikely to be MS)
-aphasia
-hemianopia
-muscle wasting
potential differentials for MS
-SLE
-sjogren's
-AIDS
what investigations might you do in suspected MS?
-MRI of brain and spinal cord → lesions may be seen around ventricles
-lumbar puncture → CSF
what medication might you give to someone to reduce the relapse severity of MS?
short course steroids e.g. methylprednisolone
describe the pharmacological treatment for MS
-beta interferon (anti-inflammatory)
-natalizumab (mono-clonal antibody)
-stem cell transplant
-muscle relaxants for spasticity and other symptom relief
what is a UMN?
upper motor neuron → neurone located entirely in the CNS (cell body in the primary motor cortex)
signs of UMN weakness
-spasticity
-increased muscle tone
-hyper-reflexia
-minimal muscle atrophy
causes of UMN weakness
-MS
-brain tumour
-stroke
what is LMN?
neurone that carries signals to effectors → cell body located in the brain stem/spinal cord
signs of LMN weakness
-flaccid
-reduced muscle tone
-hypo-reflexia
-muscle atrophy
-fasciculations (muscle twitches)
what is epilepsy?
tendency to have seizures
define seizure
convulsion caused by paroxysmal discharge of cerebral neurones → abnormal and excessive excitability of neurones
give causes of transient loss of consciousness
-syncope
-epileptic seizures
-non-epileptic seizures
-intoxication e.g. alcohol
-ketoacidosis/hypoglycaemia
-trauma
give causes of epilepsy
-flashing lights
-CVD e.g. stroke
-genetic predisposition
-CNS infection (e.g.
-trauma
signs of an epileptic seizure
-30-120s in duration
-'positive' symptoms e.g. tingling and movement
-tongue biting
-head turning
-muscle pain
define syncope
insufficient blood/oxygen supply to the brain causing paroxysmal changes in behaviour, sensation and cognitive processes
give signs that a transient loss of consciousness is due to syncope
-situational
-5-30s duration
-sweating
-nausea
-pallor
-dehydration
what is likely to last for longer, an epileptic or non-epileptic seizure?
non-epileptic seizure can last from 1-20 minutes whereas an epileptic seizure lasts for 30-120s
what 2 categories can epileptic seizures be broadly divided into?
-focal epilepsy → only one portion of the brain is involved
-generalised → the whole brain is affected
give 3 examples of focal epileptic seizures
1. simple partial seizures with consciousness
2. complex partial seizures without consciousness
3. secondary generalised seizures
give 3 examples of generalised epileptic seizures
1. absence
2. myoclonic
3. generalised tonic clonic
describe a generalised tonic clonic seizure
sudden onset rigid tonic phase followed by a convulsion (clonic phase) in which the muscles jerk rhythmically
*episode lasts up to 120s and is associated with tongue biting and incontinence
describe a myoclonic seizure
isolated muscle jerking