tx 2 : lec 5 blood and blood products
1/95
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
96 Terms
when are circumstances that whole blood is used (as it is extremely limited in use)
for massive transfusion to correct for hypovolemia (low blood volume)
trauma
shock
exchange transfusion
autologous donation
what is the #1 characteristic whole blood needs to have if it is getting used in a transfusion?
MUST be ABO identical
vast majority of the red cell units you see in the transfusion medecine lab in canada fall into what catregory
packed RBC leuco reduced
indication for use of rbcs
Symptomatic anemia caused by
decreased bone marrow production (lekemia or aplastic anemia)
decreased rbc survivqal (hemolytic anemia)
surgical/traumatic anemia
typically, prbcs should increase hb how much in adults and children?***
adults: 10-15 g/L
children: 20-30 g/L
typically prbcs should increase hct how much in adults and children?***
adults: 3-5%
children: 6-9%
is there a Hb value that triggers the need for transfusion?
no
every institution has their own policy
tx are based on more factors than Hb
A patient has a baseline hemoglobin
count of 60g/L. After receiving 4 units
of packed red blood cells, what would
you expect the post-transfusion
hemoglobin count to be?
****each unit of prbc typically increases Hb by 10 g/L
therefore 4 × 10 = 40
40 + 60 = 100
we would expect the post transfusion hb count to be 100 g/L
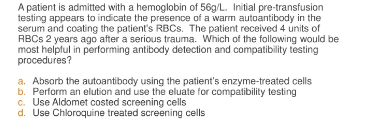
when would we used deglycerolized rbcs (lr)
rare blood types
IgA antibodies
ppl w multiple abs
ppl w abs that are high incidence abs
when are washed red cells used
for people experiencing allergic reactions (usually to plasma components)
neonates undergoing replacement tx / massive tx
when to use irradiated rbc
immunocomps
pts needing bone marrow/ stem cell transplant
intrauterine tx
when would you tx plts
pts actively bleeding and are experiencing thrombocytopenia/ thrombocytopathy
generally plt tx is given when plt count is below what value
20 × 109/L
if a pt has <20 × 10 ^9/L plts (thrombocytopenia), you would give them a tx unless they have?
ITP idiopathic thrombocytopenic purpura)
TTP (thrombotic thrombocytopenic purpura)
DIC (inc consumption)
HUS (hemolytic uremic syndrome)
THESE CONDITIONS ARE A RESULT FROM INCREASED DESTRUCTION SO THERES NO POINT TO TX BC ITS GNA GET DESTROYED ANYWAYS
***generally, ABO specific compatibility is recommended for plt tx. when can this rule be “broken”
INCOMPATIBLE GROUPS MAY BE GIVEN USUALLY IN SHORT TERM BUT MUST DO SPECIAL TEST
isohemagglutinins
monitor pt for complications
what is/why is an isohemagglutinin test done and when is it done?
it is a titration test done to detect high titer of anti-A or anti-B abs in donor/ pt samples.
usually done when group O plts/ plasma is given to non group O individuals.
done to reduce the risk of acute hemolytic transfusion reaction
one unit of buffy coat poor platelet is expected to raise the adult count by *****
20.0 × 10^9/L
one unit of random donor platelet raises adult count by ******?
5 × 10^9/L
what is it called when you dont get the expected incremental increase of platelets (20.0 × 10^9/L for buffy coat poor plts or 5 × 10^9/L in randim donor)
platelet refractoriness
platelet refractoriness can be treated by giving?
Apheresis HLA matched plts
the rate of increase for apheresis plts are?****
8-10 × 10^9/L
PLTS should be ____ compatible with the recipient
ABO/Rh (bc there may still be a little amt of rbc in it)
A patient has a baseline platelet count
of 30.0 x 10⁹/L. After receiving two
unit of BCP platelets, what would you
expect the post-transfusion platelet
count to be?
2 × 20= 40
40+30 = 70.0 × 10^9/L
when would you transfuse granulocytes
pts w very low neutrophil counts
bacterial infection (unresponsive to antibiotics)
t/f granulocytes need to be crossmatched for tx****
T
granulocytes for transfusion are stored at what temp and expire when?
RT (20-24 DEGC), expire in 24 hours but best if given ASAP
who are CMV negative cellular blood products for?
CMV negative individuals that are at risk for CMV infections
CMV negative women
those getting bone transplant
prenatal infants/ premature infants
which plasma derivative: is defined as plasma collected by plasmapheresis and
intended for further manufacture into plasma derivatives
source plasma
which plasma derivative: is plasma recovered from whole blood donations that is
shipped frozen to a manufacturer
recovered plasma
which plasma derivative is separated from the plasma and used for the production of
Factor VIII concentrate.
cryoprecipitate
cryoprecipitate is separated from the plasma and used for the production of _______
Factor VIII concentrate.
when would u use FFP/ FP24
used to treat replacement of multiple clotting factors in pts w/
liver disease
DICe
vit K deficiency
warfarin overdose
massive tx
would you use ffp / fp24 for volume expansion or protein replacement? why or why not
no, safer products are available
when is cryoprecipitate reduced plasma used for in tx
for tx/ plasma exchange in TTP patients
t/f you are not able to used thawed and liquid plasma for factor V and/ or factor VIII deficiency
t
what population can get transfused with thawed and / or liquid plasma
those experiencing warfarin overdose
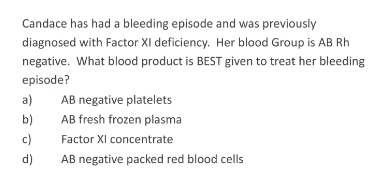
those w factor XI deficiency
plasma exchange for TTP, HUP, HELLP (abbreviation of the 3 main features of a syndrome found in pregnant individuals: hemolysis, elevated liver enzymes, low platelet count)
if doing plasma tx, does it need to be ABO/Rh compatible
should be ABO compatible with the recipient but the Rh type doesnt need to be compatible
(competency) each bag of cryo should contain at least ____ of fibrinogen and __ of factor VIII/unit.
150 mg/dL of fibrinogen and 80 units of factor VIII
(competency) each bag of cryo should contain at least 150 mg/dL of _____ and 80 units of ____ /unit
fibrinogen; factor VIII
cryo was used as?
a fibrin sealant/ glue now replaced w safer products; forms a quick plug to minimize the bleeding
instead of with cryo, mild/ moderate factor VIII deficiency is now treated with _____
desmopressin acetate
t/f for cryoprecipitate it is best to be ABO compatible but not important due to the
small volume
t
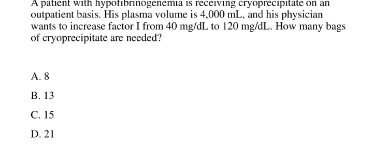
whats the formula for the adult dosage for Cryo
number of units = (required increase in Fibrinogen (mg/dL)/ 100) x Plasma volume (mL)/150
Consider an example of an adult patient with a fibrinogen of
60 mg/dL and a fibrinogen goal of 100 mg/dL. Assuming that
the patient has a plasma volume of 3000 mL, the correct
number of units of cryoprecipitate to transfuse is:
x= (100mg/dL- 60 / 100) x (3000/150)
= 0.4× 20
= 8 units of cryo
patients with Hemophilia A or Factor VIII deficiency are treated with ____
Factor VIII
Patients with _______ or Factor VIII deficiency are treated with factor VIII
Hemophilia A
A 70kg hemophiliac patient has Hct
of 30% an initial Factor VIII level of
4%(4 units/dL or 0.04 units/mL). How
many units of Factor VIII should be
given to raise the Factor VIII level to
50% or 0.50?
Formula:
(Desired factor- initial factor)x plasma volume(mL)=
Units of Factor VIII Required.
Step 1:
Calculate blood volume= weight (kg) x 70 mL/kg
70 kg x 70 mL/kg = 4900 mL
Step 2:
Calculate plasma volume = blood volume(mL) x (1.0 – Hct)
4900 mL x (1.0 - 0.30) = 3430 mL
Step 3: USE FORMULA
(0.50 - 0.04) x 3430 mL = 1578 units
what is factor IX used to treat
ppl w factor IX deficiency (hemophilia b)
pts w factor VII or X deficiency
selected pts w factor VIII inhibitors
reversal of warfarin overdose
formula to calculate dose needed of factor 9
(Desired factor- initial factor)x plasma volume(mL)=
Units of Factor IX Required.
FXIII is used to treat?
factor XIII deficiency ( severe autosomal recessive bleeding disorder)
_______ concentrates are licensed for use in
the United States for patients with hereditary
deficiency of antithrombin.
antithrombin
Largely replaced immune serum globulin as
the therapeutic agent for patients with
congenital immune deficiency
intravenous immune globulin (ivig)
Licensed indications for IVIG available in
Canada:
– Primary immunodeficiencies
– Secondary
hypogammaglobulinemia
- CLL with
hypogammaglobulinemia
in patients who have had
at least one episode of
major infection
- Hypogammaglobulinemia
in post bone marrow
transplant recipients
– Immune thrombocytopenic
purpura (ITP)
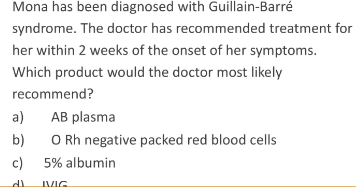
– Kawasaki syndrome
– Guillain-Barré syndrome
RhIg is used to treat
– Prevention of Rh HDN
– Treatment of ITP
Prepared from pooled human plasma from donors with high titers
of anti-D
RHIg(D) Immune Globulin
Passive anti-D globulin
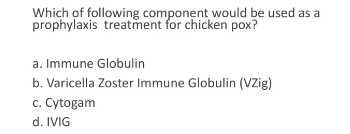
what is immune serum globulin (IM) used for
used as a prophylaxisis
used in exposure
to Hepatitis A, and measles
Dose ordered by MD
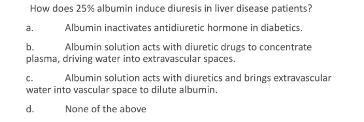
what tx product is used for patients requiring volume replacements
albumin
____ solution acts with
diuretics and brings
extravascular water into vascular
space to dilute albumin
25% albumin
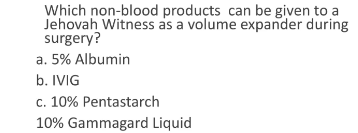
what tx product can be used with jehovahs witnesses
PENTASPAN (10% PENTASTARCH IN 0.9% NaCl)
in an emergency tx, what blood products do u use and dk the pts blood type
Use of Group O Rh negative and Rh positive RBCs
during the tx process, how long should the nurse stay witht he patient
for the first 15 mins
the tx should not take longer than ___ hours bc of the risk of bacterial proliferation at RT
4 hrs
what are the characteristics needed to return a blood bag that has been sent out back into the blood bank
bag ports not opened
they have ot been issued longer than 30 mins unless stored in a controlled blood storage environment
temo is less that 1 deg C
at least one sealed segment is still attached
_____ is given now instead of cryoprecipitate
fibrinogen
Jenna has been typed and screened. her results indicate that she is B Rh neg, and has an allo ab to a clinically sig high incidence ag. she decides to store her blood in case she requires a transfusion in the future.
a) what would he blood component be?
b) how would this component be stored?
c) what is added to this unit prior to storage?
a) what would he blood component be?
prbc
b) how would this component be stored?
-65 deg c (good for up to 10 yrs)
c) what is added to this unit prior to storage?
glycerol (so they don’t burst at that temp)
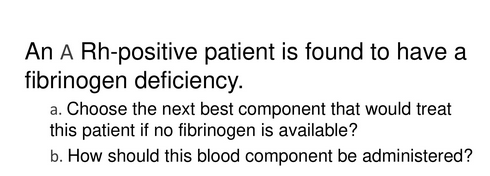
a) cryoprecipitate
b) calculate the dosage, thaw, and pool the cryo
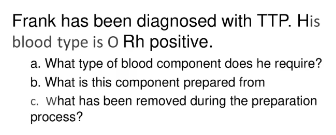
a) cryoreduced plasma (bc plasma)
b) ffp
c) cryoprecipitate
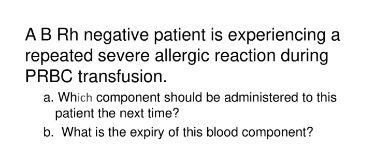
a) washed rbcs
b) 24 hrs if open system
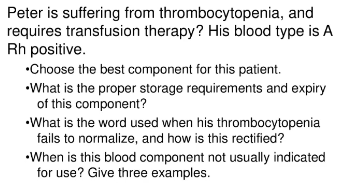
a) plts
b) RT, expires after 7 days agitation needed thruout
c) plt refractoriness; switch to apheresis plts
d) dic, hus, ttp (eats up plts)
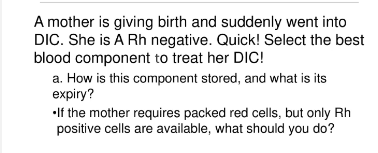
a) any antithrombolytic component, ffp, help for dic
b) o rh neg, ab plasma, a pos or o pos with Rhig
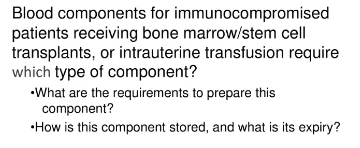
a) irradiated, cmv neg
b) rbc = -60 deg, irradiated therefore 14 days
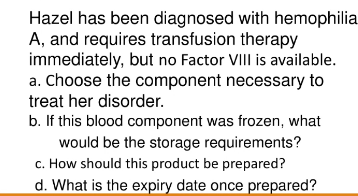
a) prothrombin complex, cryorecipitate, ffp
b) -60 deg c
c) defrost, completely thaw
d) transfuse w/ in 24 hrs if stored at 1-6 deg c
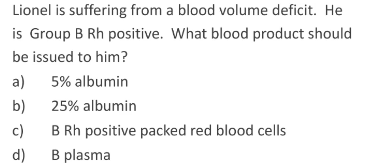
a (25 % is for hypotonic individuals)
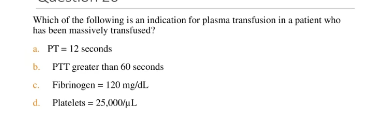
d
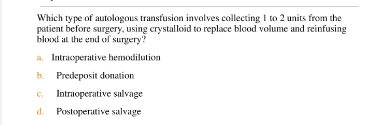
c
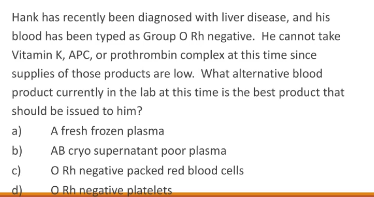
a (whenever the question mentions liver disease, think ffp bc thats where we make all our coag factors and stuff yar)
c
b
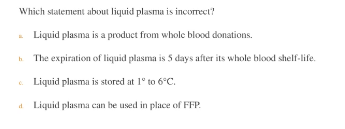
d (liquid plasma doesnt have labile factors)
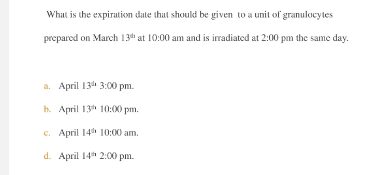
NONE OF THE ABV: granulocytes are only good for 24 hrs (should be march 14)
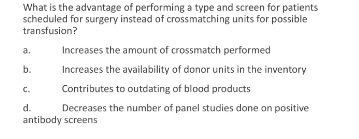
b
c
b
a
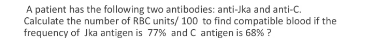
7 units
c
13
a