Disorders of Integument System
1/142
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
143 Terms
epidermal layers deep to superficial
stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, stratum corneum
keratinocytes
keratin
melanocytes
produce melanin
langerhan cells
present processed antigen to T cells
merkel cells
function as slowly adapting mechanoreceptors
fibroblasts
secrete collagen
mast cells
release histamine
macrophages
phagocytic immune cells; includes histiocytes in CT
blood supply in the skin
papillary capillaries
innervation of the skin
sympathetic nervous system regulates vasocontriction/vasodilation through a-adrenergic receptors
*regulated by arteriovenous anastomoses
pressure ulcer
result of unrelieved pressure on skin causing underlying tissue damage
how do pressure ulcers result
shearing forces, friction, moisture, occluded capillary blood flow resulting in ischemia and necrosis
decubitus ulcer
results when an individual lies or sits in one position for too long
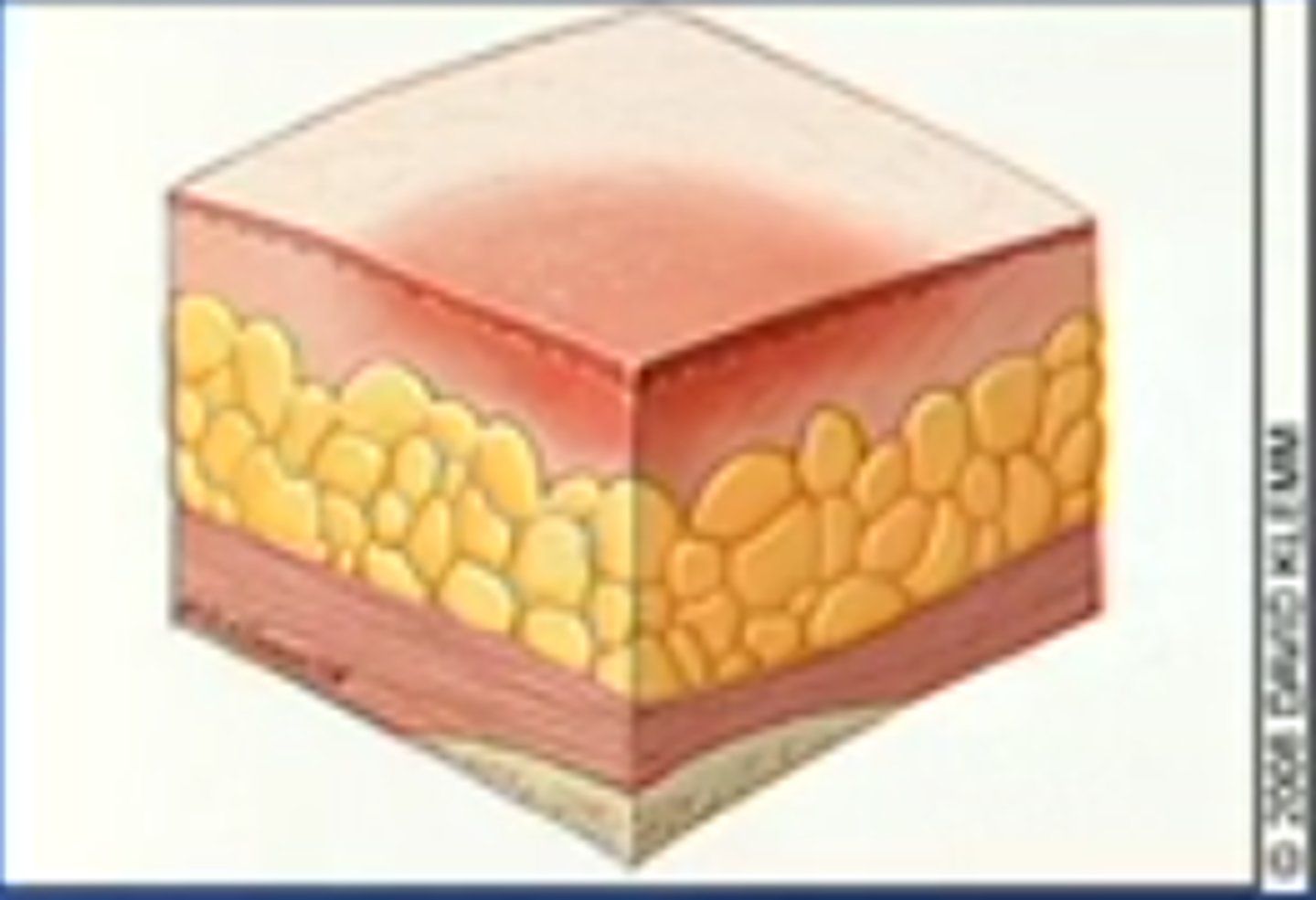
stage I pressure ulcer
nonblanchable erythema of intact skin
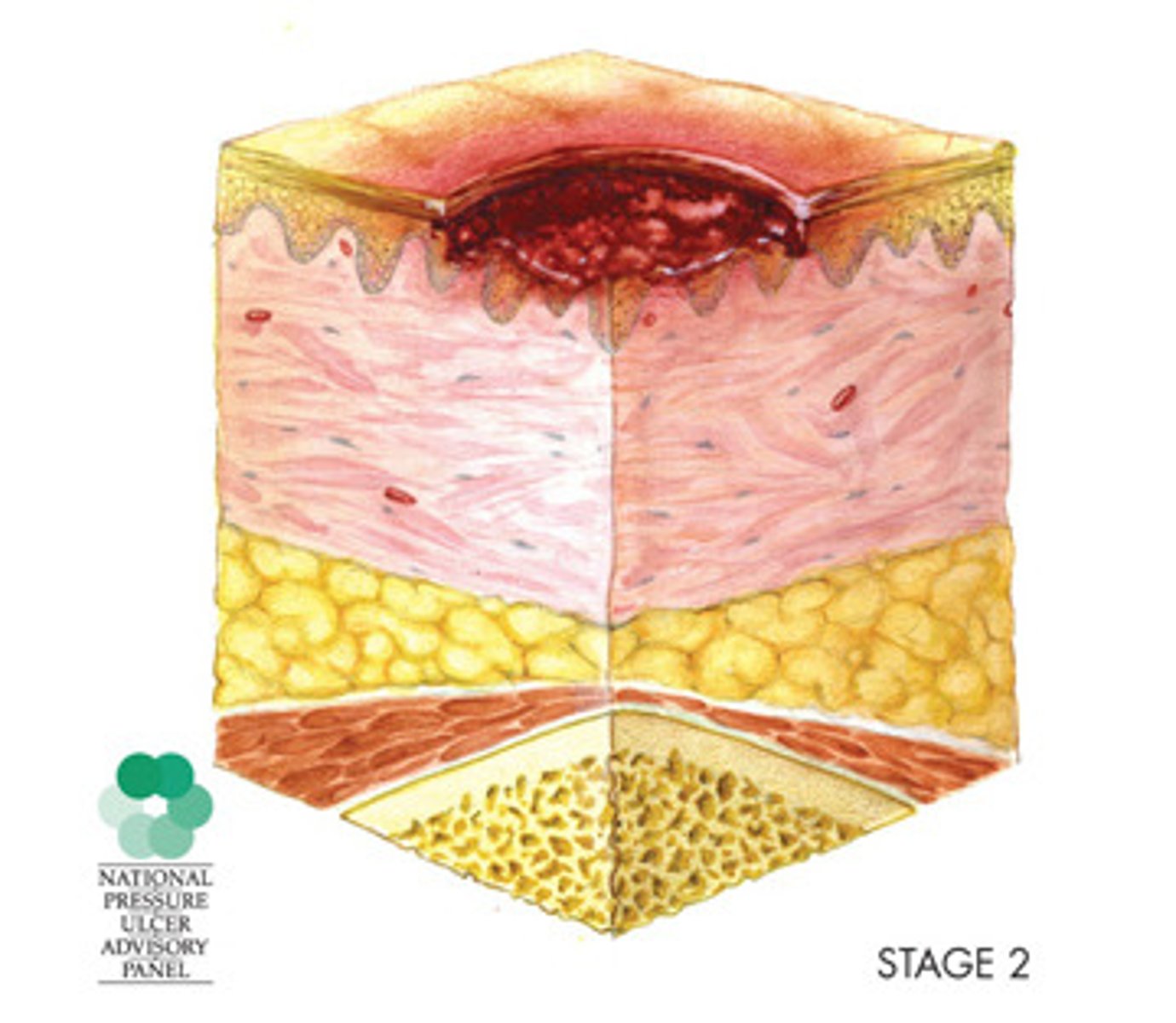
stage II pressure ulcer
partial-thickness skin loss, including epidermis or dermis
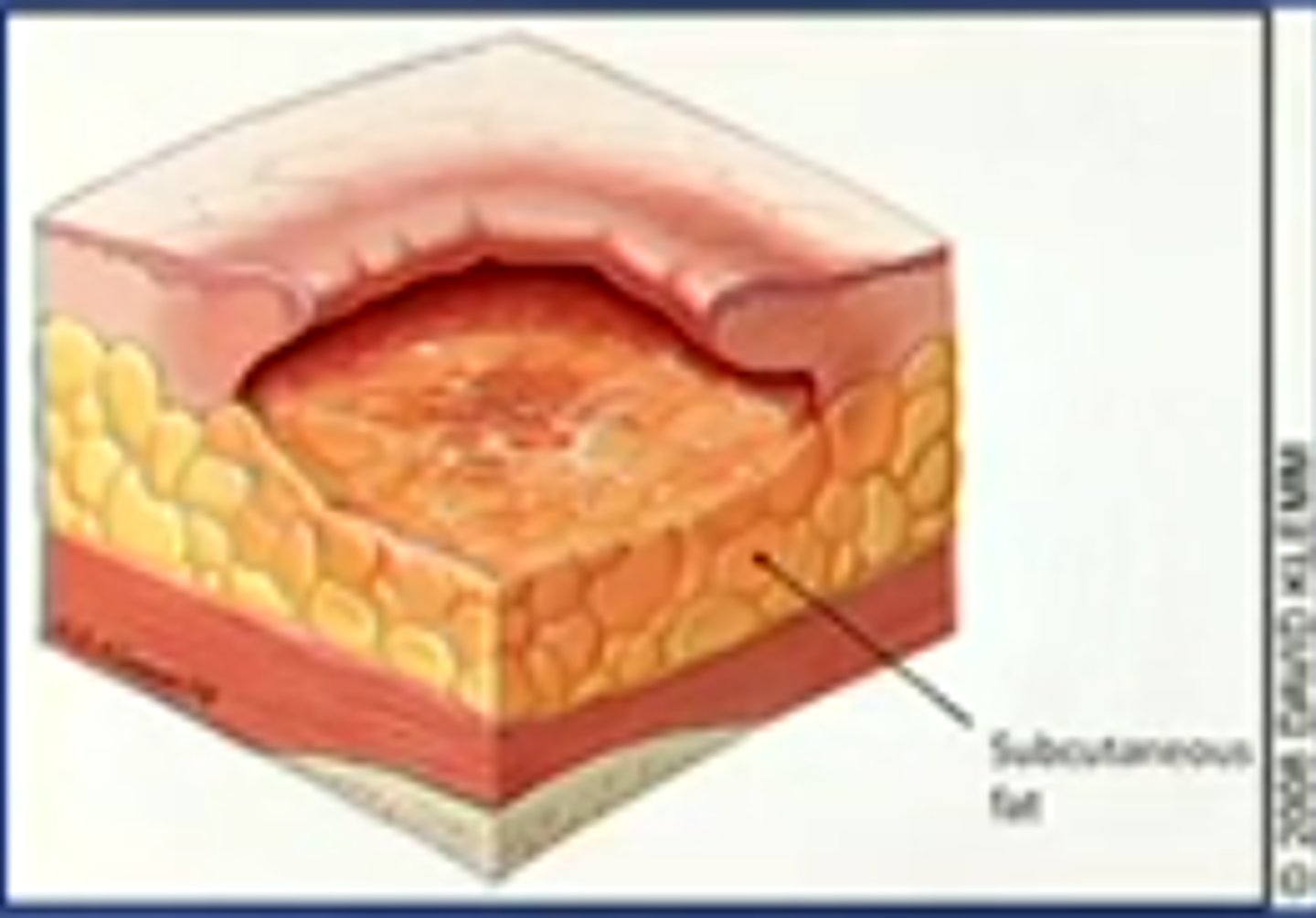
stage III pressure ulcer
full-thickness skin loss, involving damage or loss of subcutaneous tissue
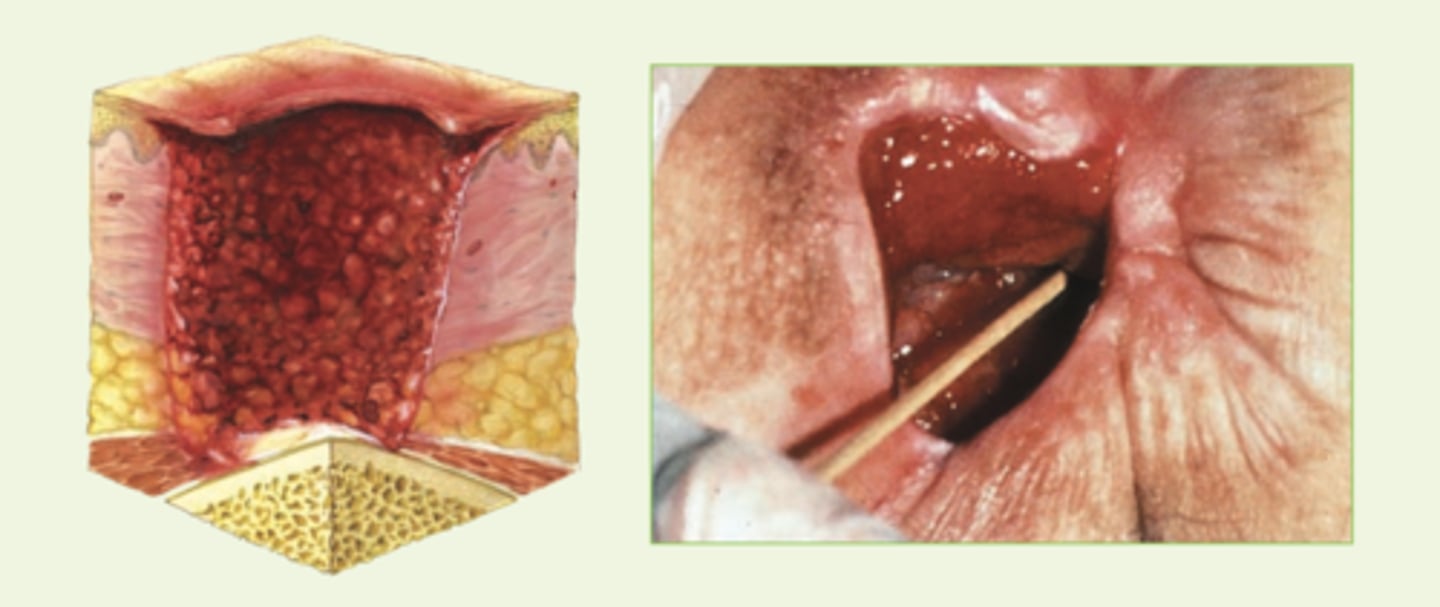
stage IV pressure ulcer
Full-thickness skin loss with damage to bone, muscle, or supporting structures
suspected deep-tissue injury
localized in an area of purple or maroon discolored intact skin or a blood-filled blister caused by underlying soft-tissue damage from pressure and/or shearing
unstageable pressure ulcer
full thicknes tissue loss with the base of the ulcer covered by slough or eschar, or both, in the wound bed
most common sites for pressure ulcers
sacrum, heels, ischia, greater trochanters
how to predict pressure ulcers
braden scale
What does the Braden Scale take into account when predicting risk for pressure sores? (6)
Sensory perception, moisture, activity, mobility, nutrition, friction & shear
keloid
excessive collagen formation/abnormal fibroblast activity; clawlike margins extend beyond original site
Where are keloids common?
darkly pigmented skin types and burns
hypertrophic scar
elevated erythematous fibrous lesions that do not expand beyond injury border
most common symptom of primary skin disorders
pruritus (itching)
what causes itch
specific unmyelinated C-nerve fibers
what can itch cause
scratching- can lead to to skin trauma, infection and scarring
what NS is itch modulated by
CNS
neuropathic itch
Related to any pathologic condition along an afferent pathway
psychogenic itch
Psychologic disorders
most common inflammatory disorders
dermatitis or eczema
what is dermatitis/eczema characterized by
pruritus, lesions with indistinct borders, and epidermal changes
chronic eczema
Thickened, leathery, and hyperpigmented skin from recurrent irritation and scratching
Allergic Contact Dermatitis (ACD)
common form of T-cell mediated or delayed hypersensitivity (type IV)
Cellular process of ACD
allergen comes into contact with skin --> binds to carrier protein to form sensitizing antigen --> langerhan cells process antigen --> carries to T cells --> become sensitized to antigen
clinical manifestations of ACD & ICD
erythema, swelling, pruritus, and vesicular lesions
Irritant Contact Dermatitis (ICD)
nonimmunologic inflammation of the skin caused by chemical irritation or prolonged exposure to irritating substances
atopic dermatitis
aka allergic dermatitis, common in childhood/infancy and can last into adult life
what is atopic derm associated with
fam hx of allergies, hay fever, elevated IgE, increased histamine sensitivity
stasis dermatitis
occurs in legs as a result of venous stasis, edema, and vascular trauma
sequence of events in stasis derm
edema, pruritus, scaling, petechiae, hyperpigmentation, ulcerations
seborrheic dermatitis
chronic skin inflammation involving the scalp, eyebrows, eyelids, nasolabial folds, axillae, chest and back; periods of remissions and exacerbations
what is a common term for seb derm in infants
cradle cap
clinical manifestations of seb derm
greasy, scaly, white, or yellowish plaques
psoriasis
chronic relapsing proliferative skin disorder
what percent of world population has psoriasis
1-8%
does psoriasis have family tendency
yes; complex genetic mechanisms including HLA
psoriasis is a _____ mediated skin disease
T-cell autoimmune
What type of T cells are associated with psoriasis?
helper t cells
What interleukins are associated with psoriasis?
IL-23, IL-17 loop
manifestations of psoriasis
Scaly, thick, silvery, and elevated lesions, usually on the scalp, elbows, or knees with remissions and exacerbations
what layers of the skin does psoriasis thicken
epidermis and dermis
epidermal turnover with psoriasis
3 to 4 days - cells do not have time to mature or keratinize
how is increase in cell metabolism accommodated for with psoriasis
capillary dilation and increased vascularization, causes erythema
plaque psoriasis
most common type (80-90%) and common on scalp, elbows, and knees as well as sites of trauma
early onset of plaque psoriasis patho
inflammatory lesion with epidermal hyperproliferation and presence of activated T lymphocytes
typical plaque psoriasis looks like
well-demarcated, thick, silvery, scaly, erythematous plaque surrounded by normal skin
inverse psoriasis
rare, involves lesions that develop in skinfolds
inverse psoriasis looks like
large, smooth, dry, and deep red
guttate psoriasis
develops after strep respiratory infection, more common in children, resolves in weeks to months
pustular psoriasis
blisters filled with noninfectious pus, develop over areas of plaque psoriasis
erythrodermic psoriasis
exfoliative dermatitis characterized by widespread red, scaling lesions that are itchy and painful
systemic complications of psoriasis
psoriatic arthritis, ankylosing spondylitis, psoriatic nail disease
Psoriasis is a risk factor for the development of:
IBD, metabolic syndrome (HTN insulin resistence, dyslipidemias, and abdominal obesity), atherosclerosis and CVD
pityriasis rosea
benign self-limiting inflammatory disorder usually occurring in spring and fall
what virus is pityriasis rosea associated with
HHV-6 and HHV-7
manifestations of pityriasis rosea
herald patch (circular, demarcated, salmon-pink)
lichen planus
benign autoinflammatory disorder of skin and mucous membranes
etiology of lichen planus
unknown
autoimmune nature of lichen planus
involves T cells, adhesion molecules, inflammatory cytokines and antigen-presenting cells
clinical manifestations of lichen planus
non-scaling papular violet-colored with pruritis on wrists, ankles, lower legs, and genitailia
acne vulgaris
Inflammatory disease of the pilosebaceous follicles
Pilosebaceous Follicle
the sebaceous glad continuous with a hair follicle
acne vulgaris causes hypertrophy of
sebaceous glands and telangiectasia
when is acne vulgaris most common?
adolescence
acne rosacea
skin inflammation associated with chronic inappropriate vasodilation resulting in flushing and sensitivity to the sun
acne rosacea typically presents in what age group?
middle-aged adults
4 lesions with acne rosacea
erythematotelangiectatic
papulopustular
phymatous (nose enlargement)
ocular
lupus erythematous
inflammatory autoimmune systemic disease with cutaneous manifestations
female:male lupus ratio
10:1
discoid lupus erythematous manifestations
restricted to the skin - photosensitivity, butterfly rash on nose/cheeks
can discoid lupus lead to systemic lupus
yes
patho of discoid lupus
altered immune response w/ development of self-reactive T and B cells
decreased regulatory T cells
increase proinflammatory cytokines
what causes tissue damage with discoid lupus
autoantibodies and immune complexes
Vesiculobullous Disorders
a group of diseases that have different causes and clinical courses but share the common characteristic of vesicle or blister formation
pemphigus
rare, autoimmune, chronic, blister-forming disease of skin and oral mucous membranes
manifestations of pemphigus
blisters in deep and superficial layers of epidermis
what causes pemphigus
circulating IgG autoantibodies --> directed against cell surface adhesion molecules in the epidermis
pemphigus vulgaris
acantholysis at suprabasal layer
patho of pemphigus vulgaris
IgG autoantibodies and C3 complement bind to desmoglein adhesion molecules --> destruction of cell-to-cell adhesion (acantholysis) in epidermis --> fluid accumulation causes blisters
manifestations of pemphigus vulgaris
oral lesions precede skin blisters, prominent on face, scalp, and axilla
pemphigus foliaceus
milder form, acantholysis at subcorneal level
manifestations of pemphigus foliaceus
blistering, erosions, scaling, crusting, and erythema usually on face and chest
NO ORAL INVOLVEMENT
most severe form of pemphigus
paraneoplastic pemphigus
paraneoplastic pemphigus
associated with lymphoproliferative neoplasms
affects internal organs leading to paraneoplastic autoimmine multiorgan syndrome
more benign than pemphigus vulgaris
bullous pemphigoid
bullous pemphigoid
autoimmune disease with bound IgG and IgE, blistering of subepidermal skin
what causes loss of dermal-epidermal adhesion in bullous pemphigoid
inflammatory cytokines
what distinguishes pemphigoid from pemphigus
subepidermal blistering and eosinophils