Unit 1
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Objectives
Chapters 1, 2 (2.1-2.3, 2.5), 3, 4 (4.1-4.3, 4.5)
1. Discuss the principles of Stop the Bleed |
2. Examine nursing interventions in administering Narcan (naloxone) |
1. Examine the components and span of population health
2. Discuss the foundations of Public/Community health
3. Review the historical influences in public health nursing
4. Examine the principles, standards, and competencies of public health nursing practice.
5. Determine the levels of prevention in caring for individuals, families, groups, and communities
6. Identify the challenges for public health nurses in the 21st century
7. Evaluate health status indicators and trends
8. Discuss global health security
Think of examples
Discuss principles of stop the bleed
Identify S/S- Bright red, spurting, pool of blood, pts clothes are soaked
1. Your safety is your first priority
ABC’s of stop the bleed
A- Alert 911
B- Bleeding ( find where it is coming from)
C- Control the bleed
Stop the bleed
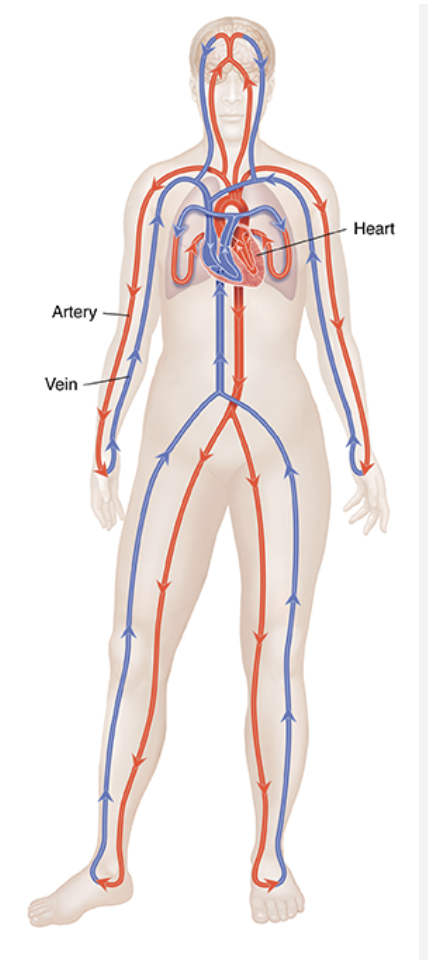
Apply pressure- Carotid, brachial, femoral
Packing ( Kerlix) Carotid, chest, head, groin, brachical( up into the armpit) , femoral. In our big arteries we want to pack or hold pressure and not use a tourniquet. Packing upwards.
Tourniquet- Extremities, Amputation ( use 2 tourniquets, rotate 2nd tourniquet a little more)
S/S of continuous/arterial bleeding - Gushing blood, bright red, pulsating
Notes- Roll pt on their back- do claw search to look for other holes/ trauma.
Dont want the pt standing, wrap them up in a warm blanket bc as temp decreases the blood starts to thin.
For extremities we can pack the wound and then put a tourniqet over.
Ideally take the tourniquet off in 2 hrs
When an artery is cut- dont want to pack down
Dont unbuckle a pt
2. Examine nursing interventions in administering Narcan (naloxone) |
•Opioid refers to all natural, semi-synthetic and synthetic
•May be ingested through swallowing, snorting, smoking or injected
•An overdose causes respiratory depression/failure
Opiod Agonist- Always get it on - Will stimulate/ activate Ex. Morphine- control pain
Antagonist- naloxone, will get on receptors but it just blocks it
Signs & Symptoms of an Opioid Overdose
•Pale, clammy skin
•Speech infrequent, not breathing, very shallow breathing
•Deep snorting or gurgling
•Unresponsive to stimuli (calling name, shaking or sternal rub
•Slowed heart beat/ pulse
•Cyanotic skin coloration (blue lips, fingernails)
•Pinpoint pupils
Naloxone / NARCAN
Opioid antagonist which reverse opioid overdose
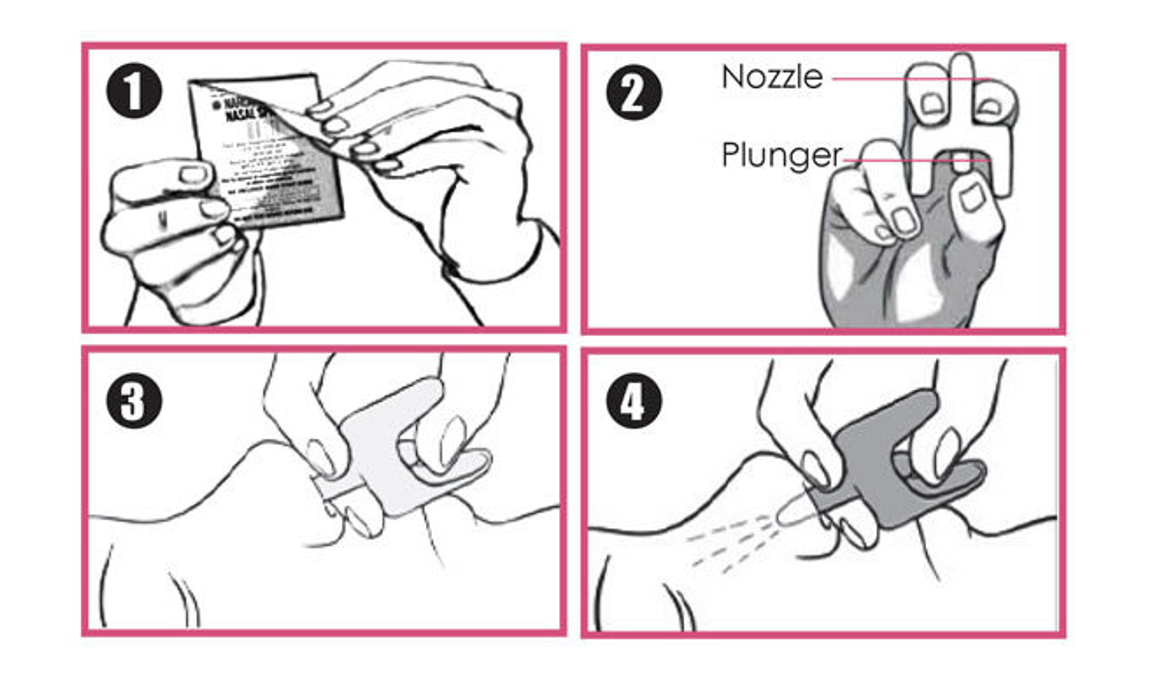
Used in the form of intranasal spray or injectable

•Narcan only reverses the effects of opioid drug overdoses
•If someone overdoses and you are not certain of the medication type, Narcan WILL NOT cause harm to the individual if given. It will just not help them.
•Is safe for use with children
•Each box contains two doses of 4 mg nasal spray
•A second dose can be administered in 2-3 minutes if the first dose is not enough
Step 1: Check Responsiveness
•Tap the person on the shoulder asking “Are You OK?”
•Shout their name and Wake up
•Call 9-1-1
Step 2: Roll the person onto their back
•APPLY GLOVES
•Place the person gently on their back
•Tilt the head
•Lift chin

Step 3: administer Narcan
Step 4: Recovery Position
•Place the patient on their side in the recovery position.
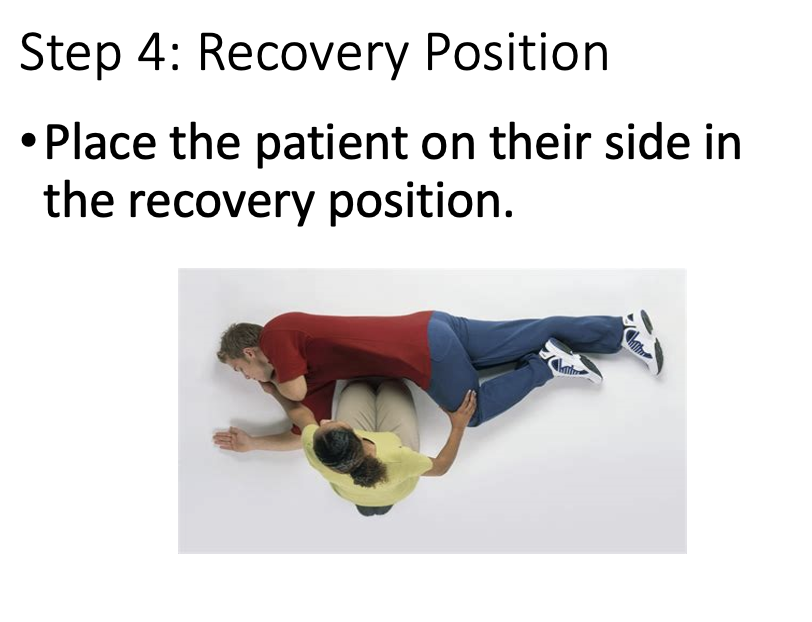
•More than one dose may be needed
•Individuals must seek medical attention after Narcan use
•Remember Narcan has no effect on the individual if an opiate is not present
What are Common Opioids Narcan can reverse:
•Codeine
•Fentanyl (Duragesic)
•Heroin
•Hydrocodone (Vicodin)
•Hydromorphone (Dilaudid)
•Illicitly-made fentanyl (IMF)
•Methadone
•Morphine
•Oxycodone (Oxycontin, Percodan, Percocet)
What drugs will narcan not work for?
▪Non-opioid sedatives:
▪Alcohol
▪Clonidine
▪Clonopin
▪Elavil
▪Valium
▪Xanax
▪Stimulants:
▪Amphetamines
▪Cocaine
What is population health
a comprehensive approach that spans the entire health care continuum- from public health prevention to disease management. Ex. Exercise, diet
Span:
focuses on Proactive rather than being Reactive. Ex. Tobacco cessation- we do preventions. it would also consider the broader factors contributing to smoking rates and smoking uptake across the population. Developing community-wide antismoking campaigns, Advocating for schools, businesses, restaurants, and other public places to develop smoke-free policies
Holistic view.- well being for all in all aspects of life
Healthy People 2030 objectives/goals! Every 10 years…working on 2040.
Population health priorities- chronic diseases, maternal child- why we have poor fetal outcomes esp for AA. Violence prevention, mental health- health behavior, the environment
What are the factors in public health
Allocation of resources: Time and money for greatest impact. Want to make sure our resources do the most good.
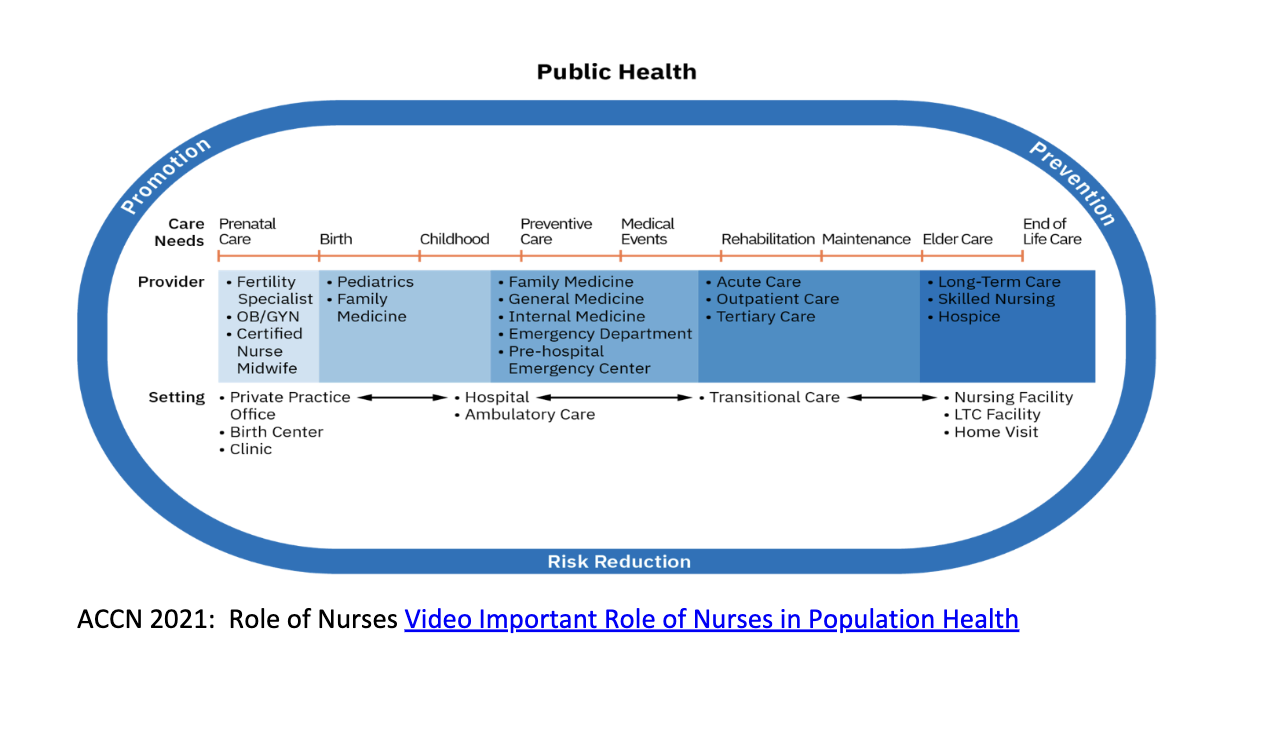
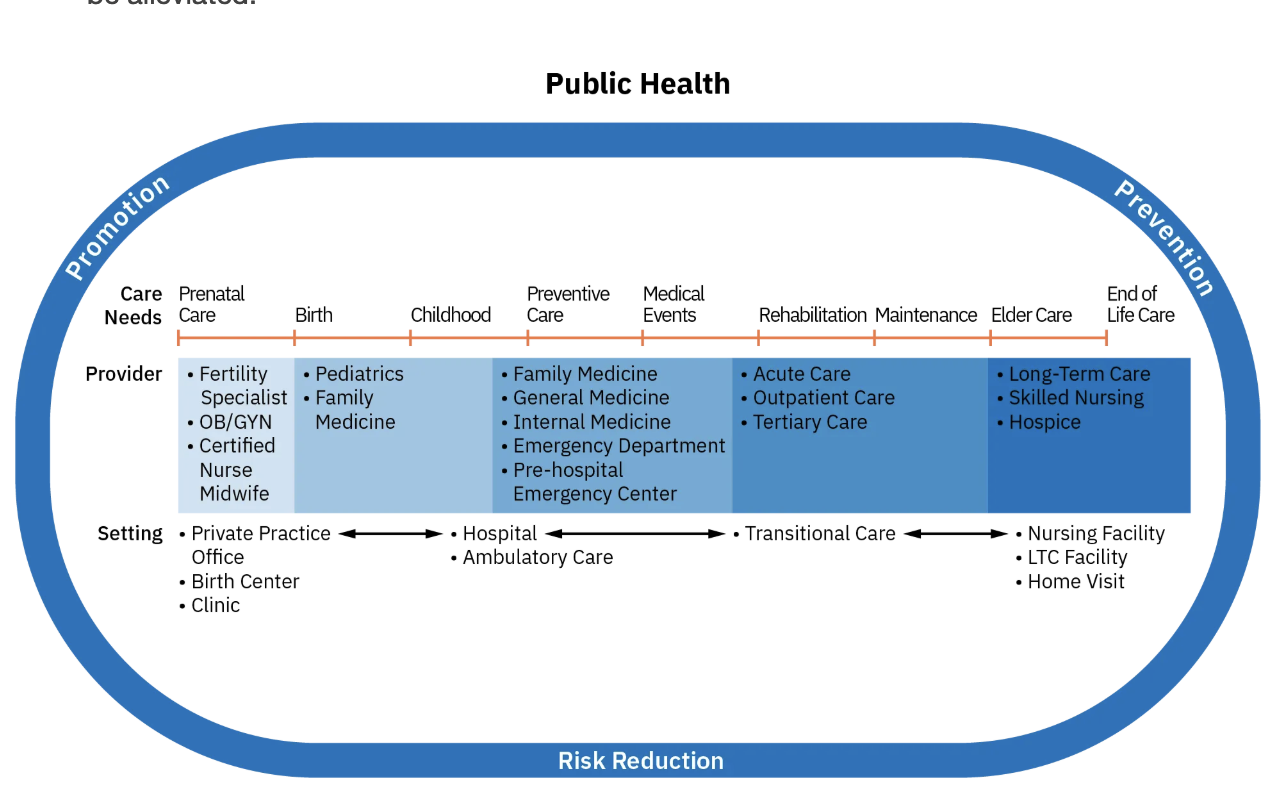
Health Care Continuum: p.23
The health care continuum encompasses public health, acute care, ambulatory care, and long-term care to collectively address a population’s diverse health needs.
- Full meal- from beginning to end of life. Includes aspects of public health. Role of nurses= advocating for policies, implementing interventions, justice, access, goals focused on health promotion, disease prevention, risk reduction, and emergency preparedness.
ex. Teaching young that smoking is bad
How do we reduce the burden of cost and reduce ill health
Collaborate w pts. Ask pts what wellness looks like to them- work with them to make a plan. Start young before they try it. Be proactive.
Patient Protection and Affordable Care Act (ACA)- A shift from treatment more towards prevention and populations. Ex. Not being in the middle of a fire but keeping the fire from happening. Prevention and health promotion is our ideal. Ex. Flu shot.
Quintuple Aim:
1. Improving client experience- help the client. Improve client outcomes
2. Improve the health of the population and the environment
3. Reduce the cost of healthcare and ill health
4. Improve the wellbeing of healthcare professionals
5. Equity and access- Ex. Should be able to get access, not just race, its even where you live. Ex. Nacogdoches has less.
Ex. Faucet left running- will flood house. Ex. Mopping up floor- reacting. Our healthcare system deals with floods- adress causes rather than just fixing ( proactive)
What are 4 key concepts in advancing population health
Outcomes- are all possible results.Ex. Rates in measures. Health outcomes are indicators or data points that reflect the degree to which health interventions are effective in supporting the health status of populations.
Disparities= inequalities / differences. stem from a form of injustice. Ex. Access to clean air. parents of children have a higher average income and donated money so that each classroom could have an air conditioner.
HEALTH CARE DISPARITIES: Inequalities, location housing, nutrition, what is in a community They are gaps in healthcare experiences by the population
*****Determinants- factors that influence health conditions. . The social conditions in which people work, play and pray. They effect outcomes and risks related to income, social status, education, work environment. literacy level, home and work environment, support networks, gender, culture. Looking at quality of life and functioning. Availability of health resources.
SOCIAL DETERMINANTS OF HEALTH- SDOH.
Risk factors- behaviors and choices- more individual. For example- environmental pollution falls under determinants vs Smoking is a risk factor- both effect health but one is bigger its an influence that they have less control over. Ex. increase the likelihood of acquiring or the severity of a health condition.
What are the 5 domains that shape the social determinants of health
five domains that shape the social determinants of health (SDOH)
1 Economic stability- money
2 Education access and quality
3 Healthcare access and quality
4 neighborhood, built in environment- shelter
5 Social and community context- your village/ social support.
What are approaches to improve health
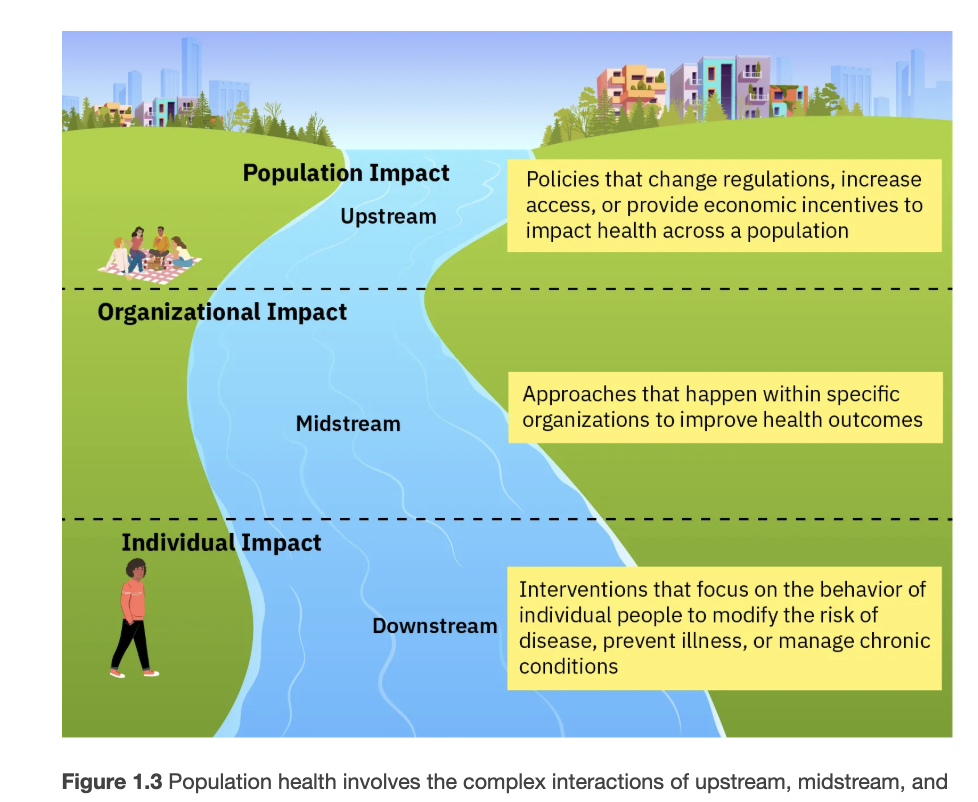
APPROACHES TO IMPROVE HEALTH- visualize a river. Group of people upstream- prevention is about keeping them from falling in. Ex. Flu vaccines. Large groups – river= state of illness. All work to improve health
Upstream – interventions involve enacting policies that change regulations, increase access, or provide economic incentives to impact health across a population. Examples include policy changes regarding the fast food or tobacco industry, provision of universal health care, and compensation for hospitals with lower inpatient admission rates ( hospital is being paid)
Midstream- Workplace incentives ( specific organizations) . Ex. Hand Sanitizer, a workplace may provide healthy lunches to employees each day
Downstream – End up in ER, individual, costs a lot. We can never just ignore downstream. Individual interventions focus on the behavior of individual people to modify the risk of disease, prevent illness, or manage chronic condition. For example, a nurse might counsel a client with hypertension about consuming a low-salt diet.
What is global population health?
GLOBAL POPULATION HEALTH:
Global reaching – Looking at the environment and how it impacts . Covid Vaccines- working to improve health. Gaza- Polio 1st case – bc of gap in vaccinations. Transportation- access issues- We have Telehealth. mortality= death rates. Morbidity- like deck of cards- the body. Ex. Here you get diabetes, making bids on your cards, Specific health conditions.
What are health indicies
summary scores that describe the health status of individuals or populations
Mortality rates -
Infant Mortality – Specific deaths before they reach 1yrs old.
Life Expectancy –
Morbidity rate – Prevalence of specific health conditions. Ex. How many people have asthma,
Health Care Utilization – use of healthcare services. How many point of contact w the healthcare system. Ex. SFA health hub, they track data for specific diseases. Ex. How many times in your 4 yrs of SFA have you gone.
Quality of Life –
Disability Adjusted Life Years (DALYs) – help describe the burden of diseases and conditions. Estimate of health years lost following premature death and disability associated condition.
–A way to measure how much illness or injury affects a population by counting how many healthy years of life are lost because people get sick, become disabled, or die early.
WHat are the benefits of population health
Can reduce cost
Can reduce death
Can reduce poverty
Can increase educational attainment
Can improve social and economic stability of populations
What are some approaches in public health
APPROACHES
Medical Interventions – flu vaccines
Social interventions – things that can significantly have an influence on the developing or worsening of health conditions. Hand wash stations, reading, smart design. Ex. Hospital without a sink right by the door. Helping little kids to read.
POPULATION BASED NURSING CARE
Siloing – ** single view in not taking in all components. Multiple healthcare providers not knowing what the other is doing or looking at other areas. Only focusing on one thing. Ex. How does primary doctor know whats going on with specialities? Who’s making sure everything’s fitting together?
What is the continum of health
Continuum of health p. 23 figure 1.6
Public health focuses on prevention measures and reduce inactive disease, improve outcomes
Acute care involves hospital and emergency departments, for sudden, severe, and emergencies. Can involve car, training, mass shooting. It is timely and effective, helps prevent mortality and complications among population and acute care.
Ambulatory care includes outpatient, health centers, annual exams, clinics, health visits to manage ongoing conditions Ex. Chronic. Targeted clinics and specialized health services in areas where select conditions are common or especially burdensome in a population.
Long-term care services are skilled nursing facilities SNIFS, private care- in homes, hospice, palliative care- comfort while undergoing. Ex. Cancer- undergoing infusions outpatient- Can introduce aspects of hospice- bc they may be going in that direction. Chronic illness, disabilities, functional limitations, Goal- minimize disabilities and support a dignified death. Can help pts and families.
TRANSITIONAL CARE – Pts need coordination, Reduces harm and provides sharing of information. Ex. Helping to fix The siloing problem.
What are population health nursing competencies ( ability to perform a role or job)
AACN 2021 (American Association of colleges of Nursing)– nursing program essentials
1. Manage Population Health
2. Engage in effective partnerships
3. Consider the socioeconomic impact of the delivery of health care.
4. Advance equitable population health policy.
5. Demonstrate advocacy strategies
6. Advance preparedness to protect population health during disasters and public health emergencies.
What is paternalism?
Public health – Research, policies, programs- will not test- just know it’s a larger group, community you can attach yourself to.
Community health – Use it; impactful to a group. (ANA says okay to combine!)- will not test
Paternalism – making decisions for others. You know better than they do. involves authority figures making decisions for others in a manner that suppresses their identity and autonomy.
What is the global impact on domestic wellness
We are not alone.
Public Health Nurses contributions include… surveillance.- Monitoring trends and identifying potential threats. Preparation, Respond- jump in to help.
Prevention, preparation for diseases though controlled efforts.
Vaccines. Education starting young.
Involving members of the community in Identifying problems. Assessing what the community needs. Partnerships help us determine what those are and whether or not they want an intervention.
What are upstream and downstream encounters in public health?
Upstream - system/ society and unhealthy circumstances. Mass. Can effect downstream- Workers who come to work sick instead of being sent home. Ex. Feeling like you need to test while being sick. Root cause.
Downstream – individual factors and personal choices. The individual can effect upstream. Ex. Worker comes to work sick and effects others. It impacts larger group. Ex. Can’t afford to not have a paycheck.
Downstream can affect upstream and upstream can affect downstream
Think of Healthy Communities – access to fresh food, walking paths, clinics for care, water and sanitation.
What is populations health vs public health?
Population health is society and the community, actions and interventions- know people
Public Health is more about ensuring conditions for good health – policies and government services and regulations, think larger societal level . Public health- just an agency.
In brief, population health nursing focuses on the health status and health outcomes of groups of people, while public/community health is a broad discipline that consists of organized efforts to develop, implement, evaluate, and revise policies and programs to support the well-being of all people. Public health extends beyond nursing; its principles provide the foundation for population health and for public health and community health nursing practice.
WHat are historical perspectives
Industrial Revolution – workers were injured- poor conditions.
Public health began and in the 20th century we evolved.
EPA – environmental protection agency- air quality standards. Difference of policies. (EPA), support public health through policies and regulations that enforce healthy air indoors.
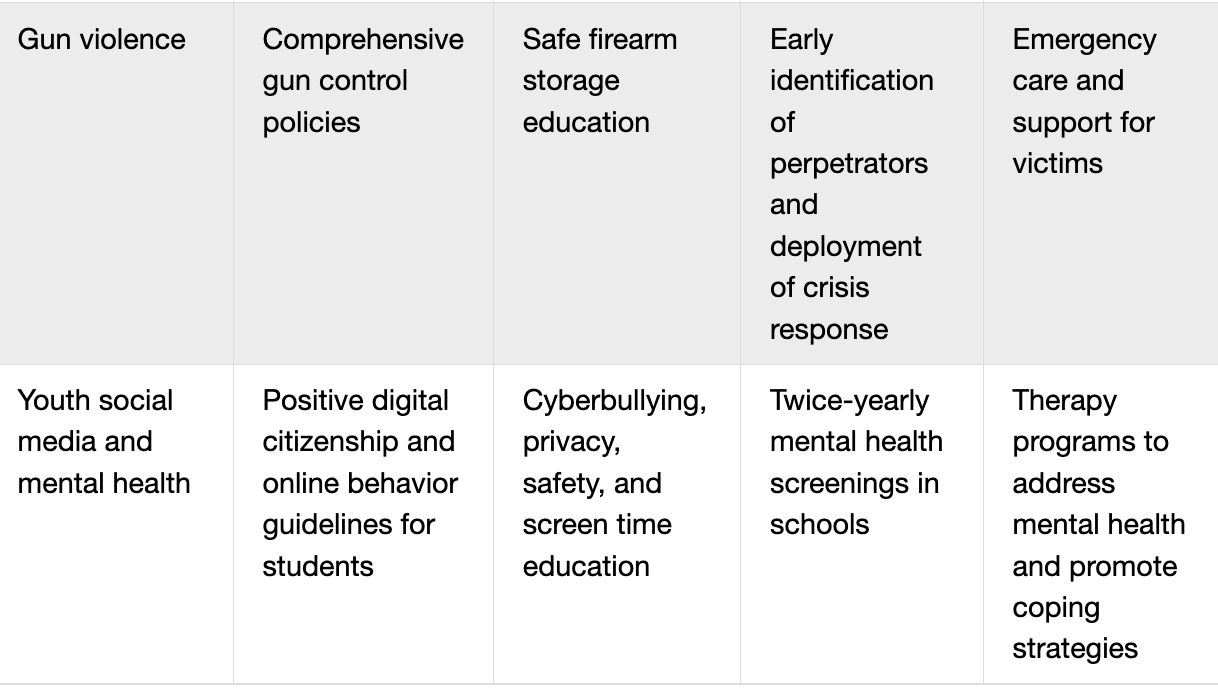
What are contemporary issues
Public health emergencies – national, state or local officials can declare these emergencies. Public health emergencies are illnesses or health conditions that pose a significant risk to communities that are either occurring or may imminently occur. For example, COVID-19 was a public health emergency.
Allows for awareness and funding.
Qualifiers for PHE:
1. Iminent- about to happen.
2. Significant risk to public
3. Require timely and comprehensive response
One of the tough things about these emergencies are the supplies and keeping them ready and available because everything we use expires.
Other types
Social media concerns, mental health,
Nurses get into all of this how? Identify and share accurate info, evidenced based info.
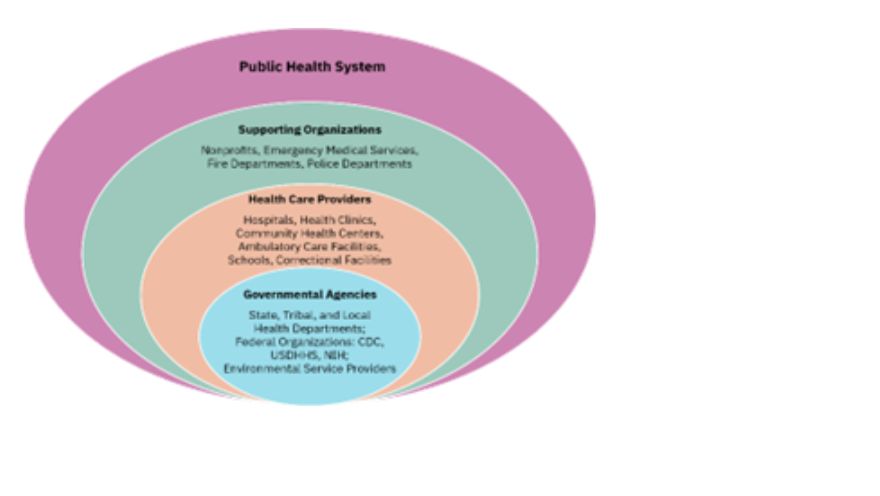
Figure 2.4 The U.S. public health system comprises many organizations at the national, state, and local levels. (attribution: Copyright Rice University, OpenStax, under CC BY 4.0 license)
What are the different levels?
CDC-
Federal level:- especially for surveillance and regulations for health practices, disease monitoring food preparation..
CDC
US Dept of Health and Human Services
NIH – national institute of health
FDA - all of these are federal
State level – collection of data from HCP, clinics, hospitals
Emergency preparedness- prevention.
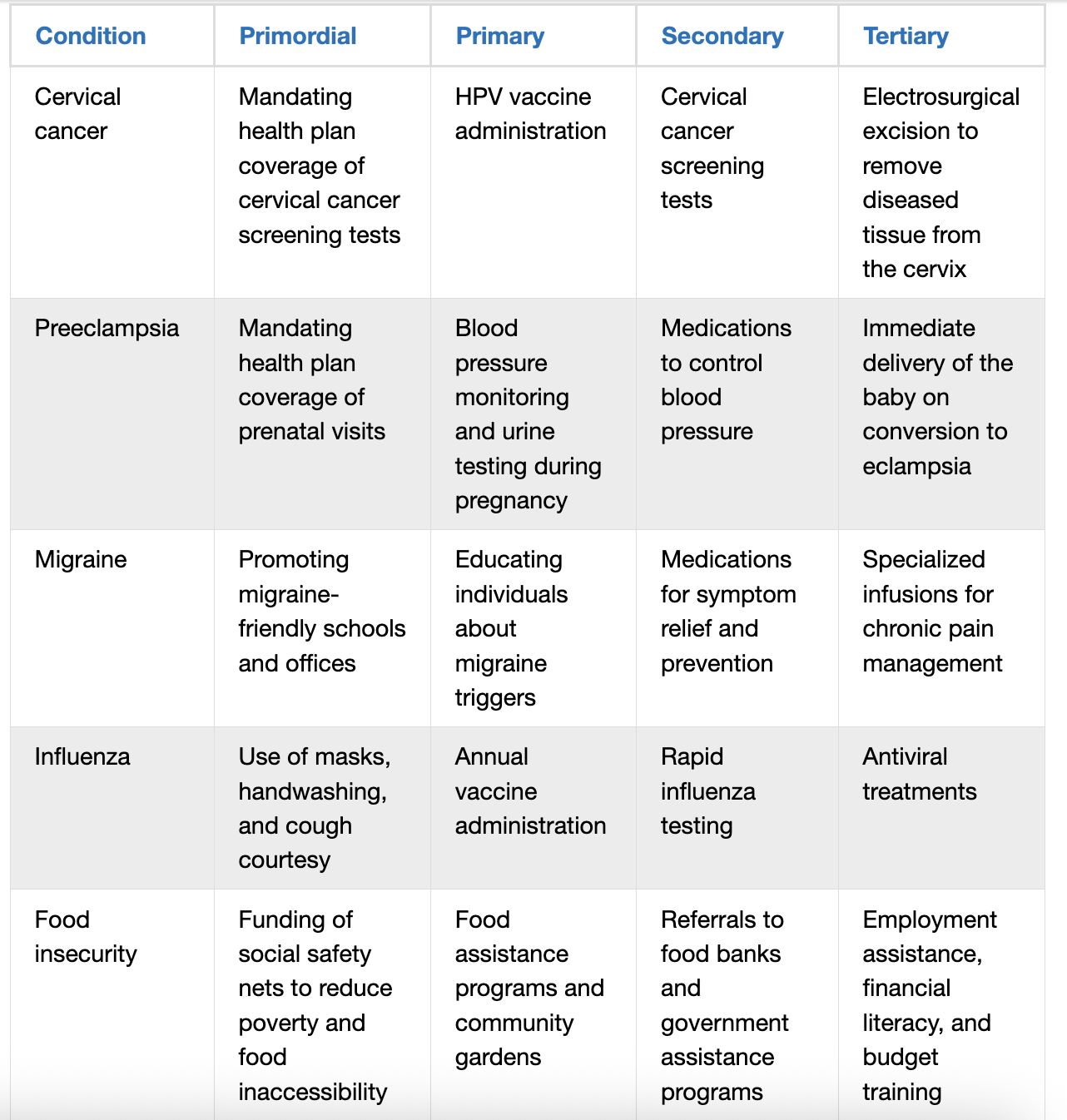
WHat are the levels of prevention
LEVELS OF PREVENTION
We are not going to 5…3 is enough! Look at Table 2.2 for some good examples!
NON-MALEFICENCE – think of examples
Primary- primoriol . Tartgeting risk groups, immunization, education programs
Secondary – Early disease detection- screening.
Tertiary- have it but lessen impact and prevent complications.
What are the PUBLIC/COMMUNITY HEALTH NURSING HISTORICAL PERSPECTIVES
In 1949 the National Organization of Public Health Nurses distinguished community health nursing from public health nursing. Community health nursing is caring for individuals and families with latest practices, while public health nursing is primarily concerned with population-based strategies.
Many historical events shaped public/community health nursing practice:
World War II—community health nurses contributed in WWII. In 50’s we got antibiotics. Beyond the care nurses provided to manage acute and chronic health conditions, they educated the public to raise awareness of health and health issues, prevent the spread of diseases, and promote vaccine uptake (the proportion of the population receiving a vaccination).
Legionnaires’ Disease— a national nonprofit group supporting military veterans held a convention. 1977). Investigations eventually identified a new deadly bacteria named Legionella pneumophilia. concerning level of harm because they could be aerosolized and spread via the air-conditioning system.
HIV and AIDS— Public/community health nurses provide education to prevent HIV transmission and to promote testing, treatment monitoring, and counseling as part of the ongoing efforts to combat HIV and AIDS globally.
COVID-19 Pandemic and Beyond—. One key role of public/community health nurses during the first 18 months of the pandemic was contact tracing and disease surveillance
Passage of ACA - health equity
Shortage of nurses- there has never been enough nurses.
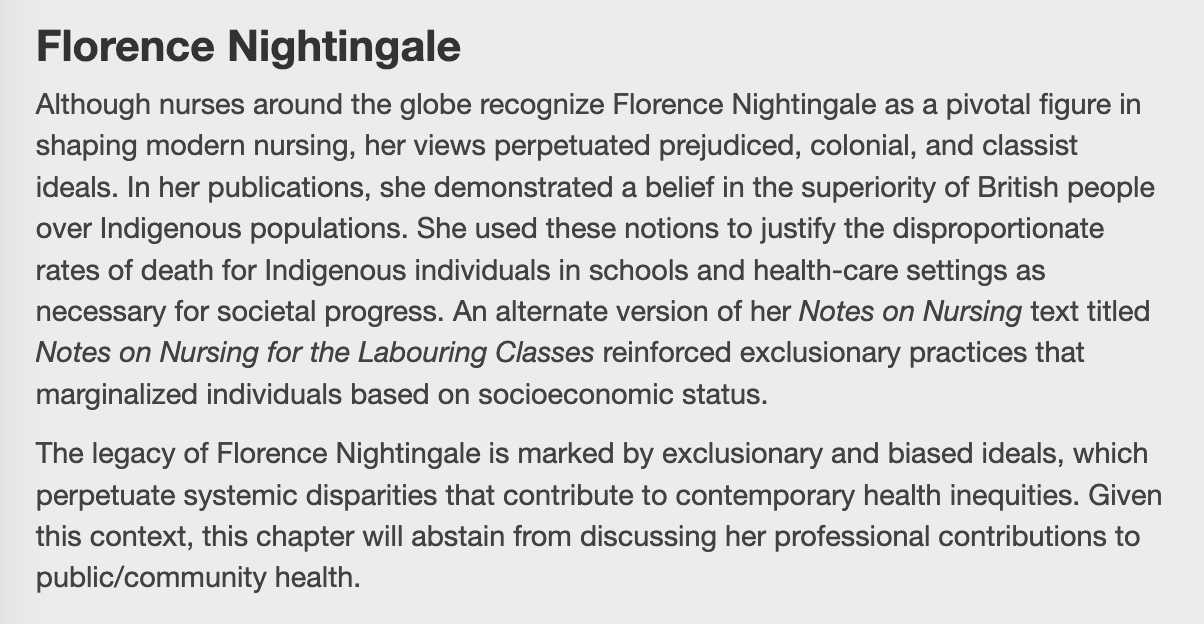
What are public health nurse leaders
Florence Nightingale— back then nurses were not well regarded. She came from a fancy family. Crimean war. Infection- cleaned the wars. Decreased mortality rate. It was disgusting in the hospitals. Infection control- advocate – she made a difference.
Harriet Tubman— ensalaved nurse- treated black soldiers during the civil war.
Lillian Ward— founder of modern public health. Helped sick people get resources in their homes food, cab fares, loans, childcare, cleaning, and job training. Went into the communities and took nurses into those communities.upstream interventions, She was a nurse dedicated to policy reforms to
What is the scope of practice and practice standards
Scope of Practice—refers to the professional activities involved in a particular role
Standards of Practice—principles and guidelines to which a professional must adhere
What are the nine core concepts of practice identifies by the ANA for public health nursing: guide us
Social determinants of health
Community collaboration
Population health
Ecological model of health: Micro- to macro-levels
Culturally congruent practice: Respectful, equitable, and inclusionary
Levels of prevention
Ethics
Social justice
Health equity (ANA, 2022)
Public/community health nurses need knowledge of
Epidemiology – hey study the "what, who, where, when, and why/how" of health events
Environmental health
Social determ of health
Social influences / statistics
Evidence based practice
Health promotion
Factors that impact health
Statistics- want data to be meaningful.
AND people skills – communication and relationship building
What is the interface of public health nursing care
Interface- a point where two systems, subjects, organizations, etc. meet and interact.
Public health and political care Can interact daily to support health across the populations
Connections / collaborations
Infectious disease response
What is THE ROLE AND SIGNIFICANCE OF THE COMMUNITY HEALTH NURSE
Health Promotion and Education— pts, families, on health topics
Social Prescribing— involves referrals to community resources other than those traditionally considered directly related to the health care setting.. Financial planning. also decrease utilization of formal health care services and
Community Assessments— Find out what community needs to determine health problems, health risks, and the need for teaching or other interventions. Community assessments can also reveal problems or areas of opportunity related to health equity.
Health Advocacy—Advocate for services and programming that the community needs to achieve health.
What is the disease and disaster response
prevent the spread of diseases by:
Immunizations
Screening for infections
Education on infection control
Disasters
Establishing response plans
6.coordiante and mobilize resources
7. Ensure resources needed to stay safe and healthy are available
What Does It Mean to be Healthy?
Ex. Someone who has asthma may see themselves as unhealthy.
Ex. Someone with a holistic view may see themselves as healthy even with a chronic condition.
Well-being: subjective perception that life is going well.
Health-related quality of life (HRQL): perceived physical and mental wellbeing of an individual or population.
Factors needed for attaining health:
1. Access to health care – health literacy and trust, able to get insurance
2. Safety – Environment and transportation
3. Healthy food and habits - from smoking or the harmful use of alcohol
4. Mental health/social supports- Mental health issues, such as depression, anxiety, and stress, have a negative effect on health.
HEALTH OUTCOMES
“A change in health status of an individual, group, or population tied to a particular intervention or series of interventions…” (WHO, 2021a, p. 20)
Look at broad outcomes related to the targeted population like mortality rates. Outcomes are metrics/ statistics- they have data with them. Performance metrics
What are performance metrics?
Health indicators: health-related measures of data referring to health status
Years of life lost (YLL)— A measure of premature mortality that considers both the frequency of death and the age at which it occurs,
Years of healthy life lost due to a disability (YLD)—
Disability-adjusted life years (DALYs)—. YLL and YLD combined
Quality-adjusted life years (QALYs)– The months or years of reasonable quality that an individual may gain following treatment; measures both length and quality of life of an individual
What are the measures of population health outcomes
have basic understanding
Life Expectancy at Birth— the average age of death.
Mortality –
Morbidity -
- know what they are
Prevalence measures the proportion of a population that has a disease or condition over time. Number that has it 56
burden of disease—the measure of both morbidity and mortality together, also seen in DALYs disability adjusted life years.
What is the THE NURSE’S ROLE IN MANAGING POPULATION HEALTH
Well positioned to identify patterns across populations
Nurses should understand basic health metrics, population health outcomes, and key health indicators
Nurses in community health in public health role work to improve health of the population at large
Tracking shifts in mortality guides public health policies and interventions.
Population health nurses must be familiar with disease trends
HEALTHY PEOPLE 2030
Within its core objectives, HP identifies some challenges.
What are the leading cause of death in the united states
Leading causes of death in the U.S. in 2021:
Heart disease
Cancer
COVID-19
Accidents (unintentional injuries)
Stroke (cerebrovascular diseases)
Chronic lower respiratory diseases
Alzheimer’s disease
Diabetes
Chronic liver disease and cirrhosis
Nephritis, nephrotic syndrome, and nephrosis
But what are the trends especially for these top items?
Rural health greater risk
Suicide rates are increasing.
Historically it was infectious diseases as cause of death, now it is chronic diseases.
Why?
What are Mortality trends in infectious disease
Infectious disease remains a public health threat in the U.S.
COVID-19 is still a leading cause of death in the U.S.
Americans of all ages at risk for mortality from other infectious diseases, such as bacterial sepsis in newborns or influenza and pneumonia for people from 1 year old through adulthood.
What are mortality trends in chronic disease
Chronic disease—condition present for more than 1 year and requires medical intervention and/or limits activities of daily living.
6 out of 10 Americans have 1 chronic disease, and 4 in 10 have 2 or more.
Major chronic diseases are heart disease and stroke, diabetes, and cancer.
Chronic disease accounts for most health care costs in the U.S.
What are Mortality Trends in Suicide and Drug Overdose
Suicide is death caused by self-directed injurious behavior with intent to die.
Rates increased by 37 percent between the years 2000 and 2018 and then decreased by 5 percent between 2018 and 2020.
Research says that increased suicide rates correlate to increases in mood and affective disorders and associated with alcohol and drug use.
Drug overdose can be intentional or unintentional.
U.S. currently in an opioid overdose epidemic.
What are Trends in Maternal-Newborn Mortality
Pregnancy-related deaths occur either during pregnancy or within a year after the end of pregnancy from a pregnancy-related complication.
Maternal mortality refers to deaths that occur while pregnant or within 42 days after the end of pregnancy from any cause aggregated by the pregnancy or its management.
Maternal mortality rate in the U.S. exceeds that of other high-income countries and is growing.
Infant mortality refers to an infant’s death before their first birthday, and the U.S. rate exceeds that of peer countries.
Infants born to Black people in the U.S. are at higher risk of mortality than those born to White people.
What are global health security risks?
Emergence and spread of new infectious diseases
Ability of diseases to spread related to increased globalization of travel and trade
Increasing drug-resistant, disease-causing pathogens
Risk of accidental release, theft, or unlawful use of dangerous pathogens
Global Health Security Agenda (GHSA) is an effort of more than 70 countries to protect the world from infectious disease threats (CDC, 2023f)
What are global public health security interventions
Surveillance Systems— allow countries to identify risks and quickly detect and stop outbreaks of infectious diseases. In the United States, the National Notifiable Diseases Surveillance System
Laboratory Systems— as they allow for the detection of pathogens that cause disease, outbreaks, and death. Reducing the spread of disease and death is possible when a pathogen is identified quickly, as confirmation allows health care workers to respond with the appropriate treatment and prevention methods efficiently. As with surveillance systems, limitations.
Emergency Management and Response— Countries must have knowledge and resources, such as emergency operations centers, to mount rapid, coordinated responses to infectious disease outbreaks.
Workforce Development— requires each country to have well-trained, highly skilled teams to investigate potential outbreaks and intervene quickly.
CDC has established the Field Epidemiology Training Program (FETP) to train “disease detectives.”
INTERCONNECTEDNESS OF POPULATION HEALTH ACROSS BOUNDARIES
Everyone is vulnerable to threats from infectious disease, which can spread nearly everywhere on Earth in as few as 36 hours
Monkeypox / Mpox
Ebola— Ebola is transmitted by infected animals, the body fluids of infected persons, or items from infected persons that are contaminated with body fluids, such as clothing. It enters the body through human-to-human transmission via contact through the eyes, nose, or mouth or an opening in the skin.a rare form of hemorrhagic fever Global health security interventions are imperative with a disease such as Ebola to contain the virus since transmission can occur even after the death of an individual, during burial practices
Tuberculosis- infectious diseas- Multidrug-resistant TB (MDR-TB) is a public health threat because it is resistant to many drugs and is easily transmitted from person to person. The WHO is providing global leadership to end TB and setting strategic priorities, including monitoring and reporting on the current global, regional, and country-level epidemic progress
Human Immunodeficiency Virus— that affects the body’s immune response. Contracting both HIV and TB is significant, as nearly all HIV-positive people with TB will die
What is the nurses role in public health security
Vital role with active participation
Writing, updating, reviewing, and exercising emergency response plans are key including collaboration
may be required to dispense vaccines, antimicrobials, and antitoxins or obtain other resources from HHS’s Strategic National Stockpile.
may assist in shelters, schools, or places with vulnerable populations.
may supply psychological support to victims, the public, and the workers who are responding to and working with bioterrorism event.