Lecture 32: Urinary System 1
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
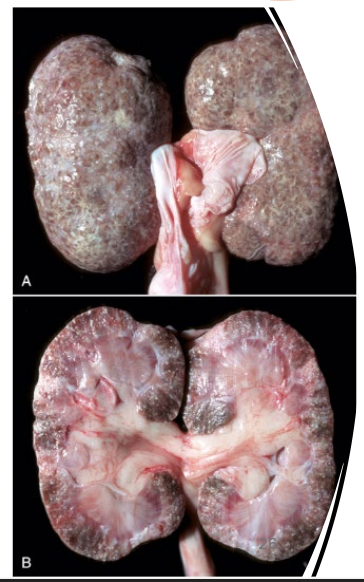
What has occurred to this kidney after a recent infection with a toxin?
renal fibrosis
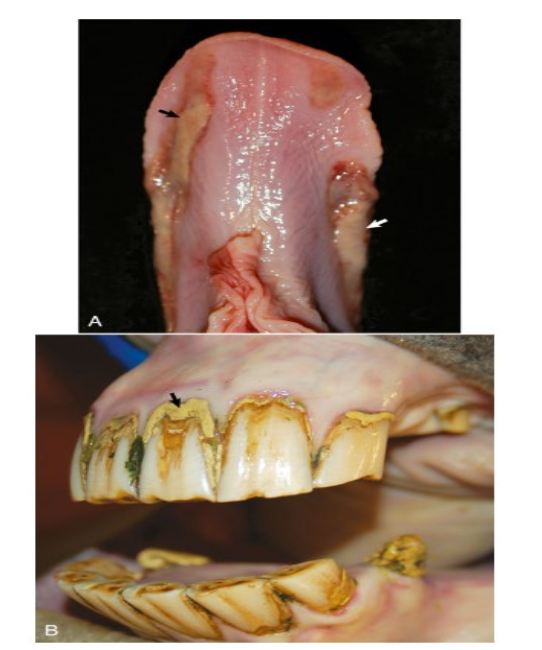
What has caused this ulcerative and necrotic glossitis/stomatitis?
uremia

How has uremia affected this tissue?
intercostal mineralization/uremic mineralization → calcification of the subpleural connective tissue of the intercostal spaces causing white-gray ladder-like thickenings

What has happened to this kidney? It feels gritty in texture upon palpation.
nephrocalcinosis due to uremia
What is the primary renal function?
filtration → reabsorption → secretion → excretion: removes waste and conserves
What is the function of RAAS (renin-angiotensin-aldosterone system)?
responds to low perfusion → induces vasoconstriction, Na+/water retention, ADH release
What hormone produced by the kidneys stimulates RBC production?
EPO (erythropoietin)
Why do the kidneys activate vitamin D?
promote Ca2+ absorption
What are the 4 structural components of the kidney?
renal corpuscles (glomerulus + Bowman’s capsule)
tubules
interstitium
vasculature
What species have unipyramidal kidneys?
dogs, cats, small ruminants, horses
What species have multipyramidal kidneys?
pigs, large ruminants (externally lobulated in cattle)
What are the steps in the RAAS?
decrease in renal perfusion → renin produced by kidney & secreted into circulation
renin converts circulating angiotensinogen produced by liver to angiotensin I
angiotensin I converted to angiotensin II via angiotensin converting enzyme
angiotensin II constricts arterioles, stimulates aldosterone secretion from adrenal gland (Na and H2O retention), and stimulates ADH (vasporessin) release from pituitary gland (reabsorb water to increased blood volume/pressrue)
What species has a yellow renal cortex due to lipid within tubular epithelial cells?
cats
What are the components of the renal corpuscle?
glomerulus and Bowman’s capsule
What is the main function of the glomerulus?
filter: remove components from blood for excretion as urine
Describe what happens as blood moves through the glomerulus?
blood enters glomerulus via afferent arteriole
filtered through fenestrated endothelium based on size, electric charge, and capillary pressure
filtered fluid accumulates in Bowman’s space
moves to proximal tubule
What part of the proximal convoluted tubule increases the absorptive surface?
microvilli brush border
What part of the nephron is highly sensitive to hypoxic stress?
tubules
What are the major functions of the renal tubules?
reabsorption back into blood stream
secretion
majority of water and solute reabsorption occurs in proximal convoluted tubules
vasa recta (blood supply) works with Loop of Henle to concentrate urine
What part of the kidney is responsible for local production of prostaglandins?
interstitium
What renal component extends into the deeper portion of the medulla with close association with the Loop of Henle in order for the countercurrent exchange that allows for concentration of urine to occur?
vasa recta
What is the general consequence of acute renal failure?
kidneys fail to excrete waste products and to maintain fluid and electrolyte homeostasis
What are the signs of acute renal failure?
metabolic acidosis (reduced blood pH)
azotemia: increased nitrogenous waste products in blood
alterations in plasma ion concentrations: potassium, calcium phosphate
excessive fluid retention if not filtering properly: pulmonary edema, hypertension
What are the three types of acute renal failure and what causes them?
prerenal: decreased renal perfusion (reduced blood flow) → shock, hypovolemia, thromboembolism
renal: intrinsic damage/comprised function (tubuluar or glomerular)
postrenal: obstruction of lower urinary tract (uroliths, neoplasia, trauma)
What are the outcomes of acute kidney failure?
hyperkalemia → bradycardia/death; fluid retention → pulmonary edema and hypertension
What are some infectious and toxic causes of acute kidney failure?
infectious: Leptospira, E. coli, streptococcus, canine hepatitis virus etc
toxins: aminoglycosides, antineoplastics, ethylene glycol, heavy metals
What pathology would you expect to find in a chronic renal failure case?
progressive nephron loss
fibrous scarring
shrunken firm kidneys with adherent capsules
What clinical signs or indicative of chronic renal failure?
PU/PD
anorexia and weight loss
vomiting
nonregenerative anemia (decreased EPO)
What would you expect to see in the blood work of a chronic renal failure case?
calcium-phosphorus imbalance: decreased GFR → hyperphosphatemia + decreased calcitriol → decreased Ca absorption → renal secondary hyperparathyroidism
What is uremia?
clinical syndrome associated with lesions of renal failure concurrently affecting different tissues and organs
What are the three uremic mechanisms?
toxins → endothelial damage → vasculitis, hemorrhage, ulceration
bacterial urease splits urea → ammonia → caustic ulcers (mouth, stomach)
phosphorus retention → hypocalcemia → secondary hyperparathyroidism
What are the common nonrenal lesions of uremia?
uremic pneumonitis: pulmonary edema and mild infiltrate of macrophages and neutrophils due to vasculitis affecting the alveolar capillaries, which results in increased vascular permeability and protein effusion
patchy or diffuse pulmonary calcification
pericarditis due to fine granular calcium deposits on the epicardium