Mechanical Ventilation (guest speaker)
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
What to consider
-what type of airway is in place:ETT, trach?
-what are the vent settings and what do they mean
-how do I respond to vent alarms
-worst case: what do I do if the vent fails
-what goes into tx planning for someone on a vent/someone who is being liberated from the vent
Why mechanical ventilation
-impending or existing resp failure
-failure to oxygenate: cell level
-failure to ventilate: mvmt air thru lungs
-combo
-airway protection: mostly risk of aspiration, agitated, stroke, anaphylaxis, opioid OD
Types of airways
-Endotracheal tube (ETT)
-oral (99% of time) and nasal (usually in facial trauma that limits ability to open mouth)
-most commonly oral, but can be nasal
-passes thru vocal cords
-cuff/balloon passes below the vocal cords: maintain pos pressure to keep airways open, increase SA of alveoli
-pts almost always restrained to avoid self-extubation
-tracheostomy: for long-term vent nds, blockage or narrowing of airway (tumor/blockage). paralysis (failure to ventilate)-usually C4 level(loss of diaphragm), prep for surgery, airway obstruction in field (cric)
-done to make mobility more comfortable
-CPAP:pos pressure to keep airways open
-BIPAP: more serious, used to avoid intubation, correct ABG imbalances
ECMO slide
-way to buy time for transplant
-take blood out to oxygenate
-cupula: over O2 to provide humidity
Tracheostomy
-can be cuffed or cuffless
-cuff if positive pressure is needed
-cuffless if pt is on "mist" or "high-flow"
-must be cuffless or cuff must be deflated to allow for speech
-more long-term airway mgmt
Vent settings
-Tidal volume (VT)
-PEEP: pressure left in lungs at end of expiration: PT contraindicated at over 15
-Mode: 2 big ones
-Rate: RR
-FiO2:fraction of inspired O2
Tidal volume (VTe)
-normal ~500mL for males, 400mL for females
-in some cases Vt needs to be decreased to protect lung tissue
-ARDS, conditions where lungs become scarred/fibrotic. Too much stretch will cause damage.
PEEP
-positive end expiratory pressure
-pressure given in expiratory phase to prevent closure of the alveoli, allows for increased surface area and increased time for O2 exchange
-for those who aren't responding to supplemental O2 via standard nasal cannula or high flow nasal cannula
-BiPAP used as last ditch effort before intubation
-will typically permit lower supplemental FiO2 needs due to increase surface area for exchange
-5 mmHg-20mmHg
-PT contraindicated at 15 mmHg or more (unless bigger pt because it may just be necessary)
FiO2
-percentage of oxygen in the air being provided to pt
-21% (room air)-100%
-prolonged exposure to O2 can be toxic and cause oxidation and alveolar collapse/atelectasis
-FiO2 >0.5 (50%)
-greater than 50% FiO2 over time can be toxic
-PEEP is a useful tool to limit O2 exposure while a pt is mechanically ventilated (baseline PEEP is 5 on vent, PT contraindicated around 15)
-high flow nasal cannula or vent can get FiO2 up to 100%
FiO2 boost on monitor
-100% O2 for 2 mins
-if they are low or
-during deep suctioning
Vent Modes: pressure control (PC)
-controlled ventilation (pressure control)
-vent initiates all breaths at a pre-set rate and TV
-will block any spontaneous breaths
-pts may be heavily sedated, even paralyzed
-volumes may vary depending on compliance of the lungs:important when trying to avoid barotrauma
Vent modes: assist control (A/C)
-vent allows a pt to initiate a breath, then vent will deliver a pre-set vol
-vent set at a min rate so that apnea doesn't occur when a breath isn't initiated
-potential probs
-hyperventilation--->respiratory alkalosis
-vent dysynchrony, breath-stacking (issue of barotrauma, can compress heart and decrease CO)
Vent modes: synchronized intermittent ventilation (SIMV)
-similar to A/C but w/o a set TV
-pt allowed to take their own breaths with their own TV
-vent will deliver a breath with a set volume if the pt doesn't initiate a breath (beware of pts "riding the vent")
-can lead to low RR if the set rate is low and the pt isn't initiating breaths
Vent modes: pressure support ventilation (PS or SPONT)
-pt initiates a breath, vent delivers pressure only to overcome airway resistance and keep airways open
-pt controls rate, TV (will likely be variable) and minute ventilation (liters of air/minute, Vt X RR)
Vent modes: continuous positive airway pressure (CPAP)
-with CPAP machine or used as a vent mode
-positive airway pressure provided during both inspiration and expiration
-can set a pressure and a flow of O2 (L/min)
-FiO2 variable depending on O2 flow
-improves gas exch and oxygenation in pts who can breathe on their own
non-invasive ventilation: BiPAP
-Bi-level airway pressure (BiPAP)
-delivered via mask (full-face, mouth and nose, nasal only)
-similar to CPAP but can be set at one pressure for inhalation and another for exhalation
-better for correcting blood gas imbalance than CPAP
-can be used to avoid intubation
Vent alarms: high pressure
resistance/increase to pressure getting in
-secretions:
-kinking/poor positioning of ETT
-Pt biting tube or fighting vent
-water in tubing
-decreased lung compliance (ARDS)
-coughing: if person can't cough it's alarming/dangerous
vent alarms: low pressure
losing pressure-->lungs not getting proper air
-tubing disconnect from vent
-pt side vs vent side
-cuff leak: holds pressure in lungs so it doesn't escape. If lost you'll lose PEEP
-extubation
-if ETT migrates too far superiorly, pt is functionally extubated w/o tube exiting mouth, can be difficult to troubleshoot
-this is why knowing your "mark at teeth" before mobilizing is important (tubes are marked in cm's so you can note where it's marked at the teeth)
vent alarms: low/high volume, low (apnea)/high rate, high/low PEEP
-volumes and rate are just what they sound like
-High PEEP or Auto-PEEP (breath-stacking)-sometimes use opioids to decrease respiratory drive
-excessive pos. pressure remains in alveoli at the end of exhalation and during the next inhalation, gradually increasing alveolar pressure
-increased WOB, can cause alveolar damage
-does this sound like another term we've talked abt?
-increasing expiratory time can help
-another way we increase expiratory time with our pts?
-Low PEEP
-cuff or ETT leak
How should you respond to vent alarms?
-look at the patient
-if they're not distressed they're probably fine
If it's real; disconnect pt, ambu bag pt with 100% FiO2 from wall
Tracheal/Deep suctioning
-for pts who are unable to clear secretions by cough or huff
-risks: exposure to infection, desaturation (FiO2 boost), --arrhythmia (vasovagal response)
-ICP (intracranial pressure): cough
-can be done with ETT or tracheostomy
Oral suctioning
-much less invasive
-an important part of maintaining good hygiene and decreasing risk of aspiration
-Yankauer
Complications of mechanical ventilation
-asynchrony (bucking the vent)
-autoPEEP: breath stacking
-barotrauma: alveolar damage due to excessive pressure/volume
-hemodynamic compromise: more due to being in bed (increase HR, inability of BP to adapt)
-nosocomial infection
-anxiety/stress/disruption of sleep/wake cycle
-deconditioning/vent dependence: SBT-sponatneous breathing trial (losing resp drive)
-Decreased CO
-high intra-thoracic pressure from positive pressure from vent-->compression of heart-->decreased EDV-->decreased preload-->decreased CO/Q
Which pts don't come off vent well and therefore we try to use BiPAP for?
-COVID
-CF
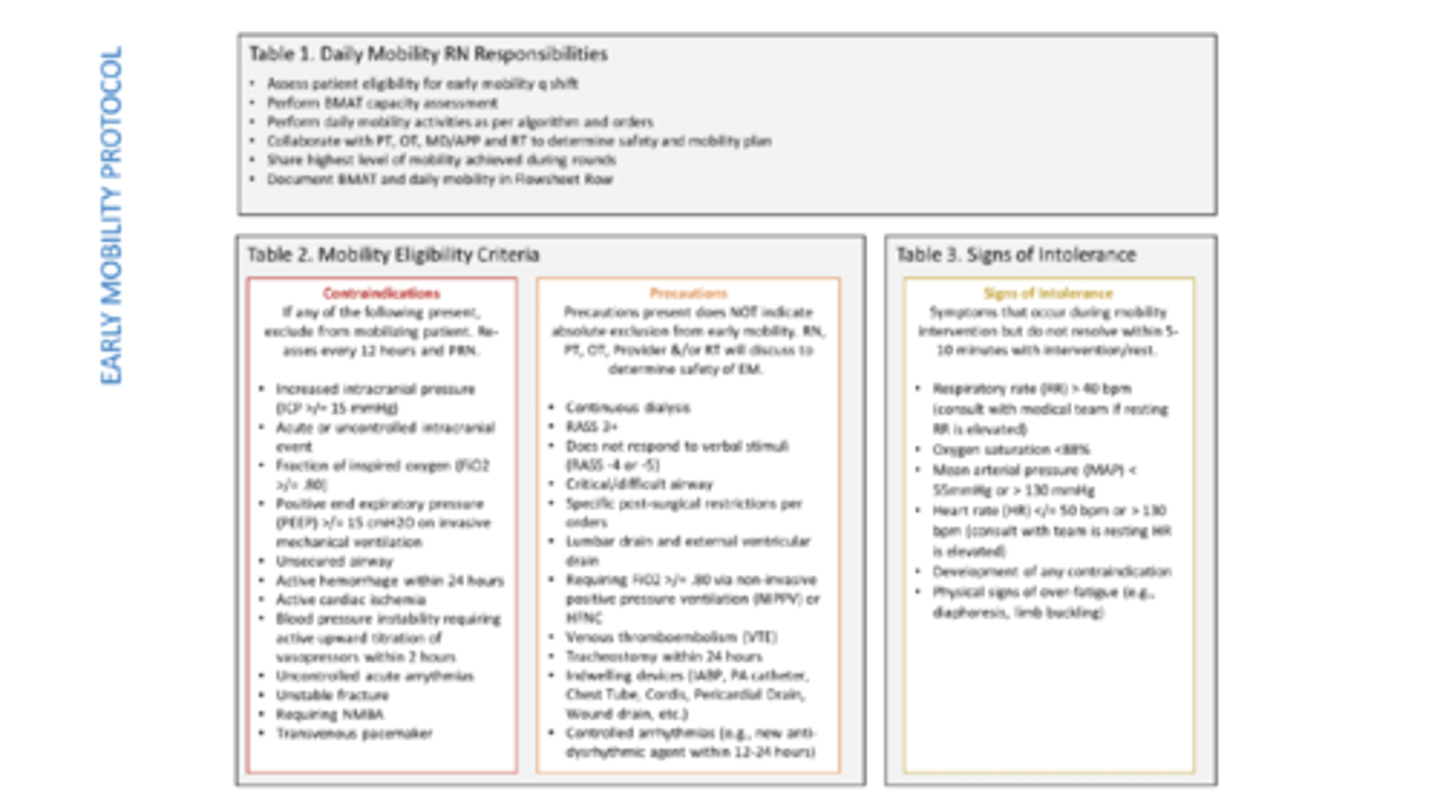
Contraindications, precautions, signs of intolerance
MAP
-important for peripheral vascularization
-usual goal of > 60
When is a cuff leak good?
-when you're about to extubate
-shows that the airway isn't occluded
Time to move
-located all tubes, lines, drains
-secure whatever can be secured to the pt
-consolidate other lines as able (wound vac on base of IV pole or hanging from walker)
-make a plan for lines