Sleep Apnea, Pickwickian Syndrome, ARDs, FBA
1/57
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
Sleep Apnea
A condition in which breathing repeatedly stops and disrupts sleep characterized by a temporary decrease in O2 and increase in CO2 in the blood
central, obstructive, mixed (complex)
3 types of sleep apnea
Central sleep apnea (CSA)
What type of sleep apnea can occur as a primary medical condition or secondary due to something like a stroke, HF, or medication ADRs?
Treat underlying, CPAP, acetazolamide
If a patient came in reporting frequent waking at night and daytime sleepiness and their partners report that there is NO snoring and periods of no breathing, what’s our treatment plan?
Obstructive Sleep Apnea
Most common form of sleep apnea that contributes to CVD in adults and behavior issues in kids in which patients report snoring, gasping, and snorting while sleeping and their partner’s report significant noises while sleeping
intraluminal pharyngeal pressure becoming negative
During inspiration, what creates the “suctioning force?”
pharyngeal dilator muscles (relaxed when asleep)
Patency of the pharyngeal airway is dependent on
soft palate (most common), tongue, base, lateral pharyngeal walls, epiglottis
What are the sites of collapse in OSA due to relaxation of muscles and lack of structural support in the pharyngeal airway?
obesity, adipose deposition in the laryngopharngeal areas, soft tissue weight reduces chest compliance, male, smoking, family hx, craniofacial/upper airway abnormalities, down syndrome, adentonsillar hypertrophy, menopause, hypothyroidism
Risk factors associated with OSA?
overnight polysomnography
Patient reports to the clinic for difficulty sleeping. He states that he wakes up frequently at night and is super sleepy during the day. The patient’s partner reports that the patient snoring, gasping, and restless while sleeping. Patient also reports dry mouth, nocturia, morning HA, trouble concentrating and a recent weight gain. On a physical you note a low-lying soft palate and a bulky uvula. Vitals are stable with the exception of HTN. What is the gold standard definitive diagnostic for this condition?
dry mouth, recent weight gain, nocturnal heartburn, diaphoresis of chest and neck, nocturia, morning HA, trouble concentrating, irritability, mood disturbances
What are non-specific findings associated with OSA?
small oropharynx with large tongue, low-lying soft palate, bulky uvula, large tonsils, high-arched palate, micro-retrognathia, nasal polyps, septal deviation
What ENT findings may be present with OSA
CBC (erythrocytosis), fiberoptic ENT exam (examine upper airway), overnight polysomnography
What are some diagnostics you can use for sleep apnea?
EEG, EKG, EOG (retina), EMG (muscles), pulse ox, measurement of respiratory airflow and effort
What does a overnight polysomnography measure?
Bradycardia and O2 sats falling during apneic periods, tachydysrhythmias as ventilation occurs
For a patient with sleep apnea what are you going to find on a overnight polysomnography?
HTN (maybe resistant), CAD, HF, arrhythmias, atherosclerosis, stroke, diabetes, depression, daytime sleepiness
What are some on the health consequences associated with sleep fragmentation, cortical arousal, and intermittent hypoxemia associated with sleep apnea?
Weight loss, CPAP (1st line), avoid alcohol/hypnotic meds, mechanical devices to hold jaw anteriorly, UPPP, Nasal septoplasty, tracheostomy (last report)
How are we treating OSA?
Uvulopalatopharyngoplasty (UPPP)
A surgical resection of the pharyngeal soft tissue and removal of the soft palate’s free edge and uvula leads to 50% improvement
nasal septoplasty
What treatment for OSA is only useful if a nasal septal deformity is causing the obstruction?
tracheostomy
What is the last resort and the only definitive treatment OSA?
CPAP, acetazolamide
What CSA treatment options do not eliminate but reduce the number of central apneic episodes?
creates mild metabolic acidosis which stimulates respirations
How does acetazolamide help with CSA?
Obesity hypoventilation syndrome (pickwickian syndrome)
What has a similar pathophysiology like OSA but occurs while awake and with obese patients and typically is due to not enough air entering alveoli with each breath eventually leading to hypercapnia and hypoxia?
BMI above 30, PaCO2 greater than 45 and other known causes hypercapnia (exclusion), sleep disordered breathing
What are the diagnostic guidelines for obesity hypoventilation syndrome?
Leptin resistance (leptin stimulates ventilation)
What is one of the theories as to why obesity hypoventilation syndrome occurs?
50% prevalence of obesity hypoventilation syndrome
Severe obesity (BMI 50+) is associated with
severe hypoxemic hypercapnic respiratory failure, Right failure from pulm HTN, DOE, elevated jugular vein pressure, hepatomegaly, pedal edema, polycythemia
What are some severe symptoms associated with obesity hypoventilation syndrome?
PaCO2 >45, HCO3 > 27, PaO2 < 70 with normal A-a gradient
How’s your blood gas look with pickwickian syndrome?
normal/restrictive pattern
How’s your spirometry look with pickwickian syndrome?
CPAP/BiPAP (1st line), avoid EtOH/sedatives, weight loss, tracheostomy (last report)
What is our treatment plan for obesity hypoventilation syndrome?
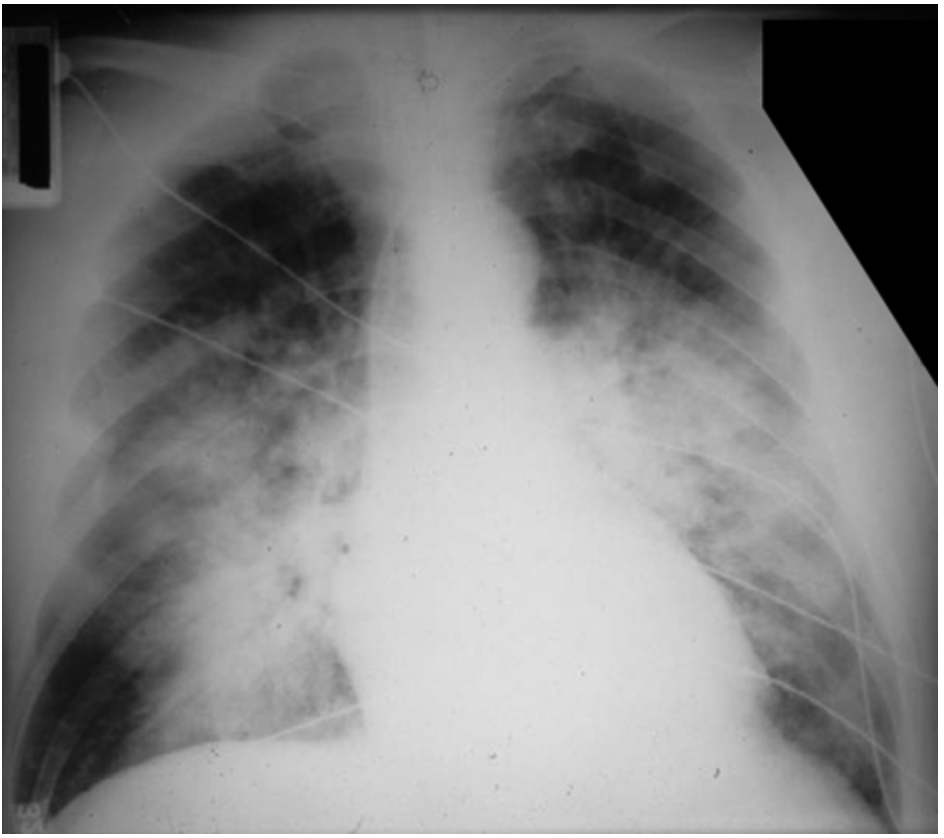
Acute respiratory distress syndrome (ARDS)
An acute, diffuse, inflammatory lung injury associated from a variety of etiologies such as sepsis, aspiration pneumonitis, pneumonia, pulmonary contusion, toxic inhalation, near-drowning, multiple blood transfusion, pancreatitis, heroin/cocaine, COVID-19
severe dyspnea (not from HF/volume overload) of rapid onset within 7 days, hypoxemia, diffuse pulmonary infiltrates not explained by pleural effusions, atelectasis, nodules
What are the 3 must haves for ARDS?
Exudative, Proliferative, fibrotic
What are the 3 phases of ARDS?
exudative phase (days 1-7)
What phase of ARDS is characterized by the injury of type pneumocytes, loss of surfactant, alveolar capillary barrier damage and increased vascular permeability leading to the deposition/accumulation of edema that is rich in proteins in interstitial and alveolar spaces and requires intubation and ventilation?
Proliferative (day 7-21)
What phase of ARDS is characterized by rapid recovery and removal from mechanical ventilations however, dyspnea, tachypnea, and hypoxemia remain and new type II pneumocytes proliferate?
Fibrotic phase (day 21+)
What phase of ARDS is characterized by the conversion of the exudate into alveolar and interstitial fibrosis leading to increased risk of pneumothorax and reductions in lung compliance - NOT ALL PATIENTS GO THROUGH THIS
Prone positioning, positive pressure mechanical ventilation, treat underlying cause, intubate, restricted fluid intake and diuresis
Patient reports to the ER for SOB. He states that he almost drowned 5 days ago due to a boating accident. On a physical exam you note labored breathing, retractions, crackles, and rales. Vitals are stable with the exception of 144 bpm, 27 RR, and 89% on RA. CXR shows diffuse/patchy bilateral infiltrates in the dependent lung zones. What is your treatment plan?
immediate hazard
In peds an upper airway obstruction is a
immediate/long term hazards
In peds a lower airway obstruction is a
less than 3 y/o
Peak incidence of pediatric FBA
food items (peanuts)
What is aspirated more often by infants and toddlers
non-food items (paper clips, coins, marbles, etc)
What is aspirated more often by older kids
round, failure to break apart, compressibility, smooth/slippery
What makes an FBA more dangerous
balloons
most common FBA associated with death
right mainstem bronchi
A majority of FBA end up where?
stridor, wheezing, salivation, dyspnea, hoarseness, voice changes, absence of all dependent breah sounds, acute respiratory distress/failure
Pediatric presentation of a laryngotracheal FBA
coughing, wheezing, hemoptysis, dsypnea, maybe respiratory distress, focal decreased breath sounds, fever, cyanosis
Pediatric presentation of a main bronchi FBA
Chest CT, diagnostic bronchoscopy
What 2 test have a 100% sensitivity for discovering FBAs?
Rigid bronchoscopy (95% success rate), Magill forceps (if equipped)
A 2 y/o presents to the ER for wheezing and stridor. Mom states that this began 30 minutes ago, she was cooking dinner in the other room while the child was playing. You note decreased focal breath sounds and dyspnea. What are treatment options for incomplete obstructions?
dislodge with back blows and chest compressions (infants), Heimlich (older kids), if unconscious start CPR, NO BLIND SWEEPS
How do you treat a complete airway obstruction in peds?
food with incomplete chewing, Nails from holding them in the mouth
What are some common FBAs with adult patients?
Cafe coronary
What is the aspiration of incompletely chewed meat that leads to the inhibition of the vagal nerve response to the heart and presents with atypical choking symptoms and looks like a MI?
cough, fever, hemoptysis, foul-smelling sputum, chest pain, wheeze
What is the adult presentation of FBA?
CXR or neck xray, Chest CT, flexible bronchoscopy (definitive)
What can we use to diagnose an FBA in an adult
attempt to remove with Magill, Heimlich maneuever, CPR once unconscious, NO BLIND SWEEPS
How are we treating a full obstruction in adults?
flexible bronchoscopy
How are we treating a partial obstruction in adults?
flexible
What type of bronchoscopy uses conscious sedation, is a smaller piece of equipment, removes small objects from lower airways, and is used for biopsies, samples. suctioning of small airways?
rigid
What type of bronchoscopy requires general anesthesia, is a large rigid piece of equipment that can remove larger objects from main bronchi and is used for procedures requiring larger tools or biopsies of upper airway and main bronchi?