Overview of the Urinary System and Kidney Functions
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
105 Terms
What are the primary functions of the kidneys?
1. Regulate H2O balance (400 ml to 23 L per day) 2. Regulate electrolyte balance 3. Help maintain proper acid-base balance in the body 4. Eliminate the wastes of bodily metabolism 5. Excrete many foreign compounds (drugs, etc.) 6. Gluconeogenesis 7. Secretion of hormones such as Renin, Erythropoietin, and Vitamin D.
What organs are included in the urinary system?
1. Kidneys 2. Ureters 3. Urinary bladder 4. Urethra.
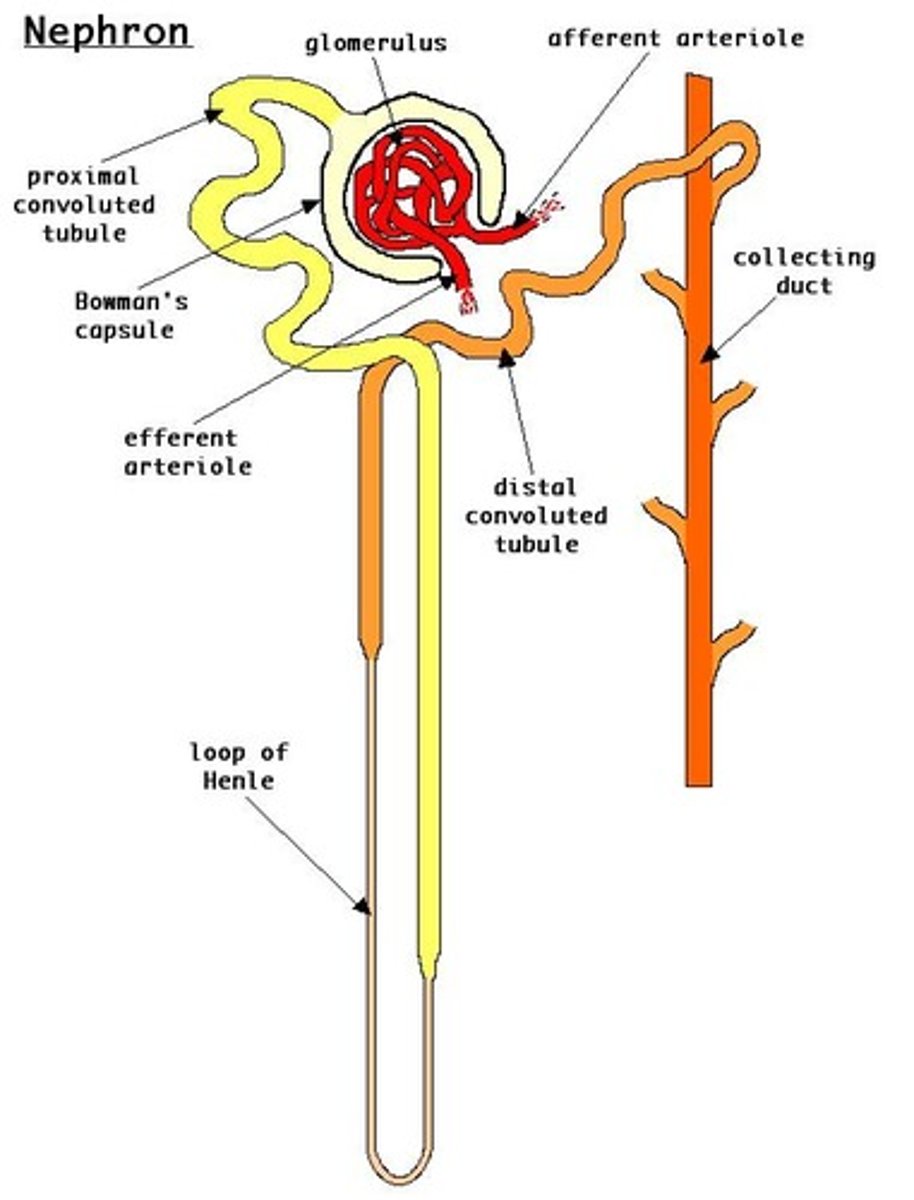
What is the nephron?
The nephron is the functional unit of the kidney and the smallest unit that can perform all kidney functions.
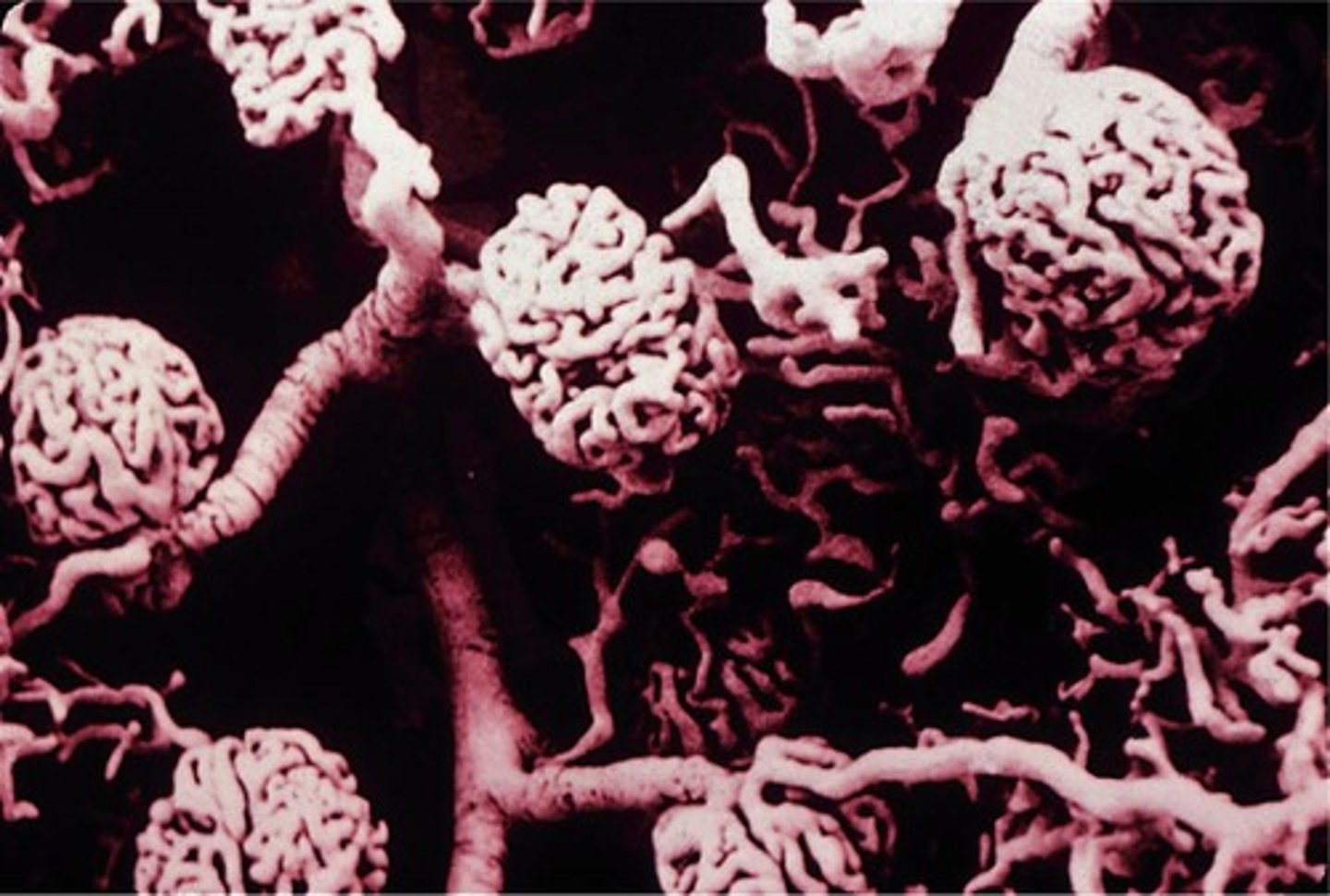
How many nephrons are there approximately in each kidney?
Approximately 1 million nephrons per kidney.
What are the two main components of a nephron?
1. Vascular component 2. Tubular component.
What are the two distinct regions of the kidney?
1. Medulla 2. Cortex.
What is the renal corpuscle?
The renal corpuscle is the initial filtering component of the nephron that forms filtrate similar to plasma but protein-free.
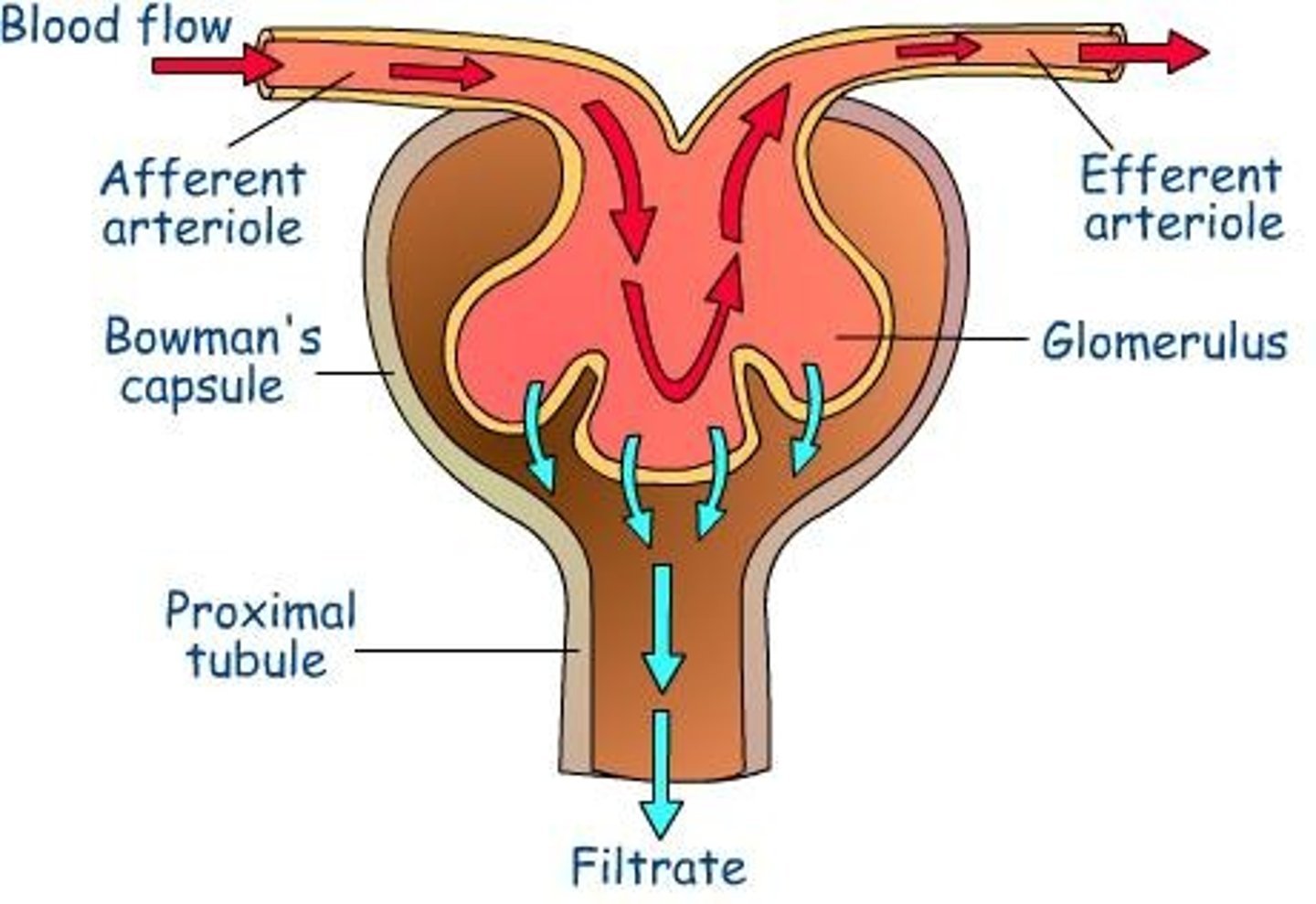
What are the four parts of the renal corpuscle?
1. Afferent arteriole 2. Glomerulus (capillary bed that filters blood) 3. Efferent arteriole 4. Bowman's capsule.
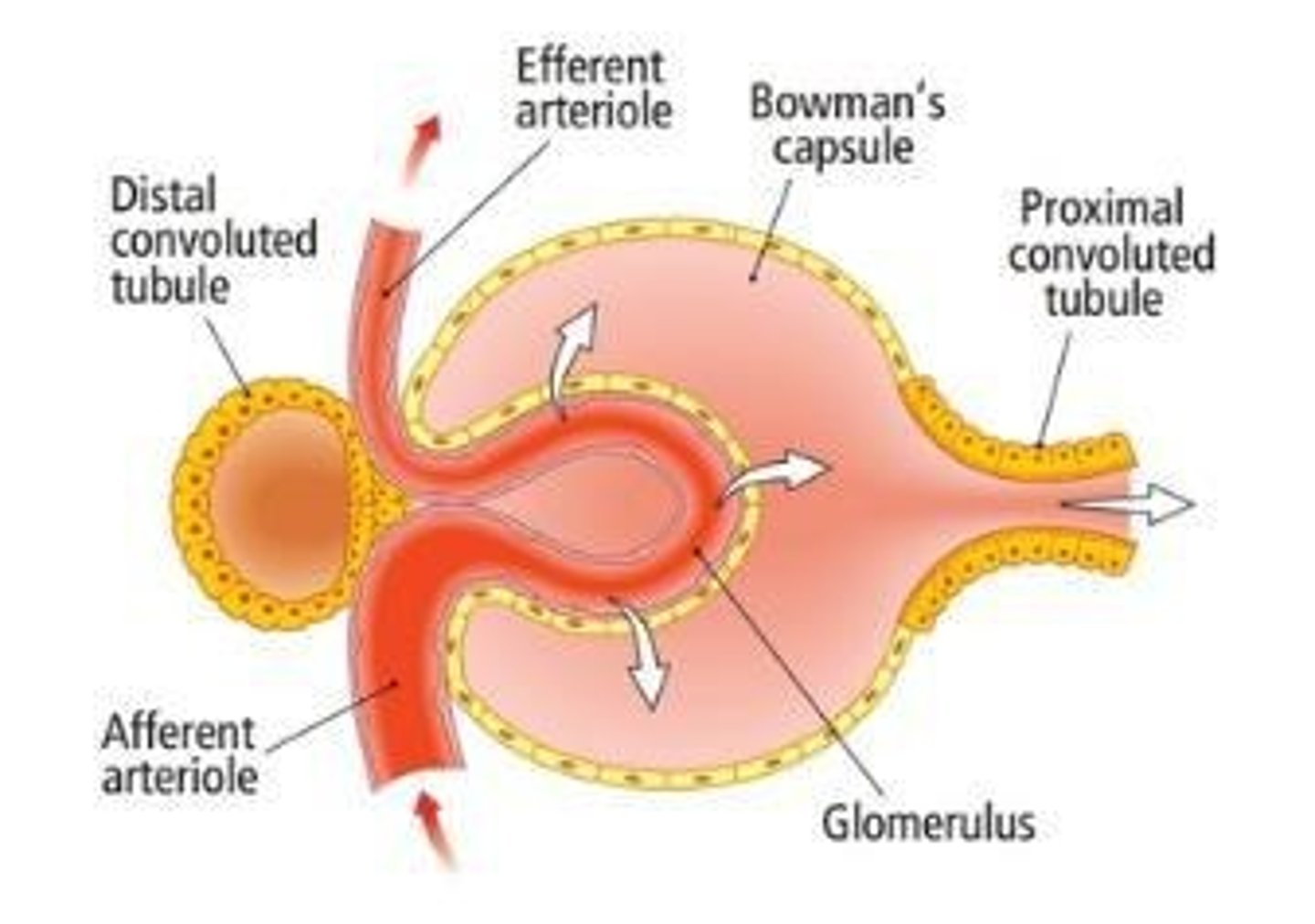
What is the function of the glomerulus?
The glomerulus is a capillary bed that filters blood.
What is the tubule in a nephron?
The tubule is a hollow, fluid-filled tube that extends from the renal corpuscle and adds or removes filtrate.
What are the components of the nephron tubule?
1. Bowman's capsule 2. Proximal tubule 3. Loop of Henle (descending limb and ascending limb) 4. Distal tubule 5. Collecting duct or tubule.
What is glomerular filtration?
Glomerular filtration is the formation of plasma filtrate.
What is tubular reabsorption?
Tubular reabsorption is the transport of substances out of the tubular lumen back into the blood.
What is tubular secretion?
Tubular secretion is the transport of substances into the tubular lumen from the blood.
What is the role of hormones secreted by the kidneys?
Hormones such as Renin, Erythropoietin, and Vitamin D play crucial roles in regulating blood pressure, red blood cell production, and calcium metabolism.
What is the significance of renal corpuscle filtration?
It initiates the process of urine formation by filtering blood to create a protein-free filtrate.
What is the role of the ureters in the urinary system?
Ureters carry urine from the kidneys to the urinary bladder for elimination.
What is the function of the urinary bladder?
The urinary bladder stores urine until it is excreted from the body.
What is the role of the urethra?
The urethra is the tube that carries urine from the bladder to the outside of the body.
What is gluconeogenesis in the context of kidney function?
Gluconeogenesis is the process by which the kidneys produce glucose from non-carbohydrate sources.
What is the formula for calculating the amount excreted in renal processes?
Amount Excreted = Amount filtered + Amount Secreted - Amount Reabsorbed.
What factors can change the rate of renal processes?
The rate can be changed based on size, charge, and shape of substances.
What are the three basic processes of glomerular filtration?
Filtration, Tubular Reabsorption, and Tubular Secretion.
What is the composition of the filtrate produced during glomerular filtration?
Filtrate is virtually the same as plasma but without proteins or cells.
What are the three layers of the filtration barrier in glomerular filtration?
Glomerular capillary endothelium, Basement membrane, and Podocytes.
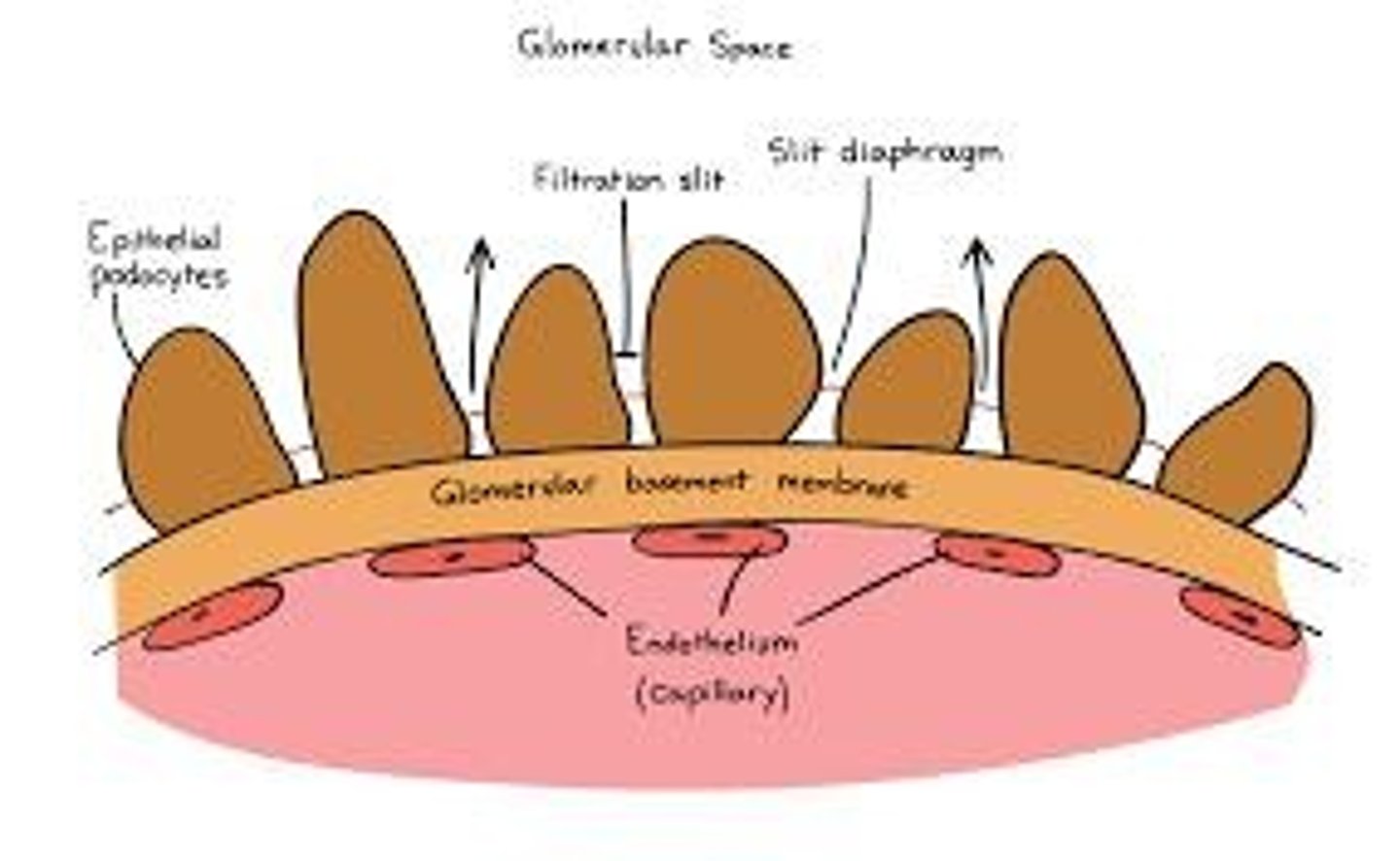
What is the role of podocytes in the glomerular filtration process?
Podocytes encircle the glomerulus and have slit diaphragms between foot processes that help in filtration.
What forces are involved in glomerular filtration?
Capillary hydrostatic pressure, Hydrostatic pressure in Bowman's space, Osmotic force of protein in capillary, and Osmotic force of Bowman's space.
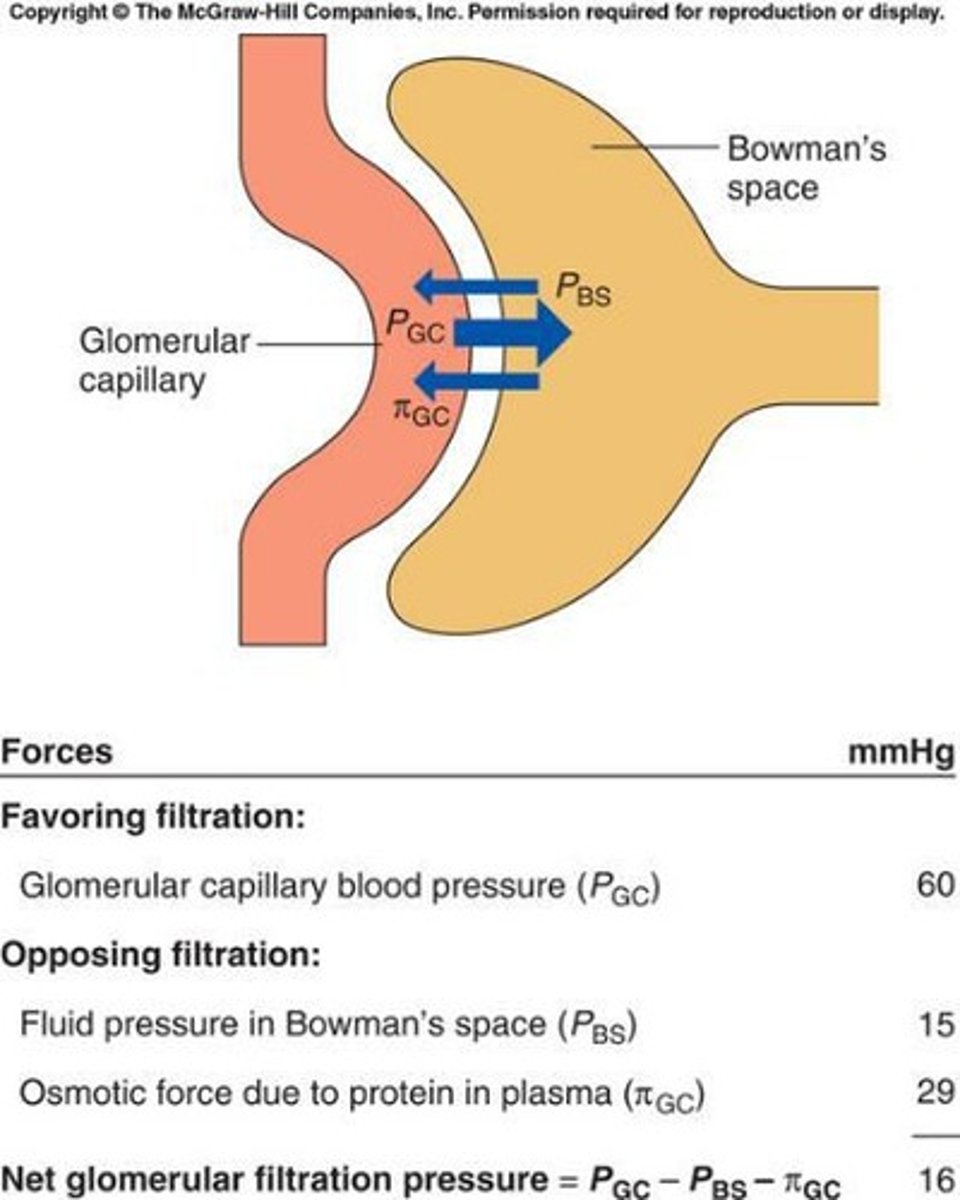
What is the Glomerular Filtration Rate (GFR)?
GFR is the volume of fluid filtered from glomeruli into Bowman's space per unit of time, typically 120 ml/min or 180 L/day.
What factors determine the Glomerular Filtration Rate (GFR)?
Net filtration pressure and permeability of membranes.
How is GFR physiologically regulated?
GFR is regulated by neural and hormonal input to afferent and efferent arterioles.
What is the significance of tubular reabsorption in renal processes?
Tubular reabsorption is highly selective and variable, allowing for the reabsorption of nutrients, ions, and water while minimizing waste.
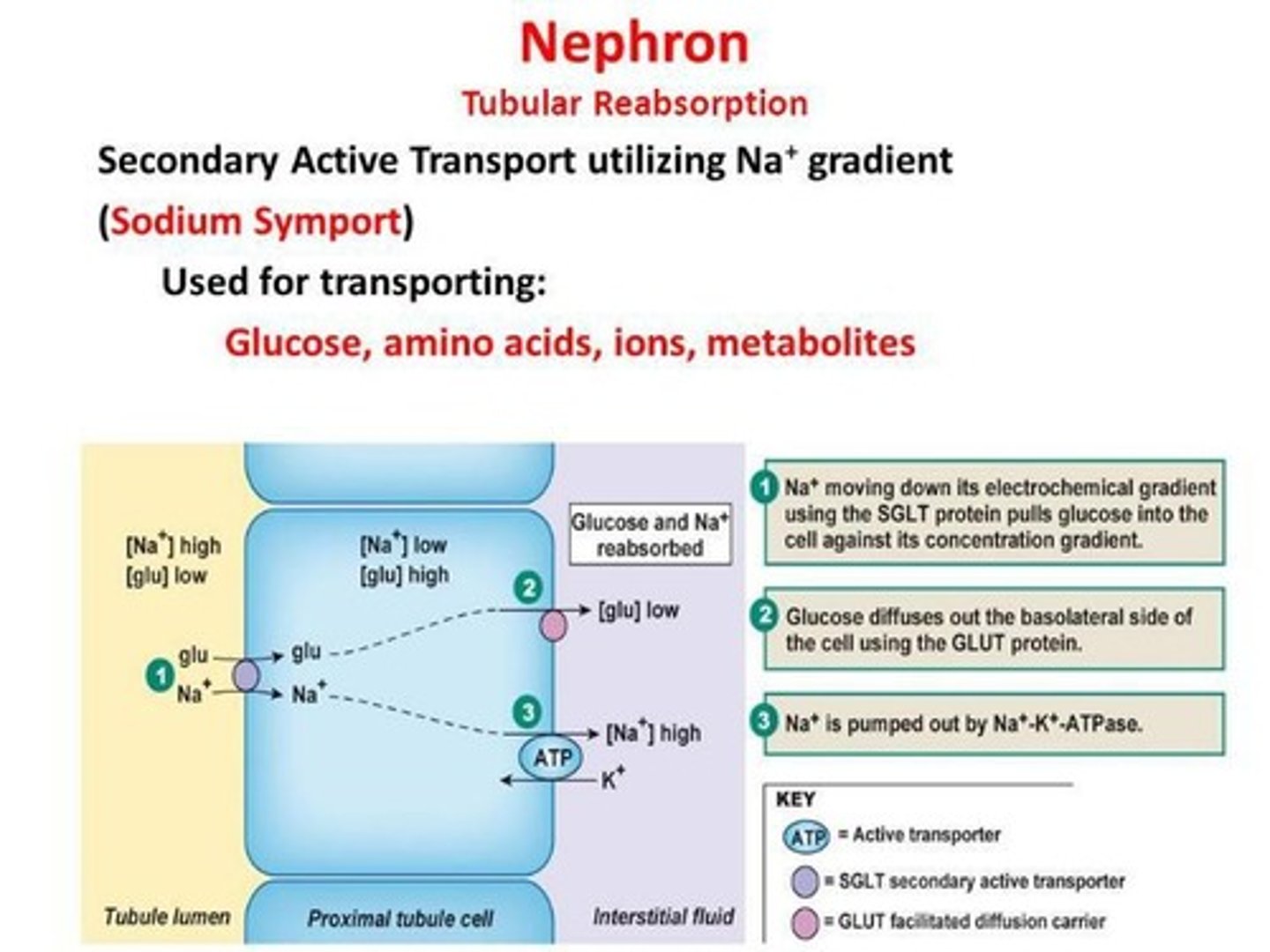
What types of transport are involved in tubular reabsorption?
Transepithelial transport, including diffusion and mediated transport.
How are glucose and amino acids reabsorbed in the kidneys?
They are reabsorbed by Na+-dependent, secondary active transport.
What limits the reabsorption of substances during tubular reabsorption?
Reabsorption is limited due to saturation of transporters (Tm).
What is tubular secretion and its basic processes?
Tubular secretion involves filtration, tubular reabsorption, and the addition of substances to the already filtered substances.
What are the main substances secreted by the kidney tubules?
H+ (for acid-base balance) and K+ (to maintain appropriate plasma K+ concentration).
What is the primary function of the kidneys in relation to organic ions?
The kidneys eliminate foreign organic compounds from the body, such as antibiotics.
What is renal clearance?
Renal clearance refers to the kidneys' ability to remove excess ions and wastes from the blood, effectively 'clearing' a substance from the bloodstream.
If the clearance of urea is 65 ml/min, what does this indicate?
It indicates that the kidney removes all of the urea in 65 ml of plasma in one minute.
What are the three processes by which substances are cleared from the blood by the kidneys?
Filtration, secretion, and reabsorption.
What does a clearance equal to GFR imply?
It implies that the substance is filtered and not reabsorbed or secreted.
What happens to a substance that is filtered and completely reabsorbed, such as glucose?
None of the filtered plasma is cleared of the substance.
What occurs for a substance that is filtered and secreted but not reabsorbed, such as hydrogen ions?
All of the filtered plasma is cleared of the substance, and the peritubular plasma from which the substance is secreted is also cleared.
What is the total body balance of water based on?
It is based on the inputs (water intake, food, liquids, metabolism) and outputs (sweat, urine, feces, insensible loss).
How does the body maintain sodium balance?
The body gains Na+ through ingestion and loses it via skin, GI, and urine, with urinary loss being the major control point.
What percentage of Na+ and water is reabsorbed in the kidneys?
99% of Na+ and water is reabsorbed, with no secretion occurring.
What is the primary mechanism for sodium reabsorption in the kidneys?
The Na, K-ATPase pump in the basolateral membrane of tubular epithelium.
How is renal sodium regulation achieved?
By calculating Na+ excretion as Na+ filtered minus Na+ reabsorbed.
What role do cardiovascular baroreceptors play in sodium regulation?
They detect changes in total body volume and help regulate sodium reabsorption.
What happens when Na+ levels are low due to diarrhea?
There is a decrease in plasma volume and blood pressure, leading to decreased firing of baroreceptors and increased sympathetic nervous system activity.
What is the Renin-Angiotensin-Aldosterone System (RAAS)?
RAAS is a regulatory system that stimulates Na+ reabsorption, K+ secretion, and controls aldosterone secretion.
What triggers the release of renin from juxtaglomerular cells?
Renin is released in response to sympathetic nervous system activity, intrarenal baroreceptor activation, or low Na+ levels.
What is the effect of RAAS on the collecting duct?
RAAS stimulates Na+ reabsorption and K+ secretion in the collecting duct.
What is the relationship between GFR and Na+ excretion?
Na+ excretion is equal to Na+ filtered minus Na+ reabsorbed, with GFR being relatively constant.
What happens to sodium excretion when blood pressure decreases?
Sodium excretion decreases as the kidneys adjust to retain more sodium.
What is the significance of the peritubular capillary in renal function?
It plays a crucial role in the secretion and reabsorption processes during renal clearance.
What is the primary active process for sodium reabsorption in the kidneys?
The reabsorption of sodium primarily involves active transport mechanisms.
What is the consequence of a substance being filtered but not secreted or reabsorbed?
The filtered plasma is completely cleared of that substance.
What is the formula for water excretion in the kidneys?
H2O excretion = H2O filtered - H2O reabsorbed.
What is the primary function of the kidneys regarding water?
The kidneys cannot replenish lost water; they can only conserve it.
What hormone is primarily responsible for water regulation in the kidneys?
ADH (Antidiuretic Hormone).
What stimulates the secretion of ADH?
A reduction in plasma volume detected by baroreceptors and an increase in osmolarity detected by osmoreceptors.
How do baroreceptors influence ADH secretion?
A decrease in plasma volume leads to decreased firing of baroreceptors, which increases ADH secretion.
What role do osmoreceptors play in ADH secretion?
Osmoreceptors in the hypothalamus increase ADH secretion in response to increased osmolarity.
What effect does ADH have on the collecting ducts in the kidneys?
ADH acts to insert aquaporins into the distal collecting duct, increasing water reabsorption.
What is the obligatory water loss in the kidneys?
0.5 L/day.
How do the kidneys concentrate urine when the body is dehydrated?
By allowing water to diffuse out of the collecting ducts due to hyperosmotic interstitial fluid.
What is the function of the ascending limb of the Loop of Henle?
It establishes a vertical osmotic gradient in the kidney.
How do collecting ducts utilize the osmotic gradient established by the Loop of Henle?
They use the gradient along with ADH to produce urine of varying concentrations.
What happens in the absence of ADH in the distal and collecting tubules?
They become impermeable to H2O, resulting in a large volume of dilute urine.
How do the kidneys maintain blood pH?
By reabsorbing bicarbonate and secreting H+.
What mechanism do proximal tubules use to exchange Na+ and H+?
Na+/H+ pumps are used to exchange Na+ out and H+ in.
How is bicarbonate reabsorbed from the filtrate?
HCO3- is reabsorbed indirectly from the filtrate.
How do kidneys compensate for respiratory problems?
They adjust bicarbonate reabsorption and H+ secretion to maintain acid-base balance.
What is the relationship between dehydration and ADH secretion?
Dehydration triggers the secretion of ADH to conserve water.
What happens to urine concentration when the body is well-hydrated?
The kidneys produce dilute urine with low ADH levels.
What is the role of the macula densa in renal function?
It helps regulate renal blood flow and glomerular filtration rate.
What is the significance of the counter-current multiplier system?
It enhances the kidney's ability to concentrate urine by creating an osmotic gradient.
What is the effect of excess water ingestion on ADH secretion?
It leads to decreased ADH secretion, resulting in increased water excretion.
What is respiratory acidosis?
A condition where the lungs cannot remove all of the carbon dioxide the body produces, leading to decreased blood pH.
What is micturition?
The process of urine elimination from the body.
How does urine in the bladder affect the body?
It stimulates stretch receptors that signal smooth muscle in the bladder wall.
What role do parasympathetic neurons play in micturition?
They signal the smooth muscle in the bladder wall to contract.
What are the main functions of the kidneys?
The kidneys filter blood, remove waste, regulate fluid balance, and maintain electrolyte levels.
What are the basic components of the urinary system?
The kidneys, ureters, bladder, and urethra.
What is a nephron?
The functional unit of the kidney, responsible for filtering blood and forming urine.
What are the components of a nephron?
The renal corpuscle and renal tubules.
What are the three basic processes of the nephron?
Filtration, reabsorption, and secretion.
What structures are involved in glomerular filtration?
The glomerulus and Bowman's capsule.
What is the significance of the glomerular filtration rate (GFR)?
It measures how well the kidneys filter blood and is regulated by various factors.
How does the sympathetic nervous system affect GFR?
It can decrease GFR by constricting afferent arterioles.
What is tubular reabsorption?
The process by which the kidneys reclaim water and solutes from the filtrate back into the blood.
What is transport maximum?
The maximum rate at which substances can be reabsorbed by the renal tubules.
What is tubular secretion?
The process of transferring substances from the blood into the tubular fluid.
What substances typically undergo tubular secretion?
Potassium, hydrogen ions, and certain drugs.
What is renal clearance?
The volume of plasma from which a substance is completely removed by the kidneys per unit time.
How does renal plasma clearance relate to GFR?
It is used to measure GFR and is affected by reabsorption and secretion.
What is the countercurrent multiplier system?
A mechanism that helps concentrate urine and maintain water balance in the body.
What stimulates ADH secretion?
Increased plasma osmolality or decreased blood volume.
How does ADH promote water reabsorption?
By increasing the permeability of the renal tubules to water.