Unit 3 Depression
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
87 Terms
What are the criteria to be diagnosed with depression?
Five or more of the following symptoms must be present during the same 2 week period and it must represent a change in functioning: either (1) depressed mood or (2) loss of interest or pleasure (anhedonia)
One of the five symptoms has to be depressed mood or loss of interest or pleasure
What are the symptoms of depression?
Depressed mood
Decreased interest or pleasure
Weight loss or weight gain
Insomnia or hypersomnia
Psychomotor agitation or retardation
Fatigue/loss of energy
Worthlessness or guilt
Decreased concentration
Suicidal ideation or attempt
How do the symptoms affect you?
impairment in functioning
not attributable to a substance or other medical condition (hypothyroidism)
no manic (mood is elevated) or hypomanic episodes
What are the signs and symptoms of depression?
SIG E CAPS
Sleep (insomnia or hypersomnia)
Interest (decrease in interest in things that one used to enjoy)
Guilt (guilt in things that you have no control over)
Energy (decreased)
Concentration/constipation (ability to concentrate is decreased; constipation)
Appetite (decreased or increased)
Psychomotor agitation or depression (agitated or slowed down)
Suicide/Sex (increased thinking about suicide/decreased interest in sex)
What are physical symptoms associated with depression?
Sleep problems
Fatigue/exhaustion
Chest pain
Aching muscles and joints
Digestive problems
Headaches
Back pain
Changes in weight/appetite
Sexual dysfunction
Appetite is decreased and insomnia - what type of depression?
typical depression
Hypersomnia (sleeping too much) and eating too much - What type of depression?
atypical depression
What can depression result from?
Life stressors can often lead to depression
Medical conditions
Being postpartum
Medications side effects
Chronic mental disorders
Intoxication/withdrawal from drugs/alcohol
Premenstrual hormone changes
Lack of bright light
Care-giving
What medical conditions are associated with depression?
Hypothyroidism
Diabetes (84%)
Chronic pain (15-100%)
Heart disease (40-65%)
Cancer (one in four)
Multiple sclerosis (40%)
Parkinson's disease (40%)
Coronary artery disease - no heart attack (18-20%)
Stroke (10-27%)
What medications are associated with depression?
anticonvulsants (benzodiazepines)
antihypertensives (beta blockers)
hormones (contraceptives and steroids)
others (alcohol, isotretinoin, varenicline)
What are the risk factors associated with depression?
Unemployment
Low income
Comorbid disorders
Physical disability
Widowed, separated, divorced
Middle aged (45-65 years)
Inheriting depression
Life stressors
Females
Native Americans
What are the risk factors for suicide?
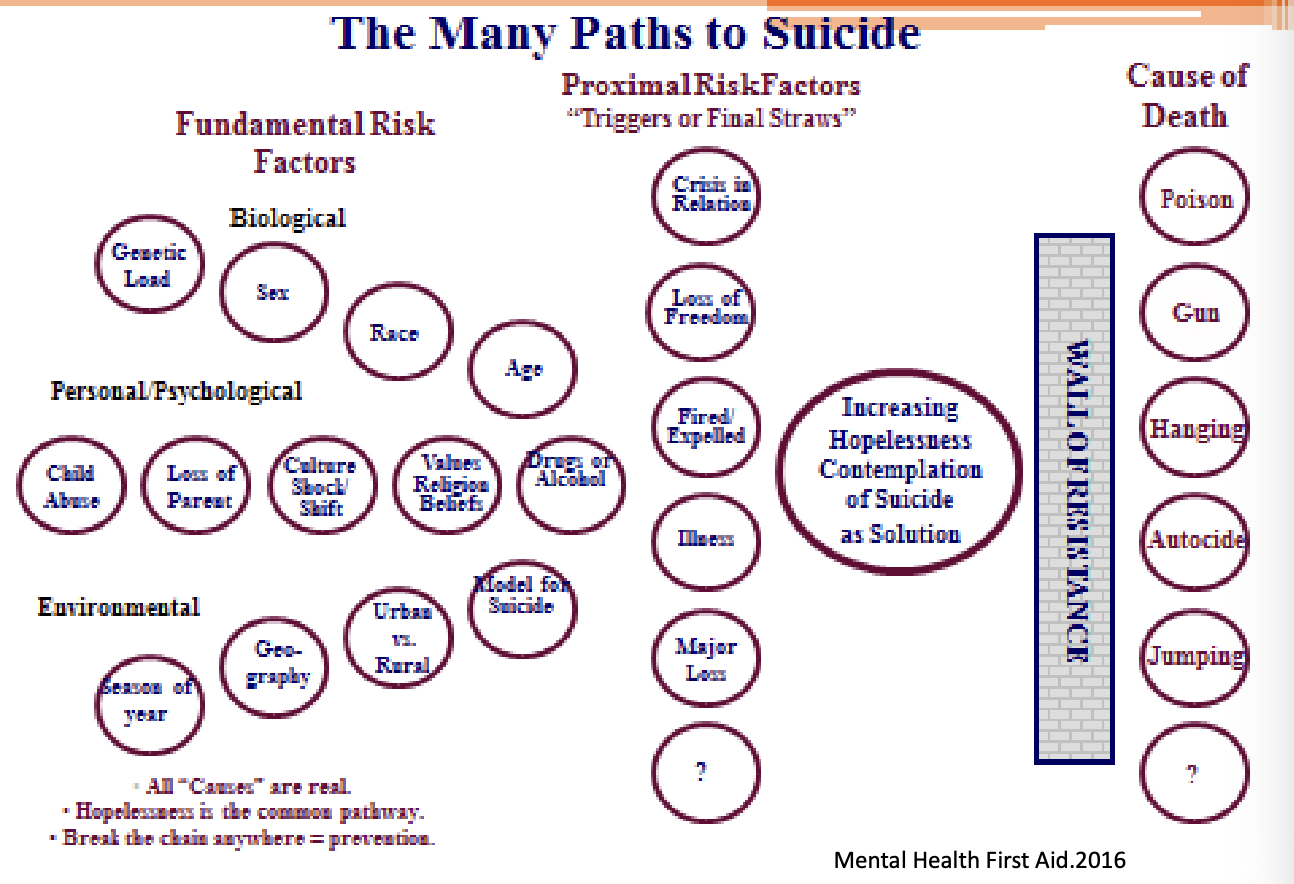
What are the warning signs for suicide?
Threatening to hurt or kill himself or herself
Looking for ways to kill himself/herself, seeking access to pills, weapons, or other means
Talking/writing about death, dying, or suicide
Expressing hopelessness
Feeling rage or anger, seeking revenge
Acting recklessly or engaging in risky activities, seemingly without thinking
Feeling trapped
Increase alcohol or drug use
Experiencing anxiety or agitation
Undergoing dramatic changes in mood
Feeling no reason for living; no sense of purpose in life
What are the treatment phases of depression?
Acute phase 6-12 weeks
Continuation phase 4-9 months
Maintenance phase >/= 1 year
What is response?
Decline in depression symptoms by at least 50%
What is remission?
Resolution of current symptoms
What is relapse?
Return of symptoms prior to 12 months
What is recovery?
You can say someone is recovered when they have resolution of symptoms at >/= 1 year
What is recurrence?
Return of symptoms after 12 months
What is the median time between the onset of symptoms and recovery (no symptoms) with adequate treatment (antidepressant)?
20 weeks
How long can untreated episodes of depression last without treatment?
6 months or longer
Are all antidepressants equally effective? What is the efficacy of antidepressants?
yes; choose an antidepressant for an individual based on the ADRs
How long does it take for antidepressants work?
4-6 weeks sometimes 8 weeks
How many patients don’t achieve remission with their first antidepressant?
two-thirds
What is treatment resistance?
A depressive episode that has failed to respond to two separate trials of different antidepressants of adequate dose and duration
What percentage of patients do not experience sufficient antidepressant response?
46%
How to determine an initial choice of antidepressant during the acute phase (first 6-12 weeks)?
Patient preference
Prior treatment response
Safety
Tolerability and adverse effects
Comorbid disorder
Potential drug-drug interactions
Pharmacokinetic parameters
Cost
Treatment moves from the acute phase to continuation phase with clinically significant improvement in symptoms, preferably complete remission of symptoms
What is the continuation phase during months 4-9?
Antidepressant treatment should continue at the same dosage as required int the acute phase for an additional 4-9 months
Risk of relapse ranges from 20-85% without continuation of treatment
Should depressive symptoms recur, potential causes of relapse should be addressed (poor treatment adherence, substance use, and psychosocial stressors)
What is the maintenance phase (treatment after 1 year, indefinite length)?
Maintenance antidepressant treatment is recommended for patients with chronic depressive symptoms or with a history of 3 or more depressive episodes
Duration of therapy is indefinite and may be lifelong
Other factors to consider for maintenance treatment
Presence of residual depressive symptoms
Psychosocial stressors
Family history
Severity of depressive episodes
Early age at onset
Elderly
When a patient has 3 or more depressive episodes, what length of therapy?
continue on indefinite therapy and may be lifelong (maintenance treatment)
What is goal of treatment?
remission or the absence of depressive symptoms
What are the drugs class of antidepressants?
selective serotonin reuptake inhibitors (SSRIs)
serotonin norepinephrine reuptake inhibitors (SNRIs)
tricyclic antidepressants (TCAs)
monoamine oxidase inhibitors (MAOIs)
norepinephrine and dopamine reuptake inhibitor (NDRI)
serotonin and alpha 2-adrenergic antagonist (NaSSAs)
serotonin antagonists and reuptake inhibitors (SARIs)
serotonin modulators
5HT1A agonists
neuroactive steroids
NMDA receptor antagonists
Which class of antidepressants causes hypertriglyceridemia?
NaSSAs (serotonin and alpha 2-adrenergic antagonist)
Which antidepressant class is the most dangerous when it comes to overdose?
TCA overdose
toxicity 2 to 6 hours
CNS depression
hypotension
seizures
anticholinergic toxicity
orthostatic hypotension
QT prolongation
How do you monitor for the efficacy of antidepressants?
Patient's response to treatment
functional status/quality of life
degree of danger to self or others
Signs of "switch" to mania
Other mental disorders
General medical conditions
Side effects of treatment
Adherence to treatment plan
rating scale (PHQ9)
monitoring should be conducted weekly or biweekly for the first 8 weeks
adherence
tolerability/side effects
depressive symptoms
What are the guidelines for depression?
Mild to moderate depression: doesn't always need therapy
St. John's Wort (first line) treats depression or psychotherapy
Moderate to severe depression
Use an antidepressant with or without psychotherapy
Severe depression
Drug plus psychotherapy
ECT (about 80% effective)
What are first line medications for depression?
SSRI's are considered first line, but most guidelines recommend if someone can't take an SSRI or if they fail two SSRIs they can use an SNRI, an NDRI, or an NaSSA first line
The reason these are considered first line is because of overall low side effects and safety
What ADRs do all antidepressants have? (3 most common ADRs for all antidepressants)
Suicide thinking
Mania
Discontinuation syndrome (feel flu-like)
What are additional adverse effects to know?
Hypertension: SNRIs and NDRIs can potentially cause elevated BP due to their noradrenergic activity
Discontinuation syndrome: SSRIs and SNRIs and potentially shorter acting antidepressants cause discontinuation syndrome which makes individuals feel like they have the flu. They may also feel dizzy, off-balance, and some complain of feeling electrical "zaps" in their brain
Serotonergic drugs (SSRIs, SNRIs, and serotonin modulators) have the potential to cause bleeding.
The above along with TCAs can cause low sodium levels (hyponatremia), which can lead to seizures
What are drug-food interactions?
Aged cheeses
Cured meats
Pickled or fermented food
Yeast extract
Alcoholic beverages
MOA for Selective Serotonin Reuptake Inhibitors (SSRIs)
MOA: Selectively inhibit presynaptic serotonin transporters, increasing synaptic levels of serotonin

side effects of SSRIs
anxiety/nervousness*, insomnia*, nausea*, headache*, serotonin syndrome, sexual dysfunction
Labeled and off-label indication for SSRIs?
depression, generalized anxiety disorder (GAD), social phobia, obsessive compulsive disorder (OCD), panic disorder, post-traumatic stress disorder (PTSD), hot flashes, premature ejaculation
MOA for serotonin norepinephrine reuptake inhibitors (SNRIs)
Selectively inhibit presynaptic serotonin and norepinephrine transporters, increasing synaptic levels of serotonin and norepinephrine
side effects of SNRIs?
anxiety/nervousness*, insomnia*, nausea*, headache*, hypertension, serotonin syndrome, sexual dysfunction
Labeled and off-label indication for SNRIs?
depression, generalized anxiety disorder (GAD), social phobia, panic disorder, diabetic neuropathy, fibromyalgia, hot flashes, urinary incontinence
MOA for Tricyclic Antidepressants (TCAs)
Inhibit presynaptic serotonin and norepinephrine transporters, increasing synaptic levels of serotonin and norepinephrine
not first line because of so many side effects
used for insomnia because side effect is sedation
labeled and off label indications for TCAs?
depression, anxiety, social phobia, panic disorder, diabetic neuropathy, fibromyalgia, obsessive compulsive disorder (OCD), insomnia
ADRs for TCAs?
sedation*, seizures, anticholinergic effects*, orthostatic hypotension, weight gain, sexual dysfunction
Off target antagonism for TCAs?
Off-target Antagonism | Effect |
Histamine ex: Benadryl | sedation, weight gain (appetite regulation) |
Muscarinic parasympathetic NS | blurred vision (can’t see), xerostomia (can’t spit), urinary retention (can’t pee*), constipation (can’t poop) |
α1-adrenergic constriction of blood vessels when activated | orthostatic hypotension, dizziness |
Na+ and K+ channels# TCAs like class I and II antiarrhythmic drugs | arrythmias, death |
off label use for urinary incontinence
MOA for monoamine oxidase inhibitors (MAOIs)?
Irreversibly# (binds irreversibly which gets rid of the enzyme entirely) inhibit monoamine oxidase MAO enzymes responsible for breaking down monoamines, increasing neuronal levels of serotonin, norepinephrine, and dopamine
After NE or 5-HT is taken back into the presynapse, it can either be degraded by MAO or repackaged into vesicles. By blocking degradation with an MAO inhibitor, more is repackaged and released into the synapse upon an action potential.
labeled and off-label indications for MAOIs)?
depression, Parkinson disease
*rasagiline only indicated for PD
ADRs for MAOIs?
orthostatic hypotension*, anticholinergic effects*, hypertensive crisis, serotonin syndrome, sexual dysfunction, weight gain, sleep disturbances (sedation/insomnia)*
MAO-A vs MAO-B?
Two subtypes, A and B,
A breaks down 5HT, NE, DA and Tyramine
B breaks down DA and Tyramine
A is found in the gut while B is not
MOA for Norepinephrine Dopamine Reuptake Inhibitor (NDRI)?
Inhibits presynaptic norepinephrine and dopamine reuptake, increasing synaptic levels of norepinephrine and dopamine
example: bupropion (Wellbutrin)
Labeled and off-label indications for NDRI?
depression, seasonal affective disorder (SAD), tobacco cessation, ADHD
ADRs for NDRI?
weight loss*, seizure activity, insomnia*
do not give drug in patient with seizures
When switching to an MAOI how long would you need to wait?
5 half-lives
fluoxetine has a half-life of 1-4 days so might take 2 weeks before starting the MAO
How long would you have to wait to switch from an MAOI?
wait 14 days to synthesize more MAO
enzymes are inhibited irreversibly so we have to make more enzymes to return to normal function
too much serotonin can cause hypertensive crisis or serotonin syndrome
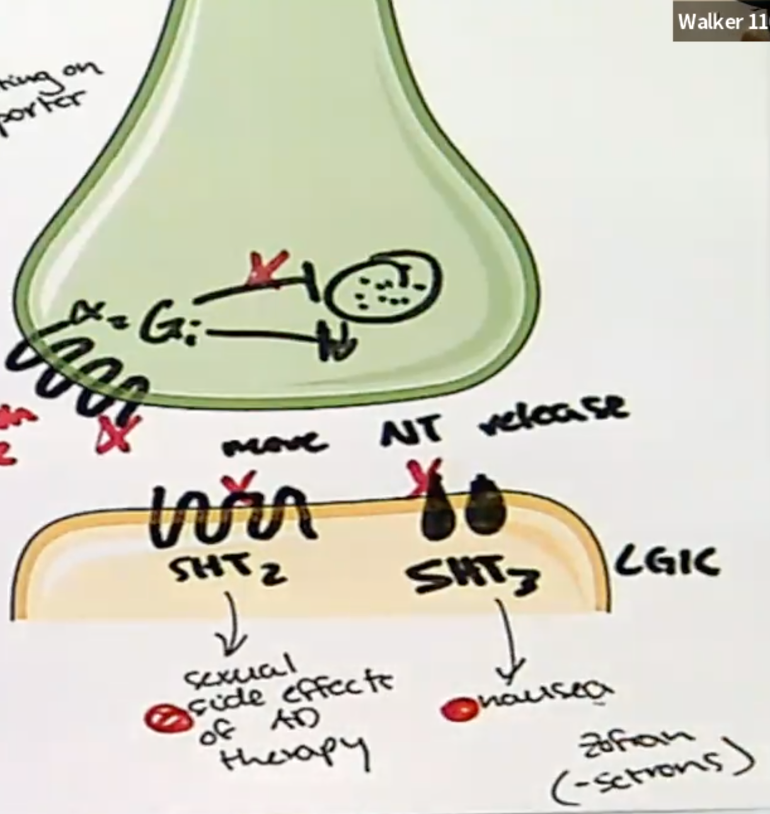
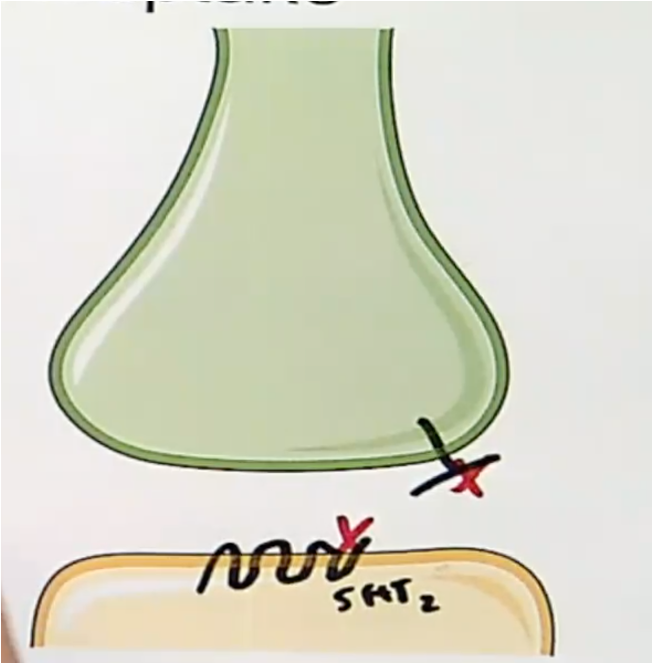
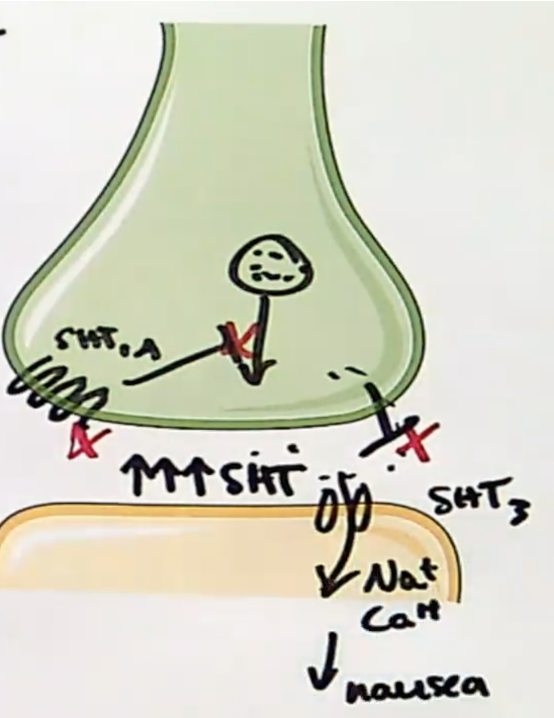
MOA for noradrenergic and specific serotonergic antidepressant (NaSSA)?
Inhibits presynaptic α2 autoreceptors as well as postsynaptic 5HT2 and 5HT3, increasing release of norepinephrine and serotonin into the synapse
labeled and off-label indications for NaSSA)?
depression, chronic tension headache prophylaxis, panic disorder
ADRs for NaSSA?
weight gain*, sedation*, hypertriglyceridemia
don’t see a lot of sexual dysfunction and nausea because of the blockage of 5HT2 and 5HT3
sedation can be beneficial in patients with insomnia (histamine related)
weight gain is histamine related
MOA for serotonin antagonist and reuptake inhibitors (SARIs)?
Inhibits reuptake of serotonin presynaptically and acts as an antagonist at postsynaptic 5HT2 receptors
Trazodone often used for insomnia
orthostatic hypotension is due to anti-alpha 1
labeled and off-label indication for SARIs?
depression, insomnia, alcohol dependence, generalized anxiety disorder (GAD), panic disorder
ADRs for SARIs?
sedation*, liver toxicity, orthostatic hypotension*, priapism, serotonin syndrome
MOA for serotonin modulators?
Selectively inhibits presynaptic reuptake of serotonin and acts as a partial agonist/antagonist at presynaptic 5HT1A autoreceptors
labeled indication of serotonin modulators?
depression
ADRs for serotonin modulators?
anxiety/nervousness*, insomnia*, nausea*, headache*, serotonin syndrome
lots of nausea because the 5HT binds postsynaptic 5-HT3
more risk of serotonin syndrome
MOA for NMDAR antagonist?
Inhibits extrasynaptic NMDA receptors, leading to preferential glutamate signaling at the synapse and enhanced action of brain-derived neurotrophic factor (BDNF)
ketamine (controlled substance with high abuse potential; administered under clinical supervision
improvement is immediate

labeled indication for NMDAR antagonist?
depression*, major depressive disorder with suicidality*, agitation, analgesia, general anesthesia, procedural sedation, rapid sequence intubation (RSI), status epilepticus
*esketamine only indicated for treatment resistant depression and MDD with suicidality
ADRs for NMDAR antagonist?
sedation*, nausea/vomiting*, dissociation*, hypertension, cognitive and motor impairment
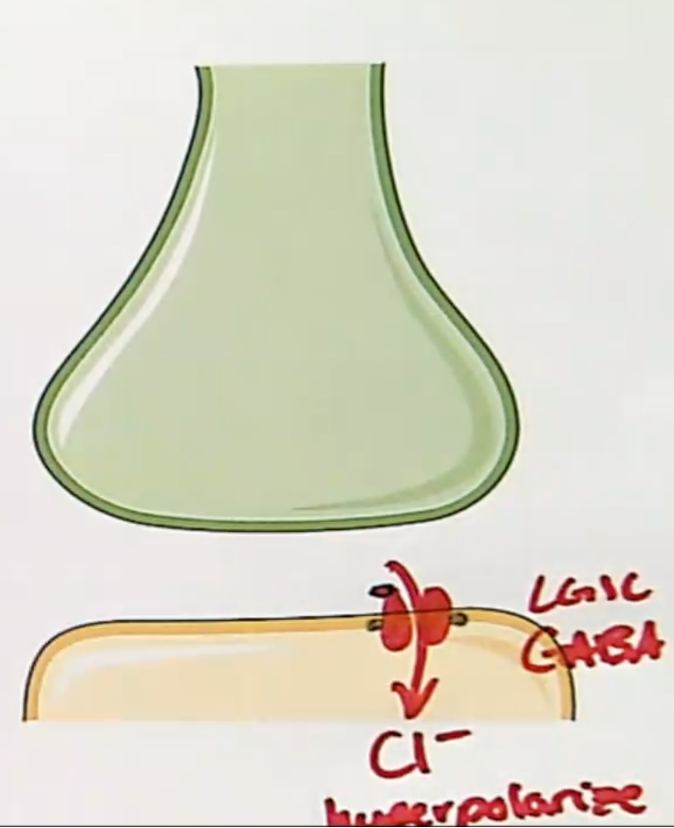
MOA for neuroactive steroids?
positive allosteric modulation (PAM) of GABAA receptors; reduces activity in hypothalamic-pituitary-adrenal (HPA) axis
brexanolone
labeled indication for neuroactive steroids?
postpartum depression
ADRs for neuroactive steroids?
sedation*, hypoxia, abuse/dependence
allosteric - means it binds somewhere other than the natural ligand
Briefly describe how inhibition of auto receptors and inhibition of reuptake transporters produce similar outcomes….
Inhibition of an auto receptor increase NT _______ from the pre synapse while inhibition of a reuptake transporter decreases _____ of NT from the synapse.
inhibition of an auto receptor increases NT release from the presynapse
inhibition of a reuptake transporter decreases the reabsorption of that neurotransmitter from the synapse
What are the NT associated with depression?
serotonin (5-HT)
norepinephrine (NE)
Dopamine (DA)
Glutamate
GABA (gamma-aminobutyric acid)
What does serotonin do?
low levels of serotonin are associated with depression
plays a role in regulating mood, sleep, and appetite
What does norepinephrine do?
deficits in NE are also linked to depression
involved in attention, focus, and arousal
What does dopamine do?
reduced dopamine levels may contribute to depression
associated with pleasure, motivation, and reward
Glutamate and depression?
excessive glutamate activity can lead to neuronal damage and inflammation, which may contribute to depression
GABA and depression?
low levels of GABA can increase anxiety and depression
Identify presynaptic mechanisms in which a drug alters neurotransmission at the synapse
Presynaptic mechanisms
drugs block presynaptic reuptake transporters (more NT in synapse)
drugs block auto receptors (disinhibition of NT release so more release)
MAO enzyme inhibitor - so more NT
Agonists vs antagonists?
Agonists: These drugs bind to and activate postsynaptic receptors, just like a neurotransmitter would. This can increase the signal or effect of the neurotransmitter.
Antagonists: These drugs bind to postsynaptic receptors but do not activate them. Instead, they block the receptors, preventing the natural neurotransmitter from binding and reducing its effect.
Identify postsynaptic mechanisms in which a drug alters neurotransmission at the synapse
Postsynaptic mechanisms: increase NT availability, block reuptake, increase receptor stimulation
GPCR (5-HT2)
GPCR are cell receptors that respond to NT
drugs (mirtaxapine) act directly on GPCRs like serotonin (5-HT) receptors to modulate mood and behavior
SSRIs work indirectly by increasing NT levels which then activates GPCRs
MAOIs block the enzymes that break down monoamine NT, which also results in more NT available to activate GPCRs
glutamate receptor (extra synaptic)
can reduce function of NMDA receptors
interfere with glutamate release (ketamine works directly by modulating glutamate receptors)
serotonin (5-HT3)
drugs affect the amount available in the brain
drugs block the reuptake of serotonin into nerve cells leaving more in the synapse
Types of agonists?
agonist: activates a receptor and causes a response
antagonist: binds to a receptor and blocks the action of an agonist but has no effect on its own
partial agonist: type of agonist that activates a receptor but produces a sub maximal response compared to a full agonist
partial agonist is also a partial antagonist
inverse agonist: binds to a receptor and produces a response opposite to that of an agonist
can only exist at a receptor that exhibits constitutive (basal) activity in the absence of natural ligand binding
it would not be beneficial to use an inverse agonist if there’s no basal activity
typical vs atypical depression?
typical: appetite is decreased and insomnia
atypical: appetite is increased and hypersomnia