Pharm II final exam (female and male repro, heart meds)
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
102 Terms
Estrogen adverse effects and CI
Adverse effects
- Endometrial hyperplasia and cancer -> give progestin to reduce risk
- breast cancer
- breast tenderness
- CV thrombotic events
- HTN
- peripheral edema
- gallbladder disease and cholestatic jaundice
- headache, migrains
- nausea
- chloasma -> facial discoloration
Contraindications
- Hx of DVT, PE, MI, stroke
- pregnancy
- vaginal bleeding w/out known cause
- liver disease
- ER positive breast cancer
- estrogen dependent cancer
Progestin adverse effect
Adverse effects
- breast tenderness, HA, arthralgias
- sleepiness
- decrease production of cervical mucus
- involution of endometrial layer (thinning) -> spotting, breakthrough bleeding, irregular menses
- in combo w/ estrogen -> increases risk of breast cancer in postmenopausal women
Menopausal hormone therapy
Low dose of estrogen (17-beta estradiol commonly)
Two regimens:
- estrogen alone (ET)
- estrogen + progestin (EPT) -> for pt w/ a uterus
Estrogen -> control menopausal symptoms
- less: hot flashes, urogential atrophy, osteoporosis
- enhanced: sleeping, libido, cognition, mood
- DO NOT give unopposed estrogen to pt w/ intact uterus
Progestin -> counterbalance estrogen-mediated stimulation of the endometrium
- decrease risk of endometrial hyperplasia/cancer
- DO NOT prescribe for pts w/ hysterectomy
Routes of administration for ERT
Oral -> most commonly used route
- needs higher dose than transdermal bc undergoes first-pass metabolism
- higher risk: dyslipidemia, venous thromboembolism, GI side effects
Transdermal -> emulsion, spray, gels, patches
Advantages
- total dose of estrogen is greatly reduced
- less N/V, lower risk for DVT, PE, Stoke
- blood levels of estrogen fluctuate less
Preferred for women with:
- history of VTE
- migrain w/ aura
- elevated triglycerides
- gallbladder disease
Recommendations for MHT
Ideal candidates: healthy, symptomatic women
- age: younger than 60yr OR within 10 yrs of menopause
- risk of complications is lower when used for ~ 5 yrs
- NOT for women over 60 starting MHT for first time
- women w/ multiple risk factors should consider diff therapy
Lowest effective dose for shortest duration necessary
- standard: 5 yrs and not beyond age 60
- recommended non-HT if symptoms persist
Menopausal symptom management
Vasomotor symptoms (hot flashes)
HT is most effective
- but some women are too high risk
Alternatives:
Selective serotonin reuptake inhibitors (SSRIs)
- escitalopram, citalopram, paroxetine (if not using tamoxifen)
Gabapentin
CBT
Genitourinary syndrome of menopause -> dryness, irritation, uncomfortable intercourse
Estrogen is most effective
- topical estrogen is best choice if this is pts ONLY symptom
- options: creams, inserts, rings
Gender affirmation dug therapy for transgender females
Goal: promote development of physical changes that match her gender identity
Medications:
Hormonal therapy
- estrogen: 17-beta estradiol
Testosterone suppression: if testes are present
- spironolcatone
- GnRH agonist (leuprolide)
Monitoring:
Estrogen levels
- physiologic female range
Serum total testosterone
- suppress to female range
Using spironolactone
- serum potassium
Breast cancer screening
Prostate screenings
Combination oral contraceptives (MOA and CI)
Estrogens used: ethinyl estradiol, estradiol
Progestins used: norethindrone, levonorgestrel, norgestrel
MOA: inhibiting ovulation, reduces fertility
- thickens cervical mucus
- alters endometrial lining
Estrogen
- suppresses release of follicle-stimulating hormone from pituitary
- inhibits follicular maturation
Progestin
- acts in hypothalamus and pituitary to suppress midcycle LH surge
- prevents ovulation
Absolute contraindications
- Hx of thromboembolism -> progestin only
- age >35 and smoking
- multiple CVD risk factors (age, smoking, DM, HTN)
- HTN (systolic >160, diastolic >100)
- VTE, ischemic heart disease, stroke, CVD
- abnormal liver function
- known or suspected breast cancer
- undiagnosed abnormal vaginal bleeding
- known or suspected pregnancy
- post-partum <21 days and <6 wks w/ breastfeeding
- migraine WITH aura
- heavy smokers
Relative contraindications
- HTN of any stage
- CAD
- diabetes
Adverse effects of COC
Adverse effects:
- HTN
- N, breast tenderness, edema, increase appetite, fatigue
Thromboembolic disorders increased risk with:
- smoking, hx, thrombophilia, diabetes, HTN, CVD, CAD, surgery/immobilization
Cancer
- promote (not cause) breast cancer growth
- protect against ovarian and endometrial cancer
- no effect on cervical cancer
Abnormal uterine bleeding
- can eliminate or reduce flow, cause spotting
Glucose intolerance
- can increase levels
Smoking increases risk of serious cardio side effects
Use in pregnancy/lactation
- contraindicated in pregnancy
- COCs can enter breast milk.
- Progestin-only during lactation
Stroke in women w/ migraines
- COCs can increase risk of thrombotic stroke
- can still use if: <35, no smoking, healthy, no aura
COC dosing schedule
Most dosed in a cyclic pattern for 28 days
- pills should be takes at same time every day
- prescribed w/ one year supply
28 day schedule:
Monophasic (preferred inititally)
- estrogen and progestin remain constant throughout the cycle of use
21 days of active pill followed by 7 days of either:
- no pill taken
- inert pill taken
- iron pill taken
Biphasic/triphasic/quadriphasic
- estrogen and progestin change as cycle progresses
Methods of starting:
- quick start method
- first day on menstrual period -> no backup needed
- first sunday after onset of menses -> backup for 7 days
Missed pills:
Missing single pill
- take ASAP, continue as normal
Missing > 2 pills
- take ASAP
- backup contraception for 7 days
- if during 1st week: emergency contraception if unprotected sex
- if during 3rd week: finish last week, skip placebos, immediately move to new pack
Combo contraceptive other routes
Transdermal contraceptive patch
- estrogen and progestin, same MOA as orals
- applied once a week
- AE and CI same as COCs
- if detached for >24 hrs backup contraception
Vaginal contraceptive ring
- estrogen and progestin
- one ring inserted each month
- comes out > 3 hrs backup contraception
- AE and CI same as COCs
Progestin only oral contraceptive
AKA minipill
- contains progestin NOT estrogen
- MOA: altering cervical secretions makes endometrium less favorable for implantation
Pros
- does not cause: thromboembolic disorders, HA, N
Cons
- less effective
- more likely to cause irregular bleeding
MUST take on time everyday
- if taken a few hours late backup protection is needed
- if two pills missed and no menstrual bleeding starts -> pregnancy test
Dosing is not cyclic, taken every day (no sugar pills)
- when starting use backup contraception for 7 days
Subdermal etonogestrel implants
Long-acting contraceptives
Route: 4-cm rod containing etonogestrel (progestin)
- implanted sub dermally in groove between biceps and triceps in non-dominant arm
- lasts 3 years
- can be used during breastfeeding after post-partum day 21
MOA:
- suppresses ovulation
- makes endometrium hostile to implantation
AE: irregular bleeding
Depot medroxyprogesterone acetate
Long-acting contraceptive
Progestin medication
- IM or SQ
- lasts 3 months
- fertility takes ~9 months to return
MOA:
- inhibits secretion of gonadotropins
- inhibits follicular maturation and ovulation
- thins endometrium to make implantation unlikely
AE
- menstrual disturbances
- weight gain, bloating, HA, depression, decreased libido
- decreased bone density
Intrauterine devices
Long acting contraceptive
Hormone-free copper IUD
- causes foreign body reaction w/ chemical changes that are toxic to sperm -> interferes w/ fertilization
- good for pts sensitive to hormones
- AE: heavier menstrual bleeding
- lasts 10 years
Levonorgestrel (progestin) containing IUD
- inhibits ovulations, prevents implantation
- AE: bleeding irregularities
- lasts 8 years
Emergency contraceptive pill
Emergency contraceptive pill
Progestin-only products
Plan B one-step or Next choice one dose (OTC)
- single dose levonorgestrel
- take w/in 72 hrs of unprotected intercourse
- MOA: delay or stop ovulation
- does NOT harm existing fetus or terminate existing pregnancy
Ulipristal acetate (UPA)
- taken w/in 5 days of unprotected intercourse (RX only)
- MOA: selective progestin receptor modulators
Insert a copper IUD
- w/in 5 days of unprotected intercourse
- MOST effective option
- expensive and not found quickly
Medical abortion
Mifepristone w/ misoprostol
Mifepristone
- MOA: synthetic steroid that blocks receptors for progesterone and glucocorticoids
Use: termination of early intrauterine pregnancy
- requires cotreatment w/ misoprostol
- w/in 12 wks of conception
- alternative to surgery for termination
AE of mifepristone and misoprostol:
- abdominal pain -> NSAIDs, heating pad
- vaginal bleeding -> 9-15 days
- infection
Contraindications
- ectopic pregnancy, hemorrhagic disorders, anticoagulation use
Follow up w/ hCG ~ 5 wks
Testosterone replacement
Indicated for:
- symptomatic men w/ primary, secondary, or mixed hypogonadism
confirmed low T (<230-350)
- must be measured in early morning
- requires confirmation of low w/ repeat level 4 wks later
NOT indicated for:
- normal T
- asymptomatic hypogonadism
- isolated ED
Testosterone pretreatment screening
Age >40
- screen for breast cancer, BPH, and prostate cancer (PSA and DRE)
Cautions
- severe sleep apnea, edema, CHF, hx of MI
Contraindications
- untreated prostate cancer
Baseline lab tests
- hematocrit, LFTs
Androgen medication classifications
Testosterone and testosterone esters
- testosterone
- testosterone cypionate
- testosterone enanthate
- testosterone undecanoate
17-a-alkylakted compounds
- fluxymesterone
- methyltestosterone
- oxandrolone
Androgen preparations for male hypogonadism
Oral
Native testosterone absorbed well but extensive first-pass metabolism makes it ineffective for hypogonadism
Oral testosterone undecanoate
- bypasses first-pass metabolism
Methyltestosterone, fluoxymesterone (17-a-alkylated androgens)
- NOT first line agents due to hepatotoxicity
Transdermal testosterone
- patches, gel (3 formations), liquid solution (1 formulation)
- FIRST-LINE -> most normal and stable testosterone conc.
Testosterone Gel
- advantages: less irritation than patches, cannot fall off
- disadvantages: can wash off, avoid bathing/swimming for 5-6hrs after application
- can be transferred to other by skin-to-skin: wash hands and any any contaminated skin
Parenteral testosterone
- advantage: dosing in wks instead of daily
- disadvantage: variable testosterone levels
Long acting -> testosterone enanthate/testosterone cypionate
- dosing every 1-2 wks injection
Extra-long acting: testosterone undecanoate
- dosing every 10 wks
Adverse effects of testosterone
Adverse effects
Virilization
- in women, girls, boys
Premature epiphyseal closure
- decrease in adult height
- perform xray hand and wrist Q 6 months
Hepatotoxicity
- 17-a-Alkylated androgens
- periodic LFTs
Effects on cholesterol
- lower HDL, elevate LDL
Prostate cancer
- does not cause but can promote growth
Thromboembolic events
Elevated Hematocrit
Breast enlargment -> T converted into estrogen
Testosterone monitoring
Testosterone targets:
- adjust dosage to achieve level of 450-600
- measure morning levels
- schedule midway between doses for injectable
- anytime for transdermal
- do NOT adjust dose based on single abnormal rest, need two consecutive level out of range
Monitor for improvement
- libido, mood, ED may take up to 6 months
Follow-up timeline
- every 2-3 months during initiation and dose adjustments
- once stable and w/in target range: annual
Serum LH
if pt has primary hypogonadism:
- if dose is adequate= LH normalizes
- elevated LH = under-treatment
Bone density -> if low density was presenting sign
- repeat DEXA every 2 yrs until normal
Prostate exam and PSA
- 3 months and then 1yr after starting T
- annually if stable
Hct
- 3-6 months after start of tx, then yearly
- stop testosterone if > upper limit of normal
Hormonal therapy for transgender men
Goal to induce physical changes to match gender identity
- stop menses
- induce virilization
- maintain hormone levels in the normal male physiological range
Principal medication: testosterone
- easiest to achieve w/ IM or SC testosterone
Monitoring:
- serum testosterone: Q3 months, then 1-2 times a year
- monitor for clinical signs of virilization, blood counts, lipid profiles
Phosphodiesterase-5 inhibitors for ED
Sildenafil, tadalafil (duration of action: 36hrs), vardenafil, avanafil
- improved erection hardness and duration in ~70% of men
- effects can last up to 4 hrs, fade after 2 hrs
MOA: Selective inhibition of PDE-5
- increases and preserves cGMP levels in penis
- MUST have stimulus
Adverse effects
Common
- headache, flushing, congestion, dizziness, dyspepsia
Serious
Hypotension
- significant drop in BP w/ nitrate (absolute contraindication), a-blocker (caution and spacing)
- can lead to syncope, cardiac events, or shock
Priapism: painful erection >6 hrs
- left untreated can permanently damage penis
- >24 hrs may never have sex again
- have to aspirate blood from corpus cavernosum, irrigated w/ vasoconstrictor
Nonarteritic ischemic optic neuropathy (NAION)
- irreversible blurring or loss of vision
Sudden hearing loss
Contraindications
Nitrates: nitroglycerin, isosorbide dinitrate
- both PDE5i and nitrates increase cGMP -> vasodilation and hypotension
- life-threatening hypotension, DO NOT combine
a-blocker: doxazosin, BPH meds
- cause arteriolar dilation
- may cause symptomatic orthostatic hypotension
- need to stagger dosing when using these and PDE5i
Caution in med w/ coronary heart disease or cardiac risk
Avoid use:
- recent CV event in last 6 months (MI, stroke, arrhythmias)
- unstable CV conditions (resting hypo/hypertension, unstable angina, decompensated heart failure)
Premature ejactulation
First line -> SSRI
MOA: serotonin can cause delay in ejaculation
- SSRI prevents reuptake of serotonin
Paroxetine is most effective
- lower dose then used for depression
Topical anesthetics -> lidocaine, prilocaine
Decrease sensitivity to glans penis
- disadvantage: transfers to partner and can delay or prevent orgasm
- use w/ condom
5-a-reductase inhibitors
Finasteride, dutasteride
- men w/ large prostates, mechanical obstruction (static)
DOC: for enlarged prostate
MOA: acts in reproductive tissue to inhibit 5-a-reductase
- enzyme that converts testosterone to DHT
- promotes regression of prostate epithelial tissue
- decreases mechanical obstruction of urethra
May take 6-12 months to have prostate shrinkage
- won't relieve acute symptoms
Adverse effects:
- decrease ejaculate volume
- decreased libido
- gynecomastia
- teratogenic to male fetus
- decrease PSA levels -> if not falling as expected, inspect for prostate cancer
a1-adrenergic antagonists
Doxazosin, tamsulosin, alfuzosin, terazosin, silodosin
DOC for mod-severe symptoms of BPH
MOA: blockade of a1 receptors relaxes smooth muscle in:
- bladder neck
- prostate
- prostatic urethra
Decrease dynamic obstruction of the urethra
- good for acute symptom relief w/ BPH
- to maintain benefits must be taken lifelong
Sildosin and tamsulosin: selective for a1a recpetors
- mostly found in prostate
- no/little effect on bp
Alfuzosin, terazosin, doxazosin: non-selective for a1-receptors
- causes vasodilation in blood vessels
- lowers bp
- do NOT combine w/ other vasodilators
Adverse effects
Non-selective agents: doxazosin
- hypotension -> caution w/ nitrates, PDE5i
- fainting (first-dose effect)
- dizziness
- somnolence
- nasal congestion
Selective agents: Tamsulosin
- abnormal ejaculation
BPH meds (PDE5i and anticholinergics)
Tadalafil -> PDE5i
- treats erectile dysfunction due to 5-alpha-reductase inhibitor
- improves BPH symptoms only, does NOT help w/ enlarged prostate
- use w/ pt who has mild BPH and ED
Oxybutynin -> anticholinergic
MOA: relax bladder detrusor muscle
- improve the urine storage capacity of the bladder
- useful for irritative voiding symptoms only (overactive bladder)
Adverse Effects:
- dry mouth, constipation
- tachycardia
- urinary retention
- agitation, confusion, drowsiness
- blurred vision
Iron deficiency (oral vs. IV and diff meds)
Oral vs. IV iron
Oral
- uncomplicated iron deficiency anemia
IV
- severe anemia (Hbg <7)
- malabsorption condition: gastric bypass, IBD, celiac
- older pts
- 2nd/3rd trimester w/ Hgb <10.5
- dialysis pt
Oral medications
Ferrous salts
- ferric citrate, ferric maltol, ferrous fumarate, ferrous gluconate, ferrous sulfate
- polysaccharide-iron complex
IV medications
- ferric carboxymaltose (FCM), ferric gluconate (FG), ferumoxytol, iron sucrose (IS), ferric derisomaltose, iron dextran
Give iron until ferritin and transferrin saturation normalizes
Oral meds for IDA
Dosing schedule: one tablet, once a day
- daily doing
- every other day: reduced GI side effects
Duration of therapy: different options
- stop when hemoglobin levels normalize -> helps detect anemia from further blood loss
- 6 months of treatment after Hgb normalized -> completely replenishes iron studies
6-8 wks to fully ameliorate the anemia
6 months to replete iron stores
Enhance absorption
Do not give w/ food
- take separately from calcium-containing food and beverages
- take w/ vitamin C to increase absorption
pH: needs acidic environment
- give 2 hrs before or 4 hrs after ingestion of antacids
Adverse effects
- constipation
- metallic taste
- itching
- black/green stools
Re-evaluate in 2 wks after starting medication
- check Hgb, reticulocyte count, iron tolerability by pt
- Hgb should rise by at least 1g/dL
IV meds for IDA
When to use:
- poor adherence to orals, GI side effects w/ oral
- prefer shorter tx course
- ongoing blood loss (ex. menorrhagia)
- malabsorption (gastric bypass, CKD)
- coexisting inflammatory state (IBD, celiac)
Adverse effects:
Infusion reactions: <1% of pts
- always do a test dose w/ any parenteral formulation
- consider pre-medicating asthmatics/allergies
Fishbane rxn
- flushing, myalgias of chest and back
Arthritic flare w/ inflammatory arthritis
Risk of infection
- bacteria like iron
Re-evaluate 4-8wks after iron administration
- can get an early spike in iron, need to wait to get true level
Vitamin B12 deficiency
Cyanocobalamin
- oral, IM, deep SubQ, sublingual, nasal
- NOT given IV as most will be excreted in urine
- most pts do oral therapy
Symptomatic pts: parenteral administration
- severe symptomatic anemia OR neuro findings
- switch to oral once symptoms resolve
Folic acid
Hazards
- does NOT treat neurologic damage
- treat the anemia but mask B12 deficiency
- should NOT be treated w/ folic acid alone
- check both folate and vit B12
Adverse effects: none
- excess vitamin is excreted when stores are adequate
Duration
Lifelong:
- gastric bypass, strict vegans, pernicious anemia
- need blood work every 3-6 months
Discontinue once corrected:
- diet
Folic acid deficiency
Consequences
Developing fetus: neural tube defects (spina bifida, anencephaly)
- imperative women of reproductive age ensure adequate folic acid levels BEFORE pregnancy occurs
- should consume 400-800 supplemental folic acid + what they get from food
Treatment
- if poor diet: correct w/ dietary measures (unless pregnancy)
- if malabsorption: need supplemental folate
Oral folic acid
- if reversible cause: 1-4 months of tx OR hematologic recovery
- if chronic cause: indefinitely
IV folic acid
- if cannot take oral meds (vomiting, obtunded)
- severe or symptomatic anemia
Sickle cell
Treatment -> Hydroxyurea
MOA
- increases fetal hemoglobin level >>> dilutes abnormal hemoglobin S
Use
- reduce frequency of pain crises, ACS, transfusions
Side effects:
- bone marrow suppression, monitor CBC every 2-4 wks
- cutaneous vasculitis/ulcerations
- teratogenic
Pain management
Mild-mod pain
- NSAIDs, acetaminophen
Mod-severe vaso-occlusive crisis:
- morphine, hydromorphone, oxycodone
Intro to diuretcis
Classified according to their site of action
- MOA: blockade of sodium and chloride reabsorption to decreased reabsorption of water
Greater the reabsorption blocked -> greater the diuresis
- act early in nephron -> block greatest amount of reabsorption, greater diuresis
- act late in nephron -> block very little
Loop diuretics
Furosemide, bumetanide, torsemide
MOA: inhibit the luminal Na/K/2Cl co-transporter in the ascending limb of loop on henle
- increased loss of: Na, Cl, H2O, K, Mg, Ca
- most potent diuretics
- "high ceiling diuretics" bc they can inhibit reabsorption of 25% of filtered sodium
Site of action: loop of henle
Adverse effects
Electrolyte distrubances:
- hyponatremia, hypocholeremia, hypokalemia (U wave), hypomegnesemia, hypocalcemia
Dehydration
- minimize risk -> start low, go slow, monitor weight
- dry mouth, unusual thirst, oliguria, excessive weight loss -> withhold furosemide
Tinnitus (ototoxicity) -> dose related
- ALL are ototoxic
Hypotension -> substantial drop in BP
- symptoms: dizziness, lightheadedness, fainting
- minimize postural symptoms by rising slowly
- if occurs -> discontinue
Other SE
- possible metabolic alkalosis, hyperuricemia (relative contraindication in gout), hyperlipidemia, hyperglycemia
Thiazide diuretics
Chlorthalidone, chlorothiazide, hydrochlorothiazide
MOA: inhibiting the Na/Cl symporter in the distal convoluted tubule
- only 10% of filtered Na -> less diuresis than loops
- amount of diuresis dependent on kidney function
- NOT effective in GFP < 15-20
Site of action: early distal convoluted tubule
Side effects
Electrolyte disturbances:
- hypokalemia, hypochloremia, hypomagnesemia
- hypercalcemia
- check Cr and electrolytes 1-2 wks after starting
Possible metabolic alkalosis
Hyperuricemia
- relative contraindication in gout
Hyperlipidemia, Hyperglycemia
Potassium sparing diuretics
Aldosterone antagonists:
- spironolactone, eplerenone
Non-aldosterone antagonists (ENAC blockers):
- triamterene, amiloride
Therapeutic use:
Hypertension
- usually in combo w/ thiazide or loop to combat K-wasting
Edema in CHF
- produces direct effects on the heart to reduce aldosterone-induced cardiac remodeling that impairs contractility and diastolic relaxation
Side effects
Hyperkalemia esp when used alone
- can cause fatal dysrhythmias if K>5
- monitor K levels and Cr
Spironolactone specific SE
- gynecomastia, menstrual irregularities, impotence, hirsutism, deepening of the voice
Trimterene specific SE
- N/V, leg cramps, dizziness
Aldosterone antagonists vs. non-aldosterone antagonists potassium sparing diuretics
Aldosterone antagonists/mineralocorticoid receptor antagonists (MRAs)
- spironolactone, eplerenone
MOA: competitive antagonist of aldosterone in late DCT and collecting ducts
- BLOCKS action of aldosterone
- retention of potassium
- increased sodium excretion (prevents reabsorption)
- scant diuresis -> decreased SV
Site of action: distal nephron
Non-aldosterone antagonists (ENAC blockers)
- Triamterene, amiloride
MOA: inhibit sodium channels in the late distal tubule and collecting ducts
- reduction in potassium secretion (increase K)
- decreased sodium reabsorption (decreased Na)
- scant diuresis
Site of action : distal nephron
- used in HTN
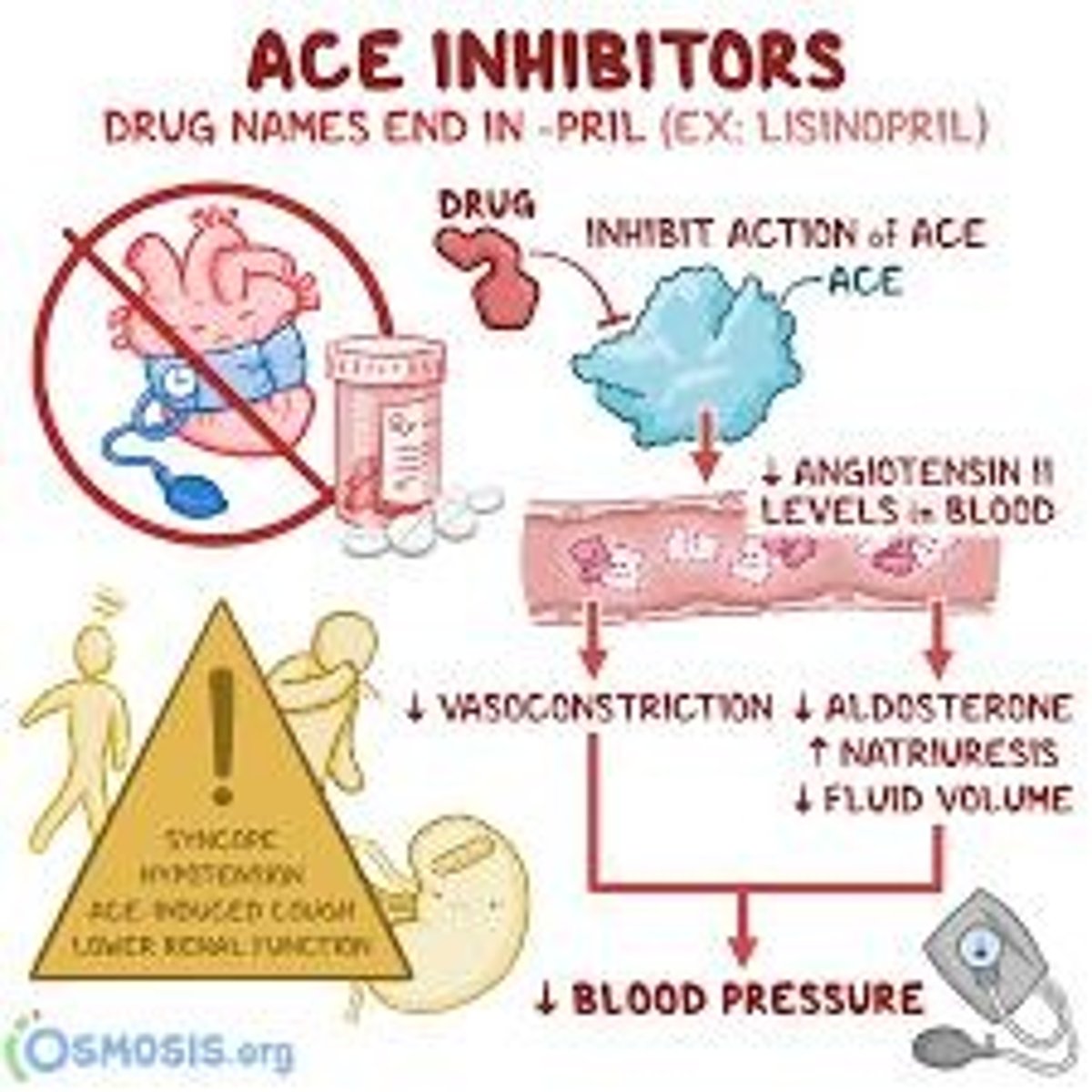
Angiotensin converting enzyme inhibitor
End in -pril (ex. lisinopril)
MOA
- inhibit ACE to block conversion of angiotensin I to angiotensin II
- decreases angiotensin II formation
- increase levels of bradykinin
Vasodilation -> decreased SVR -> decreased BP
Decreased aldosterone decretion -> decreased SV
- prevent of reverse pathologic changes in heart and blood vessels
- increase excretion of sodium and water
Therapeutic use:
- HTN, heart failure, MI
- LV dysfunction
- diabetic nephropathy
Avoid use/or use caution in:
- pregnant pts -> fetal injury
- pts w/ history of angioedema -> increased bradykinin
- pts w/ B/L renal artery stenosis -> can cause acute renal failure
Adverse effects
- dry cough -> d/t increased bradykinin
- angioedema -> d/t increased bradykinin
- hyperkalemia -> check levels 1 wk after starting
- AKI -> check Cr levels 1 wk after starting
- teratogenic
- first dose hypotension
Angiotensin receptor blocker
end in -sartan (ex. losartan)
MOA
- block effects of angiotensin II at the receptor level
- decreases angiotensin II action -> vasodilation -> decrease SVR
decrease aldosterone secretion -> decrease SV
- prevents pathologic changes in the heart and vessels
- increase excretion of sodium and water
More complete blockage of angiotensin II than ACEi
- does NOT affect bradykinin levels
Therapeutic uses:
- HTN, heart failure, MI, diabetic nephropathy
Avoid use/or use caution in:
- pregnant pts -> fetal injury
- pts w/ history of angioedema -> increased bradykinin
- pts w/ B/L renal artery stenosis -> can cause acute renal failure
Adverse effects
- cough -> less then ACEi
- angioedema -> less than ACEi
- hyperkalemia -> check 1wk after starting
- AKI -> check C levels 1wk after starting
- first dose hypotension
Aldosterone antagonists
Eplerenone, spironolactone
MOA
- blocks aldosterone receptors at the mineralocorticoid receptor
- promotes K retention and Na/H2O loss
- decreases BP
Therapeutic uses
- HTN, heart failure
Adverse effects
- eplerenone has less antiandrogen side effects
- gynecomastia
- hyperkalemia
Calcium channel blockers (dihydropyridines)
End in -dipine (ex. amlodipine, nifedipine)
MOA
- blocks CC in vascular smooth muscles
- promotes vasodilation
- little blockage in the heart -> cannot be used for dysrhythmias
Hemodynamic effects
- primarily cause arterial vasodilation (NOT venous)
- decrease BP
- may cause reflex tachycardia due to decrease BP
- do NOT alter contractile force
Adverse effects
- postural hypotension
- facial flushing
- gingival hyperplasia
- headache
- edema of ankles and feet
- reflex tachycardia -> increases cardiac oxygen demand -> increases anginal pain -> combine with BB to prevent
Calcium channel blockers (non-dihydropyridines)
diltiazem, verapamil
MOA
- blocks CC in the vascular smooth muscles AND the heart
- promotes vasodilation (less than DHP)
- decrease HR and contractility
Hemodynamic effects
- have more balanced effect on both the heart and blood vessels
- lower blood pressure through vasodilation
- decrease HR and contractility
Adverse effects
- MC complaint is constipation
- dizziness, facial flushing, headache
- gingival hyperplasia
- edema of ankles and feet
Cardiac effects
- SA node: bradycardia
- AV node: partial or complete AV block
- Myocardium: decreased contractility
Do NOT use in pts w/:
- sick sinus syndrome
- second or third degree AV block
- decompensated heart failure
Beta-adrenergic antagonists aka beta-blockers
Nonselective -> B1=B2
- propranolol, sotalol, timolol
Cardioselective B1>>B2
- atenolol, metoprolol
W/ vasodilating actions -> mixed alpha and B1=B2
- carvedilol
- labetalol
Mechanism of action -> all BBs
Heart
- Block action of norepinephrine and epinephrine at β1 receptors on cardiac muscles
- inhibit nodal cell from firing -> reduce HR
- inhibit contractile cell from firing -> reduce contractility
- Overall Effect: decreased CO/SV = decreased BP
Kidney
- Decrease renin release from juxtaglomerular cells → decreased SVR=decreased BP
Adverse effects
- Bradycardia
- Hypotension- Reduced CO
- Precipitation of Heart Failure
- AV heart block
- Rebound cardiac excitation- with abrupt cessation
- Impotence
- Fatigue
B2 blockage
- bronchoconstriction
- hypoglycemia awareness decreased
Caution and CI
All BBs
- Avoid and/or use caution in: Patients on concurrent non DHP CCBs, Patients with bradycardia , Heart block
Nonselective BBS
- avoid/use caution in: pts w/ asthma and COPD and in diabetics
Central alpha-2 agonists
Clonidine, methyldopa
MoA: Stimulate central α-2 receptors in the central nervous system (α-2 agonist)
- Suppress central sympathetic outflow
- Suppresses release of NE -> decreased BP
Avoid use in:
- older adults -> sedation, hypotension, dizziness
Side effects
All
- Orthostatic hypotension
- Dizziness
- Headache
- Sedation/Drowsiness
- Dry mouth
- Constipation
- Confusion
Methyldopa ONLY
- Fluid retention
- Lupus-like syndrome
- Hepatitis -> Monitor LFTs
Advantages
- Clonidine is fast acting -> good for urgent blood pressure control
- Methyldopa ONLY -> can be used in pregnancy
Disadvantages
- rebound HTN when abruptly stoped
alpha-1 blockers
-zosin Doxazosin, prazosin, terazosin
MOA: Block effect of norepinephrine at arterial α-1 receptors (α-1 blocker). Non-selective.
- Vasodilation → decreased SVR
Avoid and/or use caution in: Elderly
- Orthostatic hypotension
Adverse effects
- “First-dose” phenomenon
- Orthostatic hypotension
- Dizziness
- Headache
- Syncope
- Fluid retention
Advantages
Effective for management of BPH
Disadvantages
Evidence demonstrating less efficacy in reducing CV events
ACC/AHA HTN initial tx recommendations
Initiate single agent if meets any of the following
- ASCVD
- CKD
- Diabetes
- Calculated 10-year ASCVD risk greater than ≥ 10%
- Anyone with BP >160/100, regardless of risk
Choose from following first-line agents
- ACE, ARB, CCB (-dipine or verapamil/diltiazem), thiazide diuretic
Elevated BP (120-129/<80)
- lifestyle modification
Stage 1 HTN (130-139 OR 80-89)
- consider single agent
Stage 2 HTN (>= 140 OR >= 90)
- 2 meds from 2 diff classes
Start w/ 2 meds from 2 diff classes with:
- stage 2 HTN
- SBP is >20 or DBP >10 from goal
- in AA pts
Individualizing therapy for HTN
Renal disease
All classes work: ACEI/ARBs work best
- Most cases also add diuretic
- Advanced renal insufficiency thiazide is not useful- use a loop
Diabetes
Preferred meds: ACEI/ARBs
- slow progression of renal damage
Other Meds:
- BB: can decrease morbidity and mortality, use with caution can mask hypoglycemia
- Thiazide and loop diuretics: cause hyperglycemia, use with caution
Older adults >55 y/o
Follow same general treatment principles:
- Initiate at lower doses- ½ of younger adult dose
- Titrate doses slower
Increased risk of orthostatic hypotension and dizziness
- Cardiovascular reflexes are blunted
- Avoid central α-2 agonists and α-1 blockers
HTN stepped care approach w/ NO compelling indications
Step 1
- ACEi/ARB or CCB or Thiazide
Step 2
- ACEi/ARB plus CCB or Thiazide
Step 3
- ACEi/ARB plus CCB plus Thiazide
Step 4
- ACEi/ARB plus CCB plus Thiazide
- plus Spironolactone
Loop diuretics for HF
First-line for fluid retention in HFrEF & HFpEF
- ↓ Symptoms of congestion (edema, dyspnea)
- Helps maintain euvolemia
- Associated with ↓ hospitalizations (not mortality)
When to Use:
- Patients with current or prior signs of fluid overload
Mechanism of Action:
- Inhibits Na⁺/K⁺/2Cl⁻ co-transporter in the ascending loop of Henle
- ↓ Sodium and water reabsorption → ↑ diuresis
Side effects
- Hypokalemia (15%) – prophylactic potassium repletion may be needed
- Hypomagnesemia (15%)
- Acute kidney injury (pre-renal)- > Increased SCr
- Ototoxicity
- Hypotension
- Hyperuricemia (often asymptomatic) (18%)
- Hyponatremia (7%)
ACEi (-pril) for HF
- Improve functional status and reduce mortality by ~47%
- Recommended for all HF patients without CI
- Favorably influence cardiac remodeling
Hemodynamic Benefits:
Arteriolar dilation:
- ↑ Stroke volume (SV) and cardiac output (CO)
- ↑ Renal blood flow → ↑ sodium and water excretion
Venous dilation:
- ↓ Venous pressure → ↓ pulmonary congestion, preload, cardiac dilation
Aldosterone suppression:
- ↑ Sodium and water excretion
Potassium retention
Net Effect:
- ↓ Preload and afterload → ↓ cardiac workload
AE: hypotension, hyperkalemia, cough, angioedema, renal failure, teratogenic
ARB (-sartan) of HF
Similar effect to ACEI
- Less effect on cardiac remodeling than ACEI -> ACEI is preferred
- Use: HF who can’t tolerate ACEI
Hemodynamic Benefits:
Arteriolar dilation: ↑ Stroke volume and cardiac output, ↑ renal blood flow, ↑ Na⁺/H₂O excretion
Venous dilation: ↓ Venous pressure → ↓ pulmonary congestion, preload, cardiac dilation
Aldosterone suppression: ↑ Sodium/water excretion, potassium retention
Net Effect: Arterial and venous vasodilation → ↓ preload and afterload → ↓ cardiac workload
AE: hypotension, hyperkalemia, cough, angioedema, renal failure
Aldosterone antagonists for HF
Spironolactone and eplerenone
Indication:
- Stage II–IV HFrEF
- Reduce morbidity and mortality
Mechanism: Block aldosterone receptors in heart and kidneys
- ↓ Cardiac remodeling and fibrosis
- ↓ Sympathetic nervous system activation
- ↓ Baroreceptor reflex activation
AE: hypotension, hyperkalemia, gynecomastia (with spironolactone), impotence (with spironolactone)
ARNi for HF
Sacubitril/valsartan (entresto)
Indications:
HFrEF with NYHA Class II–III symptoms
- Reduces morbidity and mortality
- Preferred over ACEi/ARB in appropriate patients
- ACEi/ARB reserved for those who cannot tolerate ARNi
Components:
- Valsartan: ARB → blocks angiotensin II receptors
- Sacubitril: neprilysin inhibitor → prevents breakdown of natriuretic peptides
- Net Effect: ↑ Natriuretic peptides → promote vasodilation, natriuresis, and ↓ blood volume/preload
Important Pearl:
- Sacubitril must be combined with an ARB because neprilysin inhibition alone increases angiotensin II levels
- The ARB component blocks the effects of excess angiotensin II
Side Effects:
- Hypotension, hyperkalemia, increased SCr, Angioedema
Important Precautions:
- Do not administer with an ACEi or within 36 hours of last ACEi dose (risk of angioedema)
- Contraindicated in patients with a history of angioedema from any cause
Monitoring: Similar monitoring requirements as ACEi/ARB
- Serum potassium (K)
- Renal function
- Blood pressure
Beta-blockers for HF
ONLY -> carvedilol, metoprolol succinate, bisoprolol
- First-line therapy for all patients with HFrEF
- Reduce all-cause mortality and hospitalizations
- Improve ejection fraction (EF)
Clinical Considerations:
- Start only when HF is stable and patient is euvolemic
- Dose must be carefully titrated to avoid worsening HF
- Benefits may take 1–3 months to manifest
MOA -> block B1-adrenergic receptors in heart
- reduce sympathetic effects
- ↓ Heart rate -> allows more ventricular filling time
- ↓ Contractility initially -> reduces workload and oxygen demand
Long-term: improves ventricular function by reversing remodeling
- ↓ Risk of arrhythmias by stabilizing cardiac electrical activity
AE:
- Fluid retention and worsening HF -> especially if started too quickly
- Fatigue
- Hypotension
- Bradycardia
- Heart block
Cardiac glycoside for HF
Digoxin
Indications:
- Add-on therapy for patients still symptomatic despite standard HF meds
- Rate control in HF patients with afib and low BP
- Reduces hospitalizations only — no mortality benefit
Toxicity risk
- seen w/ levels >2
MOA
Inhibits Na⁺/K⁺ ATPase pump in myocardial cells
- ↑ Intracellular Na⁺ → ↑ Ca²⁺ influx via Na⁺/Ca²⁺ exchanger
- Net effect: increased cardiac contractility (positive inotrope)
Common Symptoms:
- Fatigue, weakness, confusion, delirium, psychosis
- Nausea, vomiting, anorexia
- Visual disturbances: halos, photophobia, red-green or yellow-green vision
Cardiac Effects:
- Arrhythmias: ventricular tachycardia, Vfib
- AV block, sinus bradycardia
Risk Factors for Cardiac Toxicity:
- Low magnesium (↓Mg)
- Low potassium (↓K)
- Low calcium (↓Ca)
Reversal Agent:
- Digibind® — antibody fragments that bind digoxin for renal excretion
Stages of HF
Stage A -> high risk for developing HF, but no Sx
Aggressive RF control
- HTN -> ACEi or ARB
- CV risk reduction -> stop smoking, manage dyslipidemia
- diabetes -> SGLT2i
Stage B -> no sx but stuctural heart disease
Goals
- prevent symptomatic HF and cardiac injury
- delay remodeling and LV dysfunction progression
Treatment plan
- ALL stage A tx
- plus ACEi/ARB and BB
Stage C -> structural HD plus HF symptoms
All stage A tx
- change to ARNi
- BB, aldosterone, SGLT2i
- Loop diuretic PRN
Additional options
- digoxin -> rate control esp. in hypotensive pts
- hydralazine + isosorbide dinitrate -> for AA pts
Stage D -> marked sx w/ recurrent hospitalizations
All treatments of stage A-C
- chronic inotropic meds -> symptom relief
- LVAD
- palliative care
Other recommendations for HF
Calcium channel blockers
Avoid Diltiazem and Verapamil
- May worsen HF and increase mortality
Amlodipine / Felodipine
- Do not improve HF outcomes
- Can be used for uncontrolled HTN (target BP <130/80)
The following are not indicated for HF by itself, but should be used if indicated for other disease states are present
- Anticoagulation
- Antiplatelets (including aspirin)
- Statins
Omega-3 fatty acids may be reasonable in patients with NYHA II-IV symptoms
HMG-CoA reductase inhibitors
Statins
MOA
- Inhibit HMG-CoA reductase
- rate limiting step in cholesterol biosynthesis
Effects on lipid profile
- Decrease LDL (20 – 55%)
- Decrease TG (10-30%)
- increase in HDL (5-15%)
Statin therapy recommended for:
Clinical ASCVD or LDL >190
- high intensity
LDL 70-189:
- dibetes -> moderate intensity statin
- multiple RF and 50-75 -> high intensity
ASCVD risk
- >20% -> high intensity
- 7.5-20% -> moderate intensity
- 5-7.5% -> lifestyle vs. moderate intenisty
- <5% -> lifestyle
Adverse effects:
Most common SE:
- constipation, diarrhea, dyspepsia, nausea, abdominal pain
Myopathy:
- Affects 5–10%: muscle aches, tenderness, weakness
- Rare: Myositis → very rare: Rhabdomyolysis
- Rosuvastatin = highest risk
- Get CK at baseline and if symptoms develop
- Discontinue if CK >10x ULN
Hepatotoxicity:
- Check baseline LFTs, repeat if symptomatic
New-Onset Diabetes: 1 in 500
- Benefit >risk. Keep taking
Teratogenic
Monitoring and interactions for Statins
Monitoring
Lipid panel
- Baseline
- 4-6 weeks after starting treatment then annually
Liver Function Tests
- Baseline for all patients
- Follow-up only if symptomatic
Creatine phosphokinase
- Baseline CK
- Recheck if muscle symptoms
Interactions
CYP Enzyme Interactions
- CYP inhibitors → ↑ statin levels → ↑ risk of myopathy
- Rosuvastatin & Pravastatin = least CYP interactions
Grapefruit juice
- Inhibits CYP3A4: ↑ absorption and ↓ metabolism of atorvastatin, lovastatin, simvastatin
- Moderate intake OK: ≤ 8 oz/day or ½ grapefruit/day
Amlodipine
- ↑ levels of atorvastatin, lovastatin, and simvastatin
Gemfibrozil
- contraindicated with statins
- ↑ risk of severe myopathy/rhabdomyolysis
Switching statins
- if drug/food interaction choose pravastatin
- if need high intensity -> rosuvastatin
Cholesterol absorption inhibitors
Ezetimibe
MOA
- Inhibits cholesterol absorption in the small intestine
Effects on lipid profile
- Decreases LDL (18-23%)
- Decrease TG (5-10%)
- Increase HDL (1-3%)
Reduction in ASCVD events s/p MI when combined with a moderate intensity statin
- Contraindicated in active liver disease or persistent elevations in LFTs
Adverse effects: generally well tolerated
- Myalgias, diarrhea, arthralgia
Adenosine triphosphate-citrate lyase inhibitor
Bempedoic acid
MOA
- inhibits ATP-citrate lyase (ACL)
- ACL is upstream of HMG-CoA reductase in cholesterol synthesis
- Works only in the liver, not active in skeletal muscle
Effects on lipid profile
- Decreases LDL (20-25%), better when added to statin
Reduction in ASCVD events
Adverse effects: generally well tolerated
- Hyperuricemia (caution in gout), back pain, muscle spasm, tendon rupture
Bile acid resins
Cholestyramine, colesevelam
MOA
- Bind bile acids in intestine → form complexes → excreted in feces
- This depletes bile acid, forcing liver to use cholesterol to make more bile acids → lowers LDL
Effects on lipid profile
- Decrease LDL (15-20%)
- Increase or no change in TG (5%)
- DO NOT USE IN PATIENTS WITH TG ≥ 300 mg/dL- can -reflex cause hyperTG
- Increase HDL (3-5%)
Adverse effects & drug interactions: not absorbed through the GI tract, so devoid of systemic effects
GI side effects:
- constipation, abdominal pain, cramping, bloating, gas, dyspepsia
Decreased absorption of fat-soluble vitamins (A, D, E, K) - - especially with cholestyramine
May impair absorption of other meds
- administer other drugs 1 hour before or 4 hours after
Fibrates
Fenofibrate, gemfibrozil
MOA
- Activate PPAR-α (peroxisome proliferator-activated receptor-alpha)
- ↓ VLDL production → ↓ triglycerides
Effects on lipid profile
Decrease LDL (5-20%)
Decrease TG (20-50%)
Increase HDL (15%)
Contraindicated in severe liver disease, gall bladder disease
Adverse effects
- Increase LFTs
- Myopathy- increased risk with used with statin (especially Gemfibrozil)
- Gallstones: upper abdominal discomfort, intolerance of fried foods, bloating
Monitoring
- LFTs, renal function
PCSK9 inhibitors
Alirocumab, evolocumab, inclisiran
MOA
- Monoclonal antibody (“biologic”) that inhibits proprotein convertase subtilisin kexin type 9 (PCSK9)
- Net effect: increased LDL clearance
- Dramatic decrease in LDL when combined with a statin (60%)
Administered subcutaneously, every 2-4 weeks
Adverse effects
- Injection site reactions
- Nasopharyngitis
Monitoring
- LDL at baseline and then at 4-8 weeks to assess response
Niacin
Niacin
MOA
- Decreases rate of hepatic synthesis of VLDL and LDL
Effects on lipid profile
- Decrease LDL (5-25%)
- Decrease TG (20-50%)
- Increase HDL (15-35%)
Do not use in active liver disease, peptic ulcer disease
Adverse Effects:
- Hepatotoxicity
- Can increase blood glucose-benefit outweighs risk for most patients
Most common
- Flushing -> Pre-med w/ aspirin 325 mg 30-60 min prior to niacin (may use other NSAIDs)
- Take with food, but avoid alcohol, hot beverages, spicy foods with administration
Increase Uric Acid Levels-caution in Gout
Monitoring
- LFTs at baseline then every 6 months
- Blood glucose/A1c (if DM)
- Uric acid (if gout)
Omega-3 fatty acids
OTC fish oil
MOA -> unknown
- used for severe hypertriglyceridemia (>= 500)
Affect on lipid panel
- Decreases TG by 25-45%
- May increase LDL by as much as 45%
- Minimal effect on HDL
Adverse effects:
- Dyspepsia, fishy burp, diarrhea, GI discomfort
- Reduction in platelet aggregation -> increased risk of bleeding
- Caution in patients with fish or shellfish allergy
Aspirin
Anti-platelet
MOA -> suppresses platelet aggregation
- irreversible inhibition of thromboxane 2 (TXA2) via COX-1
- COX-1 inhibition -> decrease TXA2 -> decrease platelet aggregation
- last for life of the platelets (7-10 days)
Indications
- ischemic stroke, TIA
- chronic stable angina, unstable angina
- coronary stenting
- acute MI, previous MI, prevention of MI
Prophylactic dosing
- used only for prophylaxis NOT treatment of VTE
Adverse effects
- dyspepsia
- nausea
- bleeding/bruising
Do NOT take NSAIDs w/ aspirin
- NSAIDs block aspirins access to COX-1, antagonising its irreversible platelet inhibition
- if need to: take aspirin first than NSAID 2+ hours later
Clopidogrel
Anti-platelet
MOA -> suppresses platelet aggregation
- irreversible inhibition P2Y12 ADP receptor on platelets
- ADP inhibition -> decrease GPIIb/IIa complex -> decrease platelet aggregation
- last for life of the platelet (7-10 days)
- slower onset than aspirin
Indications
- ischemic stroke, TIA
- coronary stending
- acute MI, previous MI, prevention of MI
Prophylactic dosing
- prevent recurrence of thrombotic event
- drug-eluting stent -> 6-12 months
- post-MI or stroke -> 12 months
Side effects
- bleeding/bruising
- rare: thrombotic thrombocytopenia purpura (TTP)
- do NOT take w/ PPIs
Ticagrelor
Anti-platelet
MOA -> suppresses platelet aggregation
- reversibly inhibits the P2Y12 ADP receptor on platelets
- platelet function recovers faster after stopping
- preferred over clopidogrel in high-risk ACS pts
Indications
- ischemic stroke, TIA
- coronary stending
- acute MI, previous MI, prevention of MI
Side effects
- bleeding/bruising
- dyspnea
Prophylactic dosing
prevent recurrent of thrombotic event
- generally at least 12mo post-MI or stent
Unfractionated Heparin
Anticoagulants
MOA -> binds and enhances antithrombin III
- potentiates inhibition of factor Xa and factor IIa (thrombin)
- prevents conversion of fibrinogen to fibrin
Indications
- prophlaxis and treatment of venous thromboembolism (VTE)
Adverse effects
- bleeding and bruising -> requires monitoring
- heparin-induced thrombocytopenia (HIT) -> MC complication of HIT is VTE
- epidural/spinal hematoma risk
HIT treatment
- stop ALL heparin and warfarin products
- AVOID platelet transfusion unless actively bleeding
Start non-heparin anti-coag
- argatroban, fondaparinux, DOACs (apixaban, rivaroxaban)
Low molecular weight heparin (LMWH)/enoxaparin
Anticoagulant
MOA
- selectively inhibits factor Xa > IIa
- works via antithrombin III prothrombin
Uses
- prophyaxis and tx of VTE
- used inpatient and outpatient DVT/PE tx and bridge therapy
Side effects
- bleeding and bruising
- risk of HIT
- spinal/epidural hematomas w/ spinal puncture
Dabigatran
Oral direct thrombin inhibitor, anti-coag
MOA -> direct, reversible inhibiton of factor IIa (thrombin)
Use:
- prevention of systemic embolism in Afib
- treatment of DVT/PE
- prevention of recurrence of DVT/PE
Adverse effects
- bleeding and bruising
- GI: dyspepsia, gastritis-like symptoms -> take w/ food/PPI
- epidural or spinal hematomas
Warfarin
Vitamin K inhibitor, anti-coag
MOA -> inhibits vit K epoxide reductase
- reduced activation of vit K-dependent clotting factors (II, VII, IX, X)
- also affect natural anti-coags protein C and S
Dosing and initiation:
- NOT used alone to start VTE treatment
- requires overlap (bridging) w/ a rapid-acting anti-coag (ex. enoxaparin, heparin)
- overlap continues for minimum 5 days and until 2 consecutive INR readings > 2 at least 24hrs apart
INR goals
- standard anti-coag: 2-3
- prosthetic heart valve: 2.5-3.5
- low-intensity warfarin: 1.5-2.5
Drug interactions
FAB5 potentiate effect (increase INR interaction w/ warfarin -> takes even longer to clot)
- metronidazole, amiodarone, bactrim, fluoroquinolones, fluconazole
Vit K rich food (decrease INR)
Adverse effects
- exacerbates bleeding/bruising
- induced skin necrosis
- purple toe syndrome
Factor Xa inhibitors
Rivaroxaban, apixaban, edoxaban
MOA -> direct inhibiton of factor Xa, preventing activation of thrombin and clot formation
Use
- prevention of stroke in afib
- treatment/prophylaxis/reduce risk of recurrence DVT/PE
General warning
- concurrent antiplatelets, SSRIs, NSAIDs increase risk of bleeding
Side effects
- bleeding and bruising
Fibrinolytic agents
Alteplase, tenecteplase
MOA -> tissue plasminogen activator (tPa)
- enhances conversion plasminogen to plasmin, initiating fibrinolysis
- degrades the fibrin matrix of the thrombus
Side effects
- bleeding, hemorrhage (GI, ICH)
Use:
- unstable PE or severe iliofemoral DVT
- restoring catheter and shunt function
Absolute and relative contraindications
- pregnancy
- healing wounds
- Hx of CVA
- brain tumor
- intracranial bleeding
- metastatic cancer
VTE treatment
Treatment for DVT and PE similar
Basic approach
- initial phase (5-7 days) -> aggressive anti-coag
- maintenance phase (3-6 months) -> full-dose anti-coag
- extended phase -> unprovoked (higher recurrence risk) or provoked (lower recurrence risk)
Preferred agents
DOACs: apixaban, rivaroxaban
Special populations
Pregnancy
- preferred -> UFH and LMWH (does not cross placenta)
- avoid -> warfarin
- lactation -> warfarin, LMWH, UFH all safe
- DOACs -> NOT recommended
Cancer
- first-line: LMWH
- DOACs (rivaroxaban, apixaban, edoxaban) as alternative
Invassive procedures
- assess bleeding risk vs. thrombotic risk
- short half-life agents preferred
- bridging may be needed for high-risk pts on warfarin
Anticoagulation reversal agents
Warfarin
Vitamin-K (phytonadione)
- slower effect -> takes ~24hrs to significantly raise INR
- if immediate reversal needed -> consider FFP or prothrombin complex concentrate (PCC)
UFH and enoxaparin (LMWH)
Protamine sulfate IV
- neutralizes UFH completely
- partially reverses LMWH (enoxaparin)
Stopping/starting blood thinners and procedures
Warfarin
- stop 5 days before procedure
- bridge w/ LMWH is high thrombotic risk (stop LMWH 24hrs before procedure)
- re-start 12-24hrs post procedure
DOACs -> apixaban, rivaroxaban, dabigartran, edoxaban
- low bleeding risk procedure -> stop 24hrs before
- high bleeding risk procedure -> stop 48-72hrs before
- restart 24-72hrs post pocedure
LMWH (enoxapain)
Therapeutic dosing -> stop 24hrs before procedure
- low bleeding risk -> restart 24hr post-op
- high bleeding risk -> restart 48-72hrs post-op
Prophylactic dosing
- stop -> 12hrs before procedure
- restart -> 12-24hrs post-op
UFH -> IV infusion
- stop 4-6hrs before procedure
- restart 6-12hrs post-op
Aspirin (ASA)
- can continue for minor or moderate risk procedures
- stop 5-7days before major high-risk bleeding
Clopidogrel
- stop 5-7 days before
Ticagrelor
- stop 5 days before
Dual antiplatelet therapy
- dealy elective surgery for at least 6-12 months post stent
Antidysrhythmic drugs
Class 1: sodium channel blockers
- quinidine
- lidocaine
Class 2: BB
- propranolol
Class 3: potassium channel blockers
- amiodarone
Class 4: CCB
- verapamil
Class 5: others
- adenosine, digoxin
Class 1: sodium channel blockers
Quinidine
MOA -> binds Na+ channels -> prevents Na+ influx
- delays repolarization -> prolongs action potential
- strong anticholinergic effects -> increases SA node automaticity and AV conduction
- may cause ventricular tachycardia (fast ventricular rate)
Pre-treat w/ BB, verapamil, or digoxin to control ventricular rate
Uses
- treat SV and ventricular dysrhythmias
Indications
- long-term suppression of SVT, atrial flutter, afib, sustained VT
Adverse effects
cinchonism:
- tinnitus, headache, nausea, vertigo, blurred vision
anticholinergic:
- dry eyes, dry mouth, urinary retention, constipation
cardiotoxicity at high doses
Class II: BB
Metoprolol, propranolol, atenolol, esmolol
MOA -> block B-receptors, reducing effects of catecholamines
- decrease HR
- decrease contracility
- depress automaticity
Use -> control ventricular rate
- Afib, atrial flutter
Contraindications
- bradycardia
- 2nd or 3rd degree heart block
- concurrent use w/ non-DHP CCB (verapamil)
Class III: potassium channel blockers
Amiodarone
- most effective antiarrhythmic
Side effects and monitoring
Hyper- and hypo- thyroidism
- TSH/T4 baseline and every 6 months
blue-gray skin discoloration
- PE at every office visit
fulminant hepatitis
- LFTs baseline and every 6 months
pulmonary fibrosis
- CXR baseline and every 12 months
corneal microdepositis
- slit-lamp exam
Class IV: CCB
Verapamil, diltiazem
MOA -> block inward calcium current during plateau and phase 4 of action potential
Use
- supraventricular arrhythmias
- control of ventricular rate in Afib and atrial flutter
Adverse effects
- bradycardia, AV block, heart failure, vasodilation hypotension, peripheral edema, constipation
Digoxin for anti-arrhythmia
MOA -> inhibits Na/K-ATPase pump, suppresses AV node conduction, shortens refractory period
- decrease HR, increase contraction (pos inotrope)
- PO or IV
Adverse effects
- dysrhythmias
Monitoring
- ECG, HR, BP, CrCl, drug level, electrolytes, s/s toxicity
Signs of toxicity
- greenish-yellow halos, arrhythmias, blurred vision
Contraindications
- ventricular fibrillation
Atropine
MOA -> antimuscarinic, blocks acetylcholine
- monitor HR, BP, ECG
Indications
- bradyarrhythmia
Adverse effects
- blurred vision, xerostomia, urinary retention, constipation, tachycardia
Adenosine
MOA -> slows conduction time through AV node
- IV only, 6mg dose
DOC for converting acute supraventricular tachycardias (SVT)
- ultra short half life (~10 seconds)
Adverse effects
- chest pain/pressure, flushing, GI distress, dyspnea
Contraindications
- bradyarrythmias
Sinus bradycardia
HR < 60bmp
- can occur w/ sick sinus syndrome or tachy-brady syndrome
Stable -> no treatment
Hemodynamically unstable
- 1st line atropine 0.5mg IV q3-5min (max dose 3mg)
- if refractory: dopamine infusion, epinephrine infusion
Chronic management of sick sinus syndrome
- pacemaker
- HFpEF pts: continue BB + pacemaker
Atrial fibrillation
Goals of treatment
- improve ventricular function
- prevent stroke/systemic embolism
Rate control
strict goal: HR <80bpm
- if symptomatic or HFrEF
lenient goal: HR <110bpm
- if asymptomatic and preserved EF
meds
- BB (metoprolol, atenolol)
- non-DHP CCB (verapamil, diltiazem)
Rhythm control
- goal: maintain sinus rhythm + improve quality of life
- consider in younger, symptomatic pts of failed rate control
Stroke prevention
- risk scoring (CHA2DS2-VASc)
- anti-coag as needed; DOACs preferred
Meds for anginal symptoms and stable angina CAD risk reduction
Anginal rescue relief
- SL NTG
- NTG spray
Anginal symptoms prophylaxis
- BB, CCB, long acting nitrates
- ranolazine
Reduce mortality and prevent future event, pts get all 3:
antiplatelet
- aspirin 81mg OR clopidogrel
ACEi/ARB
- esp if DM, HTN, CKD, HF, prior MI
Statin
- high-intensity for ALL pts w/ known CAD
Nitrates
Rapid Acting Nitroglycerin (glyceryl trinitrate)
MOA
- Converts to nitric oxide → Relaxes vascular smooth muscle → Leads to vasodilation
Use
- Rescue therapy
- Quickly halt episode of angina once it has begun
- should be used no more every 2-3 days
1st line for acute angina attacks
- sublingual or translingual to avoid fist-pass metabolism
- call EMS if no relief after 1st dose
Pharmacodynamic actions: vascular dilation
- Peripheral Arteries → ↓ Afterload
- Peripheral Veins → ↓ Preload
- Coronary Arteries → ↑ Blood flow to the heart muscle
Dosing options
Sublingual SL tablet
- usually 0.4mg PRN for chest pain, max 3 doses
Nitroglycerin pray
- 0.4mg/spray, 1-2 sprays q5min PRN, max 3 doses
Beta blocker for angina
Mechanism of Action: Antagonize adrenergic beta receptors
- Reduce the workload of the heart
- Decrease myocardial oxygen demand
- ↓ heart rate and contractility
Titrate to resting HR of 55-60bpm
Clinical benefits
- Works at rest and during exertion
- Reduces both symptomatic and silent ischemia
- Decreases frequency and severity of angina
Side effects
- Bradycardia
- Heart block
- Mask the signs of hypoglycemia
- Impaired glucose tolerance
- Rebound tachycardia (with abrupt stop)
- Bronchospasm- especially in non cardio selective
- Hypotension
- Fatigue
- Depression
- Insomnia
- Impotence
Contraindications
- Bradycardia
- Hypotension
- Second/third degree heart block
- Uncontrolled reactive airway disease
- Severe peripheral artery disease
- DM with frequent hypoglycemia
- HFrEF and unstable fluid status
CCB for angina
Dihydropyridine (DHP) amlodipine
MOA
- relax vascular smooth muscle -> vasodilation
- use only for long acting formulas
Non-dihydropyridine (Non-DHP) verapamil, diltiazem
MOA
- slow SA/AV node conduction
- decrease HR and contractility
Goal: reduce oxygen demand by decreasing workload
Key points
- Non-DHPs are generally more effective for angina
- Both types can be used in stable angina
- Avoid combining Non-DHPs + beta blockers (risk of bradycardia/heart block)
Side effects
Non-DHPs
- Bradycardia
- Hypotension
- Heart Block
- LV depression
- Headache
- Constipation (verapamil)
Fatigue
DHP:
- Ankle/leg edema
- Reflex tachycardia
- Hypotension
- Headache
- Gingival hyperplasia
- Fatigue
Long acting nitrates
Nitroglycerin, Isosorbide Mononitrate, Isosorbide Dinitrate
MOA
- Cause vasodilation (mostly veins > arteries)
- ↓ preload by pooling blood in veins → ↓ heart workload
Important points:
Can cause reflex sympathetic activation → ↑ heart rate and oxygen demand
- Using a beta blocker can reduce this reflex increase
Nitrates require a nitrate-free interval daily to prevent tolerance (so no continuous 24-hour coverage)
- can develop w/in 1-7days of continuous use
- leads to reduced efficacy
- increase dose does NOT overcome tolerance
Dosing strategy
- require 10-14hr nitrate-free interval daily
- commonly dose at night while sleeping
- patches should be removed after 12hrs, do NOT wear for full 24hrs
Caution
- avoid in pts w/ low baseline bp
- use cautiously if combines w/ low doses of CCB or BB that cause hypotension
Side effects
- Headache -> Will likely resolve within 2 weeks
- Flushing
- Dizziness
- Weakness
- Nausea
- Postural hypotension
- Syncope
- Reflex tachycardia
- Skin irritation (topical products)
- Increase ICP
- Rebound HTN & angina -> If abruptly discontinued
Angina treatment
Sublingual nitroglycerin + long-acting antianginal drug
1) BB preferred
- Decrease mortality- especially with prior MI
- Suppress nitrate-induced reflex tachy
2) If inadequate or contraindications:
- substitute NDHPs: If not taking a BB (due to side effects) and no bradycardia, AV block, HF
- Add OR Substitute: DHPs are safer: if need to combine w/ BB, good if pt has bradycardia, AV block, HF
- add/substitute a long-acting nitrate -> Need nitrate holiday
3. If inadequate or contraindications:
- add/substitute Ranolazine
Comorbid conditions preferred medications
Asthma
- verapamil or diltiazem, AVOID BB
Hyperthyroidism
- BB preferred
Depression
- CCB preferred, avoid BB
Vasospastic angina (cocaine use)
- CCB is drug of choice
Angina treatment algorithm
Rescue Therapy
- SL nitroglycerin (or spray) as needed
Initial Maintenance Therapy
β-Blockers >>> Non-DHP CCB as first line
- alternative: CCB or long-acting nitrates
if initial maintenance unsuccessful
- add on CCB or long-acting nitrates
- ranolazine may be added on or substituted
choices depends on HR and BP and responsiveness
Vasospastic Angina
CCB’s or long-acting nitrates
- may add-on long-acting nitrates to CCB’s and vis versa
β-blockers may induce alpha reflex vasoconstriction
- DO NOT GIVE
Aspirin for stable angina
Mechanism of Action
- irreversible inhibition of thromboxane (TXA2) production via COX-1
- Effects last the lifespan of the platelet (~7-10 days)
Dosing -> 81mg to 162mg by mouth daily
- ACS: 325mg loading dose then 81 mg daily
- higher maintenance doses = no further benefit
Alternative
- clopidogrel
Side-effects / Adverse Events
- dyspepsia, nausea, bleeding/bruising, thrombocytopenia
Clopidogrel for stable angina
Mechanism of Action
- Inhibits ADP binding to platelet P2Y12 receptor
- prevents activation of GPIIb/IIIa complex
- ↓ platelet aggregation
- Irreversible inhibition (platelet lifespan 7-10 days)
Good for stable angina or lower-risk ACSACS
Indications:
- Alternative to ASA in SIHD patients who can’t tolerate aspirin
- Used in DAPT for ACS patients (especially post-PCI or stenting)
Pharmacogenetic factors
- prodrug needing conversion to active metabolite by CYP2C19
- Slower onset compared to newer P2Y12 inhibitors
Ticagrelor for stable angina
Mechanism of Action
- Inhibits ADP binding to platelet P2Y12 receptor
- prevents activation of GPIIb/IIIa complex
- ↓ platelet aggregation
- Reversible inhibition
Preferred in ACS
Indications:
- Alternative to ASA in SIHD patients who can’t tolerate aspirin
- Used in DAPT for ACS patients (especially post-PCI or stenting)
Pharmacogenetic factors
- Not a prodrug: does not need conversion to active metabolite
- Faster onset compared to Clopidogrel