applied clinical neuroscience
5.0(2)
Card Sorting
1/250
Earn XP
Description and Tags
Last updated 3:20 PM on 3/19/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
251 Terms
1
New cards
psychopathology
the systematic study of abnormal psychic experience, cognition and behavior; the fundamental professional skill of the psychiatrist, possibly the only diagnostic skill unique to the psychiatrist
2
New cards
descriptive psychopathology
simply describes with empathy and understanding. one of the most important principles is not to make assumptions about the causes or consequences of signs and symptoms of mental disorder, but merely to define, differentiate, and inter-relate them; precise description, categorization and definition of abnormal psychic experiences as recounted by the patient; includes two distinct parts: empathy (empathic assessment of the patient’s subjective experience), and observation (observed in his behavior)
3
New cards
explanatory psychopathology (e.g., psychoanalytical, behavioral)
assumes explanation according to the theoretical construct
4
New cards
empathy
the aim is to listen attentively, to accurately observe and understand the psychological event or phenomenon by empathy so that the clinician can, as far as possible, know for himself what the patient’s experience must feel like; it is this that allows the doctor to come to understand the patient’s experiences; when it fails to render a patient’s subjective experience understandable, we can then talk about that experience as being understandable
5
New cards
observation
of the objective expression of subjective experience, through meaningful gestures, bodily stance, behavior and actions
6
New cards
disease/illness
results from a pathophysiological response to external or internal factors
7
New cards
disorder
a disruption by the disease/illness to the normal or regular functions in the body or a part of the body
8
New cards
WHO definition of health
a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity
9
New cards
disorders as defined by Griesinger
diseases of the brain, but there is no “gold standard” lab test or physiological indicator for mental disorders
10
New cards
disorders as defined by Kendell
considered a statistical variation of the norm, carrying biological disadvantage e.g., reduced fecundity or a shortened life
11
New cards
individual norm
the consistent level of functioning that an individual maintains over time: suffering, maladaptiveness, vividness & unconventionality, unpredictability & loss of control or irrationality/incomprehensibility, causes observer discomfort, violates moral/social standards
12
New cards
social norm
doesn’t violate the (unwritten) rules about what is expected or acceptable behavior in a particular social group
13
New cards
statistical norm
falling outside the average range
14
New cards
biological norm
structural, functional, chemical brain alterations
15
New cards
signs vs symptoms
patient complains of symptoms, while physical signs are elicited on the examination
16
New cards
symptom
patient’s description of an abnormal mental phenomenon
17
New cards
objective
refers to features described during an interview (e.g., the patient’s appearance and behavior)
18
New cards
subjective
describes the personal account of the patient
19
New cards
form vs content
form would be an auditory hallucination vs content being that the hallication is calling him a homosexual; form is critical when making a diagnosis; content is less diagnostically useful, but important to management, and of the concern to the patient whereas form is not
20
New cards
primary
arising directly from the pathological process
21
New cards
secondary
arising as a reaction to a primary symptom
22
New cards
psychiatric examination
1. demographic info
2. source and reason for referral and mode (voluntary/involuntary)
3. present complaints/illness (symptoms and chronology)
4. previous medical history (psychiatric, physical, treatment)
5. family history
6. personal history
7. social data
8. substance
9. pre-morbid personality (patient’s relationships with other people, interests and activities)
10. mental state examination
23
New cards
mental state examination
1. appearance and behavior
2. speech
3. mood, anxiety (and risk assessment)
4. thought
5. perception
6. cognition
7. insight
24
New cards
consciousness
the whole of psychic life at any given moment
25
New cards
quantitative alterations of consciousness
hyperalert/hypervigilant (high alert)
clouding of consciousness (low alert)
somnolent (low alert)
coma (low alert)
clouding of consciousness (low alert)
somnolent (low alert)
coma (low alert)
26
New cards
qualitative alterations of consciousness
confusion
delirium (acute confusional state)
stupor
delirium (acute confusional state)
stupor
27
New cards
circumstantiality
circuitous and non-direct thinking or speech that digresses from the main point of a conversation
28
New cards
tangentiality
a communication disorder in which the train of thought of the speaker wanders and shows a lack of focus, never returning to the initial topic of the conversation
29
New cards
metonymy
figure of speech in which the name of an object or concept is replaced with a word closely related to or suggested by the original
30
New cards
neologism
a new word or expression in a language, or a new meaning for an existing word or expression
31
New cards
ability of speech
dysphonia (breaks or interruptions in speech, often every few sentences), dysarthria (slurred or slow speech), dysphasia (trouble putting the right words together in a sentence, understanding what others say, reading, and writing)
32
New cards
amount of speech
logorrhea (pathologically incoherent, repetitious speech), poverty of speech (lack of conversation)
33
New cards
rate of speech
pressure of speech (when you talk faster than usual), speech retardation (a child is not able to use words or other forms of communication at the expected ages), mutism (inability to speak, typically as a result of congenital deafness or brain damage)
34
New cards
emotions
multi-faceted, short-lived, reactive experiences. there are three main components: (i) internal subjective experiences, accompanied by (ii) physiological response (e.g., heart beating) and (iii) behavioral expressions (facial expressions)
35
New cards
sentiments
the expression of emotions where they become tied to a social object. this connect emotions with the social and cultural aspects. these are highly organized (e.g., love, jealousy, contempt, grief)
36
New cards
mood
the basal, pervasive and sustained internal emotional climate, which can influence all aspects of behavior: “that aspect of psychic activity which gives emotional tonality, the affective coloring of all that is experienced). it’s a prolonged emotion
37
New cards
mood predispositions
1. euthymia (a normal, tranquil mental state or mood)
2. dysthymia (a milder, but long-lasting form of depression)
3. hyperthymia (a mental illness and personality type in which the person is in a near-continual state of mild mania, thus having abnormally high levels of energy, enthusiasm, positivity, and the like)
4. cyclothymia (causes emotional ups and downs, but they're not as extreme as those in bipolar I or II disorder)
38
New cards
mood reactions
1. anxiety
2. irritability
3. depression
4. anhedonia (inability to feel pleasure in normally pleasurable activities)
5. apathy (lack of interest, enthusiasm, or concern)
6. euphoria
7. ecstasy
39
New cards
affect
the visible behavioral reaction a person displays toward events (emotional expression). it’s momentary
1. normal affect
2. expansive affect
3. blunted/constricted affect
4. flat affect
5. labile affect
6. emotional incontinence
7. emotional ambivalence
8. dissociation of affect
9. inappropriate affect
10. perplexity
1. normal affect
2. expansive affect
3. blunted/constricted affect
4. flat affect
5. labile affect
6. emotional incontinence
7. emotional ambivalence
8. dissociation of affect
9. inappropriate affect
10. perplexity
40
New cards
stream of thought
1. pressure of thought (thought arise in unusual variety and abundance and pass through the mind quickly. this is evidenced as pressure of speech)
2. poverty of thought (the opposite of pressure of thought, evidenced as poverty of speech)
3. thought blocking (sudden loss of the train of thought, often in mid-sentence. there is a subjective experience of the mind just ‘going blank’)
41
New cards
form of thought
1. flight of ideas (thoughts move quickly from one to another and seem to be only loosely connected)
2. loosening of associations (thoughts move quickly from one to another and seem unconnected. evidenced as muddled or illogical speech)
3. over-inclusive thinking (an inability to preserve the conceptual boundaries of thought)
4. concrete thinking (an inability to understand abstract concepts and metaphorical ideas)
42
New cards
content of thought
delusions vs other ideas
1. phobia
2. preoccupation/rumination
3. obsessions
4. magical thinking (an irrational but not delusional belief that certain outcomes are connected to certain thoughts, words, or actions)
5. overvalued ideas (idiosyncratic and firmly held belied which is in itself acceptance and comprehensible but which comes to dominate thinking and behavior, not delusional)
6. idea of reference (the idea that causal incidents and external events are referring directly to oneself, not delusional)
1. phobia
2. preoccupation/rumination
3. obsessions
4. magical thinking (an irrational but not delusional belief that certain outcomes are connected to certain thoughts, words, or actions)
5. overvalued ideas (idiosyncratic and firmly held belied which is in itself acceptance and comprehensible but which comes to dominate thinking and behavior, not delusional)
6. idea of reference (the idea that causal incidents and external events are referring directly to oneself, not delusional)
43
New cards
delusion
an unshakeable (fixed) belief that is held in the face of evidence to the contrary, and that cannot be explained by culture or religion. not necessarily false, the process by which it arises is not understandable
there can be no phenomenological definition because the patient is likely to hold this belief with the same conviction and intensity as he holds other non-delusional beliefs about himself
there can be no phenomenological definition because the patient is likely to hold this belief with the same conviction and intensity as he holds other non-delusional beliefs about himself
44
New cards
Jaspers’ characteristics of delusions (1909)
1. they are false judgements
2. they are held with extraordinary conviction and incomparable subjective certainty
3. they are impervious to other experiences and to compelling counterargument
4. their content is impossible
45
New cards
primary delusion
fully formed delusion that is unconnected to previous ideas or events and that is psychologically irreducible
46
New cards
secondary delusion
delusion that arises from, and that is understandable in context of, previous ideas or events
47
New cards
delusional perception
the attribution of delusional significance to normal percepts
“i smell food cooking and then form the delusion that the food is poisoned”
“i smell food cooking and then form the delusion that the food is poisoned”
48
New cards
delusional memory
the attribution of delusional significance to a memory or false memory
“i remember listening to a string quartet and form the delusion of being a great music composer”
“i remember listening to a string quartet and form the delusion of being a great music composer”
49
New cards
delusional mood or atmosphere
the world seems subtly altered, uncanny, portentous, or sinister. this is often the first symptom of schizophrenia and the context of which a fully formed delusional percept or intuition arise
“i already feel irritable, and when i collect my car from the garage and it makes an unexplained noise i become delusionally convinced the FBI has put a spying camera into it”
“i already feel irritable, and when i collect my car from the garage and it makes an unexplained noise i become delusionally convinced the FBI has put a spying camera into it”
50
New cards
content of delusions
1. control (first-rank symptoms of schizophrenia)
2. persecution
3. reference
4. misidentification (capgras, fregoli, doppelgänger)
5. grandeur
6. religious
7. guilt
8. nihilistic (cotard)
9. somatic (koro)
10. infestations
11. jealousy
12. love
51
New cards
sensory distortions
a real object is perceived in a distorted way
52
New cards
hallucinations
a perception-like experience with the clarity and impact of a true perception but without the external stimulation of the relevant sensory organ
\* distinguished from illusions, in which an actual external stimulus is misperceived or misinterpreted
\* distinguished from illusions, in which an actual external stimulus is misperceived or misinterpreted
53
New cards
how do pseudo-hallucinations differ from true hallucinations?
1. it is perceived to arise from the mind (inner space) rather than from the sense organs (outer space)
2. less vivid
3. less distressing
4. the patient may have some degree of control over it
54
New cards
depersonalization
an alteration in the perception or experience of the self, leading to a sense of detachment from one’s mental processes or body processes or body
55
New cards
derealization
an alteration in the perception or experience of the environment, leading to a sense that it is strange or unreal
56
New cards
cognition
orientation in time, place, and person
QI (80-120; 55-70 mild, 35-55 moderate, 25-35 severe)
the mini-mental state examination (MMSE) tests it
QI (80-120; 55-70 mild, 35-55 moderate, 25-35 severe)
the mini-mental state examination (MMSE) tests it
57
New cards
insight
patient’s attitude to his illness, difficulties, and prospects: recognition of subjective psychological change, labeling of this change as pathological in nature, cognition of need for treatment as well as compliance with treatment
58
New cards
predisposing factors
factors or areas of susceptibility that promote the risks of the presenting problem
59
New cards
precipitating factors
these are factors, events, or stressors that initiate or promote the onset of any illness, disease, accident, or behavioral response
60
New cards
perpetuating factors
these are factors that maintain the disabling symptoms. any condition or factors, either in the family or community that exaggerate the problem rather than solve it are perpetuating factors
61
New cards
protective factors
these are factors that take into account the person’s skill, competency, talent, or any supportive element that helps the patient in facing and overcoming the predisposing, precipitating, and perpetuating factors
62
New cards
DSM-5-TR
advantages:
1. standardization
2. research guidance
3. treatment guidance
\
disadvantages:
1. oversimplification of human behavior
2. misdiagnoses and over-diagnoses
3. labeling and stigmatization
1. standardization
2. research guidance
3. treatment guidance
\
disadvantages:
1. oversimplification of human behavior
2. misdiagnoses and over-diagnoses
3. labeling and stigmatization
63
New cards
64
New cards
psychodynamic diagnostic manual (PDM)
aimed to promote integration between nomothetic understanding and the idiographic knowledge that is useful for individual case formulation and the planning of patient-tailored treatment
65
New cards
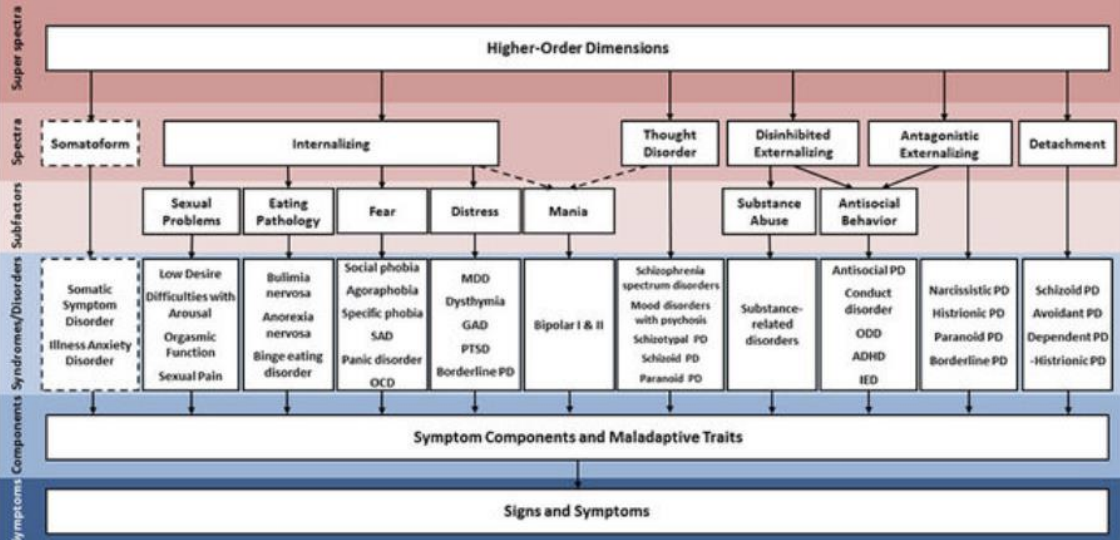
hierarchical taxonomy of psychopathology (HiTOP)
a data-driven, hierarchically based alternative to traditional classifications that conceptualizes psychopathology as a set of dimensions organized into increasingly broad, transdiagnostic spectra
66
New cards
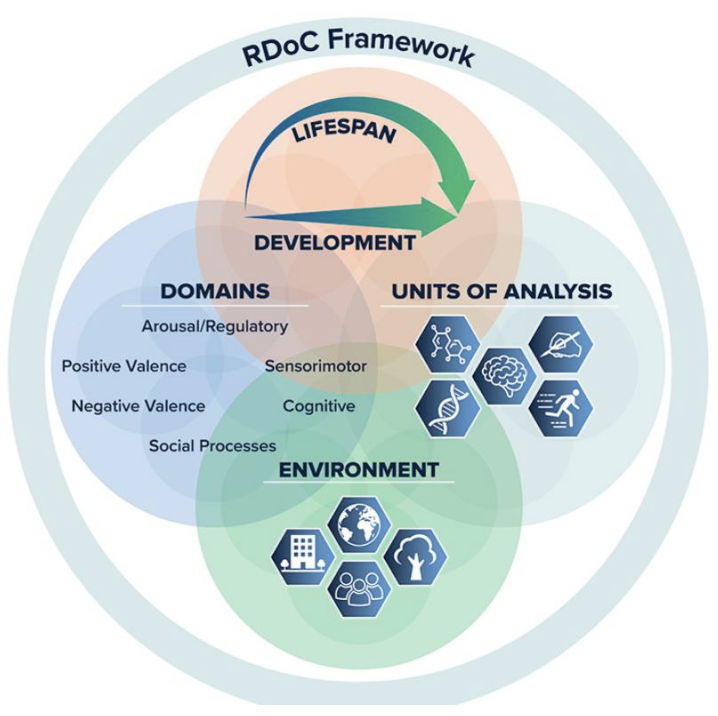
Research Domain Critera (RDoC) Framework
a research framework for investigating mental disorders. the aim is to understand the nature of mental health and illness in terms of varying degrees of dysfunction in fundamental psychological/biological systems
67
New cards
tools
clinician rated:
1. brief psychiatric rating scale (BPRS)
2. structured clinical interview for DSM-5 (SCID-5)
self rated:
1. symptom check list-90-revised (SCL-90-R)
2. general health questionnaire (GHQ-12)
3. patient health questionnaire (PHQ-9)
4. community assessment of psychic experiences (CAPE-42)
1. brief psychiatric rating scale (BPRS)
2. structured clinical interview for DSM-5 (SCID-5)
self rated:
1. symptom check list-90-revised (SCL-90-R)
2. general health questionnaire (GHQ-12)
3. patient health questionnaire (PHQ-9)
4. community assessment of psychic experiences (CAPE-42)
68
New cards
primary mood disorder
one that does not result from another medical or psychiatric condition
69
New cards
secondary mood disorder
one that results from another medical or psychiatric condition (e.g., anaemia, hypothyroidism, or substance misuse)
70
New cards
major depressive disorder (MDD)
lifetime risk of DSM-depressive disorders is about 15%
prevalence of depressive disorders is about 5%
females are more affected than men (2:1) due to genetic predisposition, hormonal influences, social pressures, etc.
peak prevalence for depressive disorders in men is in old age, while women it’s middle age
somatic presentations are particularly common in Asian and African cultures
prevalence of depressive disorders is about 5%
females are more affected than men (2:1) due to genetic predisposition, hormonal influences, social pressures, etc.
peak prevalence for depressive disorders in men is in old age, while women it’s middle age
somatic presentations are particularly common in Asian and African cultures
71
New cards
etiology of MDD
1. genetic vulnerability (degree in relatives is 15%, while 5% in general pop; 46% monozygotic twins, 20% dizygotic)
2. neurochemical alterations (monoamine hypothesis suggests that depression results from depletion of the monoamine neurotransmitters, noradrenaline, serotonin, and dopamine)
3. endocrine and immune alterations (plasma cortisol levels are increased in about 50% of depression sufferers and that 50% fail to respond to the dexamethasone suppression test)
4. organic causes
5. personality traits
6. environmental factors
7. psychological causes
72
New cards
clinical symptoms of MDD
core:
1. low mood
2. loss of interest and enjoyment
3. fatigability
psychological:
1. poor concentration
2. poor self esteem
3. guilt
4. pessimism
somatic:
1. sleep disturbance
2. early morning waking
3. morning depression
4. loss of appetite and weight loss
5. loss of libido
6. anhedonia
7. agitation or retardation
1. low mood
2. loss of interest and enjoyment
3. fatigability
psychological:
1. poor concentration
2. poor self esteem
3. guilt
4. pessimism
somatic:
1. sleep disturbance
2. early morning waking
3. morning depression
4. loss of appetite and weight loss
5. loss of libido
6. anhedonia
7. agitation or retardation
73
New cards
depression symptoms in children and adolescents
physical:
1. tiredness or low energy, even when rested
2. restlessness or difficulty concentrating
3. difficulty in carrying out daily activities
4. changes in appetite or sleep patterns
5. aches or pains that have no obvious cause
emotional and psychological:
1. persistent sadness, anxiousness or irritability
2. loss of interest in friends and activities that they normally enjoy
3. withdrawal from others and loneliness
4. feelings of worthlessness, hopelessness or guilt
5. taking risks they normally wouldn’t
6. self-harming or suicidal thoughts
1. tiredness or low energy, even when rested
2. restlessness or difficulty concentrating
3. difficulty in carrying out daily activities
4. changes in appetite or sleep patterns
5. aches or pains that have no obvious cause
emotional and psychological:
1. persistent sadness, anxiousness or irritability
2. loss of interest in friends and activities that they normally enjoy
3. withdrawal from others and loneliness
4. feelings of worthlessness, hopelessness or guilt
5. taking risks they normally wouldn’t
6. self-harming or suicidal thoughts
74
New cards
depression in older adults
1. sadness or feelings of despair
2. unexplained or aggravated aches and pains
3. loss of interest in socializing or hobbies
4. weight loss or loss of appetite
5. feelings of hopelessness or helplessness
6. lack of motivation and energy
7. sleep disturbances
8. loss of self-worth
9. slowed movement or speech
10. increased use of alcohol or other drugs
11. fixation on death, thoughts of suicide
12. memory problems (pseudo-dementia)
13. neglecting personal care
75
New cards
differential diagnosis
the process of differentiating between two or more conditions which share similar signs or symptoms.
76
New cards
course of MDD
average length is about 6 months
after the first episode, about 80% have further episodes
they tend to get longer and inter-episode intervals get shorter
about 10% of patients develop a chronic unremitting disorder, and about 10% of patients have a manic episode and so “convert” to bipolar affective disorder
after the first episode, about 80% have further episodes
they tend to get longer and inter-episode intervals get shorter
about 10% of patients develop a chronic unremitting disorder, and about 10% of patients have a manic episode and so “convert” to bipolar affective disorder
77
New cards
MDD treatment
antidepressants are NOT recommended in mild depression: just watchful waiting, problem solving and exercising are preferred
when an antidepressant is prescribed, a generic SSRI is recommended
for severe or resistant depression a combo of antidepressants and CBT is recommended
a single first episode should be treated for 4-6 months after recovery
patients with two prior episodes and functional impairments should be treated for at least 2 yrs
when an antidepressant is prescribed, a generic SSRI is recommended
for severe or resistant depression a combo of antidepressants and CBT is recommended
a single first episode should be treated for 4-6 months after recovery
patients with two prior episodes and functional impairments should be treated for at least 2 yrs
78
New cards
MDD tools
clinician administered:
1. Hamilton Depression Rating Scale (HAM-D)
2. Montgomery-Åsberg Depression Rating Scale (MADRS)
self-report:
1. Beck Depression Inventory (BDI)
1. Hamilton Depression Rating Scale (HAM-D)
2. Montgomery-Åsberg Depression Rating Scale (MADRS)
self-report:
1. Beck Depression Inventory (BDI)
79
New cards
epidemiology of bipolar disorders
the lifetime risk ranges from 0.3% to 1.5% and because it’s chronic, the prevalence rate is fairly similar
all races and sexes are equally affected
the mean age of onset is 21 yrs, first manic ep after age 50 is sus and should lead to investigation
prevalence is higher in higher socioeconomic groups
prevalence is 10-40x higher amongst artists than amongst the general public
all races and sexes are equally affected
the mean age of onset is 21 yrs, first manic ep after age 50 is sus and should lead to investigation
prevalence is higher in higher socioeconomic groups
prevalence is 10-40x higher amongst artists than amongst the general public
80
New cards
etiology of bipolar disorders
1. genetic vulnerability
2. neurochemical alterations
3. life events
81
New cards
clinical features in bipolar disorders
appearance: normally dressed in colorful clothing or in unusual, haphazard combos of clothing
behavior: hyperactive, entertaining, charming, flirtatious, vigilant, assertive, etc
mood and affect: usually euphoric, optimistic, self-confident, grandiose, but may be irritable or tearful, with rapid and unexpected shifts from one extreme to another
speech/thought: their thoughts race through their mind at high speed and as a result their speech is pressured and voluble and difficult to interrupt
thought: typically full of grandiose and unrealistic plans that they begin to act upon but soon abandon
perception/thought: people with mania may also experience psychotic symptoms
content of thought: delusional themes are usually congruent or in keeping with the elevated mood, and often involve delusions of grandeur, that is, delusions of exaggerated self-importance of special status, special purpose, or special abilities, **mania rarely complaint by the patient as symptom**
insight: w mania generally have poor insight into their mental state
behavior (interview): they often engage in impulsive, pleasure-seeking, and disinhibited behavior
behavior: hyperactive, entertaining, charming, flirtatious, vigilant, assertive, etc
mood and affect: usually euphoric, optimistic, self-confident, grandiose, but may be irritable or tearful, with rapid and unexpected shifts from one extreme to another
speech/thought: their thoughts race through their mind at high speed and as a result their speech is pressured and voluble and difficult to interrupt
thought: typically full of grandiose and unrealistic plans that they begin to act upon but soon abandon
perception/thought: people with mania may also experience psychotic symptoms
content of thought: delusional themes are usually congruent or in keeping with the elevated mood, and often involve delusions of grandeur, that is, delusions of exaggerated self-importance of special status, special purpose, or special abilities, **mania rarely complaint by the patient as symptom**
insight: w mania generally have poor insight into their mental state
behavior (interview): they often engage in impulsive, pleasure-seeking, and disinhibited behavior
82
New cards
hypomania
a lesser degree of mania and as such its clinical features are very similar to those seen in mania
doesn’t last as long or intensely as mania
doesn’t last as long or intensely as mania
83
New cards
bipolar I diagnostic criteria
manic episode may have been preceded by and may be followed by hypomanic or major depressive episodes
84
New cards
bipolar disorder type II diagnostic criteria
meet the criteria for a current or past hypomanic episode *and* the following criteria for a current or past major depressive episode
85
New cards
differential diagnosis: bipolar and psychiatric disorders
1. mixed affective states (simultaneous manic and depressive symptoms)
2. schizoaffective disorder
3. schizophrenia
4. ADHD
5. drugs such as alcohol, amphetamines, cocaine, hallucinogens, antidepressants, etc
86
New cards
differential diagnosis: bipolar and medical or organic disorders
1. organic brain disease of the frontal lobes such as MS, epilepsy, AIDS
2. endocrine disorders such as hyperthyroidism
3. systemic lupus erythematosus
4. sleep deprivation
87
New cards
course of bipolar disorder
average length of a manic ep is about 4 months; after first manic episode, about 90% of patients experience further manic and depressive episodes and inter-episode intervals get shorter; prognosis is poor and is more so in rapid-cycling and less so in bipolar ii; 10% commit suicide but attempted percentage is much higher
88
New cards
tools for bipolar
Young Mania Rating Scale (YMRS)
89
New cards
psychological symptoms: anxiety
1. feelings of fear and impending doom, feelings of dizziness and faintness, restlessness, exaggerated startle response, poor concentration, irritability, insomnia and night terrors, depersonalization and derealization
2. *globus hystericus* or *globus* is the irritating feeling of having a lump in the throat. it leads to forced swallowing and a characteristic gulping sound that is often mimicked in children’s cartoons to signal fear
90
New cards
epidemiology of anxiety-related (neurotic) disorders
1. have their onset in early adulthood, sometimes middle age
2. prevalence is difficult to estimate bc many don’t present to medical attention
3. affects around 18.6% of adults in the US
4. females are more affected 2:1
5. depressive symptoms are common and vice versa
6. comorbidity is common
91
New cards
etiology of anxiety-related disorders
1. psychiatric and medical conditions
2. genetic factors
3. neurochemical abnormalities
4. environmental factors
5. psychological theories
92
New cards
anxiety related disorders
specific phobia, panic disorder, GAD, etc.
93
New cards
phobia
a persistent irrational fear that is usually recognized as such and that produces anticipatory anxiety for and avoidance of the feared object, activity, or situation
94
New cards
generalized anxiety disorder (GAD)
characterized by long-standing free-floating anxiety that may fluctuate but that is neither situational nor episodic. there’s apprehension about a number of events far out of proportion to the actual likelihood or impact of the feared events.
common symptoms include symptoms of autonomic arousal, irritability, poor concentration, muscle tension, tiredness, and sleep disturbances
common symptoms include symptoms of autonomic arousal, irritability, poor concentration, muscle tension, tiredness, and sleep disturbances
95
New cards
treatment for anxiety
1. psychological therapy is more effective than pharmacological and should be used as first in line
2. pharmacological is effective, most evidence supports the use of SSRIs
3. benzos should only be used to treat severe anxiety
4. use the lowest dose for the shortest period of time (max 4 weeks) while medium/long-term treatment strategies are put in place
96
New cards
obsessive-compulsive and related disorders
OCD, body dysmorphic disorder, etc
97
New cards
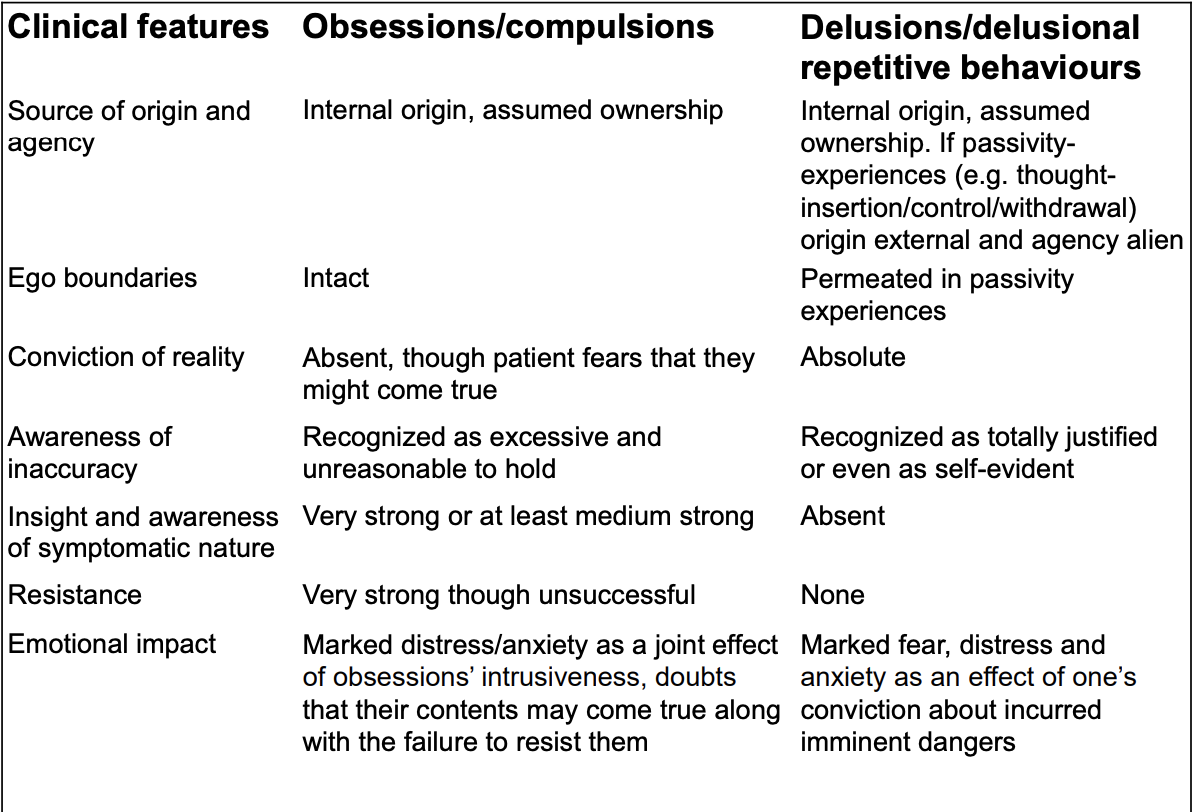
obsession
recurrent idea, image, or impulse; recognized as being a product of one’s own mind; usually perceived as being senseless; unsuccessfully resisted; results in marked anxiety and distress/impairment of functioning
98
New cards
compulsion
a recurrent stereotyped behavior; reduces anxiety but is neither useful nor enjoyable; usually perceived as senseless; unsuccessfully resisted; results in marked distress/impairment of functioning
99
New cards
obsessions v delusions
100
New cards
trauma and stress-related disorders (DSM)
PTSD, acute stress disorder, etc.