2 - Auxillary retention systems in vital and non-vital teeth
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
29 Terms
What is an auxiliary retention system?
Elements that are used to improve the retention of a restoration
What are the auxiliary retention systems?
Pins, posts, post and core
What are the indications for auxillary retention systems?
Retain a core in teeth with extensive loss of coronal structure.
When we dont have enough retention with cavity preparation.

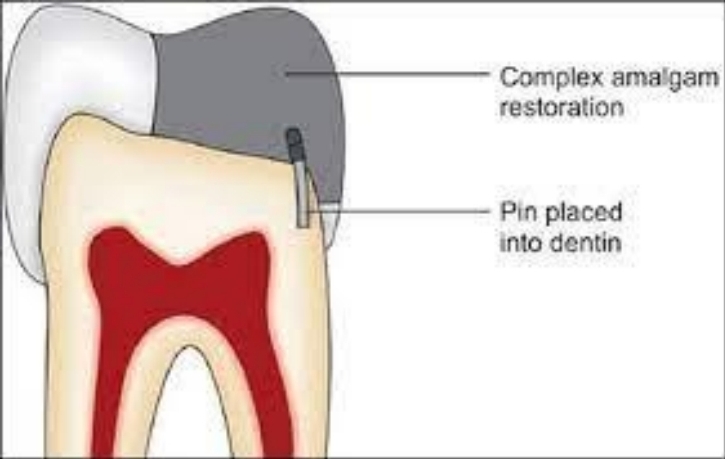
When are pins used?
Vital teeth
ALWAYS in dentin NEVER enamel or pulp. (cemented or driven in)
When are posts or post and core used?
In non-vital teeth after root canal treatment

When are pin Contraindicated?
Significant malocclusions
If direct restoration isnt possible (anatomic/functional reasons)

What are the rules for placing pins?
PA xray to evaluate:
Pulp chamber size + position
Dentin thickness
Relative crown/root inclination
Tooth axis respective of neighbouring teeth.
Location or distribution of pins:
Midway between pulp and tooth surface
Safe distance from pulp and periodontum (2mm)
Cervical third of posterior teeth
Close as possible to line angles
0.5mm away from axial or vertical wall cavity
Always on flat surfaces
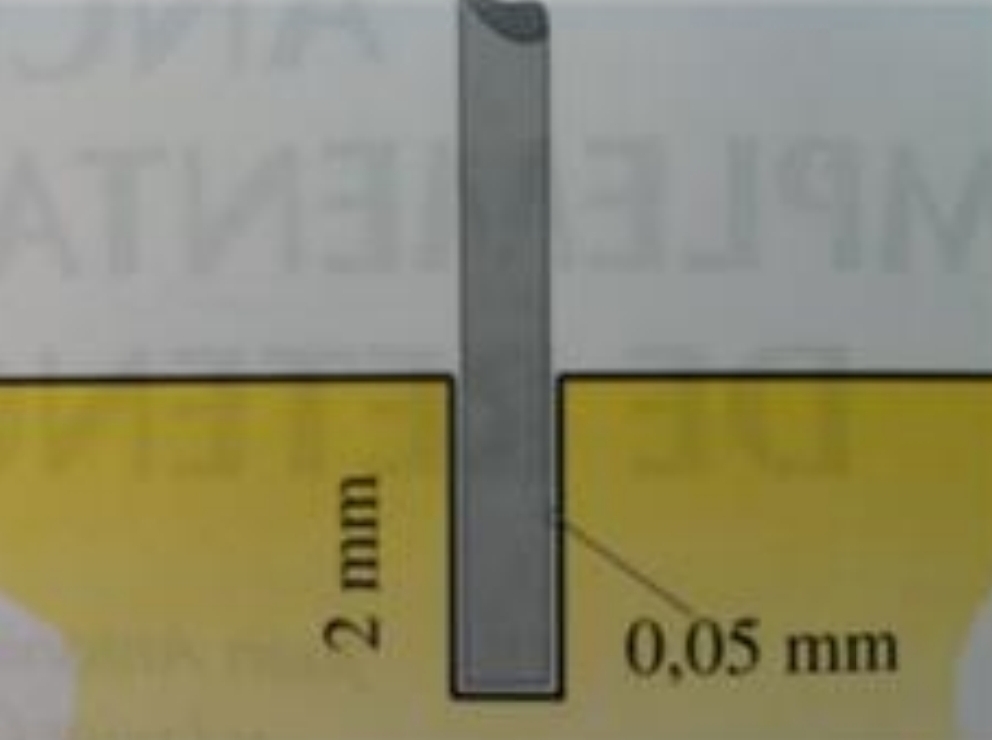
2-2-2 rule
Length of pin inside and outside dentin should be the same (2mm)
2mm inside - 2mm outside - 2mm covered in restoration material
IF length outside larger, lever forces can fracture/disinsert pin
What must you avoid when placing pins?
Interferance with cavitary walls and matrices
Pulp
Isthmus area
Furcation area
Small amounts of dentin
Mesiofacial corners of molars
What are the 4 types of pin systems?
Cemented pins
Friction-locked pins
Self threading pins
Cyanoacrylate pins
How are cemented pins used?
Drill 0.05mm wider than pin leaving room for cement
How do friction lock pins work and why are they in disuse?
Slot in dentin cut slightly lower than that of pin, which is inserted with force to reach bottom of prepared slot.
Drawbacks: dentine cracks, little retention
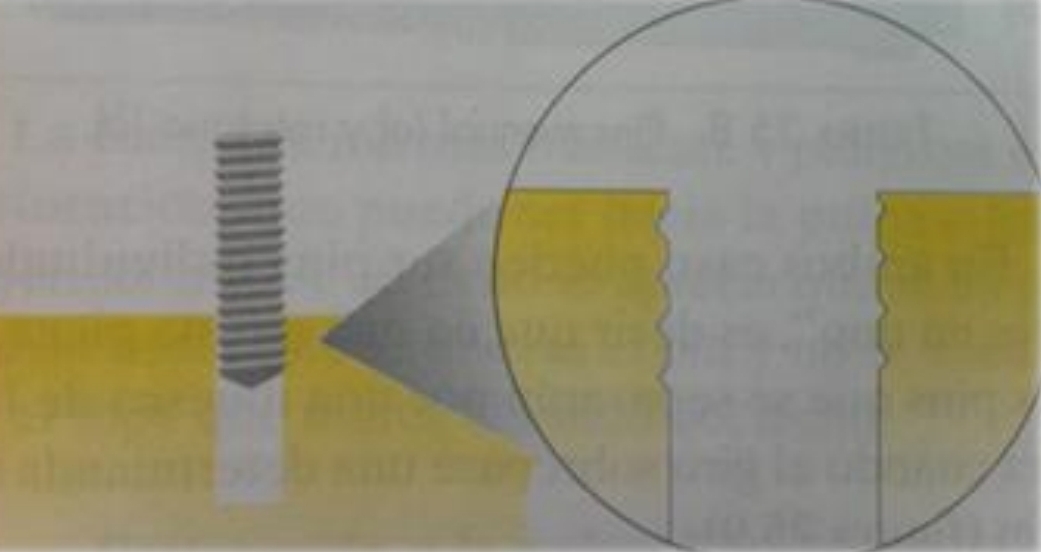
How do self-threading pins work?
Slot in dentin with 0.1 mm diameter, lower than pin. Pin works it’s own thread into slot wall.
How do cyanoacrylate pins work?
4mm pin, drill can only penetrate 2mm. (For 2-2-2 rule)

What are the disadvantages of pins?
Decreases strength of restorative materials, induce stresses in dentin which may cause:
Cracks in teeth
Microleakage
Pulpal damage
External or pulpal perforation
Perforation of periodontum (can cause tooth loss)
Chance of microleakage around pins
Looseness in duct (Laterally placed or defective drill) - issue with threaded pins, not cemented
Fracture of drill in slot - impossible to extract, leave it in place, put pin in another slot
Where are the body and head of a post positioned in the tooth?
Body - inside canal
Head - in crown

What procedural accidents are a risk when preparing and placing posts?
Strip perforation
Root fracture
According to what 5 things are posts classified?
Modulus of elasticity
Technique of clinical use
Manufacturing method
Shape
Composition
What is the desired modulus of elasticity (and hence material) for posts?
Elasticity similar to dentin (18GPa)
Fibreglass (20-40GPa) and carbon fiber
Ceramic and metal posts too ridgid - can cause fractures
What happens when two materials with different modulus of elasticity are joined?
Force is concentrated on more fragile material
What are the 3 different post techniques of clinical use (and manufacturing technique)?
Direct - Prefabricated
Indirect - Anatomical, canal impression needed, manufactured in lab, made in ceramic, noble metal or glass fibre
Semidirect - Anatomical, canal impression needed, made in clinic, with Prefabricated fibre and composite post
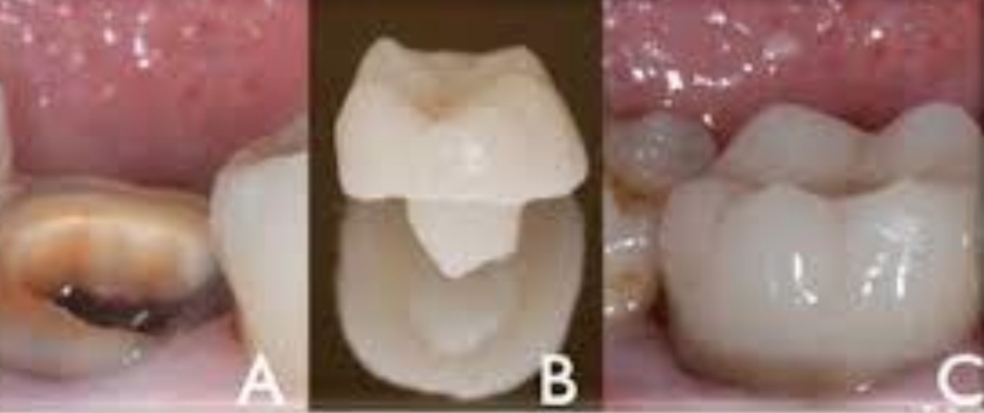
What is an endocrown?
For rtc teeth with significant structure loss, where normal crown not possible. Anchored within remaining tooth.
What are the different post shapes?
Conical (tapered) - Less retentive, more anatomical, dont thin root walls much, less clinical complcations
Cylindrical (parallel) - Good retention, need apical preparation, fracture and perforation risk
Double taper (parallel tapered) - good adaptation, better retention than conical. Most commonly used. Usually quartz fiber.
3 parts:
Coronal - cylindrical, retains filling material
Middle - conical (tapered)
Apical - another minor taper
Accesories - Conical, bundle of posts of 0.3mm, filling in wide canals to reduce amount of cement. When sleeve removed they spread and cover entire canal. Adapt to any canals morphology.
What is the composition of glass fiber posts?
Longitudinal glass fibers (42%)
Epoxy resin (29%)
Inorganic particles (29%)
Some are phototransmitters (cant be seen in xray), and some are opaque.
Can be direct or indirect. Manufactured in lab
What are the morphological and root requirements to place a post?
No cavites, fractures or resorption
Adequate length and thickness and morphology
Straight root without curvatures, with round and wide canal
Select thickest, longest and straighest root in multiradicular teeth
Where shoud you place the post in Upper/lower molars and premolars?
Maxillary molars - Palatine root
Upper premolar - Palatine root
Mandibular molars - Distal root
What are the clinical evaluation requirements for post placement?
Radiography showing correct RTC, good apical sealing, and no radiological lesions or symptoms. If necesarry, do reendo to avoid future failures.
2mm supragingival ferrule (for retention)
Periodontal status - periodontal disease must always be treated before restoration. (bone crest must be above post level)
How should you determine post length?
Should enter up to 2 thirds of the root, and be at least 4mm from the apex, and 2mm from dentin at root.
Length greater than or equal to clinical crown
In cases of periodontal teeth - length equal to half the length of root surrounded by bone
What is the clinical protocol of the placement of a direct prefabricated glass fiber post?
X ray, clinical eval, isolation- only use rubber dam when inserting post not when removing gap to avoid perforations
Post space preparation- create a correct entry, then use Gates-Glidden drills #2, #3 to remove GP, drill corresponding to the chosen post size, insert post, adjust and cut to desired length
Surface treatment of post and canal with acid etch and alcohol
Dual adhesive system inside canal
Apply fluid composite and place post, polymerise
Manufacture cure with same composite or hybrid
What are the challenges when a direct fibreglass post bonds to root dentin?
Limited vision and access
Residual GP
Hard to apply and cure adhesives in root canal
Hard to rinse etchings
Solvent may not completely evaporate
Potential oxidizing effect of NaOCl
Increased volume of luting cement to fill in space between post and root dentin wall
High C-factor (ratio of bonded to unbonded surfaces) May result in greataer polymerization stress
Variations in tubule density