11 - Childhood hospitalization, illness
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
61 Terms
Adenosine
antiarrhythmic, temporarily blocks conduction through the AV node, restoring normal sinus rhythm. Used for treatment of supraventricular tachycardia. Brief sinus pause will be noted when the AV node resets, warn caregivers and patient.
Amiodarone
antiarrhythmic, prolongs repolarization of action potential, thus slowing heart rate. Used with ventricular tachycardia, ventricular fibrillation. Monitor for prolonged QT segments with infusion.
Atropine
anticholinergic, increases heart rate, dries secretions, inhibits serotonin and histamine. Used with sinus bradycardia, asystole, pulseless electrical activity (PEA). May only repeat dosage once.
Dobutamine
adrenergic agent, primarily affects B-1 receptors, increasing myocardial contractility and heart rate. Used for ongoing short-term management of shock (hypovolemic and cardiogenic). Monitor for development of ventricular arrhythmias
Dopamine
inotropic, increases cardiac output, BP, and renal perfusion. Used for the treatment of bradycardia, hypotension, and poor cardiac output. Administer through central line if possible due to risk of extraversion.
Epinephrine
vasopressor/inotropic, stimulates a & b-adrenergic receptors, increasing heart rate and systemic vascular resistance. Used to treat bradycardia, all cardiac arrests, and anaphylaxis. In arrest, repeat every 3 to 5 minutes.
Milrinone
inotropic, phosphodiesterase inhibitor. Used in low cardiac output and following cardiac surgery. Decreases pulmonary resistance. Used in infants with pulmonary hypertension not responsive to inhaled nitric oxide.
Lidocaine
antidysrhythmic. Decreases automaticity of conduction tissues in the heart. Used to treat ventricular arrhythmias. Can also decrease intracranial pressure at higher doses. Contraindicated in complete heart block.
Computed Tomography (CT)
Uses high radiation to target specific body parts. Superior test for the evaluation of internal bleeding.
Urinalysis
indicated for children with fever, dysuria, flank pain, urgency, hematuria, or trauma to provide information about urinary tract and renal contusion.

Anesthesia bag
small collapsible bag that contains reservoir bag, overflow port, and fresh gas inflow port. Used more commonly in the post anesthesia care and neonatal care unit

Bag-valve-mask
Self-inflating oxygen delivery bag that does not require and oxygen source for resuscitation and ventilation. Effective in providing oxygen to a child who is in severe respiratory distress or who has suffered a respiratory arrest.
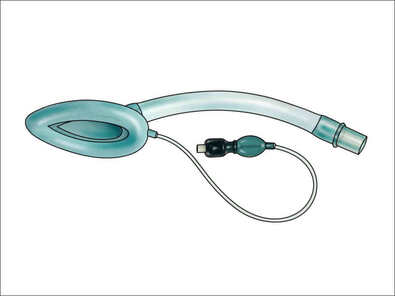
Laryngeal Mask Airway
inflatable silicone mask and rubber connecting tube that is inserted blindly into the airway, forming a seal. Usually used in the unconscious child who benefits from bag-valve-mask ventilation but does not require intubation.
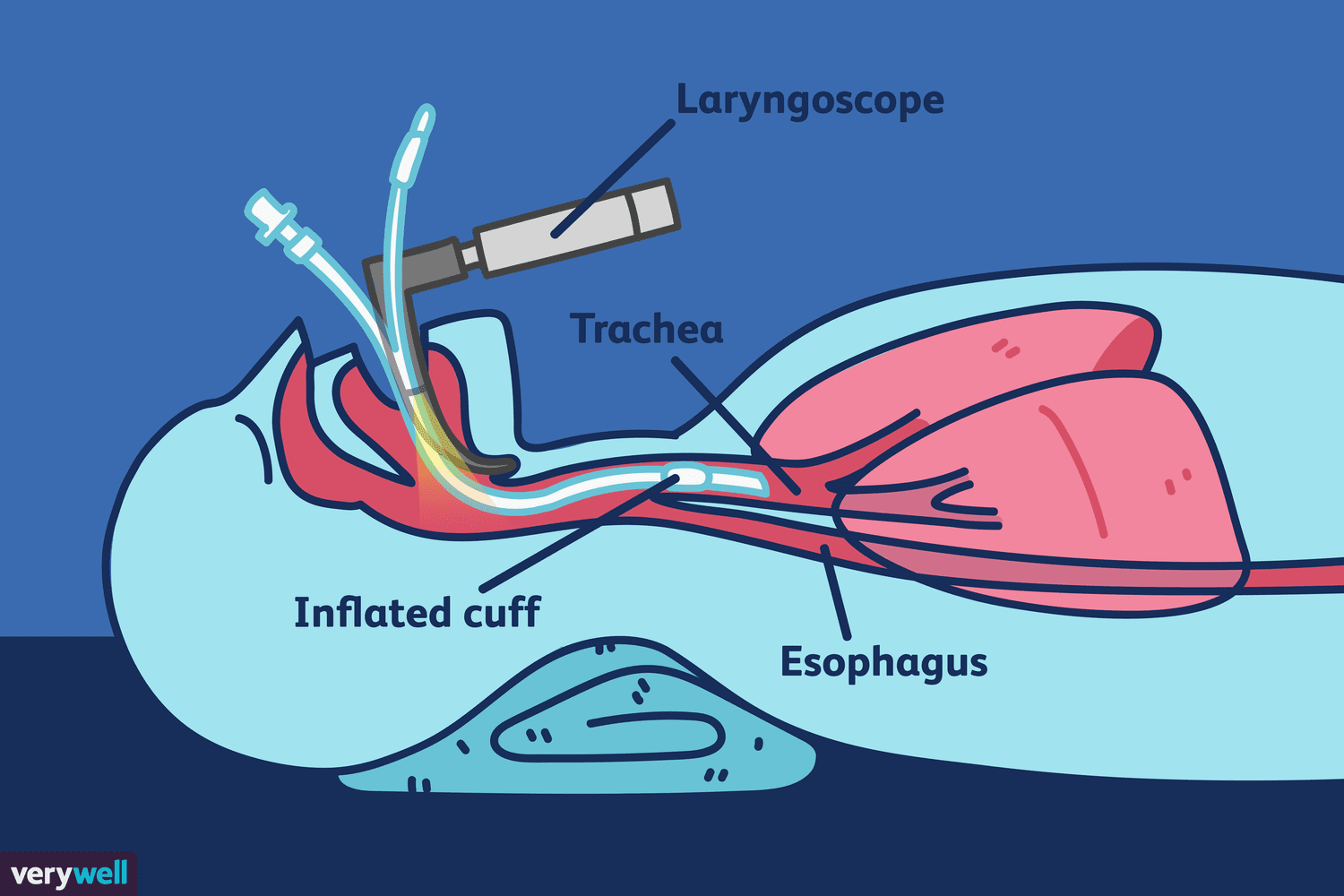
Tracheal Intubation
plastic tube inserted into the trachea to establish and maintain an airway when the airway cannot be maintained effectively using other measures. Skilled medical professional required for insertion.

Laryngoscope Blades
Straight (Miller) blades in young children and curved (Macintosh) in older children and adolescents. Lightbulb attached for visualization of the trachea.
Thiopental
Short-acting barbiturate used during intubation. Reduces intracranial pressure and oxygen demand. (Undesirable) hypotensive effects are more severe in dehydrated children. Potential for respiratory depression when given with narcotics
Midazolam
Benzodiazepine. Has slightly slower onset than thiopental but has fewer adverse effects. Lower doses cause conscious sedation, higher doses induce anesthesia.
Ketamine
anesthetic agent. Has rapid onset with sedative, amnesic, and analgesic effects. May improve BP and cause bronchodilation (helpful for children with status asthmaticus). Can cause increased intracranial pressure and should not be used for head injuries. Can caused hypertension, increased secretions, and hallucinations.
Paralyzing or Neuromuscular Blocking Agents
Include Rocuronium, Succinylcholine, Vecuronium. Used for short-term paralysis during intubation process. May be used for extended paralysis in ICU for children whom movement would be detrimental. Succinylcholine is go-to due to rapid onset and short-acting.
Septic Shock
related to a systemic inflammatory response in which there may be increased blood CO with low systemic vascular resistance (SVR) known as warm shock. More commonly in children, decrease in CO with increase in SVR known as cold shock.
Cardiogenic Shock
results from ineffective pumping of the heart with a resultant decrease in stroke volume. Children with structural heart disease at greater risk.
Distributive Shock
the result of a loss in the systemic vascular resistance. Relative hypovolemia occurs, most often with neurogenic injury-related shock and anaphylaxis. This causes the vascular compartment to expand due to systemic vasodilation. Results in larger vasculature requiring more fluid to maintain CO despite no actual fluid loss.
Moderate sedation
Used to label conscious sedation, but the term “conscious” had been replaced since it can be misleading. Medically controlled state of depressed consciousness that allows the protective reflexes to be maintained so the child has the ability to maintain a patent airway and respond to physical or verbal stimulation.
Moderate sedation
Uses: procedures that are painful and stressful. Suggested instead of restraints, especially for toddlers and preschool children undergoing frightening/invasive procedures and are manifesting extreme anxiety and behavioral upset. Additionally:
• Evidence that the child is experiencing a heightened stress reaction (e.g., attempting to flee, crying inconsolably, or flailing)
• Verbalization by the child that he or she is frightened and does not want to be touched
• Inability to remain immobilized, such as during laceration repair or computed tomography
• Any procedure that is painful and fear-provoking
Acetaminophen
Analgesic/antipyretic. Direct action on hypothalamic heat-regulating center/ inhibition of cyclooxygenase in CNS. Used for mild-moderate pain, fever, arthritis, musculoskeletal pain, headache.
Ibuprofen
Analgesic/antipyretic. Inhibition of prostaglandin synthesis. Used for mild/moderate pain, fever, treatment of inflammatory diseases. Do not give to babies.
High Humidity
used for common cold, tonsillectomy to avoid mucosal injury. Infant may require extra blankets with cool mist, and frequent changes of bedclothes as they may become damp.
Saline Lavage
Normal saline introduced into the airway followed by suctioning. Very helpful for loosening thick mucus. Child may need to be in upright position to prevent aspiration.
Chest Tube
Insertion of a drainage tube into the pleural cavity to facilitate removal of air or fluid and allow full lung expansion.
Cough and Cold Medications
Used for systemic relief of mucus build-up, cough, and congestion. Effectiveness of most has not been established in children, and most have the potential for harm. Should not be given to children under the age of 6.
B2-Adrenergic Agonists
Relax airway smooth muscle, resulting in bronchodilation. Used for acute and chronic treatment of wheezing and bronchospasm in asthma.
Nebulized L-epinephrine
Provides bronchodilation and is indicated for croup. Observe for rebound bronchospasm after administration.
Anticholinergic
Produce bronchodilation in asthma or chronic lung disease. Example ipratropium. In children, generally used as an adjunct to B2-adrenergic agonists for treatment of acute bronchospasm.
Corticosteroids
suppress inflammation and normal immune response. Used for acute asthma exacerbations, wheezing, croup, etc.
Leukotriene Receptor Antagonists
Decrease inflammatory response by antagonizing the effects of leukotrienes to control asthma in children age 1 and older. Montelukast: for allergic rhinitis in children six months and older. Not for relief of acute wheezing episode.
Respiratory Stimulants
Provide continuous airway relaxation to achieve long-term control (methylxanthines).
Inhaled Pulmonary Enzyme
Enzyme that hydrolyzes the DNA in sputum, reducing sputum viscosity in children with cystic fibrosis
Monoclonal Antibody
Used to prevent serious lower respiratory syncytial virus (RSV) disease in certain high-risk groups of children.
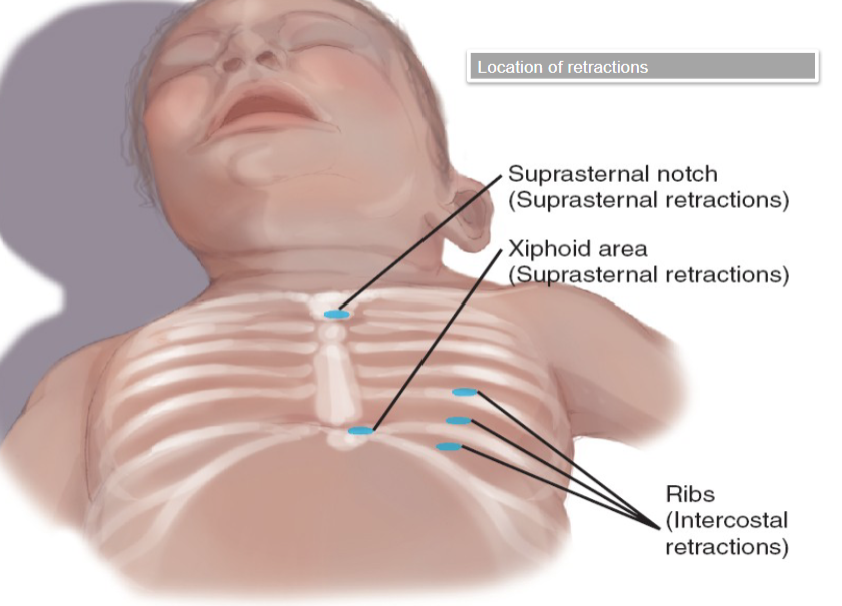
Retraction
term for the areas that sink when a person with asthma tries to inhale. I.e. a sign that someone is working hard to breathe. In children, this includes suprasternal notch, xiphoid area, and ribs.
Brain and Spinal Cord
• Development occurs within the first 3-4 weeks of life from the neural tube.
• Malformations caused by infection, teratogens and malnutrition.
• Premature infants at risk.
• Sutures and fontanelles are for flexible brain growth.
• Brain is well protected but highly vulnerable to pressure that may accumulate within the enclosure.
Rapid Acting
Aspart, lispro, glulisine. Onset within 15 mins, peaks at 30-90 mins
Short Acting
Regular. Onset 30-60 mins, peak 2-4 hours
Intermediate Acting
NPH (Humalin N, Novalin N). Onset 1-3 hours, peaks 4-10 hours
Long Acting
Glargine (Lantus), Detemir (Levemir). Onset of 1-2 hours, and no clear peak.
Epilepsy
Seizures are triggered recurrently from the brain. Commonly discovered in childhood. Diagnosed by 2 or more unprovoked seizures that occur more than 24 hours apart. Approximately 30% of people with first afebrile seizure will later be diagnosed with epilepsy. Can be partial or generalized and simple or complex.
Epilepsy
Therapeutic Management: Focus on controlling the seizures and reducing the frequency.
• Use of anticonvulsants
• Surgery
• Ketogenic diet, placement of vagal nerve stimulator
Febrile Seizures
Most common type of seizure seen in childhood. More common in boys and children less than 5 years. Associated with a fever (39C or higher) and usually related to viral illness. Generalized tonic-clonic seizure lasting a few seconds to 10 minutes. May indicate serious underlying infectious disease (i.e. meningitis, sepsis) with LP performed to rule this out.
Febrile Seizures
Therapeutic Management: determine the cause of fever and control it.
• Anticonvulsants are not recommended
• Rectal diazepam or lorazepam can be safe in terminating seizure
Bacterial Meningitis
Infection of the meninges. Very dangerous, leading to brain damage, nerve damage, deafness, stroke, and death. Requires rapid detection and treatment. Caused by gram-negative bacteria in newborns. Meningococcal outbreaks in Canada are caused almost exclusively by Neisseria meningitdis.
Bacterial Meningitis
Pathophysiology: causes inflammation, swelling, purulent exudates and tissue damage to the brain. It can occur as a secondary infection (URI, sinus infection, ear infection) or as a result of direct introduction though LP (skull fracture, severe head injury, neuro surgery, neural tube defects, VP shunt, cochlear implant).
Bacterial Meningitis
Clinical Manifestations: Fever, headache, irritability, N&V, photophobia, stiff neck, rash, drowsiness, lethargy, muscle rigidity, seizures
Bacterial Meningitis
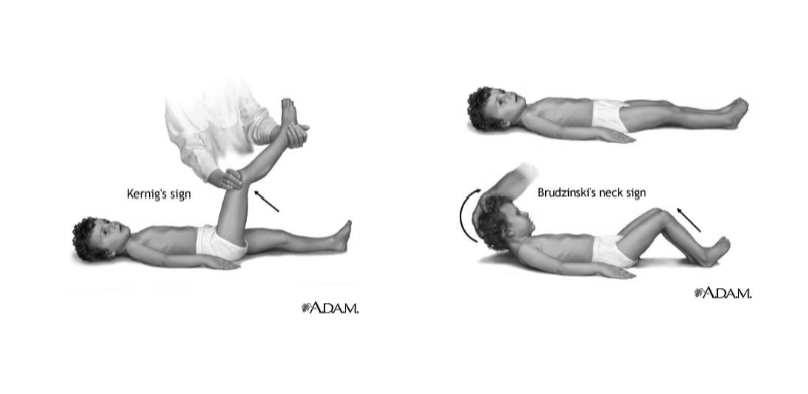
Physical Examination: opisthotonic position, positive Kerning’s and Brudzinski’s signs – indicate irritation of the meninges.
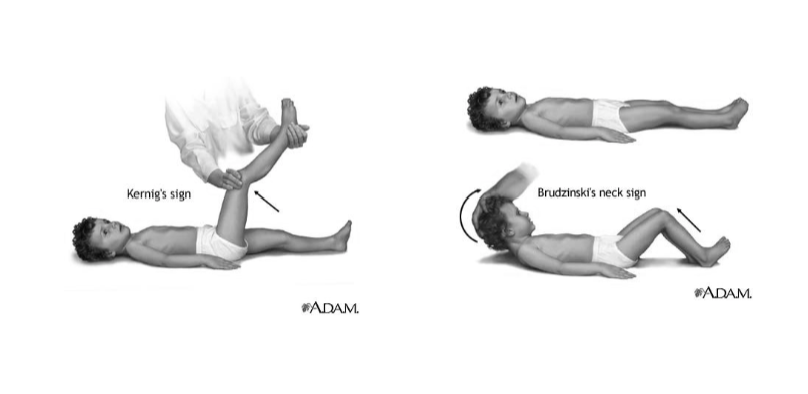
Kernig’s and Brudzinski’s Signs
The patient lies on their back with their hips flexed to 90°. The test is positive if the patient experiences pain or is unable to extend their knee when it's passively extended. The patient lies on their back with their neck passively flexed. The test is positive if the patient's hips and knees flex involuntarily.
Neural Tube Defects
Neural tube closes between the 3rd and 4th weeks in utero, the anomaly can form at that point.
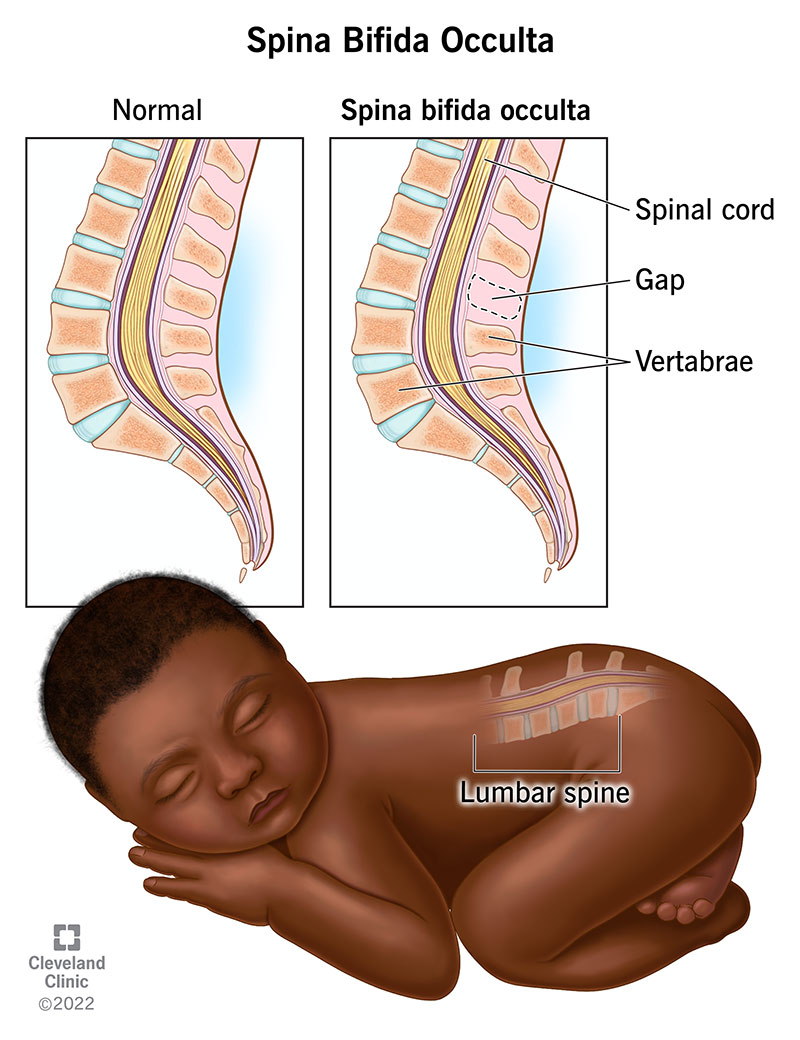
Spina Bifida Occulta
defect of the vertebral bodies without protrusion of the spinal cord or meninges. Often not visible externally and often produces no neurological signs.
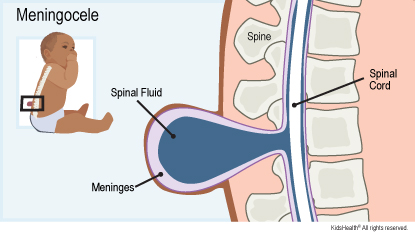
Meningocele
occurs when the meninges herniate through a defect in the vertebrae. The spinal cord is usually normal and there are typically no associated neurological deficits. Involves surgical correction of the lesions.
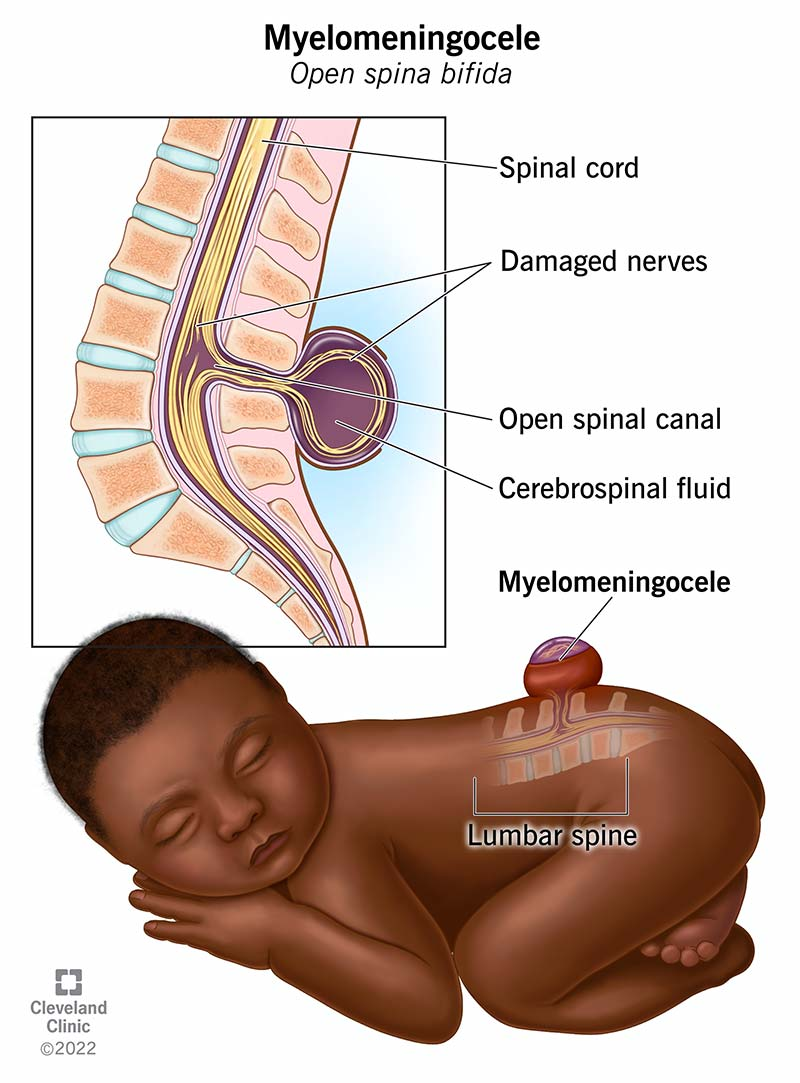
Myelomeningocele
the most severe form of neural tube defect, diagnosed by ultrasound or otherwise visible at birth. The spinal cord often ends at the point of the defect, resulting in absent motor and sensory function. There can be paralysis, bladder and bowel incontinence, neurogenic bladder.

Anencephaly
defect in the brain development resulting in small or missing brain hemispheres, skull, or scalp. Occurs when the cephalic or upper end of the neural tube fails to close. Born without forebrain and a cerebrum: incompatible with life.
Hydrocephalus
Not a specific disease – results from an underlying brain disorder. Results from unbalanced production and absorption of CSF. Classified as obstructive or non-communicating vs. nonobstructive or communicating. Increased risk of developmental disability, visual problems, and in memory, reduced cognitive function.
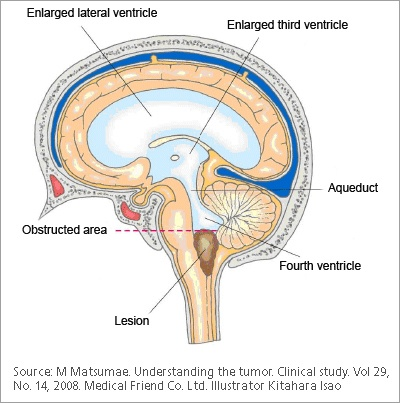
Obstructive Hydrocephalus
flow of CSF is blocked by the brain’s ventricles and cannot move between ventricles. (Non-communicating).
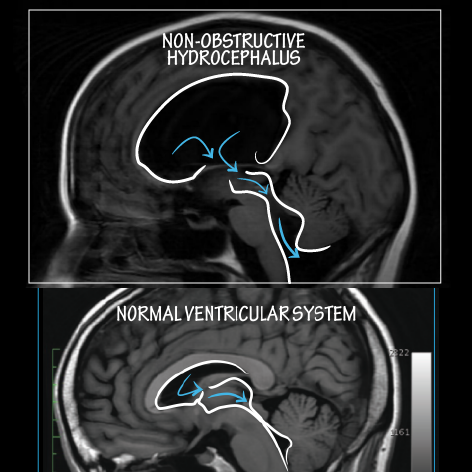
Non-Obstructive Hydrocephalus
flow of CSF is not blocked by brain’s ventricles and can still flow between ventricles (communicating).