Ella Kulman - Respiratory
1/155
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
156 Terms
Name a disease thats responsible for reversible airway obstruction
asthma
what intrinsic factors can affect pneumonia?
cold temperature, infection, stress, exercise, various pollutants
what can cause acute airway obstruction?
tumour or foreign bodies with distal collapse of the lung
what can COPD be sub-divided into?
1. chronic bronchitis
2. emphysema
is chronic bronchitis reversible?
no, its irreversible
what is the clinical diagnosis of chronic bronchitis?
persistent cough and sputum for 3+ months in 2 consecutive years
what can happen over time in a pt with chronic bronchitis?
pt may become hypercapnic, hypoxic and have progressive right sided heart failure (cor pulmonale) due to pulmonary vasoconstriction - there is fibrosis and tissue destruction
what is the pathology of emphysema?
irritants and chemicals trigger inflammatory mediators to release matrix destructive enzymes → elastin destruction and enlargement of alveolar air spaces → air trapping
what can cause chronic bronchitis?
often tobacco smoking and can be aggravated by pollution and infections
what can cause emphysema?
often tobacco smoking, can also be associated with alpha-1-antitrypsin deficiency and coal dust exposure
what is bronchiectasis?
permanent dilation of bronchi due to obstruction and inflammation, this leads to a build-up of excess mucus and predisposes someone to chest infections
what is idiopathic pulmonary fibrosis?
progressive fibrosis in the alveoli that limits the pts ability to respire
what is the name of the lung disorder group that reflects inhaled dust/toxins?
pneumoconiosis
pneumoconiosis: what might be the consequences of asbestos exposure?
-lung cancer
-persistent pleural effusion
-diffuse pleural fibrosis
-diffuse interstitial lung fibrosis
What happens to the FEV1, FVC and FEV1/FVC ratio in an obstructive lung disease?
FEV1 is decreased, FVC is normal, FEV1/FVC ratio is decreased
what happens to the FVC and FEV1/FVC ratio in a restrictive lung disease?
FVC reduced, FEV1/FVC ratio normal
give an example of an irreversible obstructive lung disease
COPD
what is the affect of COPD on residual volume and total lung capacity?
RV and TLC are increased
give an example of a restrictive lung disease
pulmonary fibrosis
what factors can commonly exacerbate asthma?
cold weather, exertion, fumes, often worse at night
what is a normal tidal volume?
500ml
what is the transfer coefficient?
the ability of O2 to diffuse across the alveolar membrane
what is the name of the test that can functionally assess respiratory function?
6 minute walk
what is consolidation on a CXR?
regions of the lung filled with liquid e.g. pulmonary oedema - the areas appear white/dense

what are the potential complications of bronchoscopy?
pneumonia and pneumothorax
give 2 early and 2 late stage symptoms of lung cancer
early → change in cough, wheeze, haemoptysis
later → weight loss, lethargy
if a chronically breathless pt is wheezing, what is the likely cause?
obstruction
give 2 examples of non-respiratory causes of breathlessness
heart disease, anaemia
what are the common affects of rheumatoid arthritis on the lung?
-pleural effusion
-fibrosing alveolitis
-airway disorders e.g. bronchiolitis, bronchiectasis
give an example of a disease where there is tissue damage due to chronic infection
COPD
give 2 examples of diseases where there is an excessive immune response
ARDS, asthma
what viruses can cause pneumonia?
adenoviruses, influenza A and B, measles, VZV
which influenza pathogen is commonly behind severe and extensive outbreaks and why?
influenza A - replicates a lot and mutations are common
How can influenza virus be transmitted?
aerosol → coughing and sneezing - inhale particles
droplet → hand to hand
what is the reproduction number?
average number of secondary cases generated from a primary case
what is the treatment for influenza?
supportive care - antivirals maybe to reduce risk of transmission
how would you describe the airways in asthma?
hyper-reactive → this leads to inflammation
why are airways hyper-reactive in asthmatics?
-inflammatory infiltrate
-eosinophils
-epithelium destruction gives easier access to bronchoconstrictors
what broad class of drugs are commonly used to alleviate symptoms in asthma?
bronchodilators
what broad class of drugs are commonly used to target inflammation in asthma?
steroids
what type of beta adrenergic receptors are found in the lungs?
beta 2
where are beta 1 adrenergic receptors found?
in the heart
where are anti-inflammatory steroids produced?
adrenal cortex
give 2 effects of hydrocortisone
-metabolic
-anti inflammatory
give some potential side effects of prolonged hydrocortisone use
-muscle wasting
-osteoporosis
-increased risk of infection
what are the main cells responsible for inflammation in asthma?
mast cells and eosinophils
what are the main cells responsible for inflammation in COPD?
neutrophils and macrophages
describe the mechanism behind aspirin induced asthma
aspirin inhibits COX → increase in arachidonic acid. this is shunted and there is increased leukotriene production = INFLAMMATION
what is the advantage of having inhaled medications in the management of asthma?
inhaled meds are more likely to reach the target sites and there is reduced chance of side effects
name some groups of people who might be at increased risk of pneumonia
-elderly
-children
-people with COPD
-immunocompromised
-nursing home residents
briefly describe the pathogenesis of pneumonia
-bacteria translocate to normally sterile distal airway
-resident host defence is overwhelmed
-macrophages, chemokines and neutrophils produce an inflammatory response
what symptoms might you see in someone with pneumonia?
-productive cough
-sweats
-fever
-breathlessness
-pleuritic chest pain
myalgia/headache/arthralgia suggests atypical pneumonia
what investigations might you do in someone you suspect has pneumonia?
-CXR → look for air bronchogram in consolidated area
-FBC (look at WBCs)
-U+E
-LFT
-CRP
-microbiology → sputum culture, blood culture, serology etc
what is CURB65 used for?
way of assessing the severity of community acquired pneumonia - predicts mortality
name 2 bacteria that commonly cause pneumonia
-streptococcus pneumoniae
-haemophilus influenzae
describe s.pneumoniae
gram +ve cocci chain
describe haemophilus influenzae
gram -ve bacilli
what antibiotic would you give to someone with haemophilus influenzae?
co-amoxiclav or doxycycline
what can be a sign of effusion of CXR?
lots of consolidation
what is empyema?
pockets of pus that have collected in a body cavity e.g. in the lungs
give some signs of empyema
-WBC/CRP don't settle with antibiotics
-pain on deep inspiration
-pleural collection
what is the usual treatment for empyema?
drainage
name 3 groups of people who might be at risk of hospital acquired pneumonia
-elderly
-ventilator associated
-post op pts
what is bronchiolitis?
airway obstruction caused by inflammation of the bronchioles and increased mucus secretions
what can cause bronchiolitis and who is it most common in?
RSV (respiratory synctial virus), children
what is the difference between bronchitis and bronchiolitis?
bronchiolitis → inflammation of bronchioles
bronchitis → inflammation of bronchi epithelium due to irritants and chemicals
what investigations might you do in someone you suspect has infective bronchitis?
-CXR (often normal)
-viral and bacterial swabs
what is the usual cause of infective bronchitis?
mainly viral. acute bronchitis can be caused by adenoviruses
is pharyngitis normally caused by bacterial or viral infection?
viral e.g. rhinovirus, adenovirus etc
what bacteria might cause pharyngitis?
streptococcus pyogenes
what is the centor criteria used for?
determine the likelihood that a sore throat is bacterial
is sinusitis usually bacterial or viral?
viral
what are the symptoms of whooping cough in adults?
chronic cough, inspiratory 'whoop' posttussive vomiting
what causes croup?
parainfluenza virus
what is croup?
acute laryngotracheobronchitis - trachea, bronchi and larynx all affected
malignant bronchial tumours can be divided into 2 groups, what are they?
small cell and non small cell
which type of malignant bronchial tumour tends to have a worse prognosis?
small cell
give 5 environmental causes of lung cancer
-SMOKING
-asbestos exposure
-radon exposure
-coal tar exposure
-chromium exposure
the 5 year lung cancer survival rate is 8-10%, why is this?
people often present very late so treatment is much harder
what are the 3 main cell types that make up non small cell lung cancer?
squamus cell → 20%
adenocarcinoma → 40%
large cell
how does PET scanning work?
functional not anatomical - FDG is taken up rapidly by dividing cells, tumours therefore appear 'hot' on the scan
give symptoms of local disease lung cancer
-chest pain
-wheeze
-breathlessness
-cough
-haemoptysis
-recurrent chest infections
give symptoms of lung cancer that has metastasised
-bone pain, esp waking in the night
-headache
-seizures
-neurological defecit
-hepatic and/or abdo pain
-weight loss
name 5 places that lung cancer might metastasise to
-bone
-brain
-liver
-lymph nodes
-adrenal glands
what are paraneoplastic syndromes?
disorders triggered by an immune response to a neoplasm
give some examples of paraneoplastic syndromes
-finger clubbing
-anorexia
-weight loss
-hypercalcaemia
-hypernatraemia
what investigations might you do on someone to determine whether they have lung cancer?
-CXR
-CT scan
-bronchoscopy
-surgical and percutaneous biopsy
-bloods
what tests might you do on a pt to determine whether they're fit for operation?
-ECG
-lung function tests
-determine performance status
example of a malignant pleural tumour
mesothelioma
treatment for mesothelioma
-symptom control
-palliative chemotherapy or radiotherapy
-radical surgery (removal of tumour blood supply)
how does the treatment differ between local and systemic lung cancer?
local → surgery and radiotherapy
systemic → chemotherapy
give some side effects of radiotherapy
-fatigue
-anorexia
-cough
-oesophagitis
-systemic symptoms
give some side effects of chemotherapy
-alopecia
-nausea/vomiting
-peripheral neuropathy (nerve damage in extremities)
-constipation/diarrhoea
how might you diagnose pleural effusion?
-good hx
-imaging
-thoracentesis
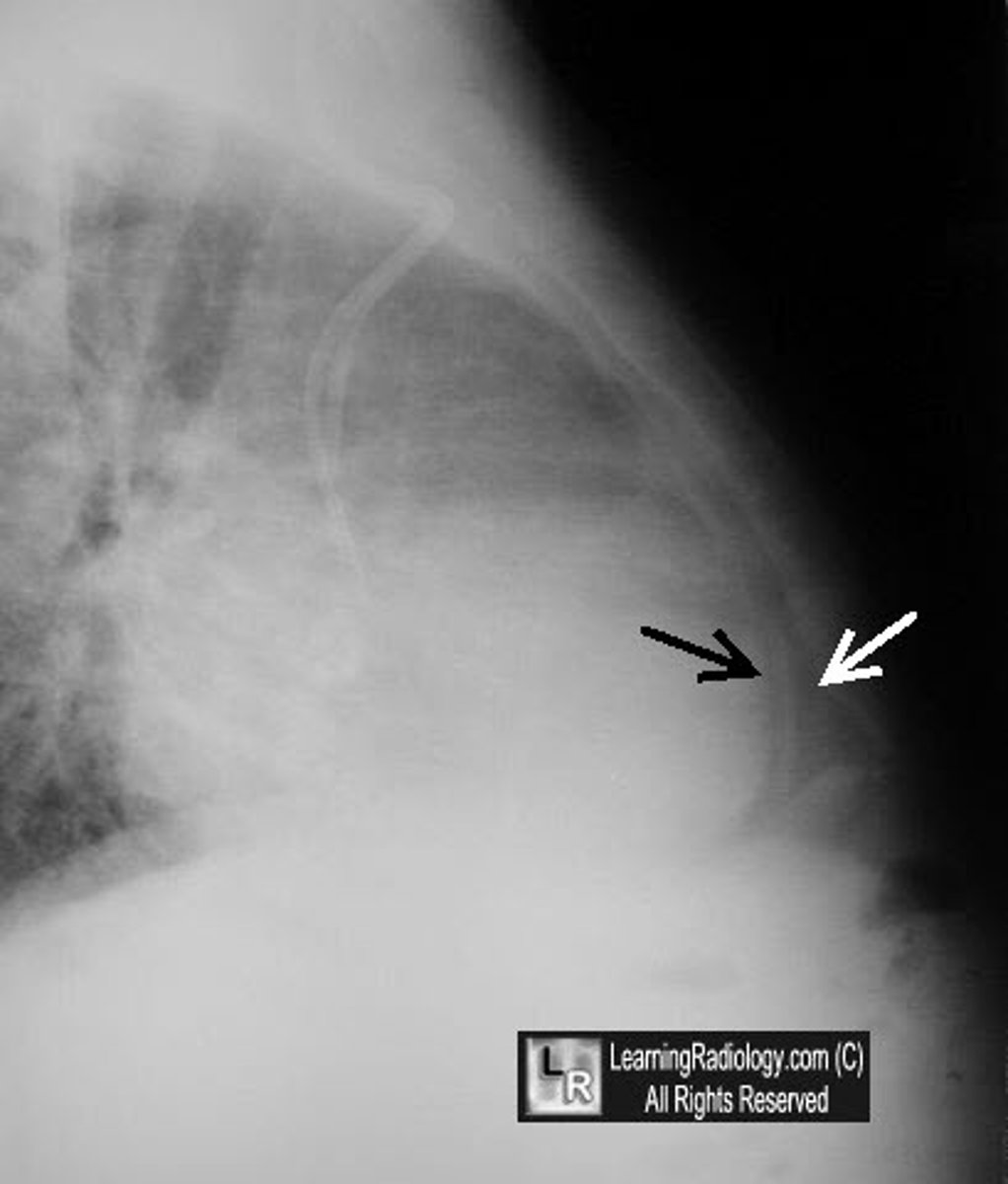
what is a pneumothorax?
air in the pleural space which can lead to partial or complete lung collapse
what do carotid and aortic bodies detect?
chemoreceptors respond to increased CO2 and decreased O2
what is type 1 respiratory failure?
hypoxia → decreased PaO2
PaCO2 is normal/slightly low due to hyperventilation
what is type 2 respiratory failure?
hypoxia and hypercapnia → decreased PaO2 and increased PaCO2 (there is alveolar hypoventilation)
give signs of hypercapnia
-bounding pulse
-flapping tremor
-confusion
what can cause type 1 respiratory failure?
-airway obstruction
-failure of O2 to diffuse into the blood
-V/Q mismatch
-alveolar hypoventilation