Lab 5 - Heart Physiology & Electrocardiography (EKG)
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
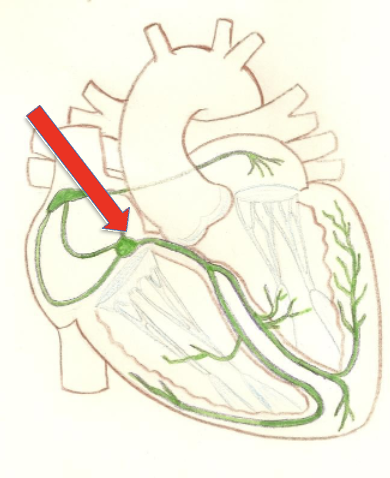
Located in the inferior segment of the interatrial septum, it briefly delays the signal from the SA node while the atria finish contracting.
delayed because fewer gap junctions and smaller diameter of conduction fibers
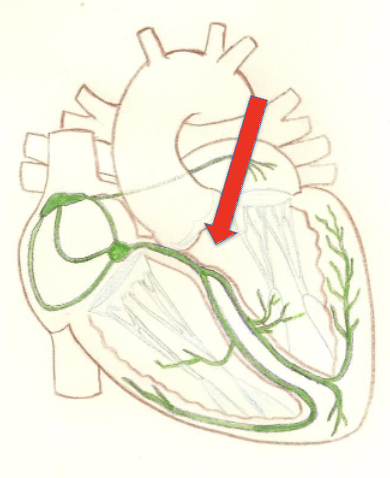
Links atrial conduction to ventricular conduction by receiving signals from the AV node.
located in the superior portion of the interventricular septum
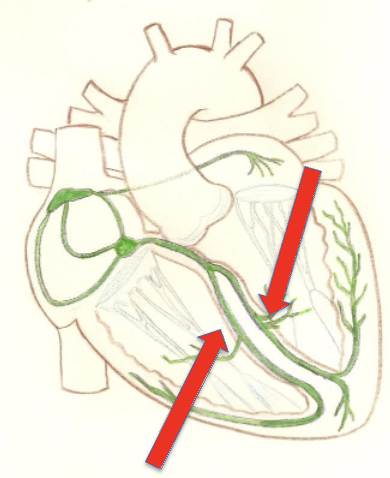
Penetrate into the apex and run into the ventricular walls, these fibers facilitate the bulk of ventricular excitation.
receives signal from the bundle branches and completes the conduction cycle
purkinje network is more elaborate in the left chamber
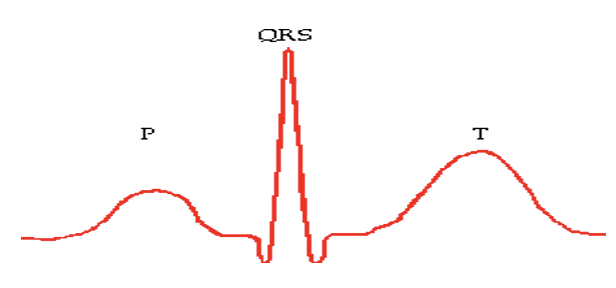
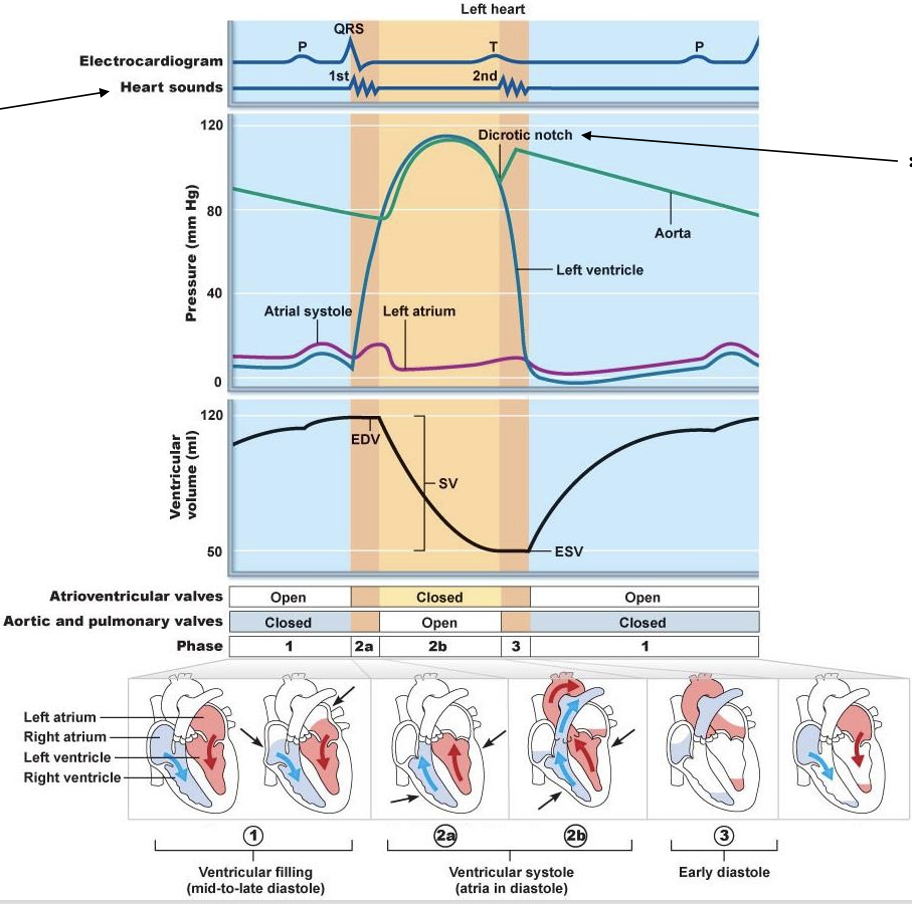
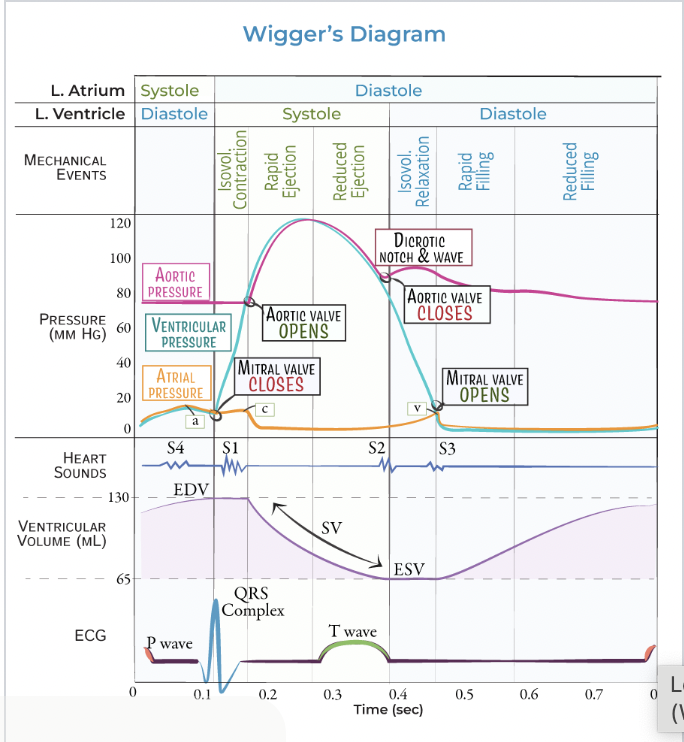
The sum of all electrical potentials generated by the cells of the heart at any time, providing key information about heart rhythm.
normal electrical activity of the heart gives 3 distinct waves
The amount of blood pumped out of each ventricle in a minute, calculated as heart rate multiplied by stroke volume. ( CO = HR x SV)
The volume of blood pumped out by one ventricle with each beat.
correlates with strength of ventricle (SV = EDV - ESV)
ECG lead
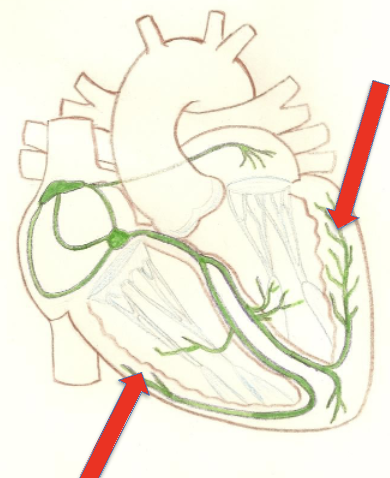
Cardiac Conduction System
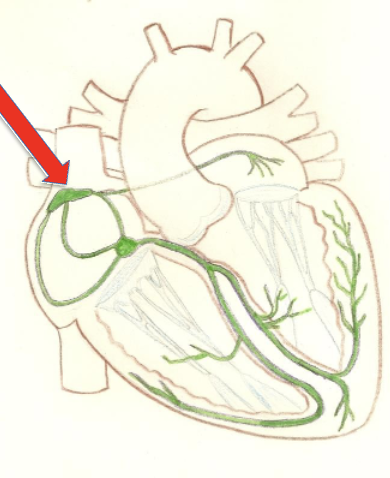
Sinoatrial Node
Atrioventricular Node
Atrioventricular bundle
Bundle branches
Purkinje fibers
Depolarization leads to
contraction
Repolarization leads to
relaxation
Contraction ___ pressure in the respective chamber vice versa for relaxation
increases
Atrioventricular valves __ when ventricular pressure is higher than atrial pressure
close
Semilunar valves ___ when arterial (aorta/pulmonary trunk) pressure exceeds ventricular pressure
close
Blood moves from
an area of high pressure to an area of low pressure
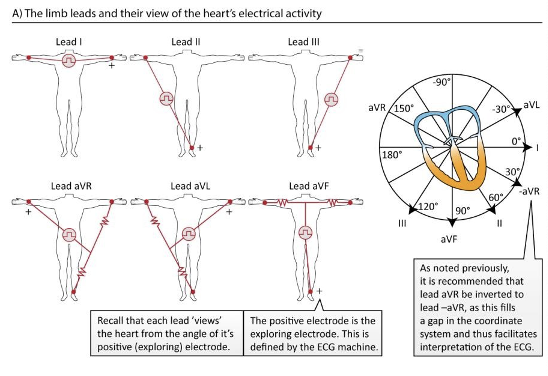
Standard limb leads
I, II, III
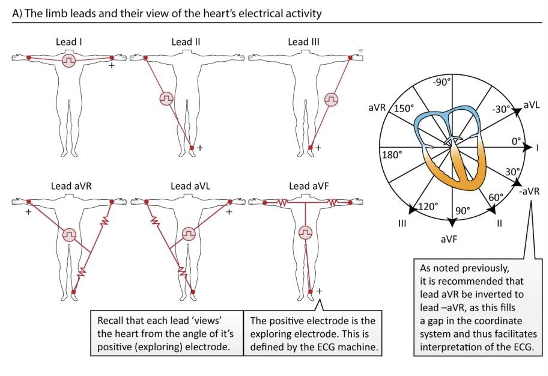
Augmented limb leads
aVR, aVL, aVF
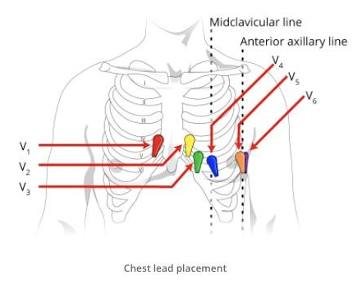
Unipolar chest leads
V1 - V6
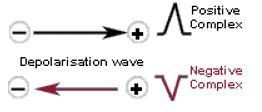
Direction of electrical vector in the heart determines the ECG trace
positive
negative
isoelectric
Left heart
Blood enters atrial chambers of the heart at
low pressure
Blood leaves the ventricles at
higher pressure
high arterial pressure provides
the energy to force blood through the circulatory system
arteries carry blood __ the heart
AWAY
veins carry blood __ the heart
TOWARDS
Are arteries or veins generally more pressurized ?
arteries
heart is enclosed within
Mediastinum - medial cavity of the thorax
apex is located
near the fifth intercoastal space
heart enclosed in sac called
pericardium
fibrous pericardium
anchors, protects, and prevents over filing of the heart
inner serous pericardium
thin, slippery, dual-layered membranous sac around the heart
2 layers - parietal layer, visceral layer (epicardium)
parietal layer
butts up against the fibrous pericardium
visceral layer (epicardium)
integral part of the cardiac wall
pericardial cavity
between the parietal and visceral layers is filled with serous fluid which allows these two layers to slide past one another as the heart beats
Pericarditis
inflammation of the pericardium
can lead to cardiac tamponade
cardiac tamponade
buildup of inflammatory fluids in the pericardial cavity which compresses and impedes the heart
myocardium
thick cardiac muscle layer of the heart
cardiac “skeleton”
branching cardiac muscles cells are arranged in interlacing spiral bundles tethered by crisscrossing collagen and elastic connective tissue fibers
! strengthens and anchors the heart to itself
endothelial endocardium
innermost layer of the heart; lines the heart valves and heart chambers
auricles of atria
allow for additional filling
Muscular ridges of the atria and ventricles
pectinate muscles (ATRIA); trabeculae carnae (VENTRICLES)
fetus exchanges gases where
placenta NOT the lungs
Why does all fetal blood not need to pass through the lungs ?
foramen ovale - opening connects the right and left atrium (allows most blood to bypass the pulmonary circuit)
fossa ovalis
impression of foramen ovale in the interatrial septum
patent foramen ovale
still open; common in adults but usually small and inconsequential
ductus arteriosus
connects the pulmonary trunk and the aorta
patent ductus arteriosus
if left untreated can lead to congestive heart failure
Some congenital heart defects
(congenital - present at birth)
Holes in the interventricular septum, valve malformations, and transpositions of the great vessels of the heart
Papillary muscles in the ventricles
link to atrioventricular valves via the chordae tendinae and function to keep the valves from everting into the atria after they shut
Why is the wall of the left ventricle more massive than the right ?
left ventricle pumps to almost the entire body against a heavy friction load while the right ventricle only pumps to the lungs which is a low pressure, low resistance, low friction circuit
pathological stenosis of the pulmonary vessels
increases pressure in the pulmonary circulation fed by the right ventricle which is not built to pump under high pressure like the left side of the heart is
! can lead to congestive heart failure
where does the heart get a majority of its nourishment from and why?
coronary circulation
heart is too thick for the blood within the chambers to adequately supply the cardiac cells
angina pectoralis
blockage in the coronary arterial circulation fleeting insufficiency of blood supply to the myocardium resulting in chest pain
myocardial infarction (heart attack)
prolonged coronary arterial blockage resulting in an oxygen and nutrient deficit in the supplied myocardium and subsequent death of these cells
cardiac cells
do not regenerate; tissue is replaced with a non-contractile scar tissue
because the cardiac cells are connected by gap junctions
the conduction system is critical to first start the contraction at the cranial portion of the atria and move down the wrong blood into the ventricles, and then rapidly shunt the signal to the apex of the heart do that the contraction will spread up to wring blood out of the ventricles and into the great vessels
pacemaker cells of the cardiac conduction system
have an unstable resting membrane potential that continuously discharges in the direction of depolarization until it reaches threshold which activates calcium channels to open and at that point generates an action potential of depolarization
more and more as time passes, due to slow sodium channels that open in response to hyperpolarization at the end of an action potential
shifting membrane potentials
termed pacemaker potential
repolarization
the falling phase
due to the opening of potassium channels which remain open until hyperpolarization closes them and opens slow sodium channels to begin the porcess again
cardiac contractions
not dependent upon nerve supply
innervation by parasympathetic vagus nerve slows the heart, and sympathetic nerves speed the basic cardiac rhythm
! CNS can affect rhythm
sinus arrythmia
respiratory activity affects the heart rate to increase as you breathe in and decrease as you breathe out
sinus rhythm
generated by SA node because the cells auto-depolarize at the greatest rate
only electrical connection between the atria and the ventricles is via the
atrioventricular (AV) node
arrhythmia
irregular heart rhythm
can be caused by defects in the conduction system
fibrillate
rapid irregular contractions not driven by SA node but instead by rapid activity in other regions of the heart
junctional rhythm
slower, no P wave
excessive use of caffeine or nicotine can cause
small regions of the heart to become hyperexcitable and outpace the SA node
resulting in premature contraction and extra time needed for the heart to fill before next contraction
heart block
ventricles receive deficient pacing signals due to damage at AV node or purkinje fibers
often treated with an implantable artificial pacemaker
second degree heart block
some SA node impulses do not conduct through the AV node
resulting in more P waves than QRS complexes on an ECG
total heart block
ventricles just beat on their own, way too slow, intrinsic rhythm
cardiac cycle
involves sequential contraction of the atria and ventricles; combined electrical activity of the different myocardial cells produces electrical currents that spread through the body fluids (large enough to be detected by recording electrodes placed on the skin)
cardiac action potential
3 phases
rapid depolarization
plateau depolarization
repolarization
rapid depolarization
as a result of fast voltage gated sodium channels opening in the sarcolemma
plateau depolarization
very obvious in ventricular fibers and caused by slow voltage gated calcium channels opening thus prolonging the depolarization