NPB 10 Midterm 2 ! (copy)
0.0(0)
Card Sorting
1/100
Earn XP
Description and Tags
https://quizlet.com/373458588/npb-10-midterm-2-flash-cards/
Last updated 10:38 PM on 2/14/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
101 Terms
1
New cards
contraction
thick filaments (myosins) and thin filaments (actin) SLIDE
2
New cards
calcium
helps in regulation of proteins on thin filaments - > causes them to move out of the way
the sarcomere shortens " sliding" of thick and thin filaments and results in contraction
the sarcomere shortens " sliding" of thick and thin filaments and results in contraction
3
New cards
mechanics of muscle contraction
in smooth and cardiac form, there are contractile proteins
\-myosin
\-actin
in skeletal muscle, the myosin is arranged thick filaments and actin is arranged in thin filaments
\-myosin
\-actin
in skeletal muscle, the myosin is arranged thick filaments and actin is arranged in thin filaments
4
New cards
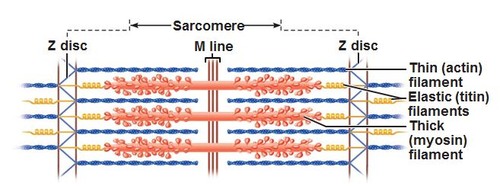
sarcomere
primary unit of contraction
\-thousands inside of muscle cells
\-thousands inside of muscle cells
5
New cards
how does sarcomere shorten in length -> contracts and slides?
\-requires ATP which drives the head bending "power stroke"
\-ATP also allows the head to let go of actin (thin filament)
\-in relaxed muscles, regulatins protein tropomyosin sits on the actin thin filaments and BLOCKS
\-ATP also allows the head to let go of actin (thin filament)
\-in relaxed muscles, regulatins protein tropomyosin sits on the actin thin filaments and BLOCKS
6
New cards
what happens when we activate a muscle?
1. calcium enters muscle cell
2. causes the tropomyosin to move out of the way
3. thick filament and the thin filaments will form crossbridge (heads bind)
4. contraction
7
New cards
exciting muscle cells results in....
a rise in calcium levels= muscle contraction
8
New cards
e
xciting muscles requires...
xciting muscles requires...
input from a neuron (efferent pathway)
1. AP travels down the alpha- motor neuron
2. AP causes neurotransmitter (acetylcholine) to be released in synapse
3. ACH binds its receptor on muscle and activates the receptor and sodium ions enter the cell
4. causes an AP in muscle
1. AP travels down the alpha- motor neuron
2. AP causes neurotransmitter (acetylcholine) to be released in synapse
3. ACH binds its receptor on muscle and activates the receptor and sodium ions enter the cell
4. causes an AP in muscle
9
New cards
what happens when AP spreads through a muscle?
Calcium enter the cytoplasm of the muscle from the outside and an organelle sarcoplasmic reticulum
10
New cards
how do you stop contraction?
1. remove calcium from the cytoplasm
2. stop having AP in the muscle cell
3. stop signaling between the neuron and the muscle
11
New cards
muscle twitch
most basic simple contraction and it can't do much as it is a fast rise to tension and fast relaxation
contracts when tension accumulates and peaks and then relaxes in a matter of milliseconds
summation of twitches allows us to generate strong force and long lasting contraction
contracts when tension accumulates and peaks and then relaxes in a matter of milliseconds
summation of twitches allows us to generate strong force and long lasting contraction
12
New cards
why study twitches?
\-a slow twitch generally has more endurance and has metabollic pathways that generate alot of aTP- > consumes oxygen in a type 1 muscle
\-a fast twitch generally generates force very quickly.
\--fatigue resistant - > type 2A muscles
\--fatiuable_ > type2B
\-a fast twitch generally generates force very quickly.
\--fatigue resistant - > type 2A muscles
\--fatiuable_ > type2B
13
New cards
motor unit
1 motor neuron and all the muscle cells it controls
14
New cards
small motor unit
neuron innervate control 10-50 muscle cells
(important for moving light loads and control)
(important for moving light loads and control)
15
New cards
large motor unit
neuron innervate HUNDREDS of muscle cells
16
New cards
recruitment of motor units
progressively activates more and more motor units which generates more force
17
New cards
primary motor cortex
first to elicit commands to do specific motor activities
18
New cards
associative motor cortex
The association cortices include most of the cerebral surface of the human brain and are largely responsible for the complex processing that goes on between the arrival of input in the primary sensory cortices and the generation of behavior.
19
New cards
cerebellum
A large structure of the hindbrain that controls fine motor skills.
20
New cards
basal nuclei
fine control of voluntary activity
21
New cards
spinal cord
mediates myotatic reflexes like a knee jerk and pain withdrawl reflexes
22
New cards
sarcopenia
age related decline in muscle function, causes are multi factoral
\-inactivity
\-genetics
exercise early in life = protective effecti
1. builds muscle
2. metabolism
sarcopenia-> leads to weakness -> leads to falls
\-inactivity
\-genetics
exercise early in life = protective effecti
1. builds muscle
2. metabolism
sarcopenia-> leads to weakness -> leads to falls
23
New cards
cardiovascular system
transports stuff throughout body
\-gases oxygen and carbon dioxide
\-fuel glucose, fats/ (free fatty acids)
\-hormones
\-wastes
\-thermal energy- heat
\-gases oxygen and carbon dioxide
\-fuel glucose, fats/ (free fatty acids)
\-hormones
\-wastes
\-thermal energy- heat
24
New cards
heart
pressure maker \n pressure gradients: differences in pressure drives flow
25
New cards
pathways
vasculature
26
New cards
blood transport medium
can move gases, fuel, signal bacteria, cells, hormones
27
New cards
systemic circulation
\-blood comes from the left heart
\-receives blood from the lungs (to the left atrium)
\-delivers oxygenated blood, low CO2
\-receives blood from the lungs (to the left atrium)
\-delivers oxygenated blood, low CO2
28
New cards
pulmonary circulation
\-blood leaves the right ventricles to the lungs ( pulmonary blood vessels)
\-oxygen poor, CO2 rich
\-right atrium receives blood from the body organs
\-oxygen poor, CO2 rich
\-right atrium receives blood from the body organs
29
New cards
1. pressure gradients= blood flow if....
2. pressure gradients= no blood flow
1. Pa > Pb
2. Pa= Pb
30
New cards
gradient of pressure
blood flow= Change in pressure/ resistance to flow
31
New cards
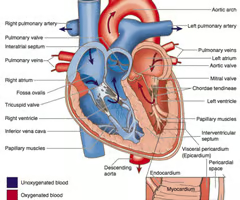
heart
know:
* superior vena cava
* atrium and ventricles ( R and L)
\-inferior vena cava
atrio-ventricular valves
\-semilunar valves
\-pulmonary veins
* apex
* superior vena cava
* atrium and ventricles ( R and L)
\-inferior vena cava
atrio-ventricular valves
\-semilunar valves
\-pulmonary veins
* apex
32
New cards
right ventricle
drives blood to lung ( pulmonary circulation)
33
New cards
left ventricle
drives blood to body (systemic circulation)
\-must shove, push blood into aorta
\-must shove, push blood into aorta
34
New cards
valves
prevents BACKWARDS blood flow
35
New cards
AV valves
prevent backwards flow from ventricles to atria
* close when ventricles contract
* close when ventricles contract
36
New cards
semilunar valves
prevent backward flow from arteries back into ventricles
\-close when ventricles relax
\-close when ventricles relax
37
New cards
aorta
The large arterial trunk that carries blood from the heart to be distributed by branch arteries through the body.
fill with blood -> stretches - > recoils -> drive blood flow when ventricles relax - > ventricles contract - > fill with blood
\*elastic artery:
fill with blood -> stretches - > recoils -> drive blood flow when ventricles relax - > ventricles contract - > fill with blood
\*elastic artery:
38
New cards
pulmonary trunk/ pulmonary arteries
fills with blood when ventricle contracts - > recoils and drives blood into pulmonary circulation
\*elastic artery
\*elastic artery
39
New cards
elastic artery
"store" energy as they fill with blood, then they recoil and drive blood out
40
New cards
arterioles
small vessels that receive blood from the arteries
\*resistance vessels: can oppose blood flow
\*resistance vessels: can oppose blood flow
41
New cards
vasodilation
reduces resistance to flow and is caused by metabolytes
42
New cards
capillaries
\-exchange blood vessels
-allow molecules to cross
\-small diameter
\-thin walls ( 8- 10 microns in diameters)
\-close to tissues
\-very slow blood flow
-allow molecules to cross
\-small diameter
\-thin walls ( 8- 10 microns in diameters)
\-close to tissues
\-very slow blood flow
43
New cards
endothelial cell
makes up walls of capillary
44
New cards
fenestra/ gaps/ pores
allow exchange between endothelial cells
45
New cards
discontinuous capillaries
have gaps between cells; found in bone marrow, liver, and spleen; allow the passage of proteins
46
New cards
fenestrated capillaries
have pores in vessel wall; found in kidneys, intestines, and endocrine glands
47
New cards
continuous capillaries
have a wall where the endothelial cells fit very tightly together.
\-found in brain
\-dont allow everything to leave the blood and then enter the tissue
\-found in brain
\-dont allow everything to leave the blood and then enter the tissue
48
New cards
venules and veins
\-drain capillaries
\-blood pressure is low
\-drain lower extremities
\-blood pressure is low
\-drain lower extremities
49
New cards
muscle pump
blood flow is driven up while muscles contract
50
New cards
venous valves
backwards flow is prevented when muscles relax
51
New cards
systolic BP
arterial pressure when ventricles contract
52
New cards
diastolic BP
arterial pressure when the ventricles relax
53
New cards
mean arterial pressure
MAP= (1/3 x SP)+ (2/3 x DP)
\-drives our blood flow and homeostatically regulates it
\-as MAP increases, it creates after-load on the ventricle so the ventricle must work harder
\-drives our blood flow and homeostatically regulates it
\-as MAP increases, it creates after-load on the ventricle so the ventricle must work harder
54
New cards
hypertension
high blood pressure
\-imposes a workload on the heart
\-imposes a workload on the heart
55
New cards
red blood cell
\-no nucleus
\-lots of hemoglobin
\-iron binds to oxygen
\-100 ml of blood and there is approximately 40% volume of RBC
\-binds to oxygen in pulmonary circulation
\-lots of hemoglobin
\-iron binds to oxygen
\-100 ml of blood and there is approximately 40% volume of RBC
\-binds to oxygen in pulmonary circulation
56
New cards
in tissues (muscle and brain) hemoglobin________ its affinity to oxygen
loses
57
New cards
in the lungs hemoglobin _______ gains affinity to oxygen
gains
58
New cards
highly metabolic tissues releases metabolytes and its hotter which....
changes the affinity of hemoglobin so that hemoglobin releases the oxygen
59
New cards
why is blood in the fetus very sticky???
it allows for fetal blood to become oxygenated
60
New cards
sickle cell hb
was evolved for places where malaria was prevalent
\-imports some type of resistance to malaria
\-changes the shape of the rbc
(shape is usually circular and it gets changed into a crescent shape, which is not as effective in carrying oxygen and results in sickle cell anemia)
\-imports some type of resistance to malaria
\-changes the shape of the rbc
(shape is usually circular and it gets changed into a crescent shape, which is not as effective in carrying oxygen and results in sickle cell anemia)
61
New cards
what organs receive constant blood flow?
brain, heart (coronary circulation), kidneys
62
New cards
what receives varied blood flow?
muscle- when activity increases, blood flow increases
63
New cards
what receives little blood flow?
fat and tissue
64
New cards
What is vasoconstriction of the arteriole caused by?
SNS input
65
New cards
where does sns input come from?
CNS (spinal cord)
\-SNS activity increases when we are scared or trying to escape something
\-SNS activity increases when we are scared or trying to escape something
66
New cards
how to increase blood flow to tissues
a. decreases SNS activity to smooth muscles, this relaxes smooth muscles
b. metabolytes that are released by tissue will cause smooth muscle to relax
b. metabolytes that are released by tissue will cause smooth muscle to relax
67
New cards
respiratory system
moves air into and out of lungs
\-gas exchange between the blood and the alveoli
\-gas exchange between the blood and the alveoli
68
New cards
internal respiration
cellular respiration
\-mitochondria: uses oxygen to generate ATP
(as we increase rate of ATP synthesis, cellular respiration increases which causes external respiration)
\-mitochondria: uses oxygen to generate ATP
(as we increase rate of ATP synthesis, cellular respiration increases which causes external respiration)
69
New cards
conductive pathways
air movement
\-mouth,nose
\-trachea
\-branches
\-bronchi
\-mouth,nose
\-trachea
\-branches
\-bronchi
70
New cards
bronchiole
Airways in the lungs that lead from the bronchi to the alveoli. no cartilage
\-warms air as we inspire and wets the air followed by removing dust, pollen, and particulates - > mucus
\-warms air as we inspire and wets the air followed by removing dust, pollen, and particulates - > mucus
71
New cards
exchange surfaces
allows gases oxygen and carbon dioxide to move between lungs and blood
72
New cards
Alveoli
tiny sacs of lung tissue specialized for the movement of gases between air and blood.
\-type 2 alveolar cells produce surfactant
\-type 2 alveolar cells produce surfactant
73
New cards
respiratory muscles
\-diaphragm
\-intercostal muscles (internal and external)
\-abdominal muscles
\-scalene and sternocleidomastoids
\-intercostal muscles (internal and external)
\-abdominal muscles
\-scalene and sternocleidomastoids
74
New cards
what happens during breathing?
inspiration involves increasing the lung volume so air can move in. expiration involves decreasing lung volume so air can move out.
\
**think of a syringe**
\
**think of a syringe**
75
New cards
what happens during inspiration?
contraction of respiratory muscles (diaphragm and external intercostal muscles)
76
New cards
what happens during expiration?
the muscles relax
77
New cards
what happens during forced expiration?
forced expiration
\-abdominal muscles and internal intercostal muscles (rib muscles) strongly decrease the thoracic volume and lung volume -> increases pressure in lungs
\-abdominal muscles and internal intercostal muscles (rib muscles) strongly decrease the thoracic volume and lung volume -> increases pressure in lungs
78
New cards
what happens during forced inspiration?
scalene and stemocleidomastoid muscle (neck) strongly increase thoracic volume
79
New cards
What happens to inspired gas?
\-move through the conductive pathways ( nose and mouth -> trachea -> bronchi - > bronchioles)
* air velocity is initially really fast _> air slows down
\-air is moistened and warmed
* dust, pollen, floating dirt are removed and stick to mucus
* air velocity is initially really fast _> air slows down
\-air is moistened and warmed
* dust, pollen, floating dirt are removed and stick to mucus
80
New cards
what happens when air hits the respiratory/ exchange surfaces of the lung?
it allows for gases to move between the blood and the lung (alveolus)
81
New cards
what do alveoli do?
type 1: cells are thin because it allows for gas exchange
type 2: secrete pulmonary surfactant which make it easier to breathe
\
premature babies are born with non functional or low functional type 2 cells -> respiratory distress
type 2: secrete pulmonary surfactant which make it easier to breathe
\
premature babies are born with non functional or low functional type 2 cells -> respiratory distress
82
New cards
how are alveoli organized?
in sacs and ducts
83
New cards
what makes up the air?
79%- nitrogen
20%- oxygen
0\.03%- CO2
Patm- 760 mmHg
Po2- 160 mmHg
20%- oxygen
0\.03%- CO2
Patm- 760 mmHg
Po2- 160 mmHg
84
New cards
when air enters the lungs?
Po2= 100 mmhg
Pco2= 40 mmHg
\
**think of these as concentrations**
Pco2= 40 mmHg
\
**think of these as concentrations**
85
New cards
pulmonary capillaries
carries blood that came from the right heart, came from body organs
86
New cards
Which direction does oxygen flow?
alveolus Po2 =100 -> capillary Po2= 40
87
New cards
which direction does CO2 flow?
alveolus Pco2
88
New cards
how do we carry oxygen in the blood?
!. dissolved
2\. bound to hemoglobin (Hb)
3\. found in RBC
2\. bound to hemoglobin (Hb)
3\. found in RBC
89
New cards
how do we carry CO2?
1. dissolved CO2
2. bound to blood proteins (hemoglobin- carb amino protein compounds)
3. convert CO2 into bicarbonate (HCO 3-) in RBC
90
New cards
blood components
1. majority is O2 bound to Hb in RBC
\-each Hb can bind 4 oxygen molecules
\-in 100 ml of blood can carry about 20-22 ml of oxygen -> sufficient for any metabolism
2. majority of CO2 is carried in the form of HCO3-
91
New cards
why does affinity of Hb change to oxygen?
in response to local metabolytes/ local conditions
\-decreases affinity Hb and gives up O2
\-"Bohr effect"
\-decreases affinity Hb and gives up O2
\-"Bohr effect"
92
New cards
Where does Hb affinity to CO2 increase?
at tissues
93
New cards
Where does Hb simultaneously bind to O2 and let go of CO2?
the lungs
94
New cards
carbon monoxide
\-poison
\-produced by burning
\-sticks to Hb STRONG
\-odorless
\-no color
\-produced by burning
\-sticks to Hb STRONG
\-odorless
\-no color
95
New cards
brainstem
major controller of cardiovascular and respiratory function
\-detect our MAP in the aorta and carotid arteries
\-detect our blood gases CO2, indirectly H+
\-low O2 and high CO2
\*receives sensory info from blood pressure sensitive baroreceptive neuron
\*if MAP is low, will activate the SNS
\*decrease activity of PNS
\-detect our MAP in the aorta and carotid arteries
\-detect our blood gases CO2, indirectly H+
\-low O2 and high CO2
\*receives sensory info from blood pressure sensitive baroreceptive neuron
\*if MAP is low, will activate the SNS
\*decrease activity of PNS
96
New cards
what increases SNS and PNS?
heart rate
97
New cards
peripheral chemoreceptors
Receptors in the carotid arteries and the aorta that monitor blood pH to help regulate ventilation rate.
\
\
98
New cards
diaphragm and external intercostal muscles
1. respiratory muscles of the chest/ thorax
2. muscles of nares and pharynx
99
New cards
Sternocleidomastoid and scalenes
neck and throat
100
New cards
what does the renal system do?
conditions the blood