1. Respiratory system (week 1-3)
1/82
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
Nonfatal congenital anomalies of the nasal cavity and sinuses include?
congenital anomalies = abnormalities of organs/tissues present at birth.
Cystic nasal conchae, cysts of the maxillary sinus, deviations of the nasal septum, cleft upper lip (harelip, hypoplastic turbinates, choanal atresia, and cleft palate-palatoschisis)
What is nasal amyloidosis and its characteristics?
A rare metabolic disturbance reported in horses
can be primary, or secondary to chronic suppurative infections/tumors.
Nodular/diffuse involvement of nasal passages, can lead to obstruction.
Grossly: smooth, waxy, opaque surface
histologically: amyloid is deposited extracellular, esp. around vessels, + also in basement membranes + CT.
Name 3 circulatory disturbances of nasal cavity and sinuses
Congestion and hyperaemia
Relate to resp. function like warming of incoming air + also seen in the clinical sings + lesions of some disease.
Haemorrhage - within nasal region
causes: trauma, inflammatory or neoplastic breakdown of vessels.
May also occur as part of haemorrhagic diatheses (syst. clotting disorders).
In rhinitis, haemorrhage is linked to mucosal alteration, seen in acute inflammation + some chronic inflammations.
Epistaxis
Definition: bleeding from the nose
origin: sites other than the nasal mucus
common, serious in all species, esp. horse due to safety while racing.
large amounts of blood - linked with pulmonary haemorrhage, often fatal in eq + cattle.
numerous causes - local trauma, neoplasm + aneurysm. Any systemic problem with coagulation mechanism, incl. vitamin K deficiency.
Inflammation of of nasal cavity, what are the types of inflammation?
Rhinitis = of nasal passages
Sinusitis = inflammation of sinuses
These usually occur together, although mild sinusitis goes undetected.
Types of inflammation:
Catarrhal: serious process, include substantial outpouring of mucus.
Purulent/suppurative: severe inflammation, large number of neutrophils present.
Fibrinous: presence of fibrin, serious vascular damage.
Pseudomembranous/pseudodiphtheritic: when exudate lies on a mucosa that is not ulcerated to its full depth.
Haemorrhagic/ulcerative: bleeding/substantial ulcers present.
Granulomatous: chronic, mononuclear cells predominate, nodules/large masses can form, as in actinobacillosis/tuberculosis.
explain Bovine Rhinotracheitis (IBR), causes, histological changes.
Also known as "rednose," caused by bovine herpes virus (BHV1).
causative virus: bovine herpes virus (BHV1)
histological changes: small areas of cell death (focal necrosis)
In the early stages (up to 3rd day after infection): acidophilic intranuclear inclusion bodies are found in the epithelial cells. (special pink-coloured spots inside infected cells nuclei).
But these infected cells die + fall off quickly, thus when animals are examined after death (necropsy), these changes are often hard to find as the damaged cells are already gone (desquamated).
What are some effects of BHV1, the virus causing IBR?
Can cause abortion, generalized disease in calves, enteritis in calves, conjunctivitis, infertility, encephalitis, and skin lesions of the udder and vulva, inflammation + necrosis of ovaries.
What is atrophic rhinitis and its main significance in swine?
Common respiratory disease in pigs, in swine-producing areas.
Grossly: atrophy (shrinkage) of turbinates + other bones, irregular hypertrophy of some areas (secondary response)
often starts (acute stages) with sneezing, coughing, serous to mucopurulent nasal discharge
causes (not completely understood): probably toxins produced by Pasteurella multocida.
with help from: Bordetella bronchiseptica, haemophilus parasuis, + environmental/genetic factors may also play role.
Viral infections (like cytomegalovirus) may contribute too.
Why big deal in swine?
impact on pig`s growth + feed efficiency
Pigs with severe atrophy → crooked snout (deviate to the affected side + median septum distorted) + nasolacrimal duct obstruction→ eye discharge.
Atrophic lesions - caused by bacterial toxins causing defective functioning of osteoblasts.
Diagnosis: cutting + examining a cross-section of the snout bw. first + second premolar teeth to check turbinate size.
Microscope: thinning (hypoplasia) of nasal bones, damage + change in surface tissue (epithelium), inflammation + sometimes small abscesses.
Histologically: hypoplasia (thinning) of cancellous bone - key lesion
changes in tissue, damage to epithelium, cuboidal metaplasia
serous/mucopurulent exudate on conchae surface
hyperactivity of submucosal glands
chronic mononuclear cell infiltration of lamina propria
microabscessation (small abscesses)
Definition of Strangles, clinical signs
definition: infectious disease of horses, involving upper resp. tract + lymph nodes, but can also spread to other organs via blood (embolism) in severe cases. important in transit, crowding or other factors stressing horses.
Clinical signs:
Fever
cough
conjunctivitis (eye inflammation)
bilateral nasal discharge (progressively serous, catarrhal, then purulent)
swollen lymph nodes - esp. submandibular, retropharyngeal → become fluctuant, rupture, drain pus
hair loss + serum oozing over swollen lymph nodes before rupture
What are the gross pathological changes seen in Strangles?
Changes in the nasal passages:
nasal discharge - serous, catarrhal, purulent exudates
purulent material is abundant (copious amounts)
Ulceration of nasal mucosa
death is rare - but can become dangerous if bacteria enter blood and spread to organs (embolism) - liver, kidney, joints, brain or other lymph nodes.
Histologically, we see mainly abscessation.
what is Glanders? clinical signs?
Serious disease of horses (equids) by Pseudomonas (actinobacillus or Malleo-myces) mallei. Mainly affecting respiratory system, but can also involve skin (farcy).
Clinical signs:
Respiratory form (most common)
nasal discharge: catarrhal to purulent exudation
nodules (about 1cm) form inside nasal submucosa, then ulcerate, and leave stellate (star-shaped) scars.
Lungs: contain many pus-filled nodules (pyogranulomas) that can merge into diffuse pneumonia.
histologically: nodules in upper + lower resp. tracts = pyogranulomas with neutrophils + necrotic debris at the centres, surrounded by epithelioid cells, some giant cells, lymphocytes, fibrous tissues.
Cutaneous form (farcy):
seen on the abdomen + legs
causes swelling of lymph vessels with pus-filled inflammation (purulent superficial lymphangitis)
Leads to ulcerated nodules arranged in lines on ventral abdomen + legs.
What is acute rhinitis in dogs usually associated with?
Upper respiratory infection of dog.
Occur as part of general resp. disease caused by canine distemper virus, canine adenoviruses 1 + 2, canine parainfluenza virus, reovirus or herpesvirus.
is bacterial rhinitis common in dogs?
No, bacterial rhinitis is uncommon and usually occurs secondary to viral infections.
Bacteria that can be involved in sec. rhinitis:
Staphylococci, streptococci, E. Coli, Bordetella bronchiseptica, mycoplasmas (m. mycoides) + various anaerobes.
Myiasis means?
Infestation of tissues by the larvae of flies
Explain infestation + effects of the parasite “Oestrus ovis” in upper respiratory airways.
Oestrus ovis (nasal bot fly) - in nasal passages + sinuses of sheep. It is the most frequent cause of upper airway inflammation + obstruction in sheep. (can also infest humans + goats).
infestation: larvae deposited at the nostrils, undergo moults, and most drop to the ground. Some get trapped in turbinates or sinuses, causing irritation.
Clinical/pathological effects:
catarrhal to mucopurulent rhinitis
mucous erosion
hypertrophy of sinus mucosa
rarely, meningitis (from larvae penetrating cranial vault or bacteria entering via olfactory tracts)
Name other parasites that may infest upper respiratory tract (in addition to Oestrus ovis).
Linguatula serrata → parasites in carnivores
Capillaria aerophila → nasal parasite of carnivores
Leeches → affect herbivores and carnivores
Habronema spp. and Syngamus nasicola → infest ruminants
Nasal tumors (neoplasia), in which species are these most common?
Dogs - particularly long-nosed breeds, like collies, german shepherds. (but not all dolichocephalic breeds).
Cats (nasal vestibule) and horses (maxillary sinus).
What types of tumors (neoplasia) can occur in the nasal region?
Various histological types of tumours can come from any of the many cell types of the region.
sarcomas: fibrosarcoma, chondrosarcoma, osteosarcoma
Epithelial tumors (most common): papilloma, squamous cell carcinoma, adenoma, adenocarcinoma, undifferentiated carcinoma
in dogs, the adenocarcinoma + undifferentiated carcinomas are reported most often
cats + horses, squamous cell carcinoma is most reported
What are nasal polyps?
Non-cancerous (non-neoplastic) masses that look like tumors, usually a result of chronic inflammation.
most often seen in horse, cat, less common in sheep.
Grossly: firm nodules or masses of varying size, sometimes ulcerated, infected or bleeding (haemorrhagic)
Histologically: similar to fibromas, but well vascularized, with an inflamed core and covered by epithelium.
What are the common circulatory disturbances of the larynx and trachea, and in which animals are they often seen?
petechial hemorrhages (small pinpoint bleeding)
type of hemorrhage usually occurring in the larynx + trachea
seen as incidental findings at slaughter in cattle + pigs
Can be part of septicemias such as: hog cholera + porcine salmonellosis
“Turkey Egg Kidney” - porcine kidneys in hog cholera.
Hemorrhagic speckling of the tracheal mucosa in slaughtered cattle
produced by small extravasation in the submucosal lymphoid follicles
in cattle that die with severe dyspnoea (sometimes sheep), these follicular haemorrhages spread in a linear form.
In severe cases, the entire mucosa is red-black.
Why do the larynx and trachea frequently become inflamed?
Because of their location - they are often involved in inflammatory diseases of the upper + lower resp. tract - laryngitis + tracheitis.
Characterize Tracheitis.
Tracheitis - inflammation of trachea, often occurs along with bronchitis, and sometimes it is a part of pneumonia.
A chronic tracheitis can also develop after a tracheotomy
In such cases, the area near the wound becomes swollen and later stages show scarring.
In dogs and cats - foci of chronic polypoid tracheitis can occur.
can narrow the airway (stenosis), causing difficulty breathing (dyspnoea).
The exact cause is unknown, but the process likely resembles that which causes nasal polyps.
Squamous metaplasia - of tracheal epithelium can occur due to:
Vitamin A deficiency
Severe iodide toxicity
Characterize Laryngitis, occurrence, causes, signs.
Laryngitis - inflammation of larynx
Can occur alone, without involvement of whole resp. tract.
It can be a part of oral necrobacillosis caused by Fusobacterium necrophorum in calves + swine.
In slaughtered feedlot cattle, ulcers or scars of previous ulceration can be found on the larynx.
these are believed to result from repeated trauma during laryngeal closure (when larynx closes repeatedly during swallowing or coughing) → damages mucosa → ulceration.
Name parasitic diseases of the larynx and trachea.
Syngamus laryngeus - cattle, by worms
capillaria aerophila - dogs, cats, by worms
Filaroides osleri - dogs, by worms
Necrotic laryngitis - cattle, sheep, by F. necrophorum
Kennel cough - dogs, by bordetella, viruses
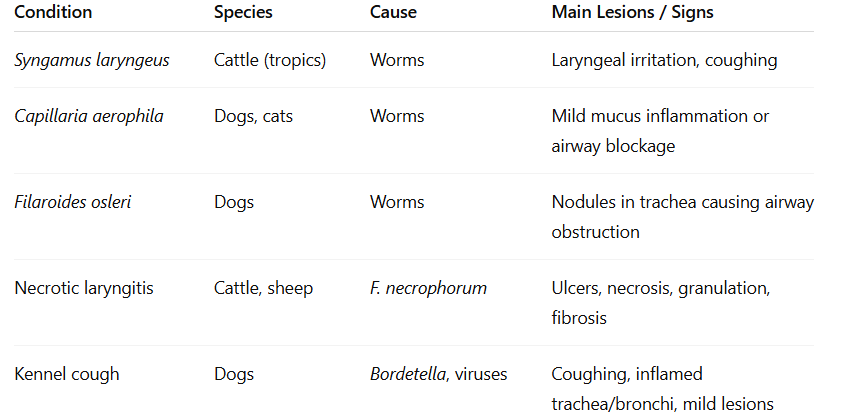
characterize syngamus laryngeus - parasitic disease
worm parasite found in larynx of cattle, mainly in tropical asia + south america.
characterize capillaria aerophila - parasitic disease
A small slender worm (2–3 cm) related to Trichuris.
Found in the trachea and bronchi of dogs and sometimes cats.
Mild infections: mild catarrhal (mucus) inflammation.
Heavy infections: more severe irritation, some obstruction to the lumen of the airways
characterize filaroides osleri - parasitic disease
A tiny worm (5–15 mm long) found in dogs and related species.
typical lesions: protruding submucosal nodules in the region of the tracheal bifurcation.
characterize necrotic laryngitis (calf diphtheria) - pathological changes, microscopy
A common disease of cattle, especially in feedlots, and also occurs in sheep.
often follows poor housing, nutritional deficiencies, intercurrent disease.
Caused by Fusobacterium necrophorum, a bacterium that also causes orolaryngeal necrobacillosis - can include lesions of tongue, gum, cheek, palate + pharynx.
produces several exotoxins + endotoxins - after getting into body by viral infections/traumatic injury.
Pathological changes/gross lesions:
Lesions consist of distinct, dry, yellow-grey, necrotic areas bounded by a zone of hyperaemia in the early stages.
with time, there is deep ulceration
if lesion is not fatal → heal by granulation
Under the microscope:
necrosis (large foci) + edges of hyperaemia (red, inflamed edges)
replaced by band of leukocytes → granulation tissue + fibrosis (scarring)
characterize canine infectious tracheobronchitis (kennel cough) - causes, lesions (pathological)
contagious respiratory disease in dogs - “kennel cough”
Similar to a “common cold” in humans — causes coughing but is usually mild.
The term “kennel cough” is used for any contagious cough in dogs - characteristics are paroxysmal coughing + canine distemper affecting lower resp. tract.
Causes:
Bordetella bronchiseptica (bacteria) + several viruses
Lesions:
May range from none at all to catarrhal or pus-filled (mucopurulent) inflammation of the trachea and bronchi. (tracheobronchitis)
Tonsils and lymph nodes may be enlarged.
Under the microscope:
Neutrophil-rich exudate (white blood cells and mucus)
Sometimes necrosis (death) of the tracheal lining (epithelium)
Types of neoplasia (tumors) of trachea, pharynx and larynx.
1. Oral Papillomatosis (Warts)
affects mouth of dogs + cattle
can extend to larynx.
2. Tumors from Tracheal Cartilage
The cartilage of the trachea can give rise to a tumor called a chondroma (benign tumor of cartilage cells).
3. Other Rare Tumors
Leiomyoma → tumor of smooth muscle
Adenoma → tumor of glandular tissue
Rhabdomyoma → tumor of skeletal (striated) muscle
These rarely grows.
Squamous cell carcinoma
Most common laryngeal + pharyngeal tumor
Other reported types:
melanoma
rhabdomyosarcoma
chondrosarcoma
osteosarcoma
Anomalies in the lungs
Congenital anomalies of lungs are rare.
accessory lungs are the most common + anomaly
can be located in thorax, abdomen or subcutaneous tissue virtually anywhere on trunk.
bronchial hypoplasia + dilatation can also occur as abnormal components of the lungs - various names including:
congenital cystic disease
congenital adenomatoid malformation
hamartoma
Number of other anomalies:
agenesis
hypoplasia
abnormal lobulation
pulmonary duplication
congenital bronchoectasis
What is atelectasis?
Atelectasis means the partial or complete collapse of lung or failure to extend - results in reduced/no air in the affected part of the lungs
Types and Causes:
Congenital Atelectasis:
Foetal atelectasis - fetus is stillborn + no respiratory efforts are made → no expansion of pulmonary tissue
Neonatal atelectasis: another form of congenital failure of pulmonary tissue to expand.
patchy in distribution, animal was able to breathe but unable to inflate enough parenchyma.
can be caused by airway obstruction with mucus/fluids at birth, anoxic damage during dystocia
special case: neonatal resp. distress syndrome/hyaline membrane disease.
Acquired Atelectasis:
Causes include:
Compression - simple presence of fluid, masses, pressure (ex. pneumothorax, hydrothorax, empyema)
Obstructive - blocked airway by exudate, foreign material, parasites or tumours.
congestive/shock lung - severe infection, trauma, blood loss
Hypostatic atelectasis - large animals at recumbency for longer times (ex. surgery)
Appearance:
The collapsed area is dark and collapsed. Can be flabby/firm (firm if there is concurrent edema/processes in shock lung).
Histologically: alveoli are collapsed/slit-like, supporting tissue becomes more visible/noticeable → stands out due to the air sacs are shrunken (changes occur even without inflammation).
what is Emphysema?
Emphysema is a condition of abnormal enlargement of airspaces of lungs, followed by destruction of alveolar walls. Most lesions occur only as components of disease conditions, where it can be related to obstruction of outflow of air/agony of slaughter.
Common finding in many lung diseases, but can also occur alone.
Occurs alone esp. in horses - chronic obstructive pulmonary disease + lesion in bovine atypical interstitial pneumonia.
Types:
Alveolar Emphysema
all species can get this condition, characterised by overdistention of the alveoli + rupture of alveolar walls.
Interstitial Emphysema
mainly in cattle
can be due to lack of collateral ventilation forces rupture of and migration into the interstitium (air escapes from alveoli → interstitial tissue - esp. under pleura → escaped air collects bw. tissue layers → air bubbles).
Appearance
The lungs appear pale, enlarged.
Alveolar form: air bubbles may be visible
if it is in interstitial empysema → bubbles of many sizes in CT bw. lobules. Large accumulations of air → bullae/bullous empysema.
all 3 types (alveolar, interstitial, and bulbous) may coexist.
Metabolic disturbances in lungs include? (2 stk)
Amyloidosis - inv. most body tissues + calcification can happen inside lung
Melanosis - black pigmentation in a lobular pattern, occassionally in ru. (black dust present in lungs.)
Name circulatory disturbances of lung
pulmonary ischaemia (lack of blood flow)
occur after emphysema or fibrosis - compress/thins the capillaries.
True ischaemia (total loss of blood) is rare due to the lungs having dual blood supply → both pulmonary arteries + bronchial arteries + many collateral (backup) vessels.
thus, congestion (too much blood) is more common than ischaemia.
Congestive cardiac failure
most common cause of generalised pulmonary congestion
often leads to pulmonary edema (fluid accumulation).
Hyperaemia + congestion
both reflected in color changes → red shade dependent on oxygenation state of blood + other components present (fibrin or edema).
histological lesions: any or all of these components, but mostly capillaries full of RBCs (engorged). RBCs may leak into alveoli and are eaten by macrophages → forming “heart failure cells”.
Haemorrhage (Bleeding in the lungs)
Causes: Severe heart failure, trauma, ruptured aneurysms, haemorrhagic diatheses by toxicity (warfarin).
vascular erosion in cattle - abscesses breaking into vessels causing haemorrhage into an airway, epistaxis - uncommon, but can cause
Exercise-induced haemorrhage in racehorses, defined as haemorrhage from dorsocaudal area of diaphragmatic lobe of lung.
signs: cough, excessive swallowing, resp. distress or decr. exercise tolerance can be seen. Often no clinical signs.
why? - unresolved, but can be due to mechanical stress on area of the biggest negative pressure.
Pulmonary edema (fluid in lungs)
causes: congestive cardiac failure, iatrogenic fluid overload, brain injury
can be part of any inflammatory process of lung or result from neoplastic obstruction of lymphatic drainage.
grossly: wet and heavy, variable color of lung. Color depends on amount of congestion/haemorrhage.
severe: can be impossible to distinguish from peracute pneumonia.
histological: difficult as fluid can be removed by fixation + processing.
Embolism and infarction
embolism: blockage of vessel (by clot, fat, bacteria etc.)
lungs rarely develop infarction (dead tissue due to blocked blood supply)
due to dual blood supply
infarction occur only if lung circulation is already damaged, like in chronic congestion.
Pulmonary infarcts: usually haemorrhagic, found mostly in caudal lobes, extend to pleura + affect sharp edges of the lungs.
explain Acute Bronchitis - inflammation of lung
Sudden inflammation of bronchi.
types of exudate (fluid/discharge in airways):
catarrhal
mucopurulent
fibrinous/fibrinopurulent
purulent (mostly pus)
change: epithelial necrosis - of bronchi
Progression: initial catarrhal phase - progression depends on nature of irritant + duration, severity of exposure.
Purulent/suppurative bronchitis: In common bacterial infections, bronchial exudate becomes yellowish + viscous.
Ulcerative bronchitis: in severe viral or bacterial infections, large epithelium areas are destroyed.
Intercurrent purulent bronchitis - often in bacterial infections
fibrinonecrotic bronchitis - in severe cases of infectious bovine rhinotracheitis + in mycotic bronchitis in cattle.
Severe necrotizing bronchitis - can occur in bronchiectasis or as a result of aspiration of foreign materials.
explain Chronic bronchitis - inflammation of lungs.
Long-term inflammation of bronchi.
Usually of bacterial, parasitic or allergic cause
in dogs: most important form is chronic catarrhal or mucopurulent bronchitis.
irritation + excess mucus causes a chronic cough, that is difficult to treat.
In cattle: chronic suppurative bronchitis often follows bronchopneumonia.
commonly linked with bronchiectasis (damaged, widened bronchi)
Bacteria such as actinomyces (corynebacterium) pyogenes + pasteurella species are most important - can be isolated from the suppurative lesions.
Definition of bronchiectasis.
Not a form of chronic bronchitis, but rather a complication/end-stage result of severe/repeated bronchitis.
Bronchiectasis = permanent dilatation of the bronchi and bronchioles with secondary infection.
it is the destruction of walls, foul luminal contents (as the walls are destroyed → pus, mucus, debris fills the lumen - bronchi) + atelectasis of parenchyma (collapse of lung tissue).
Name the two main anatomic varieties of bronchiectasis.
Saccular
thin-walled outpouchings of bronchial/bronchiolar walls (large, bag like cavities with pus/decay material).
can result from focal necrotizing bronchitis + bronchiolitis
in sheep + cattle
Cylindrical
bronchi are affected partially or along their entire length
In cattle - almost sequel to chronic suppurative bronchitis
Canine chronic bronchitis affects and does what?
Affects dogs of small/toy breeds that are obese and over 5 years old.
Causes - unclear but can be previous infections like kennel cough, air pollutants, allergy + genetics.
Grossly - viscous, mucoid-to-mucopurulent exudate in tracheobronchial lumen.
thickened mucosa, swollen with fluid (edematous), red + extra blood (hyperaemic), roughened, polypoid projections.
Histological: thickening can be due to mixed cellular infiltrations + hyperplasia of goblets cells + mucosal glands.
feline chronic bronchitis does what?
Similar clinical manifestation + pathology as for dogs, except that eosinophils are clearly seen in the walls and lumina of bronchi + sometimes bronchioles.
explain bronchiolitis, what is it?
inflammation of bronchioles (smaller airways).
bronchitis → can spread to be bronchiolitis.
It can occur at the same time as bronchitis + pneumonia. (bronchioles, bronchi and alveoli are all affected).
causes: viral infections, pulmonary toxicity (inhaling toxic gases for ex.)
Lesions + effects: mild inflammatory lesions in bronchioles → walls get thicker → difficulties in breathing.
bronchioles block easily due to their walls being easily collapsable + their small lumen size → thus, even a little mucus/pus (exudate) may block them completely. Meaning, that bronchiolitis often leads to airway obstruction.
severe bronchiolitis (exudate accumulation + epithelium does not heal) → exudate becomes organized into scars (fibrous tissue) → fills + block the bronchioles permanently → airway is obliterated (closed off).
Explain what means by “bronchiolitis Fibrosa Obliterans” (organizing bronchiolitis).
A non-specific response to severe damage to bronchioles + alveoli.
This can happen after:
Viral infections (influenza)
inhalation of toxic gases
lungworm infections
exposure to pneumotoxins - like the ones in acute interstitial pneumonia in cattle.
Chronic small airway diseases of horses (chronic bronchiolitis - emphysema complex)
In horses, long-term inflammation of small airways often occurs together with emphysema (overinflated alveoli) → “chronic bronchiolitis-emphysema complex”.
Seen worldwide in adult horses of any breed.
Causes: number of factors that can cause airway hyperactivity with similar signs + lesions (like dust, allergens, infections).
grossly: lungs often look normal, in severe cases they may be slightly overinflated. Emphysema can occur, but usually not obvious on gross examination.
Most important lesion: generalised. The disease affects the tiny bronchioles (those under 2-3mm wide), in which there is epithelial, goblet cell and lymphoid hyperplasia (all increase in number → airway narrows).
There can be peribronchial fibrosis (scar around bronchioles → stiff), neutrophils/eosinophils present.
Pneumonias is? and classified as?
Inflammation of the lung. Can be classified:
On a temporal basis as acute, subacute, chronic
on an aetiological basis by the major categories of causative agents
or accoridng to morphological features.
Pneumonias morphologically, there are which two approaches?
One approach is to classify according to type of inflammation. 2 subcategories:
Exudative pneumonias (acute) - in which the focus is on the filling of alveoli by exuate with a predominant by catarrhal, firbinous, suppurative, haemorrhagic, or necrotizing characteristic.
Proliferative pneumonia - focus is on proliferation.
Second approach is to classify according to the start site of involvement + pattern of spread of the lesion. On this basis, most pneumonias fall into 4 main categories:
bronchopneumonia
lobar pneumonia
interstitial pneumonia
focal pneumonia
Bronchopneumonia refers to? causes?
Refers to inflammation of the bronchi, bronchioles, and alveoli - that is bronchitis + bronchiolitis + exudation in alveoli. (combines them all).
Causes:
bacterial infection, but often follows a viral infection or stress that weakens the lung`s natural defenses. bacteria involved:
Pasteurella spp.
Actinobacillus pleuropneumoniae
Haemophilus spp.
Bordetella bronchiseptica
Salmonella choleraesuis
Bacteria → suppurative pneumonia.
Viruses, Mycoplasmas (Mycoplasma mycoides), and Chlamydiae can also cause it.
explain the gross appearance of bronchopneumonia
typical to look at:
The cranioventral (front and lower) parts of the lung
In animals with well-defined lobes (like cattle and pigs), the cranial and middle lobes are usually involved.
Gross appearance:
irregular consolidation (affected lung feels firm) - palpable firmness of tissue is most important criteria of pneumonia.
color: dark red, through grey pink to more grey, depending on age + nature of process.
Pattern:
Lung shows a patchy/mosaic pattern made of:
consolidated areas
atelectatic areas
congested areas
normal areas
how the pattern look like depends on how fast and severe the infection spreads + how lung lobes are divided (septation - the walls bw. lobules).
If the infection spreads quickly + evenly → whole lung area looks uniformly solid (homogenous consolidation). If slow → patchy appearance.
Cut open the affected lobe:
We can see many, evenly spaced, grey-white, raised spots (bulging foci) separated by narrow deep red zones.
The pale raised areas (bulging pale foci) = pus-filled bronchioles (exudation centres)
Red areas = nearby lung tissue that`s swollen, blood-filled or collapsed. (congested, edematous + atelectatic)
Pleura (outer surface of lung) - stays smooth in mild infection, while in severe infection, it becomes red, rough and coated with pus - yellow/grey exudate (pleuritis).
Inside of lung → wet, pus (reflects involv. of pleural surface).
in catarrhal/suppurative → consolidated lobules are moist when cut open.
mucopurulent/purulent material can be seen in small airways, fluid/foamy state in large airway.
histologically, what can we see in bronchopneumonia?
In bronchopneumonia, the inflammation starts around the small airways (bronchioles) and nearby air sacs (alveoli) — this is called the bronchoalveolar junction.
Early stage:
The bronchioles and nearby alveoli fill with neutrophils, mucus, cell debris, fibrin, and macrophages.
The lining of the bronchioles (epithelium) can become damaged (necrotic) or overgrow (hyperplastic) depending on the agent causing the infection.
The tissue around the bronchioles shows mild but acute inflammation.Surrounding alveoli (peripheral to severely inflamed bronchiolar regions):
These may be collapsed (atelectatic) or contain fluid (edema), fibrin, red blood cells, macrophages and white blood cells.
The blood vessels are engorged with blood → lungs get a reddish colour.Fluid in tissues:
Some edematous or serofibrinous fluid may be present in the tissue spaces, but this is not a major feature in early, mild bronchopneumonia.Healing:
In mild (catarrhal or purulent) bronchopneumonia, the infection can start to clear within 7–10 days, and the lungs return to normal in 3–4 weeks.
Macrophages take over later to clean up dead cells and fibrin once the infection is under control.
Severe bronchopneumonia can cause?
death - mostly due to lack of O2 in blood (hypoxemia) and blood poisoning (toxaemia).
If the disease does not cause death, it can lead to several complications, such as:
healing with scarrring, atelectasis (collapse of lung)
chronic bronchopneumonia
bronchiectasis
abscess formation or tissue death (necrosis)
If the disease is long-lasting - chronic bronchopneumonia, we see?
If the disease becomes chronic (long-lasting):
Lesions: The lung shows ongoing pus formation (suppuration) and fibrosis (scarring).
In ruminants (like cattle and sheep) and swine, the infection mainly affects the airways.
In cattle, bronchiectasis and abscesses are especially common.
The air sacs (alveoli) are collapsed (atelectatic) and scarred (fibrotic).
The exudate (inflammatory fluid) becomes organized into broad bands of moist fibrous tissue.
If the pleura (lung covering) is involved, the fibrin in the exudate can organize and cause pleural adhesions—that is, the lung surface sticks to the chest wall.
what does “Lobar pneumonia” refer to?
Lobar pneumonia means inflammation that affects a large part or an entire lobe(s) of the lung — not just small patches.
This pattern usually indicates the disease is acute (sudden) and severe, especially in ruminants and pigs.
Key Points:
Because it develops quickly, lobar pneumonia is often:
Hemorrhagic (with bleeding),
Fibrinous (with fibrin deposits),
Fibrino-purulent (fibrin + pus),
Or necrotizing and sometimes gangrenous (tissue death, usually from aspiration).
Most lobar pneumonias are fibrinous, so “lobar pneumonia” and “fibrinous pneumonia” are often used as the same term.
Characterize fibrinous pneumonia, location, effects.
Fibrinous pneumonia is actually a very acute and severe type of bronchopneumonia, common in certain animal species — sometimes treated as a separate form because of its distinct appearance and severity.
Lobar fibrinous pneumonia - in cranioventral parts of lung (front/lower)
fibrin exudate inside lung tissue (parenchyma) + on pleural surface (outer).
Lung changes color as the disease progresses - from reddish-black → deep red → reddish-brown → gray
How it develops?
The infection starts around the small airways (respiratory bronchioles) like in bronchopneumonia,
But it spreads very rapidly, so the normal lobular (patchy) pattern disappears, and the entire lobe becomes inflamed.
Explain the four phases - of changes in “Lobar fibrinous pneumonia”
Lobar pneumonia develops through four overlapping stages.
1. Stage of Congestion (First few hours):
hyperaemia (incr. blood flow) + inflammatory edema (fluid)
capillaries are distended with blood + alveoli filled with serous fluid
lobe: dark red, frim but still contains air
2. Stage of Red Hepatization (About 2 days):
affected area → consolidated/hepatized (solid) → resembling liver tissue in firmness.
completely hepatized lung tissue sinks in water.
Microscopically, congestion is still present, airless alveoli contains fibrinous, inflammatory exudate with phagocytosed organisms + RBCs.
3. Stage of Grey Hepatization:
lobe remains solid, dry, airless, has slightly incr. in size.
Exudate in still present in alveoli, but RBCs are lysed and alveolar walls are no longed congested. How much of each component of exudate varies with causative organism.
If pyogenic bacteria are the main invaders → exudate will be of mostly polymorphonuclear neutrophils. Lung architecture is preserved.
4. Stage of Resolution (Healing phase):
inflammatory exudate is digested, liquefied by lytic substances of WBCs.
Material is coughed up/drained away by veins + lymphatics.
Key point: no pus is formed at any stage of lobar pneumonia.
Although pneumonia mainfly affects the air sacs (alveoli) and their walls, it can also involve?
interlobular septa, CT, bronchi and pleura (lung covering) - it usually heals completely, but can cause complications sometimes.
What happens?
Interlobular septa + other CT structures → swollen + filled with fluid (serous exudate).
There is often bronchitis in the affected area - shown by:
loss of epithelial lining (desquamation)
inflammation with lymphocytes + other WBCs
exudate (mostly neutrophils), filling the bronchial lumen.
What is pleuropneumonia?
Occurs when the pleura (lung surface) is also inflamed and covered with a fibrinous or fibrino-purulent exudate. - if pleuritis is present.
what is the usual outcome of pneumonia?
with treatment, complete healing is common.
Possible complications can be:
Cardiac effects – right heart strain or rarely pericarditis/endocarditis.
Septicaemia – bacteria spread through blood, causing meningitis, arthritis, or abscesses.
Suppuration – empyema (pus in pleura) or lung abscesses.
Incomplete resolution – carnification
Explain what is incomplete resolution, carnification.
Sometimes, the healing process is delayed/incomplete → chronic changes in the lung. During incomplete resolution:
Alveolar cell changes - lining cells that are normally thin + flat → multiply (hyperplasia) → becomes thicker + cuboidal in shape
Persistent fibrin in alveoli - if the fibrinous exudate stays too long → body starts to organize it. Fibroblasts grow into the fibrin → turning area into fibrous tissue (scar). This process is called carnification (lung becomes solid and meaty).
similar process seen in pleuropneumonia.
fibrin layers on pleural surfaces are also invaded by fibroblasts. These layers become organized into fibrous tissue, sticking together. Results in adhesions (adhesive pleuritis).
Short:
in alveoli → carnification
In pleura → adhesive pleuritis
(by incomplete resolution, inflammatory material is not cleared away, but replaced with scar tissue):
What means by interstitial pneumonia? causes? pathogenesis?
Inflammatory condition mainly affecting alveolar walls with exudative, proliferative changes.
The term interstitial pneumonia is preferred as it incl. a wide range of causes and appearances. (but we also have “diffuse fibrosing alveolitis”).
Causes:
Many agents → acute, diffuse damage to alveolar walls → early intraalveolar exudative phase → proliferative + fibrotic changes.
Pathogenesis:
diffuse or patchy damage to alveolar walls
Unlike bronchopneumonia, lesions are not centered around/in airways. Instead, lesions are seen throughout the lungs.
Lungs → enlarged, rubbery, pale/mottled
may/may not have edema (fluid) or emphysema
Histological findings of interstitial pneumonia (microscopic changes we see).
Refleft camage to capillaries + epithelium
Early (acute) stage:
fibrin + edema fill alveoli, + debris and other materials (hyaline membranes) → line resp. surface of alveoli.
after 3 days:
Alveolar type II cell hyperplasia which cuboidal cells begin to replace damaged type-I pneumocytes
by 1-2 weeks:
differentiates into type-I cells
fibroblasts + collagen appear → fibrosis develops
infiltration by lymphocytes, macrophages + smooth muscle hyperplasia (incr. in number of cells)
chronic forms may become granulomatous
Examples of interstitial pneumonias are?
viral pneumonias:
bovine respiratory syncytial virus in cattle
maedi in sheep
influenza in horse
canine distemper in dogs
blood borne toxins.
Other relevant terms with focus on more chronic disease in pneumonia (except interstitial pneumonia) are?
chronic diffuse infiltrative lung disease
diffuse interstitial pulmonary fibrosis
What is focal pneumonia?
Localized inflammatory processes in the lungs that affect specific areas (foci) rather than being spread throughout (like interstitial pneumonia). (process in lung with focal (multifocal) distribution).
These include:
embolic pneumonias (variety of bacteria)
pulmonary abscessation - pus-filled cavities
granulomatous pneumonias - such as tuberculosis + systemic mycosis
metastatic neoplasms - cancer spread
some parasitic infections, like Mullerius in sheep + paragonimus in cats
Embolic pneumonia is? Causes?
Type of focal pneumonia.
Consist of single/multiple foci usually in form of abscesses.
Lesions are discrete, size varies, throughout any/all lobes.
Pathogenesis:
Emboli (particles/clots) coming from somewhere else in the body and gets trapped i lung capillaries.
These can develop into abscesses
May also result from:
other types of pneumonia
thoracic trauma
aspiration of foreign material
Embolic pneumonias - clinical signs?
Usually silent (no symptoms) unless:
large numbers of emboli arrive suddenly
lesions are widespread (→ respiratory failure)
abscesses/lesions erode blood vessels (→ severe bleeding/sudden death)
Granulomatous pneumonia (definition, causes)
Definition:
A chronic form of pneumonia characterized by granuloma formation — clusters of macrophages, lymphocytes, and sometimes giant cells — that form in response to persistent irritants (like bacteria, fungi, or foreign material) which the body cannot easily eliminate.
Causes/categories of causes:
Bacteria:
Actinobacillus, Actinomyces, Nocardia spp.
Often linked to local lung damage (trauma, aspiration of foreign bodies) or immunodeficiency (ex. dogs with distemper or arabian foals with combined immunodeficiency).
Major granulomatous infections:
Tuberculosis (Mycobacterium spp.)
Fungal infections (pneumonomycoses).
those caused by Inhaled or aspirated particles:
Dusts (e.g., silica in horses)
Feed particles or other foreign bodies → foreign-body granulomas.
Tuberculosis in cattle - example of Granulomatous pneumonia.
In cattle:
Lesions start at the bronchiolar–alveolar junction and spread into alveoli. It is initially sublobular/lobular.
Histological: tuberculous. Cloverleaf appearance, more than one lobule can be involved.
Early lesions: small, not yet encapsulated, surrounded by dense tissue.
Caseation (cheese-like necrosis) and calcification are typical features. (can be seen in early lesions too).
Multiple small foci may merge into large caseating areas - bronchopneumonia, sometimes forming small cavities (never large due to lung septa).
Spread: mostly through airways (bronchi) → causes caseous bronchopneumonia or lobar pneumonia (patterns).
In chronic stages, tubercles (nodules) may appear in the trachea and bronchi.
Tuberculosis in horse, sheep/goat, pigs, dogs/cats - example of granulomatous pneumonia.
In horses:
Lesions look different from those in cattle — uniform, “fat-like” (“lardaceous”) tubercles, resembling sarcoma rather than cheesy tubercles.
Spread is usually through blood (haematogenous) → can be miliary (tiny spots) or nodular.
Airway spread is not significant.
In sheep and goats:
Similar to cattle
In pigs:
Usually blood-borne (haematogenous) → miliary pattern (many small nodules).
Some infections with bovine bacillus → cause solid consolidation of cranial lobes.
In dogs and cats:
Lesions in dorsal caudal lobes — firm, pale, nodules (1–3 cm).
May mimic tumors (sarcomas) in appearance, making diagnosis tricky (especially in cats).
What is gangrenous pneumonia?
form of pneumonia → lung parts die and decay (gangrene). It is usually a complication of other pneumonias where lung tissue already has extensive necrosis.
Causes:
Aspiration of foreign material (common cause)
penetration of foreign body from reticulum into the lungs - in cattle
Infection with saprophytic, putrefactive bacteria (organisms that cause tissue decay).
Gross appearance:
Lung tissue becomes:
Yellowish to greenish-black in color.
Foul-smelling
Ragged cavities form rapidly
If the gangrenous area reaches the pleura (outer lung covering):
→ Causes foul-smelling pus in the pleural cavity (empyema).
→ May also lead to putrefactive pneumothorax (gas and foul odor in the chest cavity)
what is aspiration pneumonia?
Pneumonia caused by inhaling (aspirating) foreign material/liquids, entering lungs → inflammation. Often seen in young (calves), after vomiting or during anaesthesia.
How it differs:
Aspiration pneumonia = inhalation of foreign material (liquid or food) (non-respirable - too large to reach deepest airways).
Aerogenous pneumonia = infection from small particles (bacteria ex.) inhaled into the lungs (respirable).
Causes / Risk factors:
Feeding accidents: e.g., milk or milk-gruel aspiration in pail-fed calves.
Vomiting followed by inhalation, medications
During anesthesia
Gross appearance:
Lungs appear:
Inflated and reddish (hyperaemic).
Small airways may contain exudate (fluid and debris).
No specific or distinctive pattern.
Microscopic (histologic) changes:
Acute bronchiolitis (inflammation of small airways).
Acute alveolar inflammation — variable severity depending on material aspirated.
What is Uraemic Pneumonia?
Severe uraemia (high levels of urea + other waste in blood due to kidney failure) → increased permeability of alveolar air-blood barrier → cause of pulmonary edema.
usual form of uraemic pneumopathy occurs in dogs with chronic uraemia
Principal lesion (in addition to edema):
Degeneration and calcification mainly in:
Smooth muscle
Connective tissue fibres
occurs in walls of bronchioles + alveolar ducts in mild cases.
Severe cases:
Extensive mineralization (calcium deposits) in alveolar septa (walls between alveoli) → gritty, porous texture of the lung (grossly).
explain parasitic pneumonia - definition
Lung inflammation and damage caused by parasites migrating through or living in the lungs.
The lungs are a common site of migration for many parasites, so the type and severity of pneumonia depend on:
The species and number of parasites
The host’s immune response (especially hypersensitivity)
Ascaris suum - in lungs can?
May migrate in huge members and sometimes kill pigs (natural host)
Can also kill cattle (frequent unnatural host)
The trematodes Fasciola gigantica and F. hepatica can do what in lungs?
Invade the lungs accidentally from the liver.
Being large parasites, even a few can cause:
cavitations (hollow spaces) in lung
Parascaris equorum can do what in lungs?
Migrating larvae may cause small worm nodules in lungs.
Usually mild and not clinically important.
The dictyocaulus species (lungworms) may do what in lungs?
Most important cause of parasitic pneumonia.
Species:
D. filaria → sheep, goat, small ru
D. viviparus → cattle
D. arnfieldi → horse, donkey
Lesions produced:
larval migration stage (time reaching lung)
produce inflammatory reaction in alveoli, forming small grey nodules (2-4mm), or grey with greenish center.
adult worm stage (in bronchi)
cause chronic catarrhal and eosinophilic bronchitis/bronchiolitis (mucus and allergic-type inflammation)
Protostrongylus rufescens does what in lungs?
parasitic in sheep, goats, deer.
Adults inhabit the bronchioles.
Lesions are similar to those produced by dictyocaulus spp.
Muellerius capillaris, cystocaulus ocreatus, and metastrongylus lungworms do what in lungs?
M. capillaris - sheep, goat. Most common and widespread lungworm in small ru.
“nodular lungworm” - as adults live in the alveolar parenchyma, sometimes in bronchioles.
type of lesion:
almost always make an enveloping granulomatous reaction
nodules made, present lesions of multifocal interstitial pneumonia. These can be seen anywhere but most are under the pleura.
Cystocaulus ocreatus - stated to resemble Muellerius spp.
Metastrongylus - in bronchi, bronchioles of pigs.
Lesions: same as those of Dictyocaulus spp.
initial: larvae in alveoli → multiple foci of intense acculumations of eosinophils
reproduction is active: granulomatous alveolar response - triggered by eggs and larvae.
adults: chronic catarrhal and eosinophilic bronchiolitis + bronchitis.
Neoplasia in lungs - what primary/secondary tumors do we have?
Pulmonary Neoplasia - tumors that occur in lungs. Can be primary (from lung) or secondary (metastatic - coming from another site).
Primary Lung tumors
Origin: most often from epithelial cells (lining the airways/alveoli) than those of mesenchymal origin.
Rare in domestic animals, unlike humans where lung cancer is a major cause of death.
often single nodule, but can spread to other parts of lung/body.
Incl. Papilloma, adenoma, carcinoma, adenocarcinoma, haemangioma, haemangiosarcoma
dogs + cats most affected, most carcinomas
Secondary tumors
arise from tumors elsewhere in the body, spreading to lungs by blood
more common than primary tumors
Usually multiple. Nodules may vary in size.
Metastasis efficiency: despite many tumor cells entering the blood daily → only a few successfully form new tumors - metastasis is generally inefficient.
explain anomalies of the Pleura and thoracic cavity.
congenital (birth) defects are rare.
Examples:
mediastinal cysts (dogs)
can be large → decrease pulmonary function
Thoracic duct anomalies
can lead to chylothorax (accumulation of chyle/lymph fluid in the chest)
Degenerative disturbances of Pleura and thoracic cavity - name them
pleural mineralisation
Seen in renal failure → mineralisation of alveolar ducts + arterioles in addition to oral ulcers, gastritis
Uremia → horizontal, pale thickenings on pleura bw. ribs, reflecting the renal problem.
also seen in vitamin D toxicity - similar lesions
Pneumothorax
“presence of air in the thoracic cavity, stopping the normal negative pressure needed for lung inspiration”
diagnosis: in small animals, can be seen by opening the chest while animal is under water → air bubbles escaping
causes: trauma - accidental or surgical/iatrogenic, rupture of emphysematous bullae (air blisters in lung), rupture of parasitic cysts that connect with airways.
clinical signs: resp. distress, results in atelectatic lung (partial or complete lung collapse)
Name circulatory disturbances seen in Pleura and Thoracic cavity.
Hydrothorax
accumulation of serous (watery) fluid in thoracic cavity
effect → compresses lungs → respiratory distress
Causes: congestive heart failure, low protein (hypoproteinaemia), neoplasia (tumors), toxins/pancreatitis
chronic: causes pleural opacity from mesothelial cell proliferation and fibrosis
Haemothorax
Blood in the thoracic cavity
Causes: trauma, erosion of blood vessels by tumor/inflammation, clotting disorders, ruptured aneurysms
chronic: may develop vascular papillae (small projection) on pleura, rupture → fluid appear bloody
Chylothorax
accumulation of milk-like lymph in the thoracic cavity
causes: numerous, like neoplasia, trauma, congenital anomalies of thoracic duct, post-surgical injury
Name inflammation processes of Pleura and Thoracic cavity
Pleuritis (pleurisy)
inflammation of pleura, which may involve visceral pleura (covers lungs) or parietal pleura (lining chest wall)
The inflammation may or may not spread into the lungs.
Lesions may be:
fibrinous
purulent - if this in in cavity → lesion can be called pyothorax or empyema - pyogenic organisms
granulomatous
necrotizing
haemorrhagic
Caused by trauma, ruptured lung abscesses, extension from nearby infections (such as traumatic reticuloperitonitis in cattle)
effect/sequelae: fibrous adhesions bw. visceral + parietal pleura (pleural thickening). Restriction of lung expansion + contraction due to fibrous tissue, atelectasis (lung collapse)
Pleural Tuberculosis (“pearl disease)
can be nodular, caseous (thick plaques of caseous (cheese-like) mnaterial on pleural surface) or intermediate type
Effects:
affected pleura (visceral + parietal) → thickened by fibrous granulation tissue
underlying lung tissue usually not invaded
Nodular lesions, occurs in clusters usually
Later → heavy calcification
spread (generalisation) can occur early in the disease (post-primary) or late (late generalisation)
explain neoplasia of Pleura and thoracic cavity
Pleura (cover lungs) - often secondarily affected by tumors that spread from somewhere else.
Mesothelioma - primary tumor of the pleura
rare, most in calves - can be congenital
gross: multiple discrete nodules or arborescent (tree-like) growths spreading over pleural surface.
histologic: mesothelial covering cells or supporting tissues can dominate (can appear as carcinoma or fibrosarcoma).
considered malignant, but rarely spreads.
secondary tumors of pleura - uncommon
transpleural dissemination (direct extension through pleural surfaces) of carcinomas and sarcomas can occur - from lungs, chest wall, mediastinum.