2ND QUIZ - PATHOLOGY - HSMR2304
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
Dysphagia
known as difficulty of swallowing.
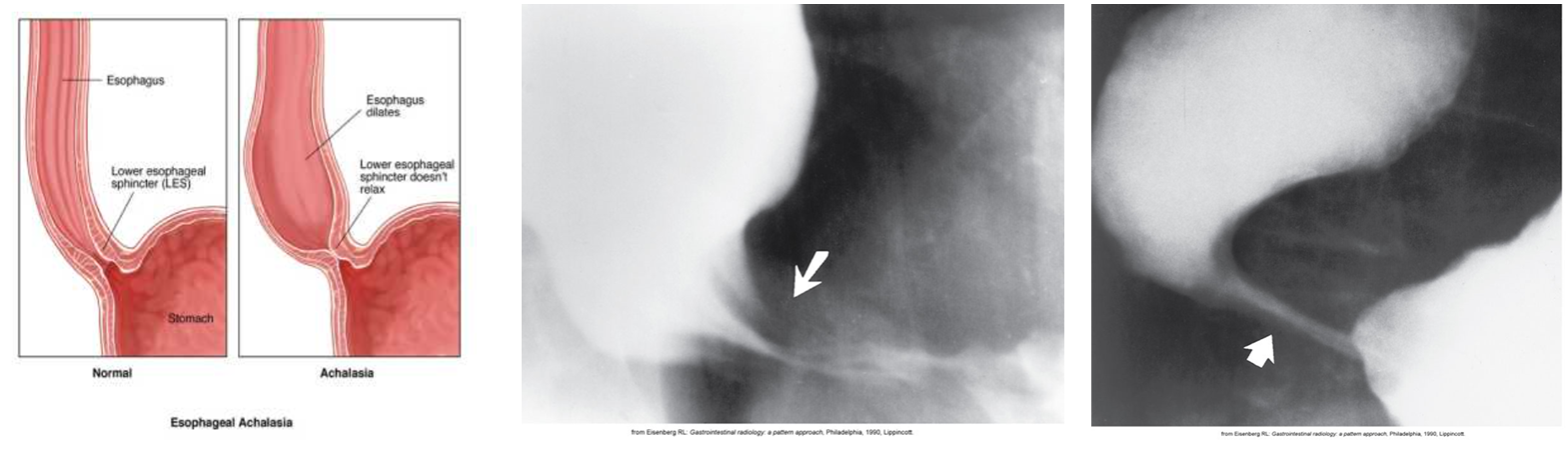
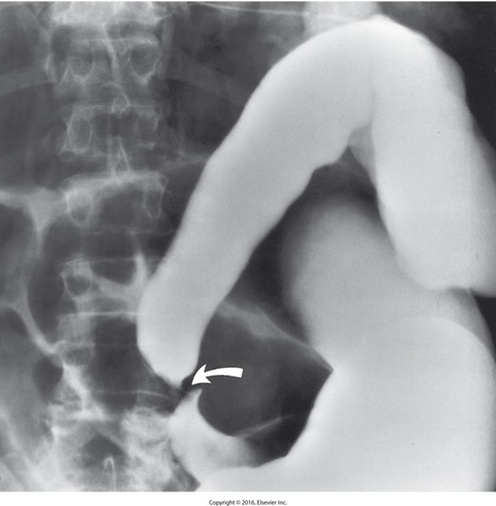
Achlasia
Functional obstruction of the distal esophagus with proximal dilation.
Caused by incomplete relaxation of the lower esophageal sphincter.
It is related to the absence of ganglion cells in the myenteric neural plexuses of the distal esophageal wall.
Radiological Appearance:
Rat Tail / Bird’s beak
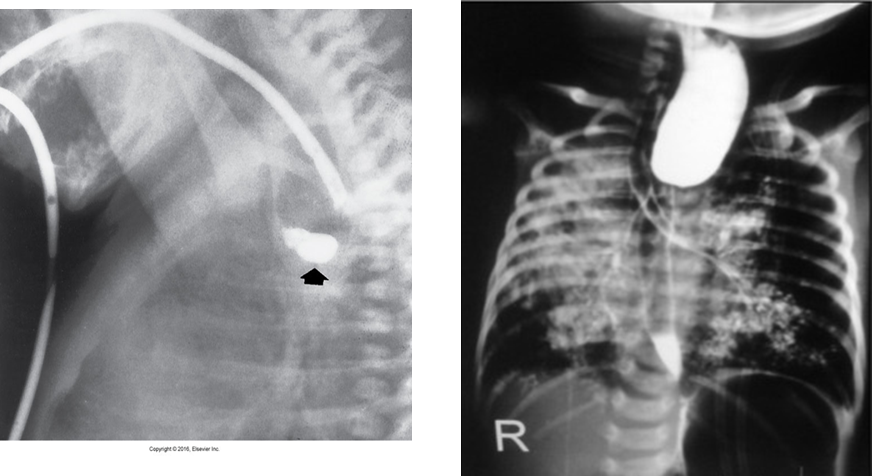
Esophageal Atresia
Is a congenital absence or closure of a normal body orifice or tubular organ.
The lack of the development of the esophageal lumen resulting in a blind pouch.
Caused by defect in cell differentiation of esophagus during 4-6 week of embryonic development.
_______ is coincident with ____.
Symptoms: appear soon after birth as excessive salivation, choking, gagging, dyspnea, cyanosis.
Radiological Appearance:
Esophageal Perforation
May be a complication of:
Neoplasm
External trauma
Esophagitis
Instrumentation
May result from severe vomiting (the most common cause) or coughing, often from dietary or alcoholic overconsumption.
Radiological Appearance:
Free air in mediastinum (Pneumomediastinum) if perforation extends throughout entire esophageal wall.
Contrast media may demonstrate extravasation

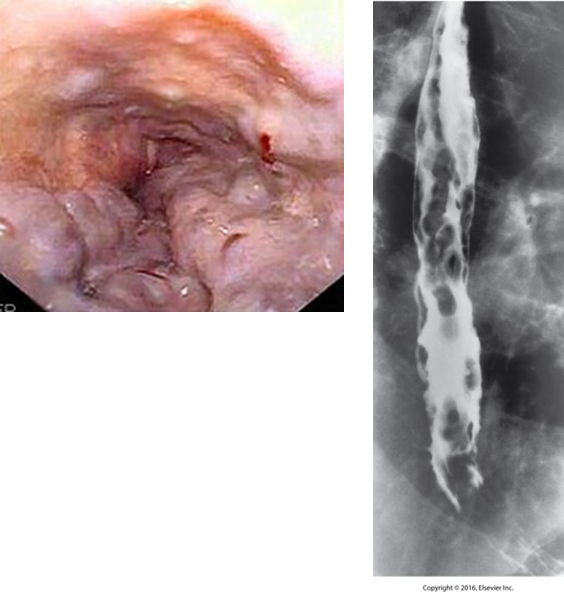
Esophageal Varices
Dilated veins in the distal esophagus.
Caused by portal hypertension.
May bleed.
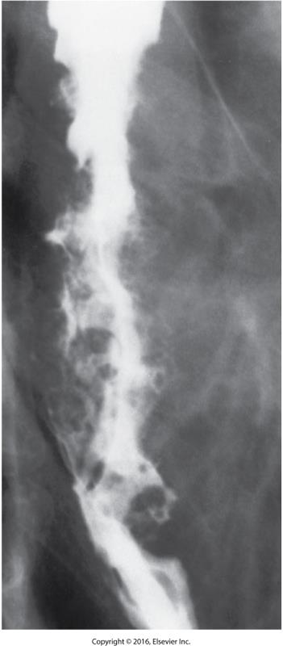
Radiological Appearance
Wavy border, thickening folds
Appear as round or oval filling defects (beads
Foreign Body

Are radiopaque / radiolucent “objects” that are seen inside the body.
Esophageal Cancer
Most are squamous cell type.
Most common site is esophagogastric junction.
Associated with excessive alcohol intake and smoking.
Dysphagia occurs late in the disease.
Demonstrated on double contrast barium swallow.
CT with contrast.
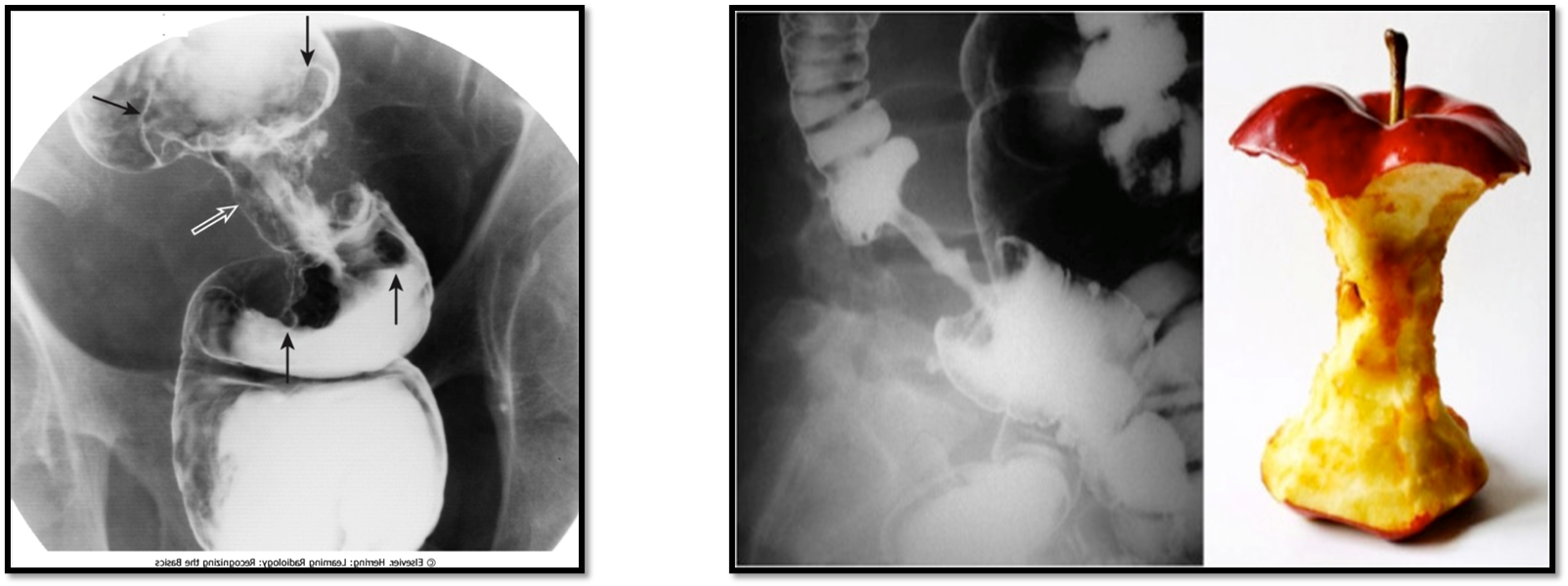
Radiological Appearance:
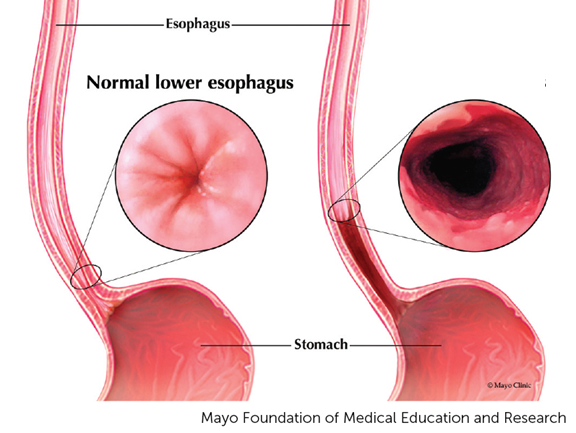
Gastroesophageal Reflux
This disease occurs when the cardiac sphincter does not completely close, stomach acid and contents reflux back into the esophagus.
When the condition is chronic and permanent changes to the esophagus occurs, it is called ________.
This is caused by scarring of the distal esophagus by chronic reflux.
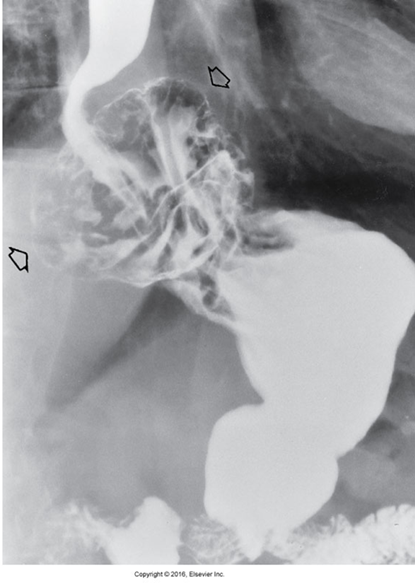
Hiatal Hernia
Protrusion of a portion of the stomach into the thoracic cavity through the esophageal hiatus in the diaphragm.
Radiological Appearance:
Appear as soft tissue mass in posterior mediastinum with air fluid level.
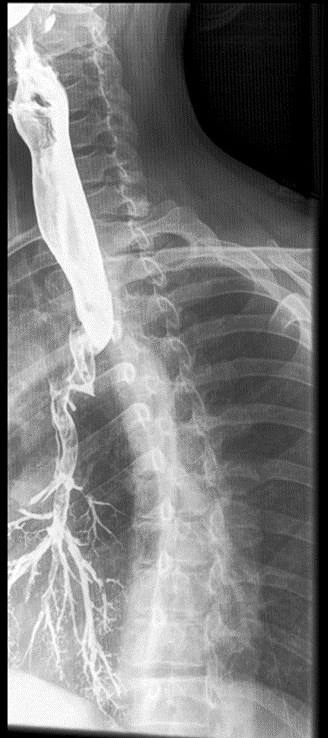
Tracheoesophageal Fistula
Congenital form – results from the failure of the esophageal lumen to develop completely separate from the trachea.
Acquired type – caused by cancer, infection, trauma, instrumentation perforation.
Radiological Appearance:
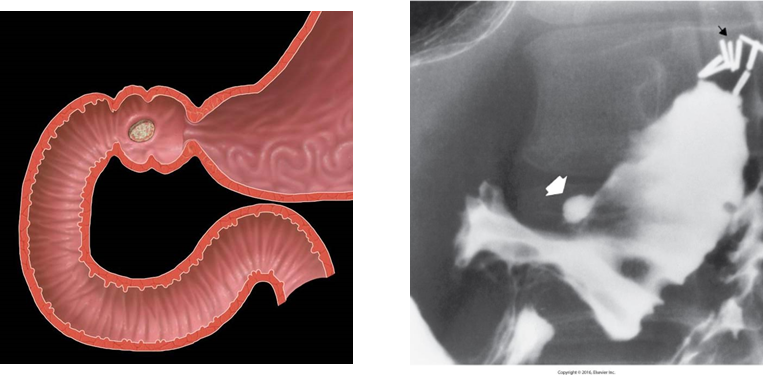
Peptic / Duodenal Ulcer
is a group of inflammatory processes involving the stomach and duodenum.
It is caused by the action of acid and the enzyme pepsin secreted by the stomach.
Most common location is the lesser curvature.
Major complications:
Hemorrhage (the most common cause of acute upper gastrointestinal bleeding).
Gastric outlet obstruction.
Perforation (Common cause of pneumoperitoneum with peritonitis).
Radiological Appearance:
Small collection of barium projection from the lumen.
Secondary sign- thickening of mucosal folds.
Hypertrophic Pyloric stenosis
is also known as infantile hypertrophic pyloric stenosis (IHPS).
Two muscular layers of the pylorus become hyperplastic and hypertrophic.
causes obstruction (incomplete or complete), preventing food from entering into the duodenum.
Can be palpated.
Demonstrates as:
Lengthening of the gastric antrum and pyloric canal
Edematous and thickened mucosa
Radiological Appearance:
Ultrasound is the modality of choice. It appears as thickened pyloric muscle and elongated pyloric canal.
Small Bowel Obstruction
Most often caused by fibrous adhesions from previous surgery.
Second most common cause is hernias.
Other causes:
Luminal occlusion (gallstone)
intrinsic lesions (neoplastic or inflammatory strictures, vascular insufficiency)
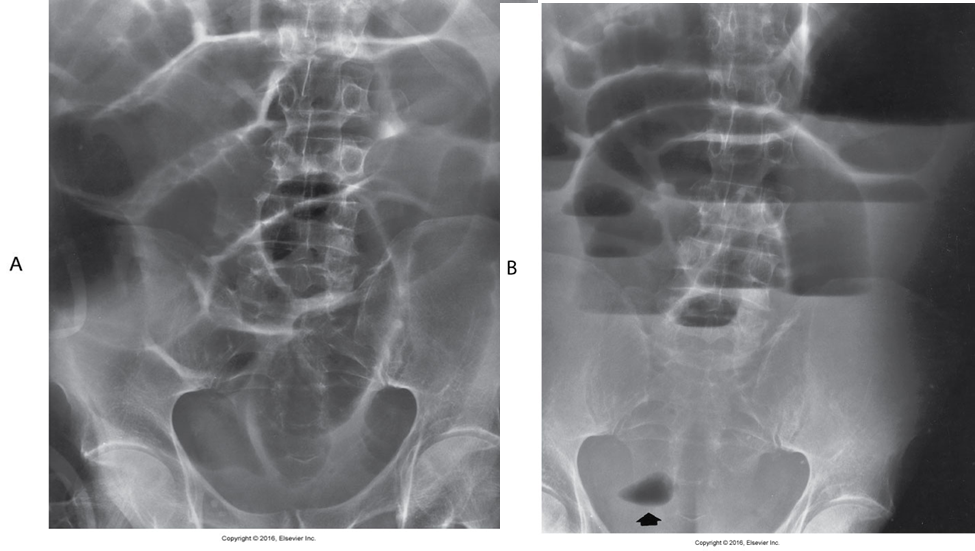
Large Bowel Obstruction
About 70% of this bowel obstruction result from primary colonic carcinoma.
Diverticulitis and volvulus account for most other cases.
It is usually less acute than small bowel obstructions.
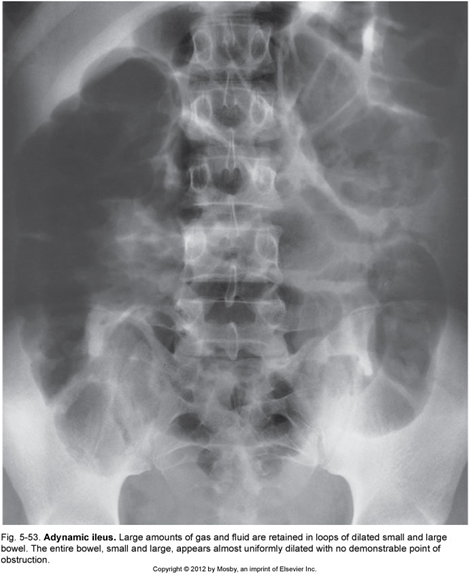
Ileus
A dynamic ileus, also termed paralytic ileus, occurs more often than mechanical bowel obstruction.
It is a common disorder of intestinal motor activity.
Fluid and gas do not progress normally through a non-obstructed small and large bowel.
It occurs in almost every patient who undergoes abdominal surgery.
Other causes:
Peritonitis
Medications that decrease intestinal peristalsis
Radiological Appearance:
Retention of large amounts of gas and fluid in dilated small and large bowel.
No demonstrable point of obstruction.
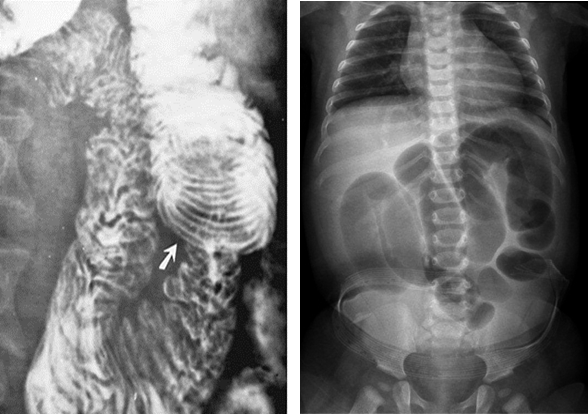
Intussusception
is the telescoping of one part of the intestinal tract into another because of peristalsis.
It forces the proximal segment of bowel to move distally within the outer portion.
Progresses forward causing increased obstruction.
Can compromise the vascular supply and produce ischemic necrosis of the intussuscepted bowel.
Common in ileocolic (ileum and colon) (ileocecal valve – ileum opens in to large intestine) region.
More common in children.
Radiological Appearance
Coiled-spring appearance of barium trapped between the intussusceptum and surrounding bowel.
A bowel obstruction (and therefore air-fluid levels and bowel dilation) proximal to it. There may be an absence of gas in the distal collapsed bowel.
Volvulus
refers to a twisting of the bowel on itself.
May cause obstruction.
Most common sites:
Cecum
Sigmoid
Water soluble enema may be therapeutic and resolve obstruction.
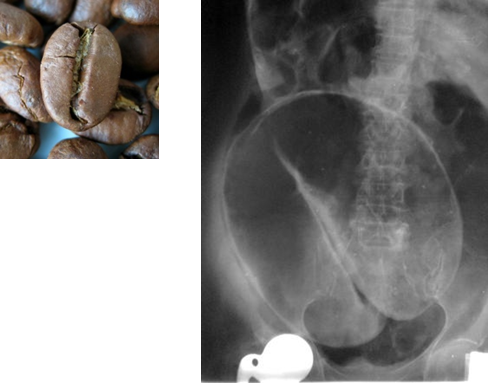
Sigmoid Volvulus
Radiological Appearance:
Coffee bean sign
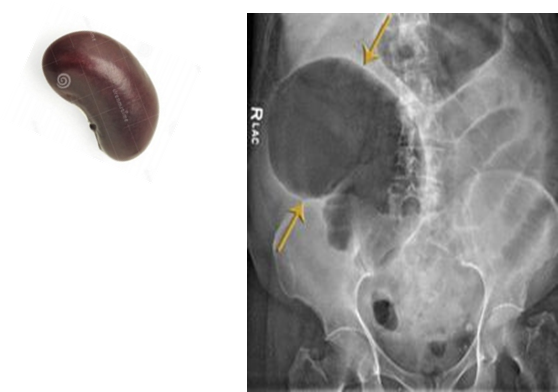
Caecal volvulus
Radiological Appearance:
Kidney bean sign
Crohn’s Disease
is an idiopathic, chronic, inflammatory bowel disease (IBD).
Although it can affect any part of the GI tract, the most affected part is the terminal area of the ileum.
It is most common in young adults.
Cause is unknown
It causes long term inflammation of the bowel.
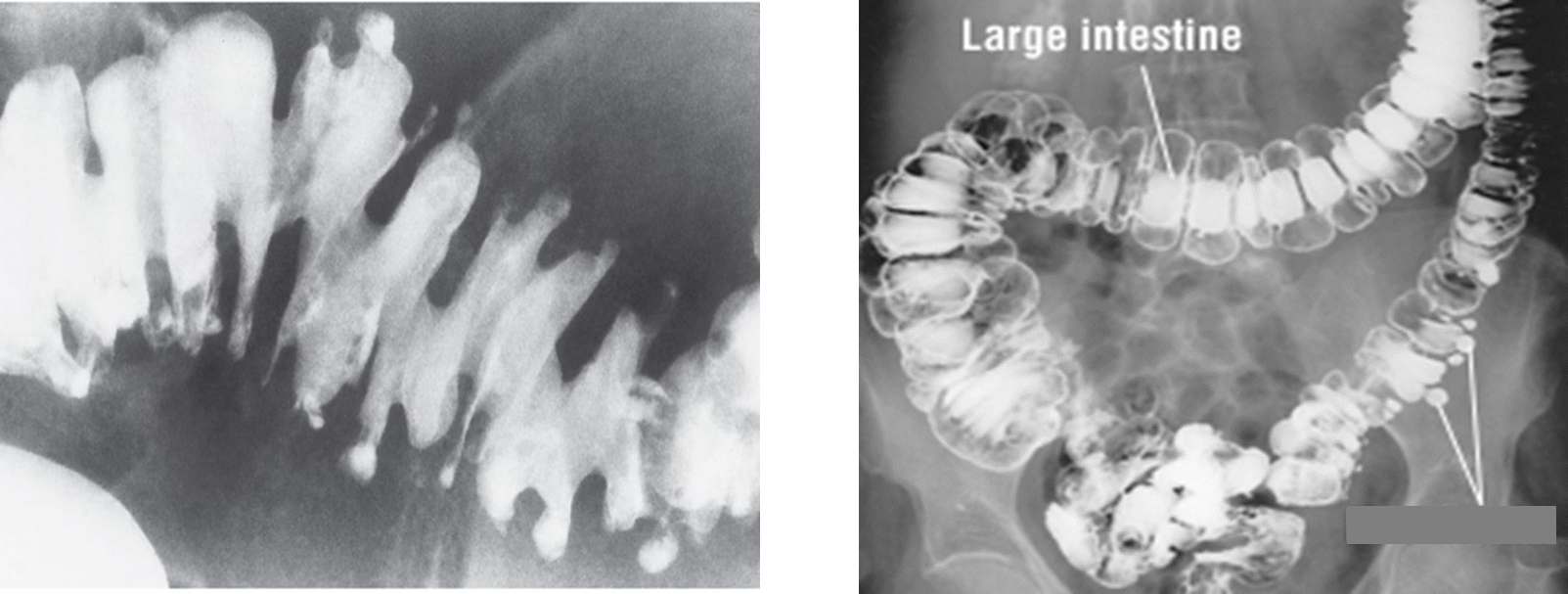
Radiological Appearance:
Skip lesions, in severe cases it resembles a cobblestone appearance

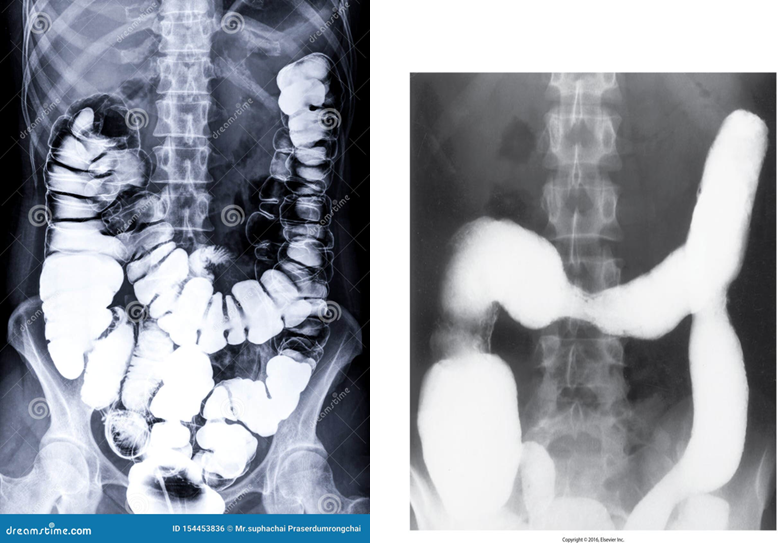
Ulcerative Colitis
is an idiopathic inflammatory disease of the bowel.
Begins in recto-sigmoid area
It causes long term inflammation of the colon and rectum.
Increased risk of malignancy is also associated.
Involves mucosal layer of colon.
Radiological Appearance:
Double contrast barium enema of early __ show fine granularity of the mucosa.
Double contrast barium enema of chronic __ show a Lead pipe sign (colon). The diseased segment of the colon exhibits a complete loss of pouch markings, resulting in a smooth-walled, cylindrical appearance.
Colorectal Cancer
_____ is the third leading cause of cancer death in the United States.
Peak age incidence is 50 to 70 years old.
It is twice as common in men.
About half of colon carcinomas occur in the rectum and sigmoid.
Obstruction is a common finding
Predisposing factors:
Long-term ulcerative colitis (UD)
Familial polyposis (glandular polyps in the colon and rectum).
Radiological Appearance:
Apple core sign
Diverticulitis
is outpouchings that are acquired herniation's of mucosa and submucosa through the muscular layers at points of weakness in the bowel wall.
Radiological Appearance:
Saw-toothed appearance
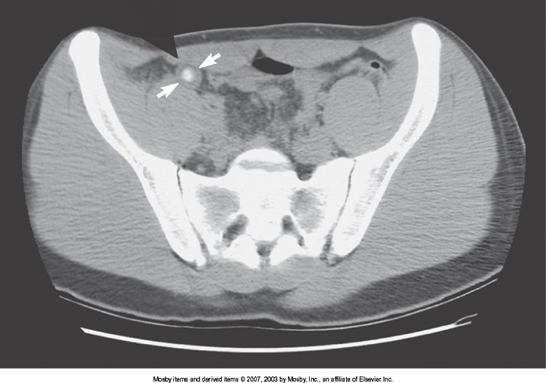
Appendicitis
is the inflammation of the appendix.
Radiological Appearance:
Diameter > 6mm
Peri appendiceal fat stranding
Linear or tubular extension

Cholelithiasis (Gallstones)
Stones found in the gallbladder
Two major types of ____:
Cholesterol – predominant type
Pigment
Radiological Appearance:
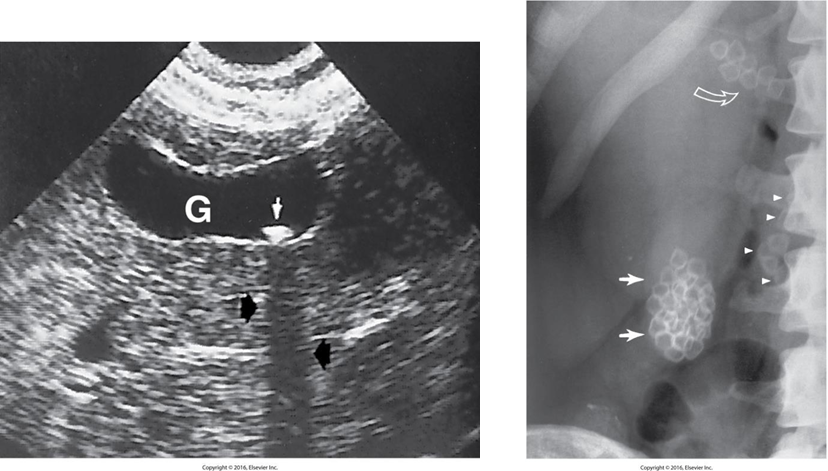
Acute Cholecystitis
is acute inflammation of the gallbladder.
It is usually caused by cystic duct obstruction by a gallstone.
Thickened gallbladders walls (>3mm)
Chronic Cholecystitis
Result of numerous attacks of acute cholecystitis with subsequent fibrosis of the gallbladder wall.
Clinically, patients may have some transient RUQ pain but not the tenderness as experienced with acute cholecystitis.
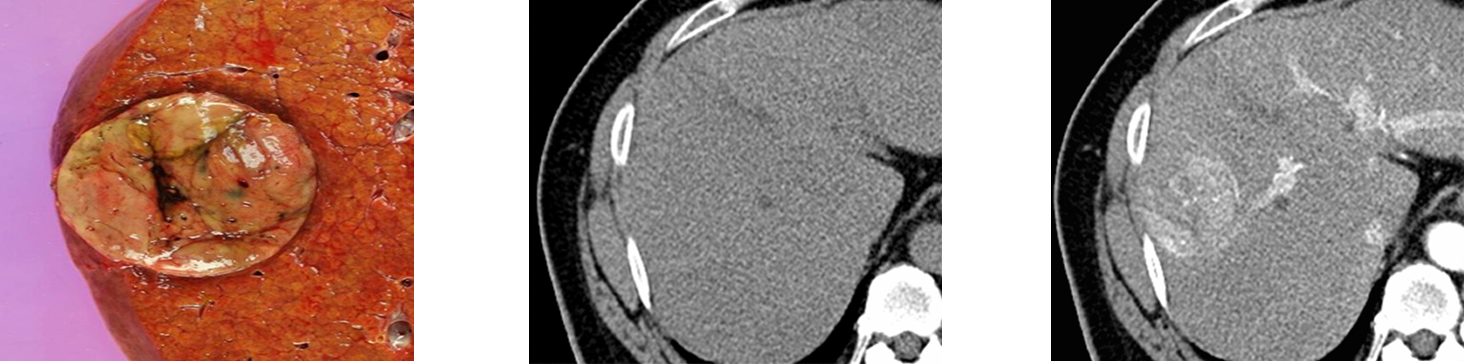
Hepatocellular Carcinoma (HCC)
______ is primary liver cell cancer.
It is most common in those with cirrhosis.
CT is modality of choice for diagnosis.
Cirrhosis
Refers to the chronic destruction of liver cells and structure, with nodular regeneration of liver parenchyma and fibrosis.
It is an end-stage liver disease.
The major cause is chronic alcoholism (i.e., 10 to 20 years of alcohol abuse).
Most characteristic symptom is ascites (Fluid accumulation in the abdomen).
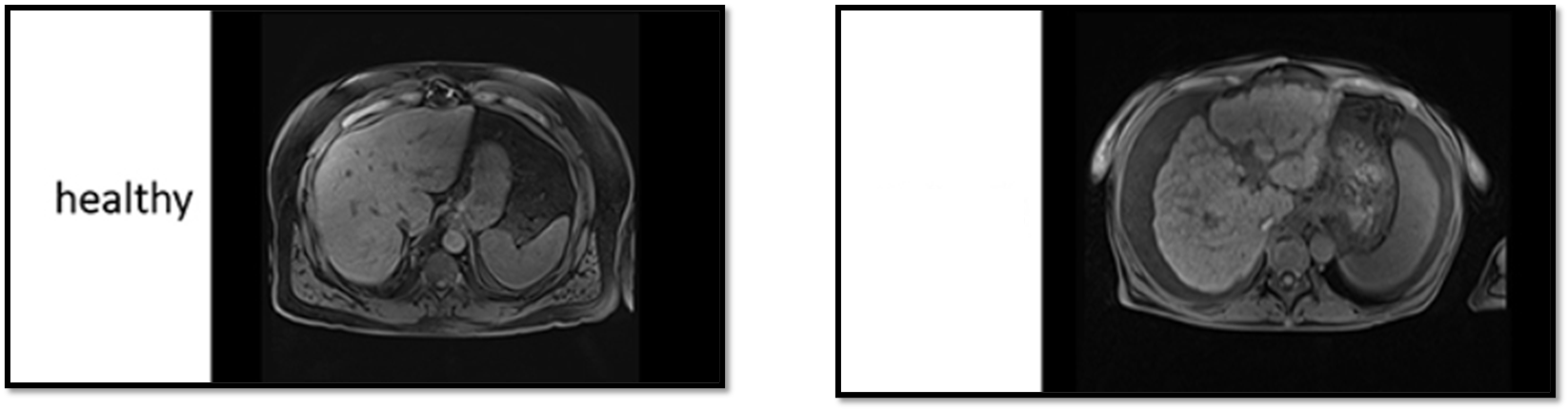
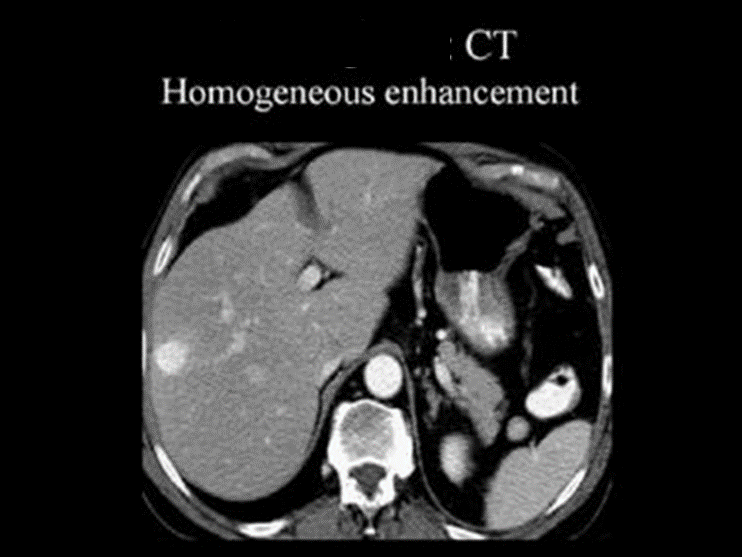
Hemangioma
An abnormal dense cluster of blood vessels.
Can be anywhere. Most common on the face, chest, back, and scalp.
Can be found in the liver.
Thought to be congenital.
Adenocarcinoma
Most common type of cancer of the pancreas is _____.
advanced at time of diagnosis.
Prognosis is poor.
Most common site is the head of the pancreas.
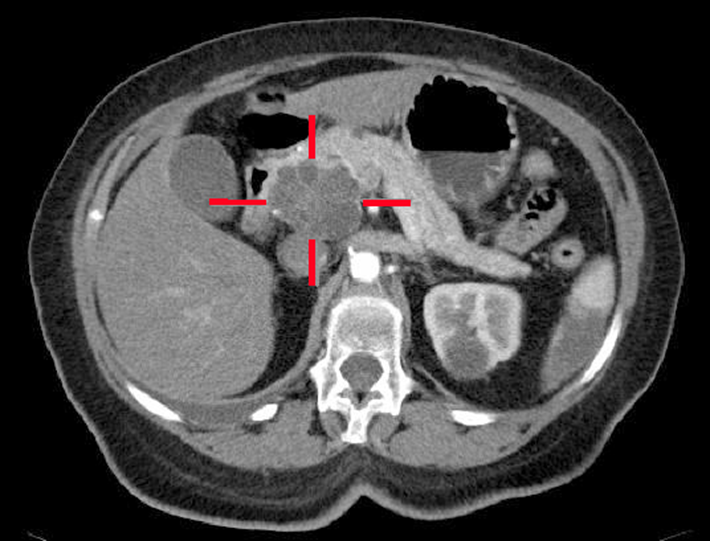
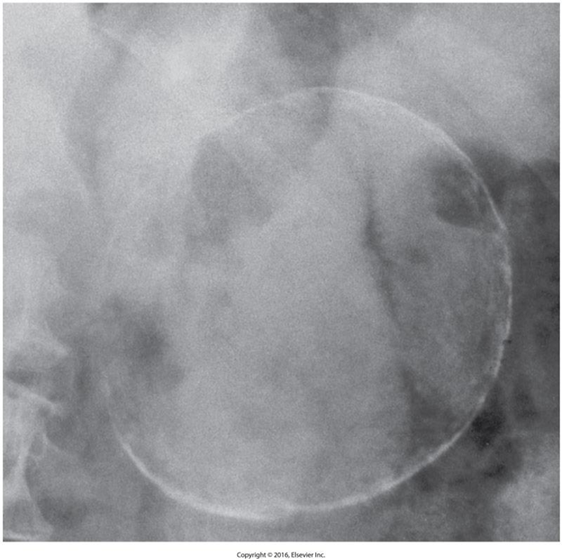
Pancreatic Pseudocyst
is defined as fluid-filled cavity.
They occur due to inflammation, necrosis, or hemorrhage.
Causes:
Acute pancreatitis
Trauma
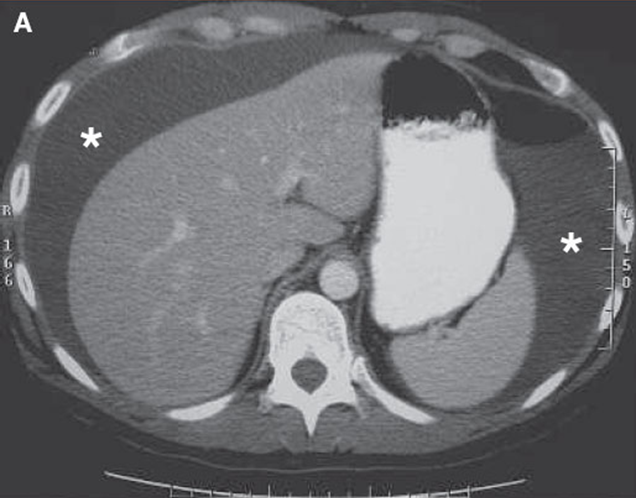
Splenomegaly
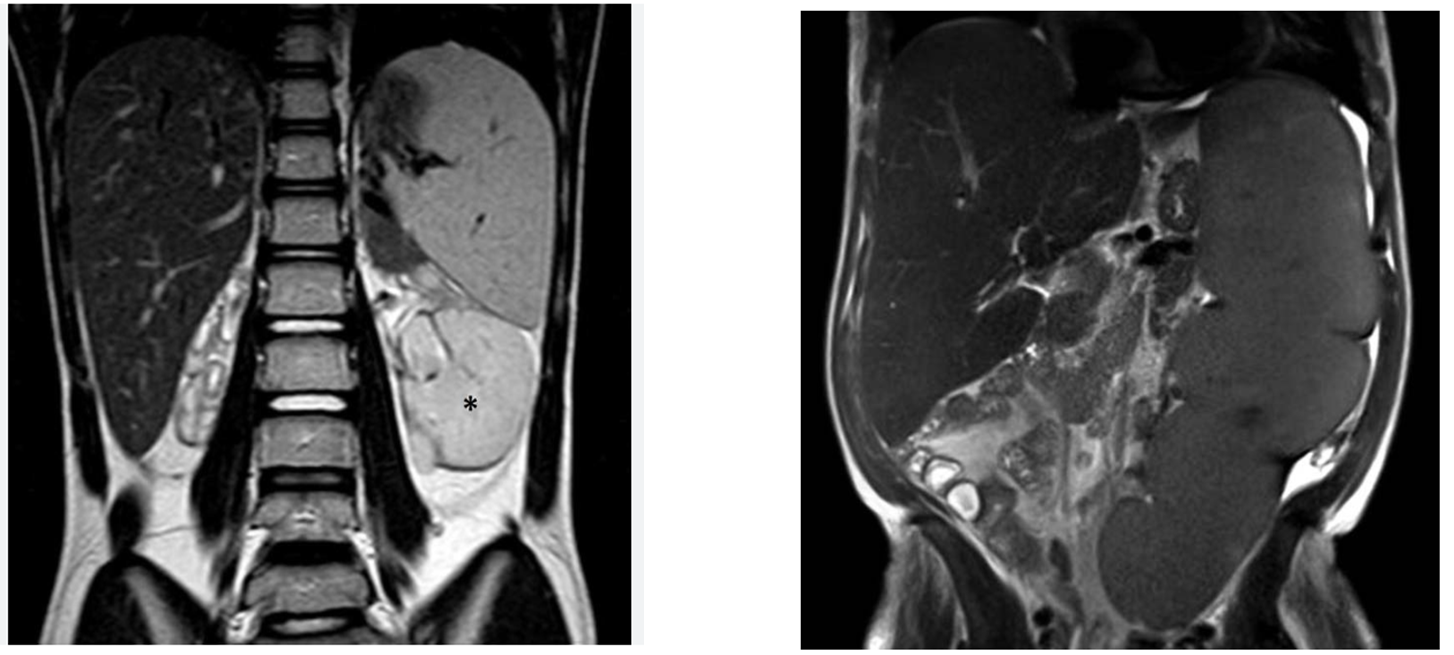
Ascites
Fluid in the peritoneal cavity
This is not a primary pathology. This is always a symptom of a bigger pathology
Common causes are:
Cirrhosis
Carcinoma
Situs Inversus
A rare congenital disorder where all of the organs and vessels develop on the opposite side of the body.
Pneumoperitoneum
Lung Hyperexpansion
Diaphragmatic Rupture
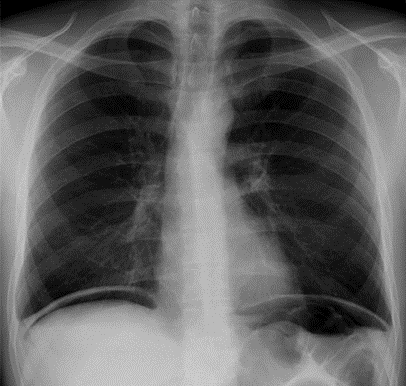
Penumothorax
A _____ forms when there is air trapped between the outer layer of pleura and the inner chest wall.
Trauma that causes penetrating injury (e.g. stabbing, gunshot, or fractured rib) is the main cause of _____.
Radiological Appearance:
Decreased lung volume
No vascular markings
tracheal deviation

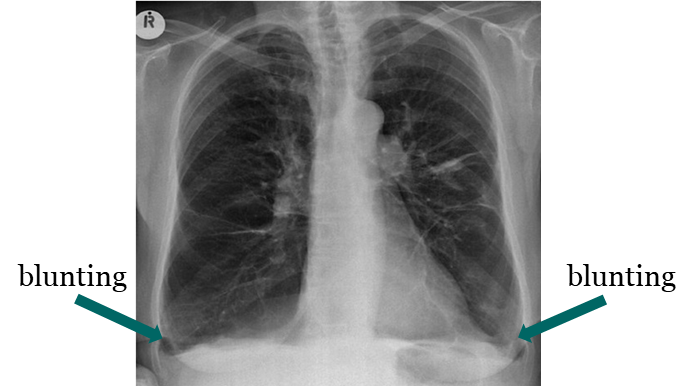
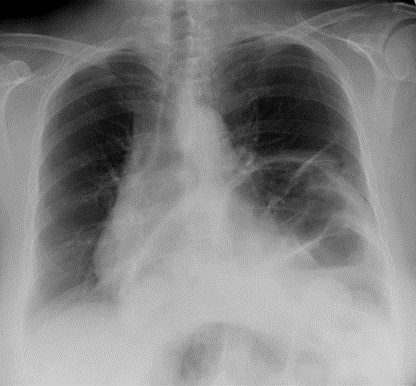
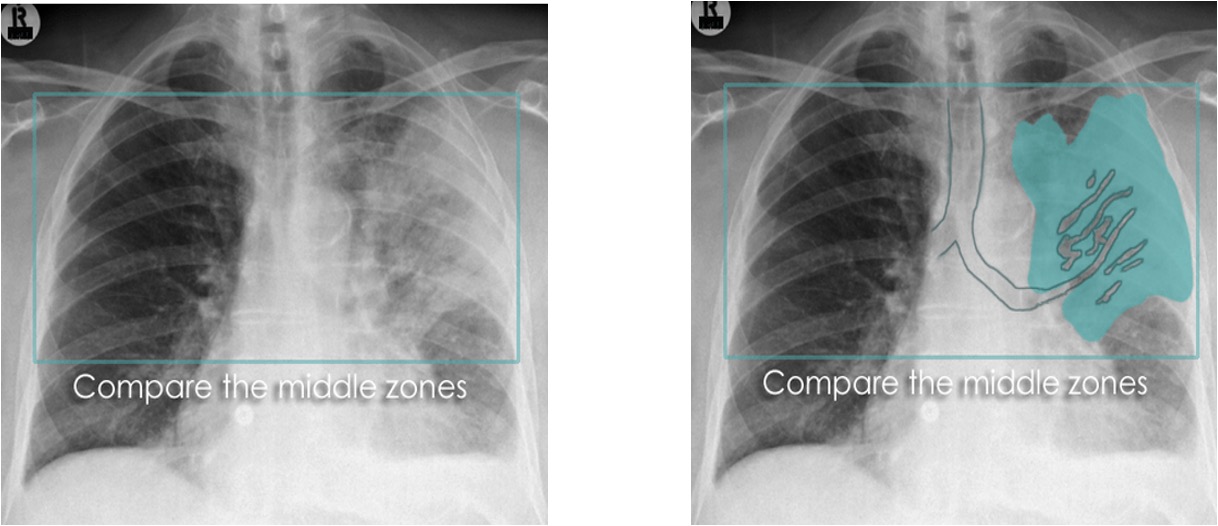
Pleural Effusion
____ is defined as the accumulation of fluid in the pleural space.
____ is seen in the costophrenic angle only (seen on Lat. views), unless it is a high level ___ (Lat. and PA views).
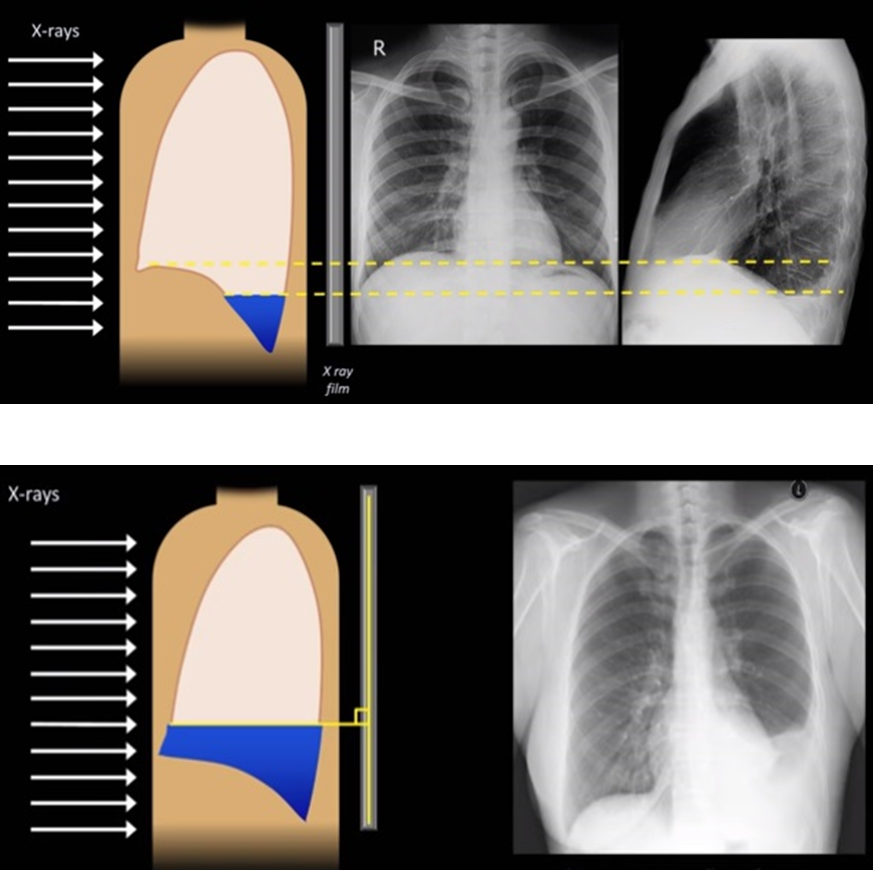
Subpulmonic effusion
____ is an accumulation of fluid between the lung base and diaphragm. It does not blunt the costophrenic angles.

Empyema
is defined as a rare accumulation of infected liquid or frank pus in the pleural space.
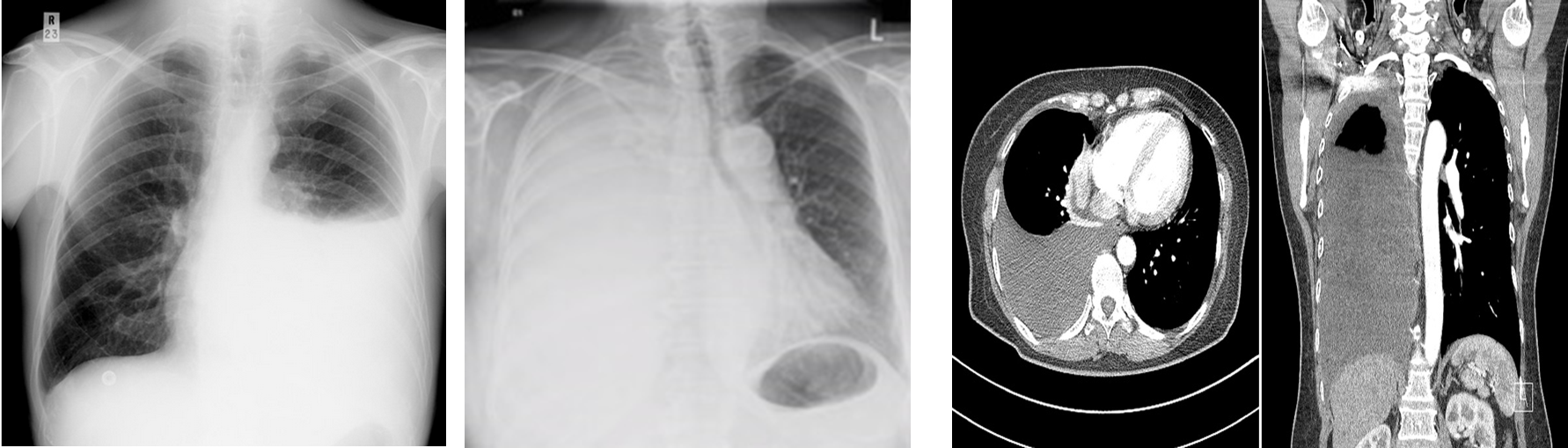
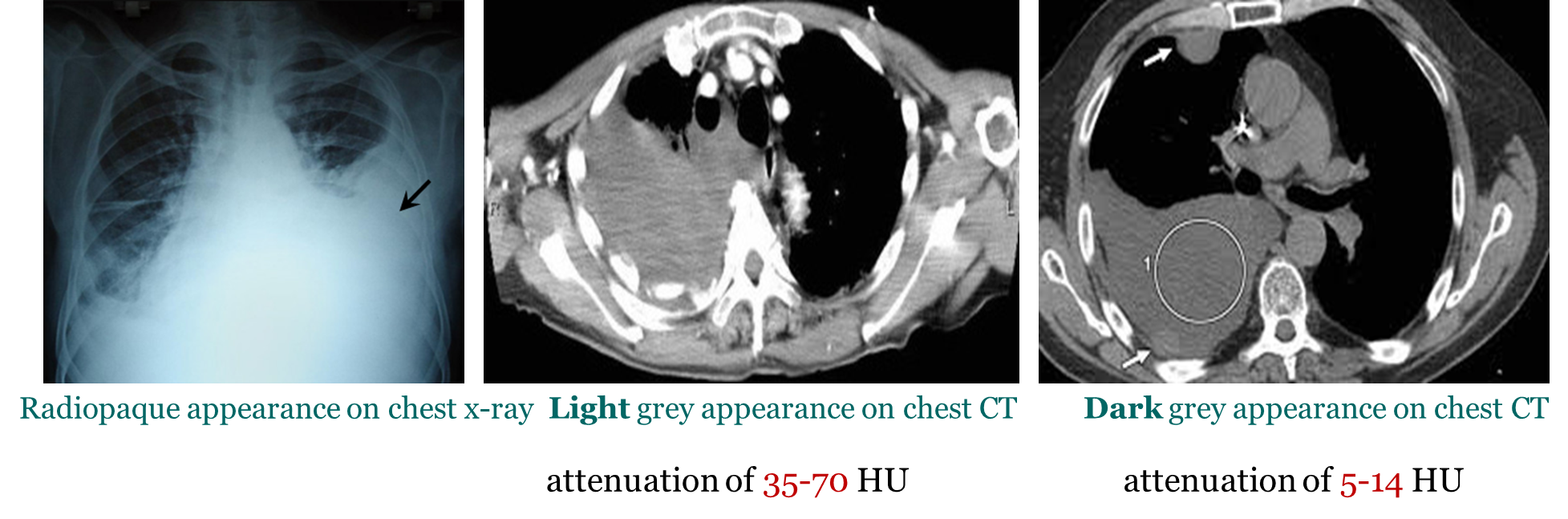
Hemothorax
_____ is a collection of the blood within the plural space (between visceral and parietal layers).
This pathology typically has an attenuation of 35-70 HU.
Pleural effusion typically has an attenuation of 5-14 HU.
Asbestos plaques
Small areas of thickened tissue in the lung lining, or pleura. They typically develop 20 – 30 years after prolonged asbestos exposure (mainly in coal mines).

Consolidation
describes the filling of the air spaces of the lung with material other thena air
CXR appearance reflect the loss of air, hence the increase in opacity
Consolidation Pneumonia
Type of Consolidation
Air spaces filled with pus
Consolidation Pulmonary Hemorrhage
Type of consolidation
Air spaces filled with blood
Consolidation Pulmonary Edema
Type of consolidation
Air spaces filled with fluid
Consolidation Cancer
Type of consolidation
Air spaces filled with cells
Severe Acute Respiratory Syndrome (SARS)
is an air-space disease and may be indistinguishable from pneumonia of other causes
Ground glass opacity sign
This refers to the hazy gray areas that show up in CT scans of the lungs

Tuberculosis
Caused by Myobacterium tuberculosis
Spreads mainly by droplets in the air
Primarily a disease of the lungs but can spread to GI, GU, and skeletal system
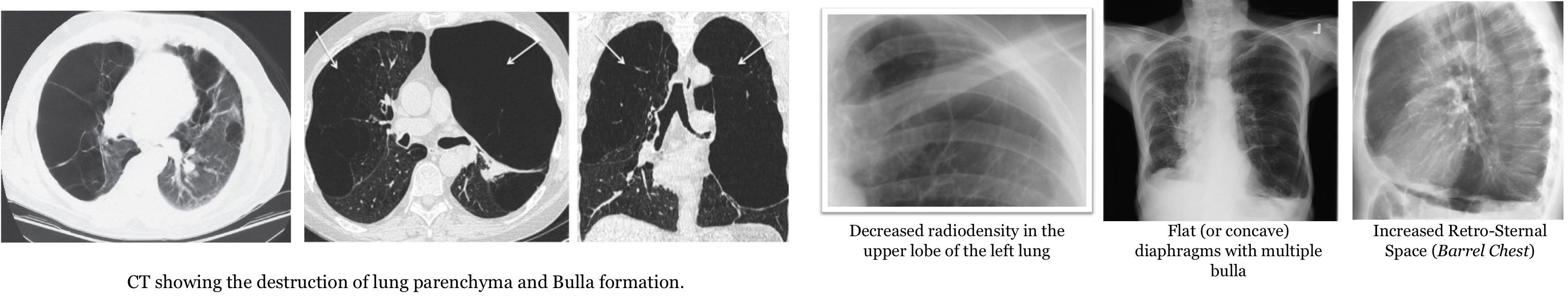
Emphysema
Abnormally expanded air spaces distal to terminal bronchiole with destruction of walls of involved air spaces.
The alveolar walls are destroyed trapping air in the spaces on exhalation.
Lung elastic recoil is damaged further increasing the air trapped in the lungs.
Radiological Appearance
lungs are hyperinflated, decreased radiodensity
Flat or concave diaphragms
Bullae formation: large radiolucent air containing systic spaces
Lung Collapse
This occurs due to obstruction of supplying bronchus by aspirated foreign body or any other material,
Types:
Partial Collapse (Atelectasis)
Complete collape
Radiological Appearance
increased brightness
Tracheal deviation
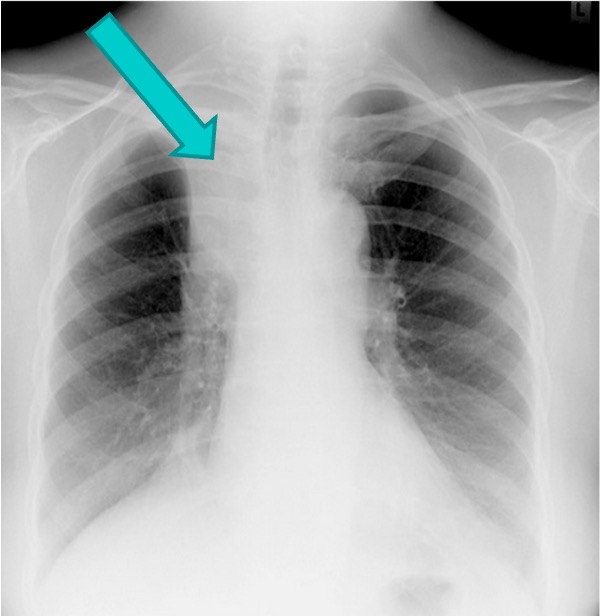
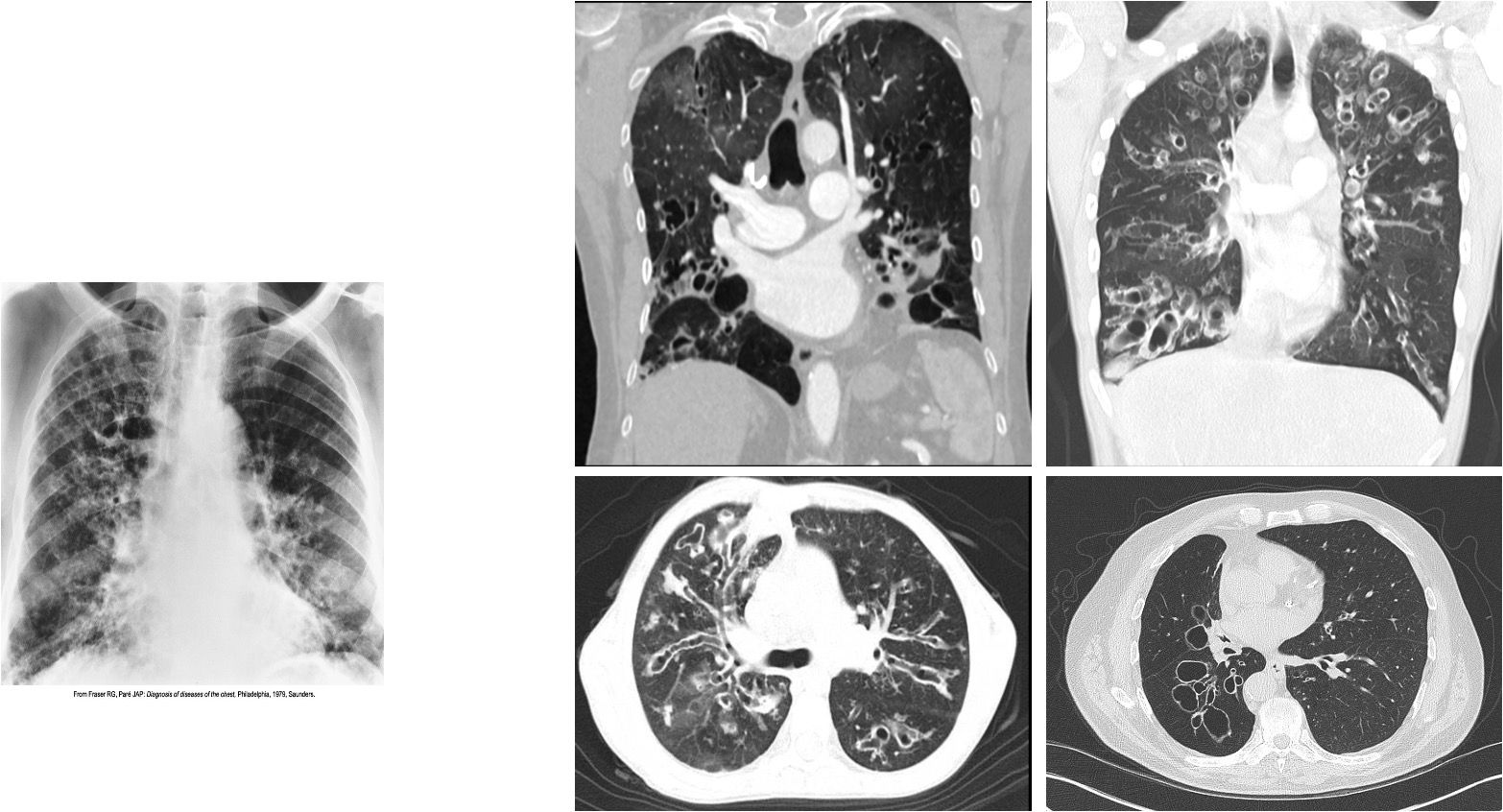
Bronchiectasis
Severe coarseninh of interstial markings involves the bases and right upper lobe
oval and circular cystic spaces, which resembles a honeycomb-like pattern, are best seen in the right upper lobe.