cell recognition and immune system
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
types of pathogens
viruses, bacteria, fungi, protists, prions
antigens
a foreign protein that stimulates an immune response or the production of antibodies
proteins found on: pathogens, toxins including those produced by pathogens, abnormal body cells such as cancer cells, non-self material e.g. cells from another human
the effect of antigen variability on disease prevention
inhibits to control some infectious diseases
pathogen
an infectious agent that causes disease or illness in a host
utilise two mechanisms of disease: releases toxins and kills cells
self receptors/proteins
- proteins on your own cells
- have a specific tertiary structure
tissue rejection
- immune system recognises tissue as non-self
- it attempts to destroy the transplant
- to minimise tissue rejection:
→ donor tissues are matched closely with the recipient-proteins that are similar in tertiary structure - best matches come from genetically close relatives
→ immunosuppressant drugs administered to reduce the immune response
antibodies (immunoglobulins)
- a protein specific to an antigen, and is produced by B plasma cells
- Y shaped. quaternary structure cuz made up of 4 polypeptide chains (2 heavy, 2 light)
- variable and constant regions
- disulfide bonds → very strong → joins the polypeptide chains together
- every mammal is able to make millions of different antibodies, each with a different pair of binding sites specific for an antigen
- antigen binding sites → must have complementary shape to antigens they’re binding to
variable region: slightly different in structure compared to constant region → different sequence of amino acids → different tertiary structure
antigen-antibody complex
- antigens and antibodies are able to bind together
- the variable region on the antibody has a specific amino acid sequence
- the tertiary structure of the binding site is complementary to specific antigens
- this forms an antigen-antibody complex
antigen-antibody complexes lead to the pathogens being marked for attack by phagocytes or complement proteins
reasons for antigen-antibody complex
1. agglutination of cells - easier for phagocytes to locate
2. markers that stimulate phagocytes to engulf the bacterial cells
3. neutralised toxins
white blood cells
phagocytes (e.g. neutrophils, monocytes, macrophages, etc.)
lymphocytes (B & T)
non-specific response
physical and chemical barriers
phagocytosis
what are the two types of defence mechanisms?
non-specific
specific
physical barriers
skin
chemical barriers
- hydrochloric acid (found in stomach)
- mucus (found in airways)
- enzymes in your tears
phagocytosis
1. several receptors on phagocytes that recognise chemical products of pathogens or abnormal cells
2. phagocytes move along a concentration gradient
3. phagocyte engulfs pathogen forming phagosome
4. lysosomes fuse with phagosome containing antibodies. lysozyme enzymes hydrolyse the pathogen
5. the soluble products are absorbed into the cytoplasm
6. pathogens’ antigens presented on cell membrane (APC)
specific response
1. cell-mediated response → T lymphocytes
2. humoral response → B lymphocytes
T cells
mature in the thymus gland
cell mediated immunity
T cells recognise foreign material such as:
→ phagocytic antigen presenting cells (APCs)
→ body cells invaded by viruses presenting viral antigens
→ transplanted cells
→ cancer cells presenting antigens on their cell surface membrane
e.g. helper, cytotoxic, and memory
cell mediated immunity
immunity involving body cells only
cell-mediated response (T cells)
complementary helper T cells to antigen on a phagocyte
attachment activates T cell to divide rapidly by mitosis and form a clone of MANY genetically identical T cells
→ becomes a memory cell that circulates in the blood and tissue fluid in readiness to respond to a future infection by the same pathogen
→ this helper T cell stimulates a specific B cell
→ B cells divide by mitosis
→ stimulates phagocytosis by phagocytes
→ activates cytotoxic T cells to kill infected cells by making holes in their cell-surface membranes
cytotoxic T cells
kill abnormal cells and body cells infected by pathogens
produce perforin protein that creates pores in the cell-surface membrane
the cell is now permeable to all substances → cell dies because water leaves and therefore no metabolic reactions can take place
the action of T cells is most effective against viruses as they replicate inside host cells
B cells
mature in the bone marrow
humoral immunity (involves antibodies in the blood/tissue fluid)
many different B cells, each producing their own specific antibody that responds to and is complementary to a specific antigen
the humoral response
1. helper T cell binds to APC, activated helper T cell stimulates specific B cells to divide by mitosis
2. clones of identical B cells produced - clonal expansion
3. clones only produce the specific antibody for that particular foreign antigen
4. results in plasma and memory cells
5. endocytosis of antigen into B cell, presented on surface
6. T helper cell binds to processed antigen, stimulates B cells to divide by mitosis, clonal selection
7. each clone produces 1 specific antibody - monoclonal antibodies
B-plasma cells
produce and secrete identical and specific antibodies that are complementary to the antigen (monoclonal antibodies)
short lived
primary immune response
B-memory cells
circulate in the blood and tissue fluid to provide long-term immunity
do not produce antibodies, but can divide rapidly
involved in secondary immune response
monoclonal antibody
antibodies with the same tertiary structure, cloned from the same B plasma cell
- each antigen will induce a different B cell to divide by mitosis
- each of these clones produce one type of antibody (clonal selection)
- monoclonal antibodies have a number of useful functions
once antibodies bind to complementary antigens they:
are markers and attach to phagocytes
cause agglutination
neutralise any toxins released by pathogen
secondary response
memory cells circulate in the blood/tissue fluid, when they encounter the same antigen again, they divide rapidly to produce more memory and plasma cells
the many memory cells that have been created detect antigens quicker, and are stimulated
memory cells divide by mitosis to form more plasma and memory cells, even more antibodies
much stronger and quicker response, and can destroy the pathogen before it can cause any harm
primary immune response
the first time you are exposed to a new pathogen: phagocytes detect foreign antigens, ingest them, present them, activate T cells, which then activate B cells (plasma and memory)
after the pathogen has be defeated, plasma cells and antibodies die, they don’t remain in blood
antigen variability
some viruses have many strains (e.g. influenza)
antigens produced and presented on their surface are constantly changing
so when a new strain is encountered, a primary immune response occurs
passive immunity
when we don’t encounter the antigen, but get ready made antibodies for it
e.g. injected, cross the placenta from mother to baby, babies ingest antibodies from breast milk
limitation: no memory cells, so no long-lasting immunity
strength: immediate protection
active immunity
produced by stimulating the production of antibodies by the individuals’ own immune system
natural active immunity: become infected, body produced its own antibodies
artificial active immunity: vaccination/immunisation → an immune response is created, but no symptoms occur
strength: long-lasting immunity
limitation: takes time to develop immunity
vaccination
the introduction of disease antigens into the body (via injection or orally)
after first treatment, antibodies and memory cells against the antigen are made (primary response)
after second treatment, large numbers of B and memory cells are made (secondary immune response)
these memory cells can react rapidly, if the patient is infected again with that particular pathogen (with the same antigen)
vaccines are made harmless by:
- killing the pathogen, but leaving the antigens unaffected
- using bacterial toxins (antigens) to produce less harmful toxoids
- weakening the pathogen (attenuated), leaving antigens unaffected
- using genetically engineered eukaryotic cells to produce a microbial protein/antigen
successful vaccines
must be economically available to immunise most of the vulnerable population
few side-effects (this could discourage people from getting the vaccine)
low amount of doses
ability to produce, store and transport (requires hygienic conditions, refrigerated transport)
training staff to administer the vaccine properly
must be possible to vaccinate majority of the population to produce herd immunity
herd immunity
a large proportion of the population are vaccinated to prevent the spread of a pathogen
vaccination should be carried out at one time to achieve herd immunity - so for a certain period there are very few individuals with the disease and transmission of the pathogen is less likely
who cannot always be vaccinated?
babies / very young children
those who are ill or a have compromised immune system
diseases can be extremely difficult to eradicate (even with vaccines)
fails to induce immunity for those with defective immune systems
may develop the disease immediately after having the vaccine (haven’t had enough time to create antibodies and memory cells)
pathogen may mutate - antigenic variability
difficult to develop a vaccine for pathogens with multiple strains (e.g. cold virus)
pathogens conceal themselves from the immune system
individuals may object to vaccines (religion, ethical or medical reasons)
ethics of vaccines
vaccines save millions of lives, however:
involve the use of animals
side effects can cause long term harm
human immunodeficiency virus (HIV)
- can lead to AIDS
- is a retrovirus because it has RNA in it
- affects and invades T helper cells
- you can use antiretrovirals
structure of HIV
- lipid envelope
- attachment proteins
- capsid (protein layer)
- 2 RNA strands and enzymes
- reverse transcriptase enzyme catalyses the production of DNA from RNA
- retrovirus
transmission of HIV
- when the body fluids of a HIV positive individual mix with a HIV negative individual
- sexual intercourse (bodily fluids)
- blood transfusions
- intravenous drug users
- infected mother to baby via childbirth, breast milk or placenta
how to prevent transmission of HIV from mother to baby
caesarean
antiretroviral drugs are taken throughout pregnancy
antiretroviral drugs are given to babies for up to 4 weeks after birth
babies are bottle-fed with formula milk instead of breastfed
reverse transcription
to make amino acids viruses will want to go through protein synthesis
however, since they don’t contain DNA, viruses convert RNA back to DNA using the enzyme reverse transcriptase
the DNA is then inserted into T cells
HIV life cycle
HIV enters the bloodstream and circulates; virus enters the cell by endocytosis; HIV proteins bind to CD4 proteins found primarily on helper T cells; capsid fuses with the cell-surface membrane, RNA and enzymes enter; HIV reverse transcriptase (occurs outside nucleus): viral RNA → DNA; viral DNA inserted into helper T cell’s DNA, helper T cell undergoes transcription; HIV DNA is made into mRNA using the T cells enzymes; protein synthesis creates a new virus particle (RNA and viral proteins); new HIV particles leave the cell, taking some of the cell-surface membrane with it to form the lipid envelope; (replication of HIV often goes into dormancy, years later it can lead to AIDS)
virion
the complete ineffective form of a virus outside a host cell
how is HIV replicated?
attachment proteins attach to receptors on T helper cells
nucleic acid/RNA enters cell
reverse transcriptase converts RNA to DNA
viral protein produced
virus particles assembled and released from cell
how is HIV replicated once inside the T cell?
1. RNA converted into DNA using reverse transcriptase
2. DNA inserted into helper T cell DNA
3. DNA transcribed into HIV mRNA
4. HIV mRNA translated into new HIV proteins for assembly into viral particles
what is a vaccine?
a substance that contains antigens and stimulates production of antibodies
how do vaccines protect us against pathogens?
1. antigen binds to surface receptor on a specific T cell
2. T cell stimulates a specific B cell to divide by mitosis/produce clones (plasma and memory cells)
3. B plasma cells release antibodies
4. some B cells become memory cells
5. memory cells produce larger amount of plasma cells/antibodies faster when the antigen is encountered again
testing for HIV
enzyme-linked monoclonal antibodies to show a colour change which indicates the presence of the HIV antigen
why are antibiotics ineffective against HIV?
- antibiotics like penicillin inhibit enzyme required to form the murein cell walls on bacterial cells
- this weakens cell walls so they cannot withstand pressure (to prevent osmotic lysis)
- water enters via osmosis, causing the cell to burst and the bacterium dies
- viruses lack their own metabolic pathways as they use the host cell, so it’s difficult to target a pathway to distrupt
- viruses do not have a murein cell wall to target
- viruses are often found inside host cells, where antibiotics cannot reach them
- viruses also can have antigenic variability
what are the advantages of direct monoclonal antibody therapy over radiotherapy and chemotherapy?
direct treatment of cancer, less side effects
smaller doses
monoclonal antibodies can be used to treat symptoms in therapies or to test for and diagnose conditions - monoclonal antibodies and therapeutic drugs → direct monoclonal antibody therapy
- specific antigens on the surface of cancer cells
- complementary monoclonal antibodies can be given to a patient, antigen-antibody complexes formed
- growth factors bind to antigen on surface of cancer cells and sends signals to the cancer cell telling it to divide, this leads to uncontrollable division and tumours form
- monoclonal antibodies are made with complementary shape to binding site to block growth factor
- cancer cell can no longer replicate at an uncontrolled rate
indirect monoclonal antibody therapy
antibodies can be tagged with radioactive or cytotoxic drug
antigen-antibody complex formed
once bound, the drug will destroy the cancer cell
advantage: no need for chemotherapy which kills healthy cells as well as cancer cells
medical diagnosis e.g. prostate cancer
sufferers have high levels of Prostate Specific Antigen (PSA) in the blood
monoclonal antibodies can be used to obtain a measure of the level of PSA in a sample of blood
this can give an early indication of the possibility of prostate cancer
ELISA - e.g. HIV medical diagnosis
1. HIV antigen is attached to a plate
2. sample of patients blood added (if they have HIV, their blood will contain antibodies for this antigen). antibodies bind to antigens forming complexes
3. plate is washed to remove any unbound antibodies
4. an enzyme-labelled antibody is added that will bind to the antigen-antibody complex
5. plate is washed again to remove unbound labelled antibodies
6. colourless substrate added. enzyme hydrolyses substrate, which changes colour indicating a positive result
antibodies can detect pregnancy
antibodies are specific to bind with hCG with coloured markers are fixed onto a strip
the antibody-antigen complex will move along the strip, until trapped by another antibody
this creates the coloured lines to indicate pregnancy or no pregnancy
pregnant women produce high levels of the hormone human chorionic gondatropin (hCG) in their urine
why is the top row of immobilised antibodies necessary in a pregnancy test?
prevents a false negative result, and shows that the antibody has moved up the strip / hasn’t bound to hCG hormone
ethics of monoclonal antibodies
1. production of antibodies and cancer cells involves the use of mice that have been induced to produce tumours.
2. while they have been successful in the treatment of a lot of diseases, the use of monoclonal antibodies have been linked with the deaths of MS sufferers.
3. monoclonal antibodies are derived from mice
→ pros: mice are not killed, allows production of medicines, allows quick diagnosis + treatment because mice have quick immune response, mice are cheap to keep
→ cons: harmful to mice, might go against some religions or morals
lymphocyte apoptosis
- in the foetus, lymphocytes constantly collide with other cells
- the foetus is protected from the outside world by mother and placenta
- lymphocytes collide almost exclusively with the body’s self cells
- some lymphocyte have receptors that fit the body’s cells, these lymphocytes die or are suppressed
- the only remaining lymphocytes are those that would fit foreign material
- in adults lymphocytes initially only encounter self-antigens
- any lymphocytes showing an immune response to self-antigens undergo programmed cell death (apoptosis) before they can differentiate into mature lymphocytes
explain why the solution used to dilute the blood had to have the same water potential as the blood
to prevent too much water entering RBCs via osmosis, causing the cells to burst
to prevent to much water leaving RBCs via osmosis, causing them to shrivel up and die
ineffective vaccines
pathogens may have multiple strains (e.g. cold virus)
pathogens may mutate - antigenic variability
pathogens conceal themselves from the immune system (capsule)
may develop the disease immediately after having the vaccine (haven’t had enough time to create antibodies and memory cells)
AIDS
when HIV replicates, T cell numbers decline
helper T cells are destroyed leading to: no activation of cytotoxic T cells and B cells, and no antibodies
memory cells can become infected and destroyed
the body no longer responds to infections or cancerous cells
HIV does not directly cause death, but these secondary infections do
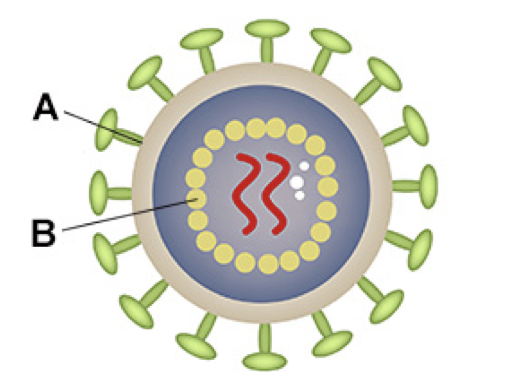
The diagram shows the structure of HIV. Name structures A and B.
A - attachment protein
B - capsid
give three types of cell, other than pathogens, that can stimulate an immune response
1. cells from other organisms
2. abnormal cells
3. cells infected by virus
Give one example of using monoclonal antibodies in a medical treatment.
blocks receptors on cells
Describe the role of antibodies in producing a positive result in an ELISA test.
1. first antibody binds to antigen
2. second antibody with enzyme attached is added
3. second antibody attaches to antigen
4. substrate added and colour changes
Describe and explain the role of antibodies in stimulating phagocytosis. Do not include details about the process of phagocytosis.
1. bind to antigen
2. antibodies cause agglutination
Describe how phagocytosis of a virus leads to presentation of its antigens.
1. phagosome fuses with lysosome
2. virus destroyed by lysozymes
3. antigens from virus are displayed on the cell membrane
what is an antibody?
a protein specific to an antigen produced by B cells
Describe the difference between active and passive immunity.
1. active involves memory cells, passive doesn’t
2. active involves production of antibody by memory cells
3. passive involves antibody introduced into body from outside
4. active long term, because antibody produced in response to antigen
5. passive short term, because antibody given is broken down
6. active can take time to develop, passive fast acting